The Functional Assessment of the Shoulder in Water Polo Players with Surface Electromyography and Kinematic Analysis: A Pilot Study
Abstract
:Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
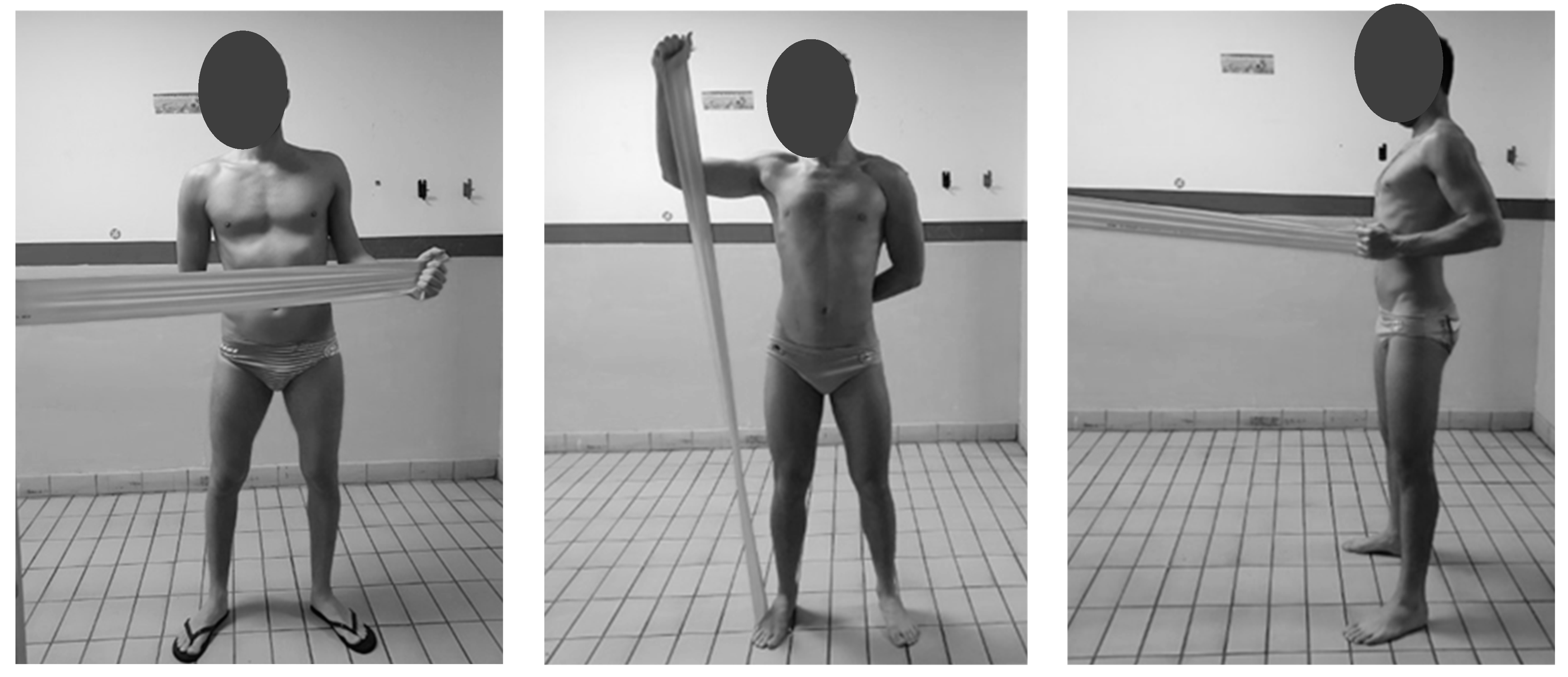
2.2. Exercise Protocol
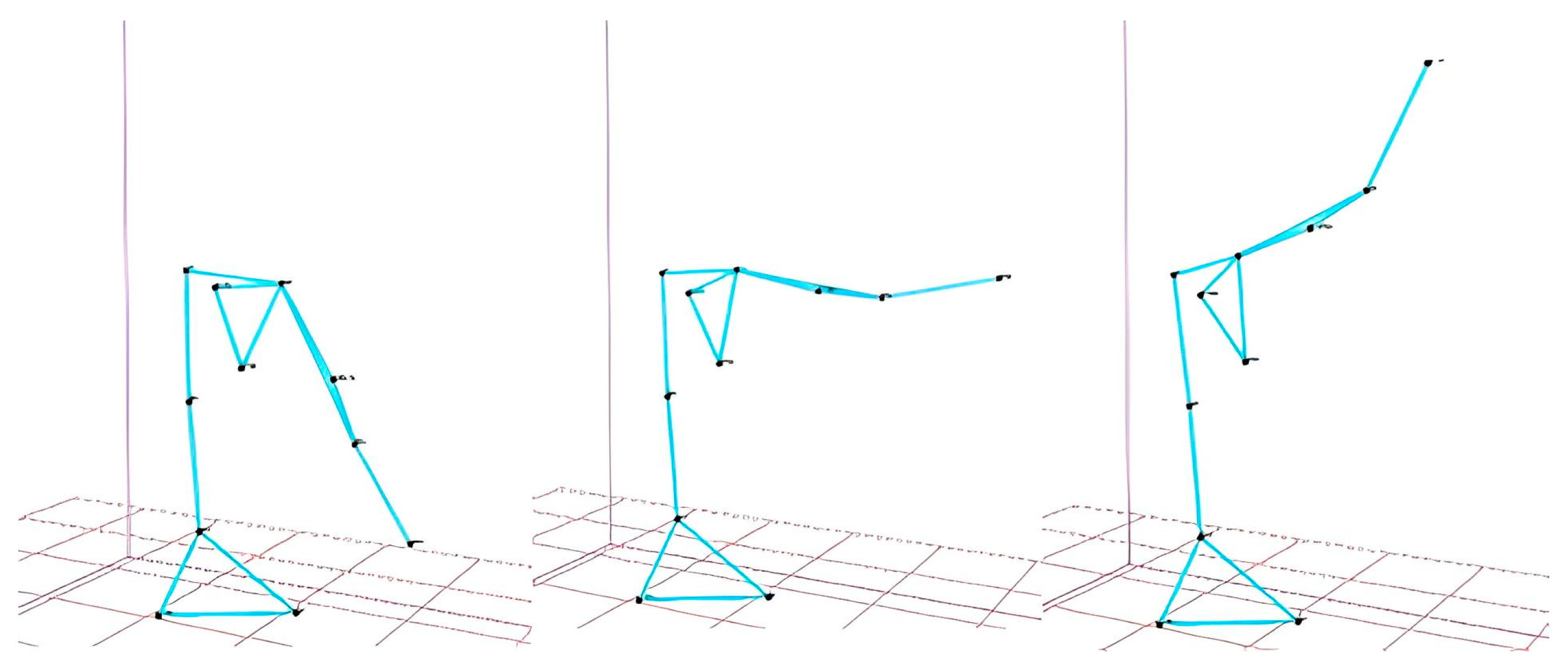
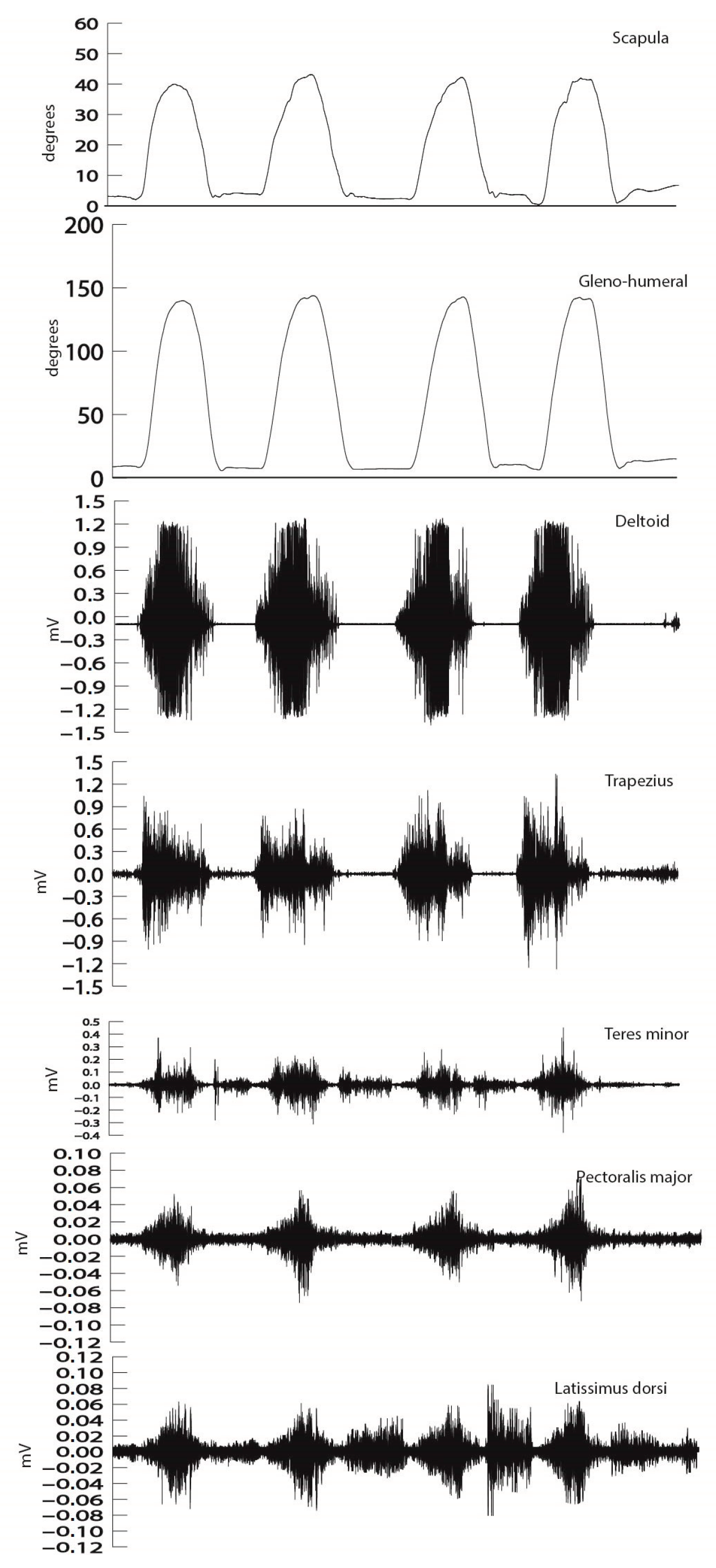
2.3. Data Analysis
3. Results
3.1. Reliability
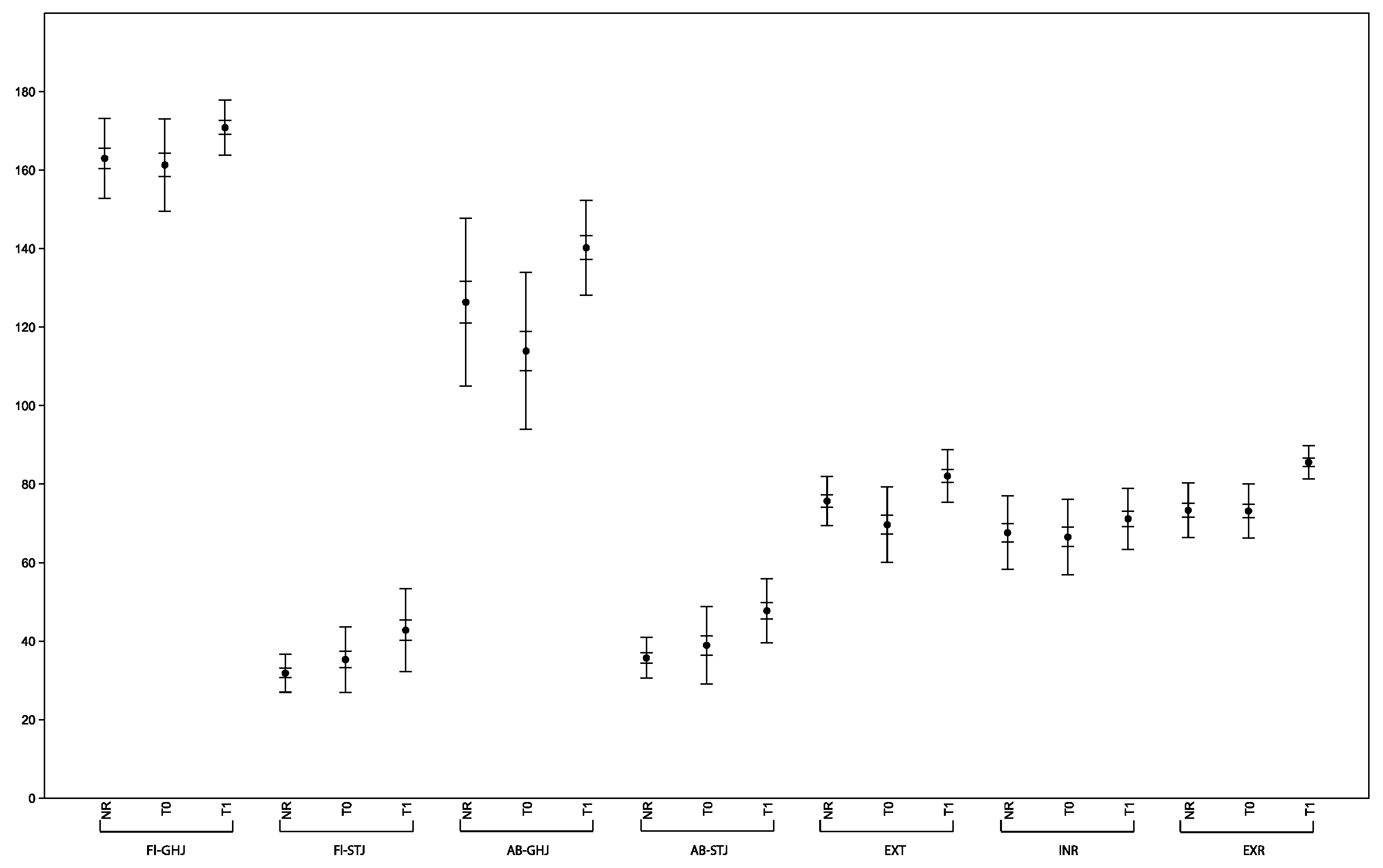
3.2. Kinematic Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Melchiorri, G.; Padua, E.; Padulo, J.; D’Ottavio, S.; Campagna, S.; Bonifazi, M. Throwing Velocity and Kinematics in Elite Male Water Polo Players. J. Sports Med. Phys. Fit. 2011, 51, 541–546. [Google Scholar]
- Miller, A.H.; Evans, K.; Adams, R.; Waddington, G.; Witchalls, J. Shoulder Injury in Water Polo: A Systematic Review of Incidence and Intrinsic Risk Factors. J. Sci. Med. Sport. 2018, 21, 368–377. [Google Scholar] [CrossRef]
- Croteau, F.; Brown, H.; Pearsall, D.; Robbins, S.M. Prevalence and Mechanisms of Injuries in Water Polo: A Systematic Review. BMJ Open Sport. Exerc. Med. 2021, 7, e001081. [Google Scholar] [CrossRef]
- López-Laval, I.; Sitko, S.; Cantonero, J.; Corbi, F.; Cirer-Sastre, R. The Effectiveness of Shoulder Mobility and Strength Programs in Competitive Water-Polo Players. Life 2022, 12, 758. [Google Scholar] [CrossRef]
- Nicolosi, S.; Quinto, A.; Lipoma, M.; Sgrò, F. Situational Analysis and Tactical Decision-Making in Elite Handball Players. Appl. Sci. 2023, 13, 8920. [Google Scholar] [CrossRef]
- O’Connor, S.; McCaffrey, N.; Whyte, E.; Moran, K. The Development and Reliability of a Simple Field-Based Screening Tool to Assess for Scapular Dyskinesis. J. Sport. Rehabil. 2016, 25, 2015-0054. [Google Scholar] [CrossRef] [PubMed]
- Papandreou, M.; Diamantis, E.; Vrachlioti, V.I.; Billis, E.; Gliatis, J. Clinical Evaluation of Static Scapular Posture in Overhead Athletes with Asymptomatic Shoulder Injuries. J. Sports Med. Phys. Fit. 2018, 58, 1071–1077. [Google Scholar] [CrossRef] [PubMed]
- Oyama, S.; Myers, J.B.; Wassinger, C.A.; Daniel Ricci, R.; Lephart, S.M. Asymmetric Resting Scapular Posture in Healthy Overhead Athletes. J. Athl. Train. 2008, 43, 565–570. [Google Scholar] [CrossRef]
- Preziosi Standoli, J.; Candela, V.; Bonifazi, M.; Gumina, S. Glenohumeral Internal Rotation Deficit in Young Asymptomatic Elite Swimmers. J. Athl. Train. 2024, 59, 731–737. [Google Scholar] [CrossRef]
- Bakshi, N.; Freehill, M.T. The Overhead Athletes Shoulder. Sports Med. Arthrosc. Rev. 2018, 26, 88–94. [Google Scholar] [CrossRef]
- De Sire, A.; Demeco, A.; Frizziero, A.; Marotta, N.; Spanò, R.; Carozzo, S.; Costantino, C.; Ammendolia, A. Risk of Injury and Kinematic Assessment of the Shoulder Biomechanics during Strokes in Padel Players: A Cross-Sectional Study. J. Sports Med. Phys. Fit. 2024, 64, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Porter, K.; Shield, A.; Pascoe, D.; Harvey, J.; Talpey, S. Does an Increase in Supraspinatus Tendon Thickness After Swimming Increase the Likelihood of Future Shoulder Pain? Sports Health 2024, 16, 358–362. [Google Scholar] [CrossRef] [PubMed]
- Ammendolia, A.; Marotta, N.; Demeco, A.; Marinaro, C.; Moggio, L.; Barletta, M.; Costantino, C. Effectiveness of Radial Shockwave Therapy in Calcific and Non-Calcific Tendinopathy of the Shoulder: A Systematic Review and Meta-Analysis. Muscles Ligaments Tendons J. 2020, 10, 40–47. [Google Scholar] [CrossRef]
- Schwank, A.; Blazey, P.; Asker, M.; Møller, M.; Hägglund, M.; Gard, S.; Skazalski, C.; Haugsbø Andersson, S.; Horsley, I.; Whiteley, R.; et al. 2022 Bern Consensus Statement on Shoulder Injury Prevention, Rehabilitation, and Return to Sport for Athletes at All Participation Levels. J. Orthop. Sports Phys. Ther. 2022, 52, 11–28. [Google Scholar] [CrossRef] [PubMed]
- Stokes, D.J.; McCarthy, T.P.; Frank, R.M. Physical Therapy for the Treatment of Shoulder Instability. Phys. Med. Rehabil. Clin. N. Am. 2023, 34, 393–408. [Google Scholar] [CrossRef]
- Ammendolia, A.; Marotta, N.; Marinaro, C.; Demeco, A.; Mondardini, P.; Costantino, C. The Synergic Use of the High Power Laser Therapy and Glu-Cosamine Sulfate in Knee Osteoarthritis: A Randomized Controlled Trial. Acta Biomed. 2021, 92, e2021237. [Google Scholar] [CrossRef]
- Palermi, S.; Gnasso, R.; Belviso, I.; Iommazzo, I.; Vecchiato, M.; Marchini, A.; Corsini, A.; Vittadini, F.; Demeco, A.; De Luca, M.; et al. Stem Cell Therapy in Sports Medicine: Current Applications, Challenges and Future Perspectives. J. Basic. Clin. Physiol. Pharmacol. 2023, 34, 699–706. [Google Scholar] [CrossRef] [PubMed]
- Carozzo, S.; Vatrano, M.; Coschignano, F.; Battaglia, R.; Calabrò, R.S.; Pignolo, L.; Contrada, M.; Tonin, P.; Cerasa, A.; Demeco, A. Efficacy of Visual Feedback Training for Motor Recovery in Post-Operative Subjects with Knee Replacement: A Randomized Controlled Trial. J. Clin. Med. 2022, 11, 7355. [Google Scholar] [CrossRef]
- Palermi, S.; Annarumma, G.; Spinelli, A.; Massa, B.; Serio, A.; Vecchiato, M.; Demeco, A.; Brugin, E.; Sirico, F.; Giada, F.; et al. Acceptability and Practicality of a Quick Musculoskeletal Examination into Sports Medicine Pre-Participation Evaluation. Pediatr. Rep. 2022, 14, 207–216. [Google Scholar] [CrossRef]
- Demeco, A.; Marotta, N.; Moggio, L.; Pino, I.; Marinaro, C.; Barletta, M.; Petraroli, A.; Palumbo, A.; Ammendolia, A. Quantitative Analysis of Movements in Facial Nerve Palsy with Surface Electromyography and Kinematic Analysis. J. Electromyogr. Kinesiol. 2021, 56, 102485. [Google Scholar] [CrossRef]
- Demeco, A.; de Sire, A.; Marotta, N.; Palumbo, A.; Fragomeni, G.; Gramigna, V.; Pellegrino, R.; Moggio, L.; Petraroli, A.; Iona, T.; et al. Effectiveness of Rehabilitation through Kinematic Analysis of Upper Limb Functioning in Wheelchair Basketball Athletes: A Pilot Study. Appl. Sci. 2022, 12, 2929. [Google Scholar] [CrossRef]
- De Sire, A.; Demeco, A.; Marotta, N.; Spanò, R.; Curci, C.; Farì, G.; Fortunato, F.; Iona, T.; Lippi, L.; Paolucci, T.; et al. Neuromuscular Impairment of Knee Stabilizer Muscles in a COVID-19 Cluster of Female Volleyball Players: Which Role for Rehabilitation in the Post-COVID-19 Return-to-Play? Appl. Sci. 2022, 12, 557. [Google Scholar] [CrossRef]
- Kraeutler, M.J.; Ciccotti, M.G.; Dodson, C.C.; Frederick, R.W.; Cammarota, B.; Cohen, S.B. Kerlan-Jobe Orthopaedic Clinic Overhead Athlete Scores in Asymptomatic Professional Baseball Pitchers. J. Shoulder Elb. Surg. 2013, 22, 329–332. [Google Scholar] [CrossRef] [PubMed]
- Sasagawa, K.; Kawabata, M.; Takaki, N.; Tsuruike, M.; Ellenbecker, T.S.; Tsuihiji, Y.; Watanabe, H.; Takahira, N.; Hirose, N. Reproducibility and Validity of the Kerlan-Jobe Orthopedic Clinic Shoulder and Elbow Score (Japanese Version). Cureus 2024, 16, e59139. [Google Scholar] [CrossRef] [PubMed]
- Walmsley, C.P.; Williams, S.A.; Grisbrook, T.; Elliott, C.; Imms, C.; Campbell, A. Measurement of Upper Limb Range of Motion Using Wearable Sensors: A Systematic Review. Sports Med. Open 2018, 4, 53. [Google Scholar] [CrossRef] [PubMed]
- Zheng, N.; Barrentine, S.W.; Fleisig, G.S.; Andrews, J.R. Kinematic Analysis of Swing in pro and Amateur Golfers. Int. J. Sports Med. 2008, 29, 487–493. [Google Scholar] [CrossRef] [PubMed]
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of Recommendations for SEMG Sensors and Sensor Placement Procedures. J. Electromyogr. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef]
- Weber, A.E.; Kontaxis, A.; O’Brien, S.J.; Bedi, A. The Biomechanics of Throwing: Simplified and Cogent. Sports Med. Arthrosc. Rev. 2014, 22, 72–79. [Google Scholar] [CrossRef] [PubMed]
- De Araújo, R.C.; Pirauá, A.L.T.; Beltrão, N.B.; Pitangui, A.C.R. Activity of Periscapular Muscles and Its Correlation with External Oblique during Push-up: Does Scapular Dyskinesis Change the Electromyographic Response? J. Sports Sci. 2018, 36, 571–577. [Google Scholar] [CrossRef]
- Seitz, A.L.; Uhl, T.L. Reliability and Minimal Detectable Change in Scapulothoracic Neuromuscular Activity. J. Electromyogr. Kinesiol. 2012, 22, 968–974. [Google Scholar] [CrossRef]
- Joseph, R.; Alenabi, T.; Lulic, T.; Dickerson, C.R. Activation of Supraspinatus and Infraspinatus Partitions and Periscapular Musculature During Rehabilitative Elastic Resistance Exercises. Am. J. Phys. Med. Rehabil. 2019, 98, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Mullaney, M.J.; Perkinson, C.; Kremenic, I.; Tyler, T.F.; Orishimo, K.; Johnson, C. EMG of Shoulder Muscles during Reactive Isometric Elastic Resistance Exercises. Int. J. Sports Phys. Ther. 2017, 12, 417–424. [Google Scholar]
- Kim, M.-K.; Lee, J.C.; Yoo, K.-T. The Effects of Shoulder Stabilization Exercises and Pectoralis Minor Stretching on Balance and Maximal Shoulder Muscle Strength of Healthy Young Adults with Round Shoulder Posture. J. Phys. Ther. Sci. 2018, 30, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Williams, G.R.; Kelley, M. Management of Rotator Cuff and Impingement Injuries in the Athlete. J. Athl. Train. 2000, 35, 300–315. [Google Scholar]
- Cools, A.M.J.; Struyf, F.; De Mey, K.; Maenhout, A.; Castelein, B.; Cagnie, B. Rehabilitation of Scapular Dyskinesis: From the Office Worker to the Elite Overhead Athlete. Br. J. Sports Med. 2014, 48, 692–697. [Google Scholar] [CrossRef] [PubMed]
- Baumgarten, K.M.; Osborn, R.; Schweinle, W.E.; Zens, M.J.; Helsper, E.A. Are Pulley Exercises Initiated 6 Weeks After Rotator Cuff Repair a Safe and Effective Rehabilitative Treatment? A Randomized Controlled Trial. Am. J. Sports Med. 2016, 44, 1844–1851. [Google Scholar] [CrossRef]
- Häberle, R.; Schellenberg, F.; List, R.; Plüss, M.; Taylor, W.R.; Lorenzetti, S. Comparison of the Kinematics and Kinetics of Shoulder Exercises Performed with Constant and Elastic Resistance. BMC Sports Sci. Med. Rehabil. 2018, 10, 22. [Google Scholar] [CrossRef]
- Peltonen, H.; Arokoski, J.; Kallinen, M.; Pullinen, T. Muscle Loading and Activation of the Shoulder Joint during Humeral External Rotation by Pulley and Variable Resistance. J. Electromyogr. Kinesiol. 2012, 22, 424–430. [Google Scholar] [CrossRef]
- Miyashita, K.; Kobayashi, H.; Koshida, S.; Urabe, Y. Glenohumeral, Scapular, and Thoracic Angles at Maximum Shoulder External Rotation in Throwing. Am. J. Sports Med. 2010, 38, 363–368. [Google Scholar] [CrossRef]
- Lädermann, A.; Chagué, S.; Kolo, F.C.; Charbonnier, C. Kinematics of the Shoulder Joint in Tennis Players. J. Sci. Med. Sport. 2016, 19, 56–63. [Google Scholar] [CrossRef]
- Anders, C.; Bretschneider, S.; Bernsdorf, A.; Erler, K.; Schneider, W. Activation of Shoulder Muscles in Healthy Men and Women under Isometric Conditions. J. Electromyogr. Kinesiol. 2004, 14, 699–707. [Google Scholar] [CrossRef]
- Thomas, S.J.; Swanik, C.B.; Kaminski, T.W.; Higginson, J.S.; Swanik, K.A.; Nazarian, L.N. Assessment of Subacromial Space and Its Relationship with Scapular Upward Rotation in College Baseball Players. J. Sport. Rehabil. 2013, 22, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Ludewig, P.M.; Reynolds, J.F. The Association of Scapular Kinematics and Glenohumeral Joint Pathologies. J. Orthop. Sports Phys. Ther. 2009, 39, 90–104. [Google Scholar] [CrossRef] [PubMed]
- Oyama, S.; Myers, J.B.; Wassinger, C.A.; Lephart, S.M. Three-Dimensional Scapular and Clavicular Kinematics and Scapular Muscle Activity during Retraction Exercises. J. Orthop. Sports Phys. Ther. 2010, 40, 169–179. [Google Scholar] [CrossRef] [PubMed]
- Dexel, J.; Kopkow, C.; Kasten, P. Scapulothoracic dysbalance in overhead athletes. Causes and therapy strategies. Orthopade 2014, 43, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Alberta, F.G.; ElAttrache, N.S.; Bissell, S.; Mohr, K.; Browdy, J.; Yocum, L.; Jobe, F. The Development and Validation of a Functional Assessment Tool for the Upper Extremity in the Overhead Athlete. Am. J. Sports Med. 2010, 38, 903–911. [Google Scholar] [CrossRef]
- Wymore, L.; Fronek, J. Shoulder Functional Performance Status of National Collegiate Athletic Association Swimmers: Baseline Kerlan-Jobe Orthopedic Clinic Scores. Am. J. Sports Med. 2015, 43, 1513–1517. [Google Scholar] [CrossRef]

| Measure | Group A | Group B |
|---|---|---|
| n | 16 | 16 |
| Age (years) | 20.8 ± 3.4 | 23.3 ± 4 |
| Height (cm) | 182.4 ± 3 | 183.7 ± 3.2 |
| BMI (kg/m2) | 23 ± 1.1 | 22.9 ± 0.928 |
| T0 | T1 | T1–T0 | Group A | ||
|---|---|---|---|---|---|
| Flexion | Fl-GHJ | 161.3° (11.78) | 170.87° (6.99) | 9.5 (9.84) | 163.00° (10.17) |
| Fl-STJ | 33.31° (8.36) | 40.5° (10.57) | 9.0 (12.98) * | 31.87° (4.84) | |
| Abduction | Ab-GHJ | 113.93° (19.98) | 140.25° (12.1) | 26.3 (19.0) * | 126.37° (21.37) |
| Ab-STJ | 38.93° (9.84) | 47.75° (8.16) | 8.8 (14.58) * | 37.75° (5.15) | |
| Extension | 69.68° (9.62) | 82.06° (6.67) | 12.4 (11.24) * | 75.68° (6.32) | |
| Internal Rotation | 68.93° (9.57) | 71.18° (7.7) | 8.8 (18.44) | 67.62° (9.35) | |
| External Rotation | 73.18° (6.92) | 85.56° (4.18) | 12.4 (7.1) * | 73.27° (6.96) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sgrò, F.; Demeco, A.; Marotta, N.; Merati, G.; Lipoma, M.; Ammendolia, A.; Costantino, C.; Iona, T. The Functional Assessment of the Shoulder in Water Polo Players with Surface Electromyography and Kinematic Analysis: A Pilot Study. Appl. Sci. 2024, 14, 7077. https://doi.org/10.3390/app14167077
Sgrò F, Demeco A, Marotta N, Merati G, Lipoma M, Ammendolia A, Costantino C, Iona T. The Functional Assessment of the Shoulder in Water Polo Players with Surface Electromyography and Kinematic Analysis: A Pilot Study. Applied Sciences. 2024; 14(16):7077. https://doi.org/10.3390/app14167077
Chicago/Turabian StyleSgrò, Francesco, Andrea Demeco, Nicola Marotta, Giampiero Merati, Mario Lipoma, Antonio Ammendolia, Cosimo Costantino, and Teresa Iona. 2024. "The Functional Assessment of the Shoulder in Water Polo Players with Surface Electromyography and Kinematic Analysis: A Pilot Study" Applied Sciences 14, no. 16: 7077. https://doi.org/10.3390/app14167077








