Exploring the Prognostic Impact of Non-Obstructive Coronary Artery Lesions through Machine Learning
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample Selection, Inclusion and Exclusion Criteria
2.2. Patient Classification Based on Coronary Angiography Findings and Follow-Up
2.3. Development of Predictive Machine Learning Models and Presentation of the Results Obtained
3. Results
3.1. General Characteristics of the Sample
3.2. Follow-Up Events
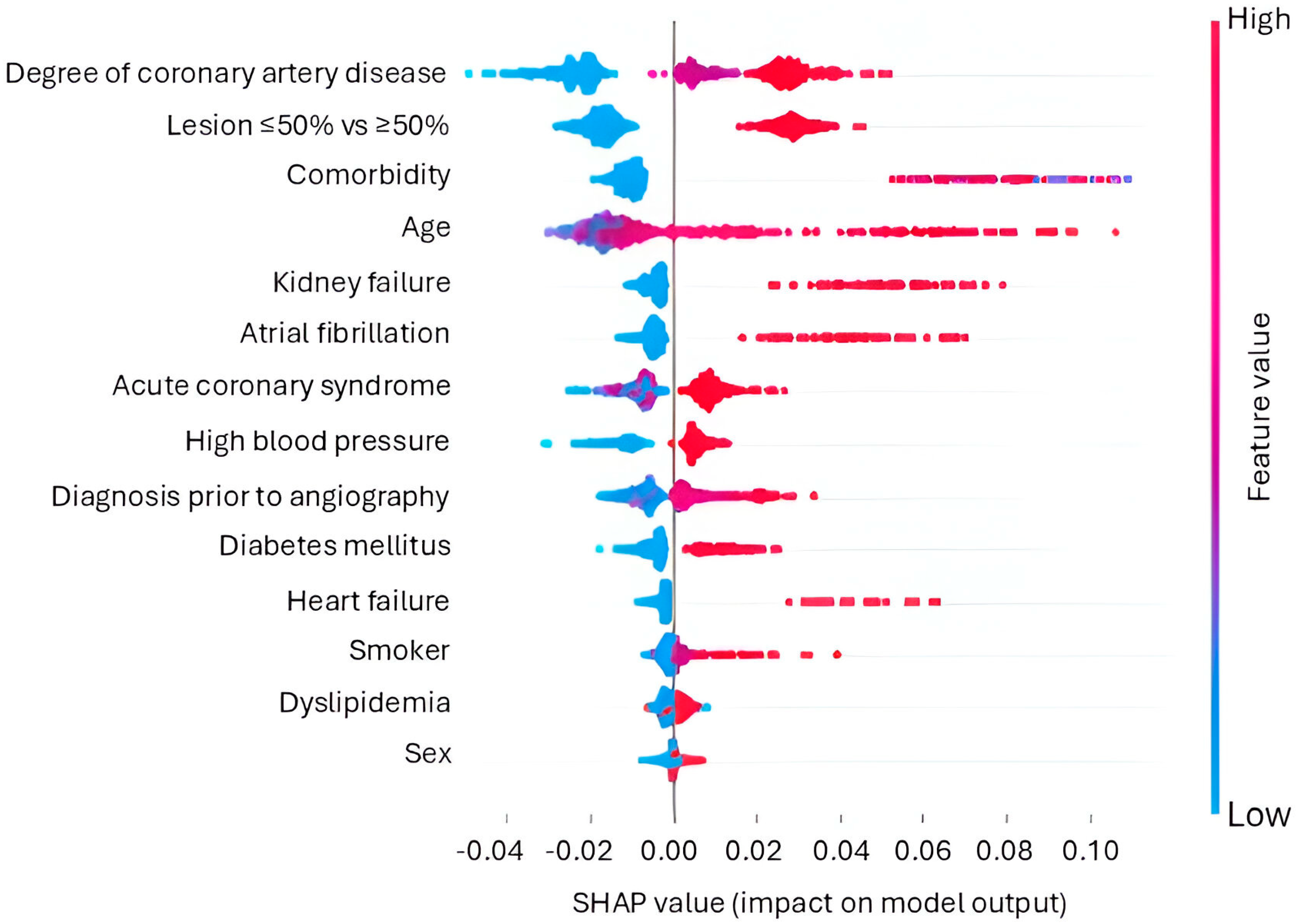
3.3. Performance of the Machine Learning Models
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.-A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the Management of Acute Coronary Syndromes. Eur. Heart J. 2023, 44, 3720–3826. [Google Scholar] [CrossRef] [PubMed]
- Finck, T.; Hardenberg, J.; Will, A.; Hendrich, E.; Haller, B.; Martinoff, S.; Hausleiter, J.; Hadamitzky, M. 10-Year Follow-Up After Coronary Computed Tomography Angiography in Patients With Suspected Coronary Artery Disease. JACC Cardiovasc. Imaging 2019, 12, 1330–1338. [Google Scholar] [CrossRef] [PubMed]
- Radico, F.; Zimarino, M.; Fulgenzi, F.; Ricci, F.; Di Nicola, M.; Jespersen, L.; Chang, S.M.; Humphries, K.H.; Marzilli, M.; De Caterina, R. Determinants of Long-Term Clinical Outcomes in Patients with Angina but without Obstructive Coronary Artery Disease: A Systematic Review and Meta-Analysis. Eur. Heart J. 2018, 39, 2135–2146. [Google Scholar] [CrossRef]
- Lee, J.M.; Choi, K.H.; Koo, B.-K.; Zhang, J.; Han, J.-K.; Yang, H.-M.; Park, K.W.; Song, Y.B.; Hahn, J.-Y.; Choi, S.-H.; et al. Intravascular Ultrasound or Optical Coherence Tomography-Defined Anatomic Severity and Hemodynamic Severity Assessed by Coronary Physiologic Indices. Rev. Esp. Cardiol. 2020, 73, 812–821. [Google Scholar] [CrossRef]
- Bzdok, D.; Altman, N.; Krzywinski, M. Statistics versus Machine Learning. Nat. Methods 2018, 15, 233–234. [Google Scholar] [CrossRef]
- Johnson, K.W.; Torres Soto, J.; Glicksberg, B.S.; Shameer, K.; Miotto, R.; Ali, M.; Ashley, E.; Dudley, J.T. Artificial Intelligence in Cardiology. J. Am. Coll. Cardiol. 2018, 71, 2668–2679. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Capitán, J.; Sánchez-Pérez, A.; Ballesteros-Pradas, S.; Millán-Gómez, M.; Cardenal-Piris, R.; Oneto-Fernández, M.; Gutiérrez-Alonso, L.; Rivera-López, R.; Guisado-Rasco, A.; Cano-García, M.; et al. Prognostic Implication of Non-Obstructive Coronary Lesions: A New Classification in Different Settings. J. Clin. Med. 2021, 10, 1863. [Google Scholar] [CrossRef]
- Cramer, J.S. The Origins of Logistic Regression. SSRN J. 2003, 4, 119. [Google Scholar] [CrossRef]
- Cortes, C.; Vapnik, V. Support-Vector Networks. Mach. Learn. 1995, 20, 273–297. [Google Scholar] [CrossRef]
- Quinlan, J.R. Induction of Decision Trees. Mach. Learn. 1986, 1, 81–106. [Google Scholar] [CrossRef]
- Breiman, L. Random Forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Friedman, N.; Geiger, D.; Goldszmidt, M. Bayesian Network Classifiers. Mach. Learn. 1997, 29, 131–163. [Google Scholar] [CrossRef]
- Costa, F.; Adamo, M.; Ariotti, S.; Ferrante, G.; Navarese, E.P.; Leonardi, S.; Garcia-Garcia, H.; Vranckx, P.; Valgimigli, M. Left Main or Proximal Left Anterior Descending Coronary Artery Disease Location Identifies High-Risk Patients Deriving Potentially Greater Benefit from Prolonged Dual Antiplatelet Therapy Duration. EuroIntervention 2016, 11, e1222–e1230. [Google Scholar] [CrossRef]
- Magboo, V.P.C.; Magboo, M.S.A. SPECT-MPI for Coronary Artery Disease: A Deep Learning Approach. Acta Med. Philipp. 2024, 58, 67–75. [Google Scholar] [CrossRef]
- Lee, C.-K.; Hong, J.-W.; Wu, C.-L.; Hou, J.-M.; Lin, Y.-A.; Huang, K.-C.; Tseng, P.-H. Real-Time Coronary Artery Segmentation in CAG Images: A Semi-Supervised Deep Learning Strategy. Artif. Intell. Med. 2024, 153, 102888. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Partinen, A.; Thurnhofer-Hemsi, K.; Rodríguez-Capitán, J.; Molina-Ramos, A.I.; Palomo, E.J. Coronary Artery Disease Classification With Different Lesion Degree Ranges Based on Deep Learning. IEEE Access 2024, 12, 69229–69239. [Google Scholar] [CrossRef]
- Mirzakhani, F.; Sadoughi, F.; Hatami, M.; Amirabadizadeh, A. Which Model Is Superior in Predicting ICU Survival: Artificial Intelligence versus Conventional Approaches. BMC Med. Inf. Decis. Mak. 2022, 22, 167. [Google Scholar] [CrossRef]
- Segar, M.W.; Hall, J.L.; Jhund, P.S.; Powell-Wiley, T.M.; Morris, A.A.; Kao, D.; Fonarow, G.C.; Hernandez, R.; Ibrahim, N.E.; Rutan, C.; et al. Machine Learning-Based Models Incorporating Social Determinants of Health vs Traditional Models for Predicting In-Hospital Mortality in Patients With Heart Failure. JAMA Cardiol. 2022, 7, 844–854. [Google Scholar] [CrossRef]
- Abdalrada, A.S.; Abawajy, J.; Al-Quraishi, T.; Islam, S.M.S. Machine Learning Models for Prediction of Co-Occurrence of Diabetes and Cardiovascular Diseases: A Retrospective Cohort Study. J. Diabetes Metab. Disord. 2022, 21, 251–261. [Google Scholar] [CrossRef]
- Zhu, H.; Qiao, S.; Zhao, D.; Wang, K.; Wang, B.; Niu, Y.; Shang, S.; Dong, Z.; Zhang, W.; Zheng, Y.; et al. Machine Learning Model for Cardiovascular Disease Prediction in Patients with Chronic Kidney Disease. Front. Endocrinol. 2024, 15, 1390729. [Google Scholar] [CrossRef]
- Mirjalili, S.R.; Soltani, S.; Meybodi, Z.H.; Marques-Vidal, P.; Firouzabadi, D.D.; Eshraghi, R.; Restrepo, D.; Ghoshouni, H.; Sarebanhassanabadi, M. Which Surrogate Insulin Resistance Indices Best Predict Coronary Artery Disease? A Machine Learning Approach. Cardiovasc. Diabetol. 2024, 23, 214. [Google Scholar] [CrossRef] [PubMed]
- Birdal, O.; İpek, E.; Saygı, M.; Doğan, R.; Pay, L.; Tanboğa, I.H. Cluster Analysis of Clinical, Angiographic, and Laboratory Parameters in Patients with ST-Segment Elevation Myocardial Infarction. Lipids Health Dis. 2024, 23, 166. [Google Scholar] [CrossRef] [PubMed]
- Oikonomou, E.K.; Aminorroaya, A.; Dhingra, L.S.; Partridge, C.; Velazquez, E.J.; Desai, N.R.; Krumholz, H.M.; Miller, E.J.; Khera, R. Real-World Evaluation of an Algorithmic Machine-Learning-Guided Testing Approach in Stable Chest Pain: A Multinational, Multicohort Study. Eur. Heart J.—Digit. Health 2024, 5, 303–313. [Google Scholar] [CrossRef]
- Forrest, I.S.; Petrazzini, B.O.; Duffy, Á.; Park, J.K.; Marquez-Luna, C.; Jordan, D.M.; Rocheleau, G.; Cho, J.H.; Rosenson, R.S.; Narula, J.; et al. Machine Learning-Based Marker for Coronary Artery Disease: Derivation and Validation in Two Longitudinal Cohorts. Lancet 2023, 401, 215–225. [Google Scholar] [CrossRef]
- Motwani, M.; Dey, D.; Berman, D.S.; Germano, G.; Achenbach, S.; Al-Mallah, M.H.; Andreini, D.; Budoff, M.J.; Cademartiri, F.; Callister, T.Q.; et al. Machine Learning for Prediction of All-Cause Mortality in Patients with Suspected Coronary Artery Disease: A 5-Year Multicentre Prospective Registry Analysis. Eur. Heart J. 2017, 38, 500–507. [Google Scholar] [CrossRef]
- Rothman, K.J.; Greenland, S. Causation and Causal Inference in Epidemiology. Am. J. Public. Health 2005, 95 (Suppl. S1), S144–S150. [Google Scholar] [CrossRef]
- Casolo, G.; Gabrielli, D.; Colivicchi, F.; Murrone, A.; Grosseto, D.; Gulizia, M.M.; Di Fusco, S.; Domenicucci, S.; Scotto di Uccio, F.; Di Tano, G.; et al. ANMCO POSITION PAPER: Prognostic and Therapeutic Relevance of Non-Obstructive Coronary Atherosclerosis. Eur. Heart J. Suppl. 2021, 23, C164–C175. [Google Scholar] [CrossRef] [PubMed]
- Nakazato, R.; Arsanjani, R.; Achenbach, S.; Gransar, H.; Cheng, V.Y.; Dunning, A.; Lin, F.Y.; Al-Mallah, M.; Budoff, M.J.; Callister, T.Q.; et al. Age-Related Risk of Major Adverse Cardiac Event Risk and Coronary Artery Disease Extent and Severity by Coronary CT Angiography: Results from 15 187 Patients from the International Multisite CONFIRM Study. Eur. Heart J. Cardiovasc. Imaging 2014, 15, 586–594. [Google Scholar] [CrossRef]
- Schulman-Marcus, J.; Hartaigh, B.Ó.; Gransar, H.; Lin, F.; Valenti, V.; Cho, I.; Berman, D.; Callister, T.; DeLago, A.; Hadamitzky, M.; et al. Sex-Specific Associations Between Coronary Artery Plaque Extent and Risk of Major Adverse Cardiovascular Events: The CONFIRM Long-Term Registry. JACC Cardiovasc. Imaging 2016, 9, 364–372. [Google Scholar] [CrossRef]
- Ouellette, M.L.; Löffler, A.I.; Beller, G.A.; Workman, V.K.; Holland, E.; Bourque, J.M. Clinical Characteristics, Sex Differences, and Outcomes in Patients With Normal or Near-Normal Coronary Arteries, Non-Obstructive or Obstructive Coronary Artery Disease. J. Am. Heart Assoc. 2018, 7, e007965. [Google Scholar] [CrossRef]
- Jespersen, L.; Abildstrom, S.Z.; Hvelplund, A.; Madsen, J.K.; Galatius, S.; Pedersen, F.; Hojberg, S.; Prescott, E. Burden of Hospital Admission and Repeat Angiography in Angina Pectoris Patients with and without Coronary Artery Disease: A Registry-Based Cohort Study. PLoS ONE 2014, 9, e93170. [Google Scholar] [CrossRef] [PubMed]
- Bugiardini, R.; Manfrini, O.; De Ferrari, G.M. Unanswered Questions for Management of Acute Coronary Syndrome: Risk Stratification of Patients with Minimal Disease or Normal Findings on Coronary Angiography. Arch. Intern. Med. 2006, 166, 1391–1395. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.J.; Zhang, L.L.; Elmariah, S.; Han, H.Y.; Zhou, Y.J. Prevalence and Prognosis of Nonobstructive Coronary Artery Disease in Patients Undergoing Coronary Angiography or Coronary Computed Tomography Angiography: A Meta-Analysis. Mayo Clin. Proc. 2017, 92, 329–346. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.H.; Park, G.-M.; Lee, S.-W.; Yun, S.-C.; Kim, Y.-H.; Cho, Y.-R.; Park, H.W.; Suh, J.; Yang, D.H.; Kang, J.-W.; et al. Long-Term Prognostic Value of Coronary CT Angiography in Asymptomatic Type 2 Diabetes Mellitus. JACC Cardiovasc. Imaging 2016, 9, 1292–1300. [Google Scholar] [CrossRef]
- Nicolosi, G.L. Artificial Intelligence in Cardiology: Why So Many Great Promises and Expectations, but Still a Limited Clinical Impact? J. Clin. Med. 2023, 12, 2734. [Google Scholar] [CrossRef]

| Characteristic | Lesion < 20% (n 1426) | Lesión 20–50% (n 643) | Lesion > 70% (n 1196) | p * |
|---|---|---|---|---|
| Age 1 (years) | 61.3 | 65.9 | 65.4 | <0.001 |
| Sex 2 (male) (%) | 40.5 | 56.8 | 73.8 | <0.001 |
| Hypertension (%) | 65.8 | 69.9 | 64.1 | 0.352 |
| Diabetes mellitus (%) | 28.0 | 29.2 | 35.7 | <0.001 |
| Dyslipidemia (%) | 47.5 | 51.8 | 50.0 | 0.233 |
| Smoking (%) | 32.7 | 39.8 | 44.5 | <0.001 |
| Acute coronary syndrome (%) | 34.6 | 38.4 | 67.2 | <0.001 |
| Heart failure (%) | 4.5 | 3.1 | 5.3 | 0.337 |
| Atrial fibrillation (%) | 13.5 | 10.3 | 6.0 | <0.001 |
| Left ventricular ejection fraction | ||||
| Normal (EF > 55%) (%) | 90.2 | 89.3 | 71.8 | <0.001 |
| Mild dysfunction (EF 40–55%) (%) | 5.7 | 5.8 | 16.0 | <0.001 |
| Severe dysfunction (Ef < 40%) (%) | 2.0 | 2.8 | 10.0 | <0.001 |
| Kidney failure (%) | 5.3 | 7.6 | 12.4 | <0.001 |
| Accuracy | Balanced Accuracy | Recall | Precision | F1 | AUC ROC | |
|---|---|---|---|---|---|---|
| Logistic regression | 0.87 | 0.52 | 0.066 | 0.41 | 0.10 | 0.74 |
| Support vector machines | 0.87 | 0.50 | 0.00 | 0 | 0 | 0.49 |
| Decision trees | 0.81 | 0.57 | 0.26 | 0.26 | 0.25 | 0.57 |
| Random forests | 0.85 | 0.53 | 0.10 | 0.26 | 0.14 | 0.69 |
| Naive Bayes classifier | 0.81 | 0.60 | 0.33 | 0.28 | 0.29 | 0.72 |
| True Negative | False Positive | False Negative | True Positive | |
|---|---|---|---|---|
| Logistic regression | 282.7 | 2.5 | 39.2 | 2.1 |
| Support vector machines | 285.2 | 0.0 | 41.3 | 0.0 |
| Decision trees | 254.1 | 31.1 | 30.1 | 11.2 |
| Random forests | 272.9 | 12.3 | 36.7 | 4.6 |
| Naive Bayes classifier | 251.6 | 33.6 | 27.3 | 14.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torres-Salomón, P.; Rodríguez-Capitán, J.; Molina-Cabello, M.A.; Thurnhofer-Hemsi, K.; Costa, F.; Sánchez-Fernández, P.L.; Muñoz-Muñoz, M.A.; Carmona-Segovia, A.d.M.; Romero-Cuevas, M.; Pavón-Morón, F.J.; et al. Exploring the Prognostic Impact of Non-Obstructive Coronary Artery Lesions through Machine Learning. Appl. Sci. 2024, 14, 9079. https://doi.org/10.3390/app14199079
Torres-Salomón P, Rodríguez-Capitán J, Molina-Cabello MA, Thurnhofer-Hemsi K, Costa F, Sánchez-Fernández PL, Muñoz-Muñoz MA, Carmona-Segovia AdM, Romero-Cuevas M, Pavón-Morón FJ, et al. Exploring the Prognostic Impact of Non-Obstructive Coronary Artery Lesions through Machine Learning. Applied Sciences. 2024; 14(19):9079. https://doi.org/10.3390/app14199079
Chicago/Turabian StyleTorres-Salomón, Pablo, Jorge Rodríguez-Capitán, Miguel A. Molina-Cabello, Karl Thurnhofer-Hemsi, Francesco Costa, Pedro L. Sánchez-Fernández, Mario Antonio Muñoz-Muñoz, Ada del Mar Carmona-Segovia, Miguel Romero-Cuevas, Francisco Javier Pavón-Morón, and et al. 2024. "Exploring the Prognostic Impact of Non-Obstructive Coronary Artery Lesions through Machine Learning" Applied Sciences 14, no. 19: 9079. https://doi.org/10.3390/app14199079






