Ultrasound-Induced Release Profile of Nimodipine from Drug-Loaded Block Copolymers after Singular vs. Repeated Sonication: In Vitro Analysis in Artificial Cerebrospinal Fluid
Abstract
1. Introduction
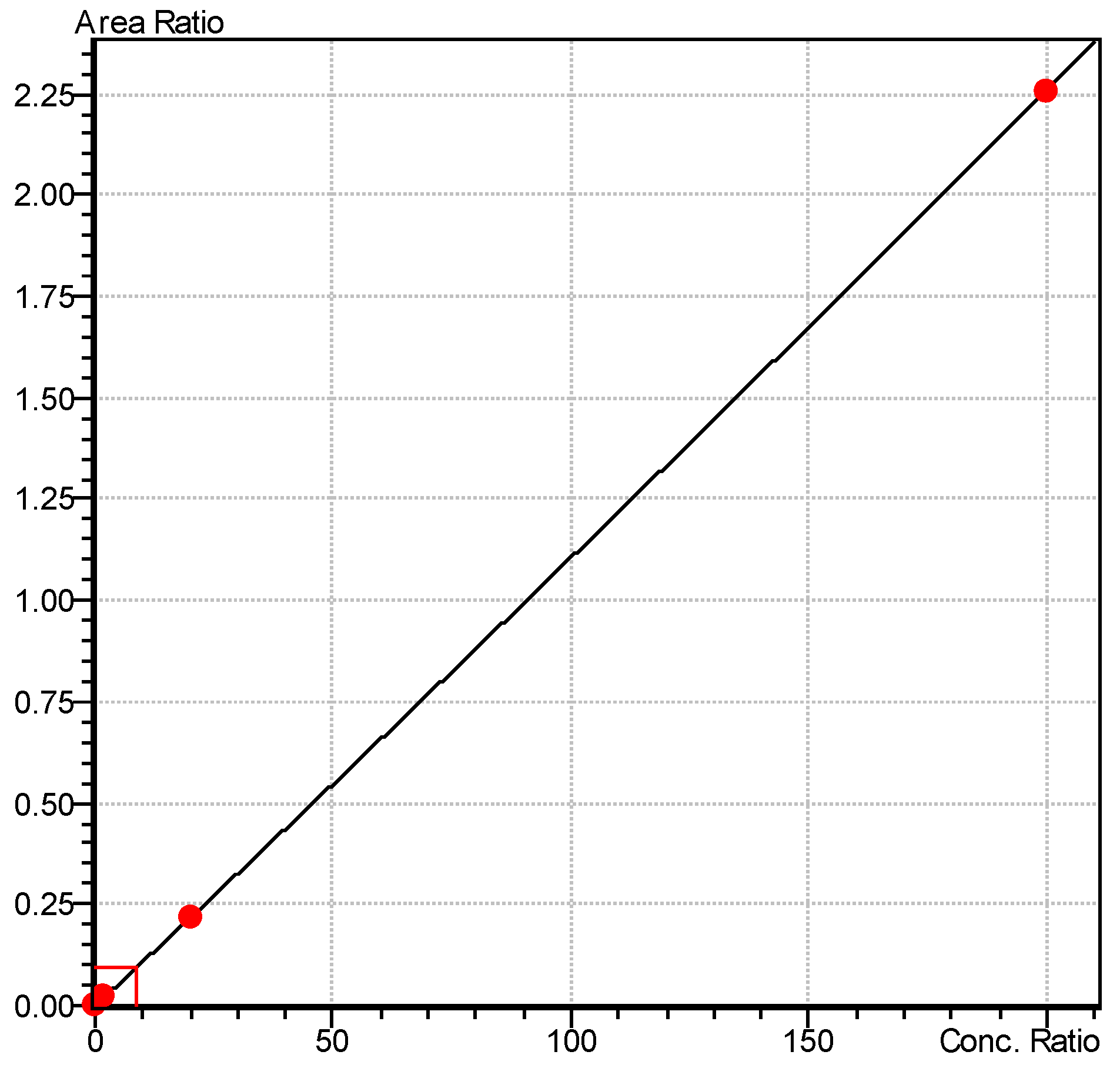
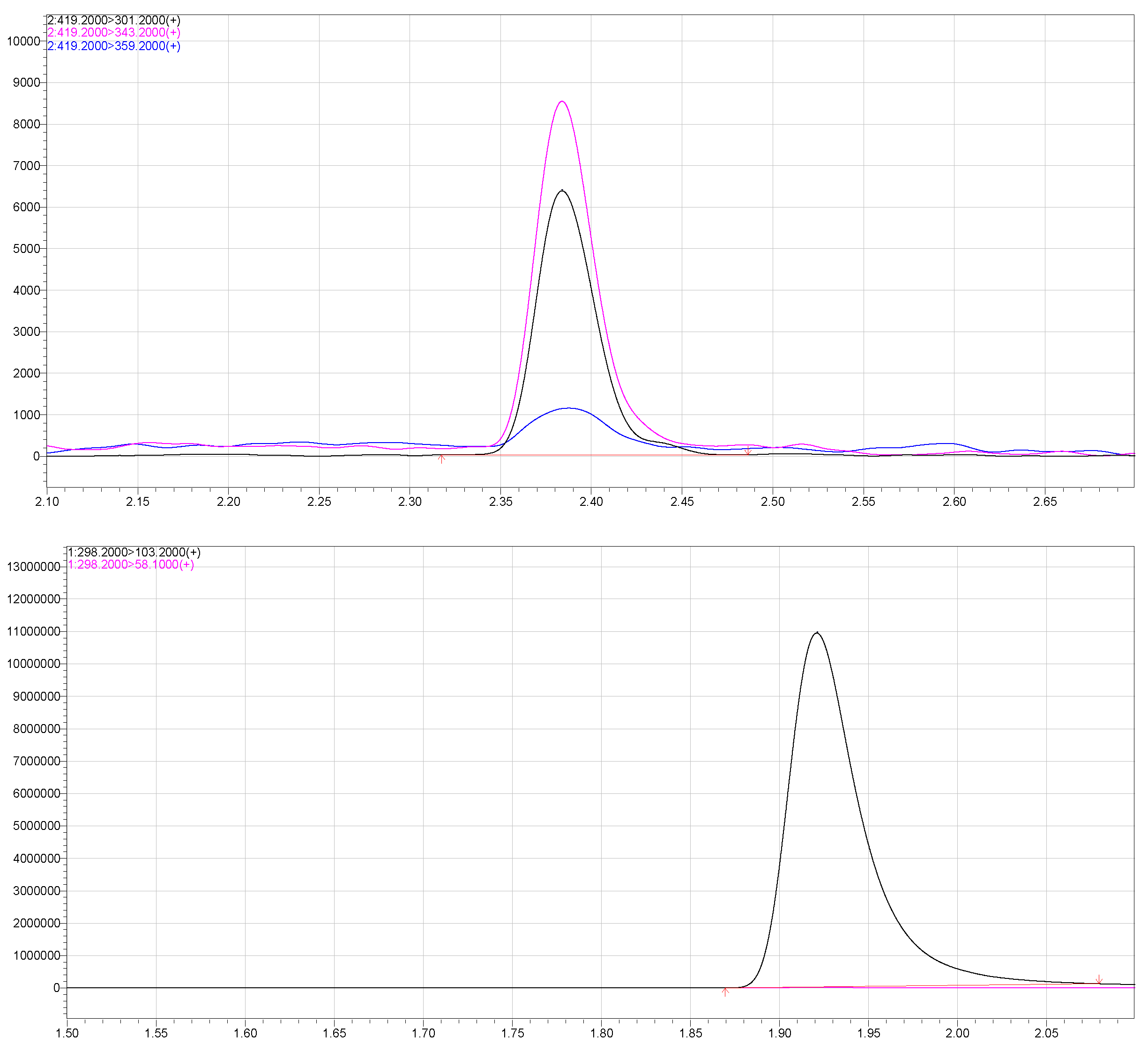
2. Materials and Methods
2.1. Artificial Cerebrospinal Fluid
2.2. Preparation of Nimodipine-Loaded Pluronic® F-127 Block Copolymers
2.3. Drug Release from Drug-Loaded-Pluronic® F 127 Block Copolymers
2.4. Spontaneous Nimodipine Release without External Influence
2.5. Ultrasound-Induced Nimodipine Release
2.6. Statistical Analysis
3. Results
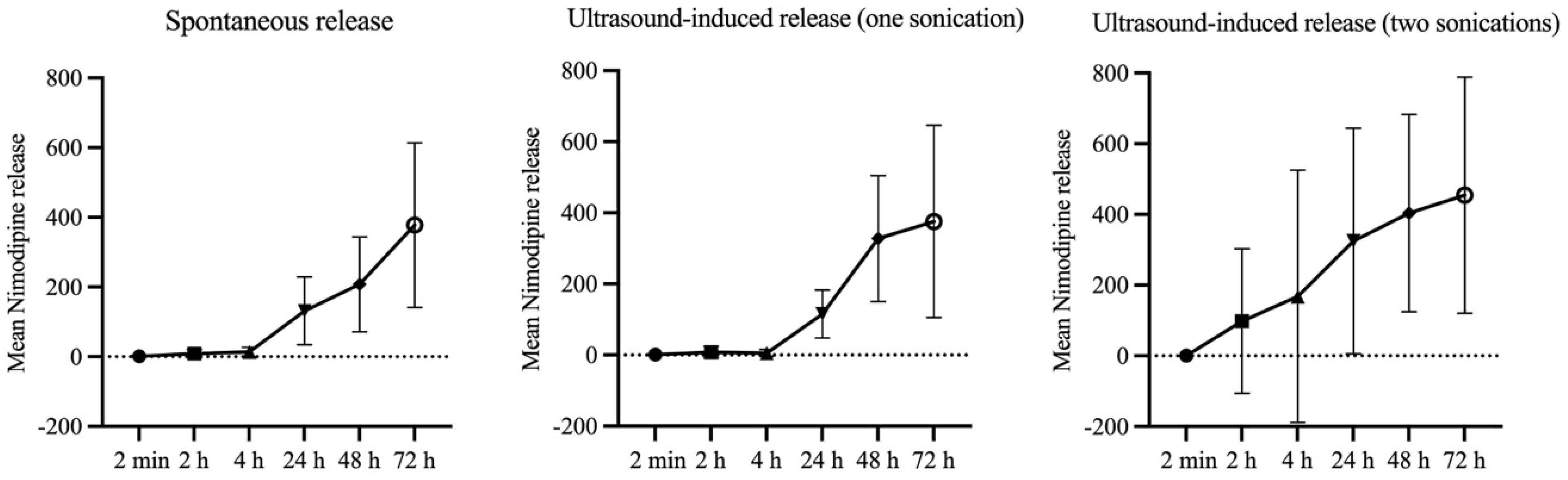
3.1. Spontaneous Release Profile of Nimodipine from Nimodipine-Loaded Pluronic® F 127 Block Copolymer
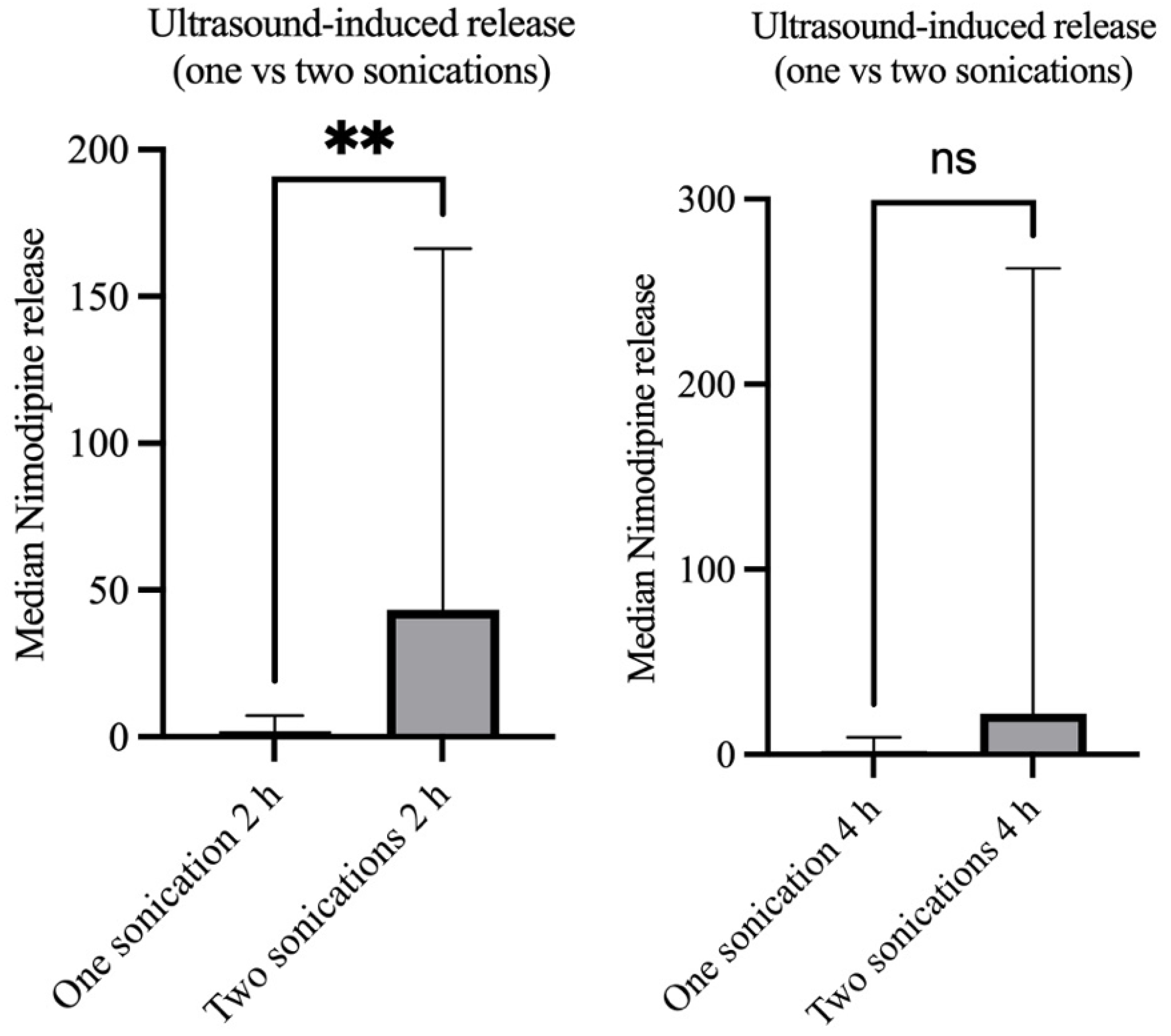
3.2. Ultrasound-Induced Drug-Release after Singular vs. Repeated Sonication
4. Discussion
4.1. Advantages and Limitations of Systemic Administration Routes for Nimodipine
4.2. Advantages and Limitation of Local Nimodipine Administration
4.3. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Budohoski, K.P.; Guilfoyle, M.; Helmy, A.; Huuskonen, T.; Czosnyka, M.; Kirollos, R.; Menon, D.K.; Pickard, J.D.; Kirkpatrick, P.J. The pathophysiology and treatment of delayed cerebral ischemia following subarachnoid hemorrhage. J. Neurol. Neurosurg. Psychiatry 2014, 85, 1343–1353. [Google Scholar] [CrossRef] [PubMed]
- Flynn, L.; Andrews, P. Advances in the understanding of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. F1000Research 2015, 4, 1200. [Google Scholar] [CrossRef]
- Francoeur, C.L.; Mayer, S.A. Management of delayed cerebral ischemia after subarachnoid hemorrhage. Crit. Care 2016, 20, 277. [Google Scholar] [CrossRef]
- Diringer, M.N.; Bleck, T.P.; Claude Hemphill, J., 3rd; Menon, D.; Shutter, L.; Vespa, P.; Bruder, N.; Sander Connolly, E., Jr.; Citerio, G.; Gress, D.; et al. Critical care management of patients following aneurysmal subarachnoid hemorrhage: Recommendations from the Neurocritical Care Society’s Multidisciplinary Consensus Conference. Neurocrit. Care 2011, 15, 211–240. [Google Scholar] [CrossRef]
- Dorhout Mees, S.M.; Rinkel, G.J.E.; Feigin, V.L.; Algra, A.; van den Bergh, W.M.; Vermeulen, M.; van Gijn, J. Calcium antagonists for aneurysmal subarachnoid hemorrhage. Cochrane Database Syst. Rev. 2007, 18, CD000277. [Google Scholar] [CrossRef]
- Sandow, N.; Diesing, D.; Sarrafzadeh, A.; Vajkoczy, P.; Wolf, S. Nimodipine dose reductions in the treatment of patients with aneurysmal subarachnoid hemorrhage. Neurocrit. Care 2016, 25, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Duran, S.; Mielke, D.; Rohde, V.; Malinova, V. Does nimodipine interruption due to high catecholamine doses lead to a greater incidence of delayed cerebral ischemia in the setting of aneurysmal subarachnoid hemorrhage? World Neurosurg. 2019, 132, e834–e840. [Google Scholar] [CrossRef] [PubMed]
- Hänggi, D.; Etminan, N.; Steiger, H.J.; Johnson, M.; Peet, M.M.; Tice, T.; Burton, K.; Hudson, B.; Turner, M.; Stella, A.; et al. A side-specific, sustained-release drug delivery system for aneurysmal subarachnoid hemorrhage. Neurotherapeutics 2016, 13, 439–449. [Google Scholar] [CrossRef] [PubMed]
- Mudshinge, S.R.; Deore, A.B.; Patil, S.; Bhalgat, C.M. Nanoparticles: Emerging carriers for drug delivery. Saudi Pharm. 2011, 19, 129–141. [Google Scholar] [CrossRef]
- Mdlovu, N.V.; Juang, R.S.; Weng, M.T.; Lin, K.S. Green synthesis and characterization of silicate nanostructures coated with Pluronic F127/gelatin for triggered drug delivery in tumor microenvironments. Int. J. Biol. Macromol. 2023, 251, 126337. [Google Scholar] [CrossRef]
- Pampaloni, N.P.; Giugliano, M.; Scaini, D.; Ballerini, L.; Rauti, R. Advances in nano neuroscience: From nanomaterials to nanotools. Front. Neurosci. 2019, 12, 953. [Google Scholar] [CrossRef] [PubMed]
- Opris, I.; Lebedev, M.A.; Pulgar, V.M.; Vidu, R.; Enachescu, M.; Casanova, M.F. Editorial: Nanotechnologies in neuroscience and neuroengineering. Front. Neurosci. 2020, 14, 33. [Google Scholar] [CrossRef]
- Hänggi, D.; Etminan, N.; Macdonald, R.L.; Steiger, H.J.; Mayer, S.A.; Aldrich, E.F.; Diringer, M.N.; Hoh, B.L.; Mocco, J.; Strange, P.; et al. NEWTON: Nimodipine microparticles to enhance recovery with reducing toxicity after subarachnoid hemorrhage. Neurocrit. Care 2015, 23, 274–284. [Google Scholar] [CrossRef] [PubMed]
- Chiappetta, D.; Sosnik, A. Poly(ethylene oxide)–poly(propylene oxide) block copolymer micellesas drug delivery agents: Improved hydrosolubility, stability and bioavailability of drugs. Eur. J. Pharm. Biopharm. 2007, 66, 303–317. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.; Wang, J.; Liu, J.; Qui, L.; Zhang, W.; Zhang, L. Liquid proliposomes of nimodipine drug delivery system: Preparation, characterization, and pharmacokinetics. AAPS Pharm. Sci. Tech. 2013, 14, 332–338. [Google Scholar] [CrossRef]
- Etminan, N.; Macdonald, R.L.; Davis, C.; Burton, K.; Steiger, H.J.; Hänggi, D. Intrathecal application of the nimodipine slow-release microparticle system eg-1962 for prevention of delayed cerebral ischemia and improvement of outcome after aneurysmal subarachnoid hemorrhage. Acta Neurochir. Suppl. 2015, 120, 281–286. [Google Scholar]
- Döring, K.; Sperling, S.; Ninkovic, M.; Schroeder, H.; Fischer, A.; Stadelmann, C.; Streit, F.; Binder, L.; Mielke, D.; Rohde, V.; et al. Ultrasound-Induced Release of Nimodipine from Drug-Loaded Block Copolymer Micelles: In Vivo Analysis. Transl. Stroke Res. 2022, 13, 792–800. [Google Scholar] [CrossRef] [PubMed]
- Sotoudegana, F.; Aminib, M.; Faizic, M.; Abofazelia, R. Nimodipine-loaded Pluronic® block copolymer micelles: Preparation, characterization, in-vitro and in-vivo studies. Iran. J. Pharm. Res. 2016, 15, 641–661. [Google Scholar]
- Döring, K.; Sperling, S.; Ninkovic, M.; Gasimov, T.; Stadelmann, C.; Streit, F.; Binder, L.; Rohde, V.; Malinova, V. Ultrasound-induced release of nimodipine from drug-loaded block copolymers: In vitro analysis. J. Drug Del. Sci. Technol. 2021, 66, 102834. [Google Scholar] [CrossRef]
- Bederson, J.B.; Connolly, E.S., Jr.; Batjer, H.H.; Dacey, R.G.; Dion, J.E.; Diringer, M.N.; Duldner, J.E., Jr.; Harbaugh, R.E.; Patel, A.B.; Rosenwasser, R.H.; et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: A statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke 2009, 40, 994–1025. [Google Scholar] [CrossRef]
- Raabe, A.; Beck, J.; Berkefeld, J.; Deinsberger, W.; Meixensberger, J.; Schmiedek, P.; Seifert, V.; Steinmetz, H.; Unterberg, A.; Vajkoczy, P.; et al. Recommendations for the management of patients with aneurysmal subarachnoid hemorrhage. Zentralbl. Neurochir. 2005, 66, 79–91. [Google Scholar] [CrossRef] [PubMed]
- Vatter, H.; Seifert, V. Vasospams pharmacology. Acta Neurochir. Suppl. 2009, 104, 115–118. [Google Scholar]
- Geraldini, F.; De Cassai, A.; Diana, P.; Correale, C.; Boscolo, A.; Zampirollo, S.; Disaro, L.; Carere, A.; Cacco, N.; Navalesi, P.; et al. A comparison between enteral and intravenoius nimodipine in subarachnoid hemorrhage: A systematic review and network meta-analysis. Neurocrit. Care 2022, 36, 1071–1079. [Google Scholar] [CrossRef] [PubMed]
- Lei, G.; Rao, Z.; Hu, Y. The efficacy of different nimodipine administration route for treating subarachnoid hemorrhage: A network meta-analysis. Medicine 2023, 102, e34789. [Google Scholar] [CrossRef]
- Mahmoud, S.H.; Hefny, F.R.; Panos, N.G.; Delucilla, L.; Ngan, Z.; Perreault, M.M.; Hamilton, L.A.; Rowe, A.S.; Buschur, P.L.; Owusu-Guha, J.; et al. Comparison of nimodipine formulations and administration techniques via enteral feeding tubes in patients with aneurysmal subarachnoid hemorrhage: A multicenter retrospective cohort study. Pharmacotherapy 2023, 43, 279–290. [Google Scholar] [CrossRef]
- Rass, V.; Kindl, P.; Lindner, A.; Kofler, M.; Altmann, K.; Putnina, L.; Ianosi, B.A.; Schiefecker, A.J.; Beer, R.; Pfausler, B.; et al. Blood pressure changes in association with nimodipine therapy in patients with spontaneous subarachnoid hemorrhage. Neurocrit. Care 2023, 39, 104–115. [Google Scholar] [CrossRef]
- Moser, M.; Schwarz, Y.; Herta, J.; Plöchl, W.; Reinprecht, A.; Zeitlinger, M.; Brugger, J.; Ramazanova, D.; Rössler, K.; Hosmann, A. The effect of oral nimodipine on cerebral metabolism and hemodynamic parameters in patients suffering aneurysmal subarachnoid hemorrhage. J. Neurosurg. Anesthesiol. 2023, 36, 317–325. [Google Scholar] [CrossRef]
- Carlson, A.P.; Hänggi, D.; Macdonald, R.L.; Shuttleworth, C.W. Nimodipine reappraised: An old drug with a future. Curr. Neuropharmacol. 2020, 18, 65–82. [Google Scholar] [CrossRef]
- Kerschbaumer, J.; Freyschlag, C.F.; Petr, O.; Adage, T.; Breitenbach, J.J.; Wessels, L.; Wolf, S.; Hecht, N.; Gempt, J.; Wostrack, M.; et al. A randomized, single ascending dose safety, tolerability, and pharmacokinetics study of NicaPlant in aneurysmal subarachnoid hemorrhage patients undergoing clipping. Brain Spine 2023, 3, 102673. [Google Scholar] [CrossRef] [PubMed]
- Kasuya, H.; Onda, H.; Sasahara, A.; Takeshita, M.; Hori, T. Application of nicardipine prolonged-release implants: Analysis of 97 consecutive patients with acute subarachnoid hemorrhage. Neurosurgery 2005, 56, 895–902. [Google Scholar] [CrossRef]
- Vandenbulcke, A.; Messerer, M.; Garvayo Navarro, M.; Peters, D.R.; Starnoni, D.; Giammattei, L.; Ben-Hamouda, N.; Puccinelli, F.; Saliou, G.; Cossu, G.; et al. Cisternal nicardipine for prevention of delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage: A comparative retrospective cohort study. Acta Neurochir. 2024, 166, 133. [Google Scholar] [CrossRef] [PubMed]
- Barth, M.; Pena, P.; Seiz, M.; Thomé, C.; Muench, E.; Weidauer, S.; Hattingen, E.; Kasuya, H.; Schmiedek, P. Feasibility of intraventricular nicardipine prolonged release implants in patients following aneurysmal subarachnoid haemorrhage. Br. J. Neurosurg. 2011, 25, 677–683. [Google Scholar] [CrossRef] [PubMed]
- Hänggi, D.; Etminan, N.; Aldrich, F.; Steiger, H.J.; Mayer, S.A.; Diringer, M.N.; Hoh, B.L.; Mocco, J.; Faleck, H.J.; Loch Macdonald, R.; et al. Randomized, open-label, phase 1/2a study to determine the maximum tolerated dose of intraventricular sustained release nimodipine for subarachnoid hemorrhage (NEWTON [Nimodipine microparticles to enhance recovery while reducing toxicity after subarachnoid hemorrhage]). Stroke 2017, 48, 145–151. [Google Scholar]
- Macdonald, R.L.; Hänggi, D.; Ko, N.U.; Darsaut, T.E.; Carlson, A.P.; Wong, G.K.; Etminan, N.; Mayer, S.A.; Aldrich, E.F.; Diringer, M.N.; et al. NEWTON-2 Cisternal (Nimodipine Microparticles to Enhance Recovery While Reducing Toxicity After Subarachnoid Hemorrhage): A Phase 2, Multicenter, Randomized, Open-Label Safety Study of Intracisternal EG-1962 in Aneurysmal Subarachnoid Hemorrhage. Neurosurgery 2020, 88, E13–E26. [Google Scholar] [CrossRef]


| Experimental Settings | Mean | SD | Median | 95% CI | IQR |
|---|---|---|---|---|---|
| Control group without sonication | |||||
| Control group 2 min | 1.439 | 3.010 | 0.20 | 0.2–7.58 | 0.20–5.40 |
| Control group 15 min | 3.588 | 8.185 | 0.20 | 0.19–20.30 | 0.19–5.40 |
| Control group 30 min | 4.867 | 6.757 | 0.24 | 0.2–17.6 | 0.20–9.12 |
| Control group 2 h | 8.547 | 11.60 | 2.91 | 0.2–28.85 | 0.46–19.11 |
| Control group 4 h | 13.35 | 13.67 | 10.88 | 0.2–36.43 | 1.01–24.42 |
| Control group 24 h | 131.6 | 96.90 | 118.3 | 0.2–246.6 | 51.93–239.6 |
| Control group 48 h | 207.7 | 136.2 | 219.0 | 0.2–382.40 | 104.1–305.7 |
| Control group 72 h | 377.7 | 236.0 | 355.3 | 0.2–681.9 | 228.3–597.1 |
| Treatment group with a singular sonication | |||||
| One sonication 2 min | 1.243 | 1.539 | 0.546 | 0.24–4.21 | 0.29–2.24 |
| One sonication 15 min | 1.303 | 2.291 | 0.454 | 0.20–5.97 | 0.21–1.88 |
| One sonication 30 min | 1.226 | 1.687 | 0.607 | 0.20–4.63 | 0.35–1.83 |
| One sonication 2 h | 8.296 | 16.31 | 1.624 | 0.20–41.50 | 0.86–13.18 |
| One sonication 4 h | 5.606 | 9.520 | 1.822 | 0.20–24.83 | 0.61–9.35 |
| One sonication 24 h | 115.8 | 67.53 | 124.2 | 0.20–200.4 | 70.40–164.1 |
| One sonication 48 h | 327.5 | 176.8 | 360.0 | 0.43–506.2 | 220.3–460.2 |
| One sonication 72 h | 375.8 | 270.1 | 357.2 | 0.20–754.4 | 145.5–632.5 |
| Treatment group with repeated sonication | |||||
| Repeated sonication 2 min | 0.532 | 0.544 | 0.27 | 0.20–1.58 | 0.20–0.90 |
| Repeated sonication 15 min | 1.292 | 2.414 | 0.20 | 0.20–6.20 | 0.20–2.11 |
| Repeated sonication 30 min | 98.72 | 177.4 | 14.85 | 0.51–364.7 | 3.82–277.5 |
| Repeated sonication 2 h | 98.25 | 204.9 | 17.48 | 6.15–516.3 | 8.10–146.6 |
| Repeated sonication 4 h | 168.0 | 357.1 | 22.09 | 0.64–896.1 | 11.96–262.7 |
| Repeated sonication 24 h | 395.6 | 461.7 | 204.0 | 0.65–1226 | 80.44–780.6 |
| Repeated sonication 48 h | 403.7 | 279.2 | 422.8 | 0.54–727.1 | 166.7–651.9 |
| Repeated sonication 72 h | 454.5 | 334.3 | 540.3 | 0.96–736.3 | 102.5–720.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Döring, K.; Sperling, S.; Ninkovic, M.; Lanfermann, H.; Streit, F.; Fischer, A.; Rohde, V.; Malinova, V. Ultrasound-Induced Release Profile of Nimodipine from Drug-Loaded Block Copolymers after Singular vs. Repeated Sonication: In Vitro Analysis in Artificial Cerebrospinal Fluid. Brain Sci. 2024, 14, 912. https://doi.org/10.3390/brainsci14090912
Döring K, Sperling S, Ninkovic M, Lanfermann H, Streit F, Fischer A, Rohde V, Malinova V. Ultrasound-Induced Release Profile of Nimodipine from Drug-Loaded Block Copolymers after Singular vs. Repeated Sonication: In Vitro Analysis in Artificial Cerebrospinal Fluid. Brain Sciences. 2024; 14(9):912. https://doi.org/10.3390/brainsci14090912
Chicago/Turabian StyleDöring, Katja, Swetlana Sperling, Milena Ninkovic, Heinrich Lanfermann, Frank Streit, Andreas Fischer, Veit Rohde, and Vesna Malinova. 2024. "Ultrasound-Induced Release Profile of Nimodipine from Drug-Loaded Block Copolymers after Singular vs. Repeated Sonication: In Vitro Analysis in Artificial Cerebrospinal Fluid" Brain Sciences 14, no. 9: 912. https://doi.org/10.3390/brainsci14090912
APA StyleDöring, K., Sperling, S., Ninkovic, M., Lanfermann, H., Streit, F., Fischer, A., Rohde, V., & Malinova, V. (2024). Ultrasound-Induced Release Profile of Nimodipine from Drug-Loaded Block Copolymers after Singular vs. Repeated Sonication: In Vitro Analysis in Artificial Cerebrospinal Fluid. Brain Sciences, 14(9), 912. https://doi.org/10.3390/brainsci14090912






