Design and Implementation of Airway Response Teams to Improve the Practice of Emergency Airway Management
Abstract
:1. Introduction
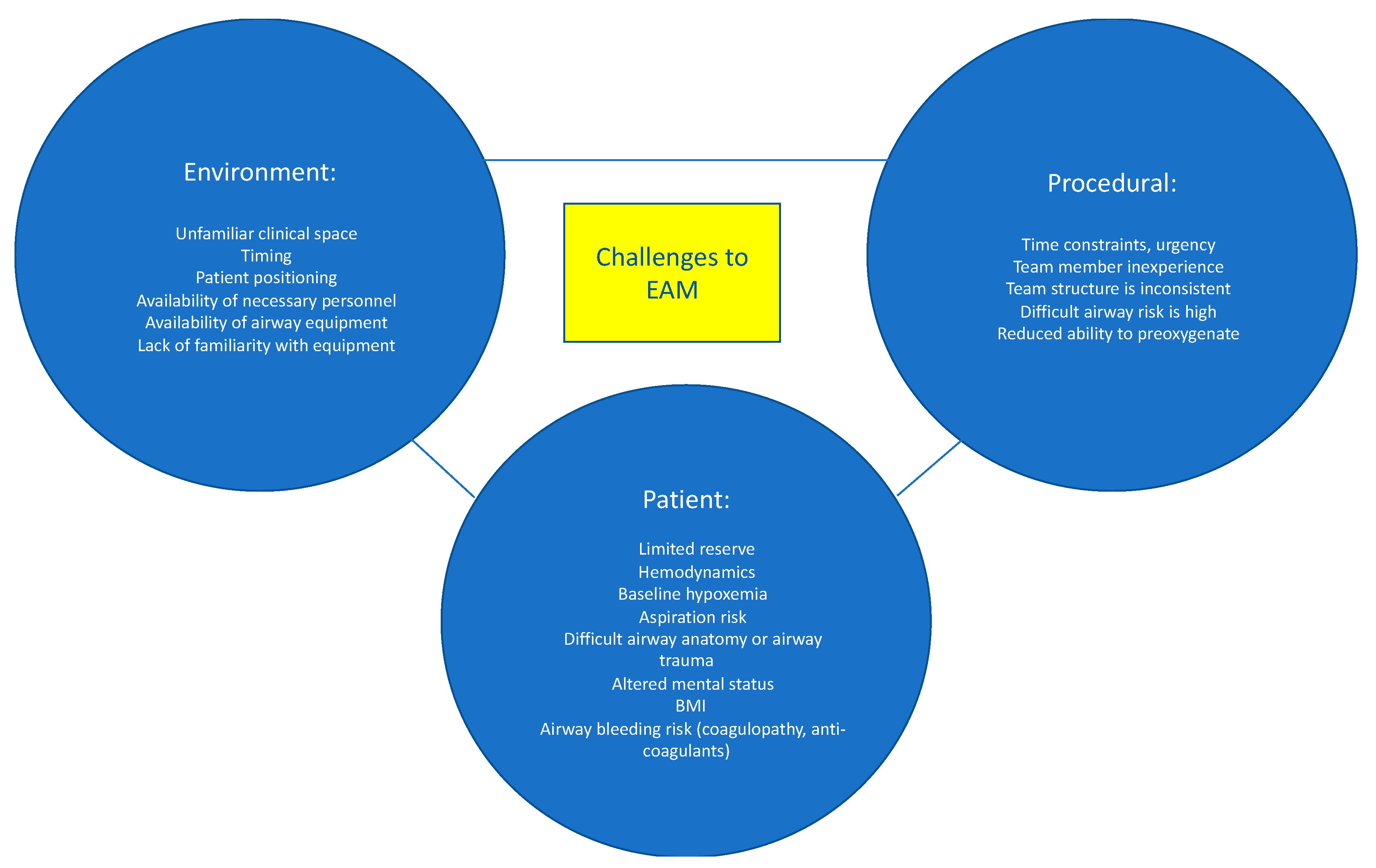
2. Risks Associated with EAM
3. Challenges in EAM
4. Rationale for an Airway Response Team
5. The Team Model
6. Activation
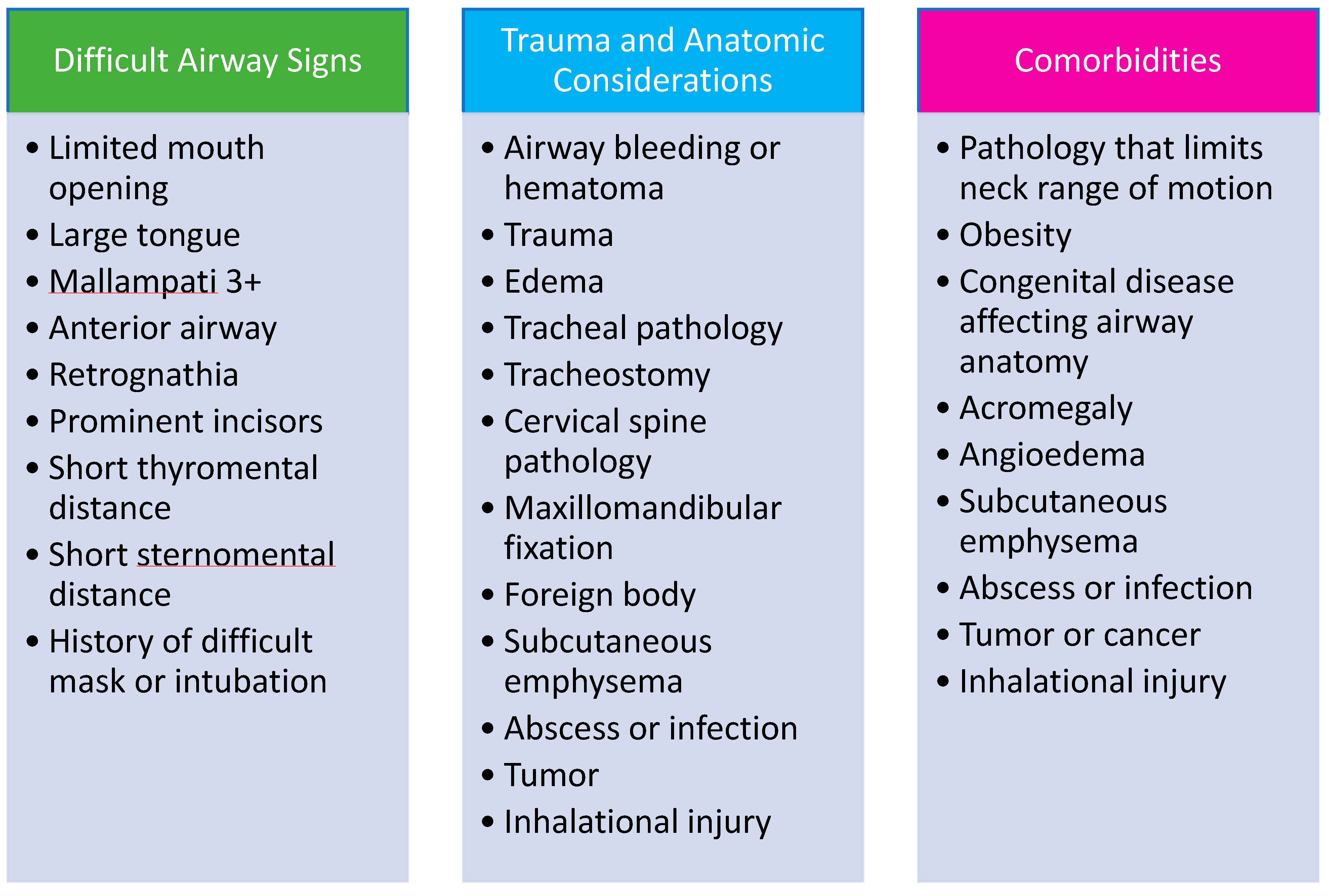
7. Identification of High-Risk Patients
8. Equipment Availability
9. Teamwork
10. Implementation
11. Education
12. Monitoring and Quality Improvement
13. Summary
Author Contributions
Funding
Conflicts of Interest
References
- Russotto, V.; Myatra, S.N.; Laffey, J.G.; Tassistro, E.; Antolini, L.; Bauer, P.; Lascarrou, J.B.; Szułdrzyński, K.; Camporota, L.; Pelosi, P.; et al. Intubation Practices and Adverse Peri-intubation Events in Critically Ill Patients From 29 Countries. JAMA 2021, 325, 1164–1172. [Google Scholar] [CrossRef] [PubMed]
- Cook, T.M.; Woodall, N.; Harper, J.; Benger, J. Major complications of airway management in the UK: Results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 2: Intensive care and emergency departments. Br. J. Anaesth. 2011, 106, 632–642. [Google Scholar] [CrossRef] [Green Version]
- Mark, L.; Lester, L.; Cover, R.; Herzer, K. A decade of difficult airway response team: Lessons learned from a hospital-wide difficult airway response team program. Crit. Care Clin. 2018, 34, 239–251. [Google Scholar] [CrossRef] [PubMed]
- Henderson, S.O.; McClung, C.D.; Sintuu, C.; Swadron, S.P. The Presence of an Emergency Airway Response Team and Its Effects on In-Hospital Code Blue. J. Emerg. Med. 2009, 36, 116–120. [Google Scholar] [CrossRef]
- Berkow, L.C.; Greenberg, R.S.; Kan, K.H.; Colantuoni, E.; Mark, L.J.; Flint, P.W.; Corridore, M.; Bhatti, N.; Heitmiller, E.S. Need for Emergency Surgical Airway Reduced by a Comprehensive Difficult Airway Program. Anesth. Analg. 2009, 109, 1860–1869. [Google Scholar] [CrossRef] [PubMed]
- Walsh, E.C.; Kwo, J.; Chang, M.G.; Pino, R.M.; Bittner, E.A. Rapid Expansion of the Airway Response Team to Meet the Needs of the COVID-19 Pandemic. J. Healthc. Qual. 2021, 43, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Higgs, A.; Cook, T.M.; McGrath, B.A. Airway management in the critically ill: The same, but different. Br. J. Anaesth. 2016, 117, i5–i9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jabaley, C.; Bittner, E.A. Myths and misconceptions regarding emergency airway management 2016. In Current Concepts in Adult Critical Care; Society of Critical Care Medicine: Chicago, IL, USA, 2016. [Google Scholar]
- Cook, T.M.; MacDougall-Davis, S.R. Complications and failure of airway management. Br. J. Anaesth. 2012, 109, i68–i85. [Google Scholar] [CrossRef] [Green Version]
- Hagberg, C.; Georgi, R.; Krier, C. Complications of managing the airway. Best Pract. Res. Clin. Anaesthesiol. 2005, 19, 641–659. [Google Scholar] [CrossRef]
- Heffner, A.C.; Swords, D.; Kline, J.A.; Jones, A.E. The frequency and significance of postintubation hypotension during emergency airway management. J. Crit. Care 2012, 27, 417.e9–417.e13. [Google Scholar] [CrossRef]
- Spaite, D.W.; Hu, C.; Bobrow, B.J.; Chikani, V.; Barnhart, B.; Gaither, J.B.; Denninghoff, K.R.; Adelson, P.D.; Keim, S.M.; Viscusi, C.; et al. The Effect of Combined Out-of-Hospital Hypotension and Hypoxia on Mortality in Major Traumatic Brain Injury. Ann. Emerg. Med. 2017, 69, 62–72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cook, T.M.; Woodall, N.; Frerk, C. A national survey of the impact of NAP4 on airway management practice in United Kingdom hospitals: Closing the safety gap in anaesthesia, intensive care and the emergency department. Br. J. Anaesth. 2016, 117, 182–190. [Google Scholar] [CrossRef] [Green Version]
- Joffe, A.M.; Aziz, M.F.; Posner, K.L.; Duggan, L.V.; Mincer, S.L.; Domino, K.B. Management of difficult tracheal intubation: A closed claims analysis. Anesthesiology 2020, 131, 818–829. [Google Scholar] [CrossRef] [PubMed]
- Asai, T.; Hillman, D. Current difficult airway management—Not good enough! Anesthesiology 2019, 131, 774–776. [Google Scholar] [CrossRef] [PubMed]
- Rassekh, C.H.; Zhao, J.; Martin, N.D.; Chalian, A.A.; Atkins, J.H. Tracheostomy complications as a trigger for an airway rapid response: Analysis and quality improvement considerations. Otolaryngol.-Head Neck Surg. 2015, 153, 921–926. [Google Scholar] [CrossRef] [PubMed]
- Thomas, A.N.; McGrath, B. Patient safety incidents associated with airway devices in critical care: A review of reports to the UK National Patient Safety Agency. Anaesthesia 2009, 64, 358–365. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adams, M.C.; Schmidt, U.; Hess, D.R.; Stelfox, H.T.; Bittner, E.A. Examination of Patterns in Intubation by an Emergency Airway Team at a Large Academic Center: Higher Frequency During Daytime Hours. Respir. Care 2014, 59, 743–748. [Google Scholar] [CrossRef] [Green Version]
- Bittner, E.A.; Schmidt, U. Examining the Learning Practice of Emergency Airway Management Within an Academic Medical Center: Implications for Training and Improving Outcomes. J. Med. Educ. Curric. Dev. 2020, 7, 2382120520965257. [Google Scholar] [CrossRef]
- Andrews, J.D.; Nocon, C.C.; Small, S.M.; Pinto, J.M.; Blair, E.A. Emergency airway management: Training and experience of chief residents in otolaryngology and anesthesiology. Head Neck 2012, 34, 1720–1726. [Google Scholar] [CrossRef]
- Merchant, R.M.; Topjian, A.A.; Panchal, A.R.; Cheng, A.; Aziz, K.; Berg, K.M.; Lavonas, E.J.; Magid, D.J. Part 1: Executive Summary: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S337–S357. [Google Scholar] [CrossRef]
- Rochlen, L.R.; Housey, M.; Gannon, I.; Mitchell, S.; Rooney, D.M.; Tait, A.R.; Engoren, M. Assessing anesthesiology residents’ out-of-the-operating-room (OOOR) emergent airway management. BMC Anesthesiol. 2017, 17, 96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Long, L.; Vanderhoff, B.; Smyke, N.; Shaffer, L.E.T.; Solomon, J.; Steuer, J.D. Management of difficult airways using a hospital-wide “alpha team” approach. Am. J. Med. Qual. 2010, 25, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Damrose, J.F.; Eropkin, W.; Ng, S.; Cale, S.; Banerjee, S. The Critical Response Team in Airway Emergencies. Perm. J. 2019, 23, 18–219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atkins, J.H.; Rassekh, C.H.; Chalian, A.A.; Zhao, J. An Airway Rapid Response System: Implementation and Utilization in a Large Academic Trauma Center. Jt. Comm. J. Qual. Patient Saf. 2017, 43, 653–660. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sterrett, E.C.; Myer IV, C.M.; Oehler, J.; Das, B.; Kerrey, B.T. Critical airway team: A retrospective study of an airway response system in a pediatric hospital. Otolaryngol.-Head Neck Surg. 2017, 157, 1060–1067. [Google Scholar] [CrossRef] [PubMed]
- Atkins, J.H.; Rassekh, C.H. Multidisciplinary airway response teams: Concept, structure, & implementation. Oper. Tech. Otolaryngol. Neck Surg. 2020, 31, 105–110. [Google Scholar] [CrossRef]
- Bittner, E.A.; Sharifpour, M. The Team Approach to Emergency Airway Management: Rationale, Structure, & Implementation. In Airway and Mechanical Ventilation Management; Bittner, E.A., Wilcox, S., Gallagher, J., Eds.; Society of Critical Care Medicine: Chicago, IL, USA, 2021. [Google Scholar]
- Aho, J.M.; Thiels, C.A.; AlJamal, Y.N.; Ruparel, R.K.; Rowse, P.G.; Heller, S.F.; Farley, D.R. Every Surgical Resident Should Know How to Perform a Cricothyrotomy: An Inexpensive Cricothyrotomy Task Trainer for Teaching and Assessing Surgical Trainees. J. Surg. Educ. 2015, 72, 658–661. [Google Scholar] [CrossRef]
- Higgs, A.; McGrath, B.A.; Goddard, C.; Rangasami, J.; Suntharalingam, G.; Gale, R.; Cook, T.M.; Difficult Airway Society; Intensive Care Society; Faculty of Intensive Care Medicine; et al. Guidelines for the management of tracheal intubation in critically ill adults. Br. J. Anaesth. 2018, 120, 323–352. [Google Scholar] [CrossRef] [Green Version]
- Dalesio, N.M.; Lester, L.C.; Barone, B.; Deanehan, J.K.; Fackler, J.C. Real-time emergency airway consultation via telemedicine: Instituting the pediatric airway response team board! Anesth. Analg. 2020, 130, 1097–1102. [Google Scholar] [CrossRef]
- Levin, B.S.; Chang, M.G.; Bittner, E.A. Teleguidance Technology for Endotracheal Intubation: A Scoping Review. Crit. Care Explor. 2021, 3, e0582. [Google Scholar] [CrossRef]
- Feinleib, J.; Foley, L.; Mark, L. What we all should know about our patient’s airway: Difficult airway communications, database registries, and reporting systems registries. Anesthesiol. Clin. 2015, 33, 397–413. [Google Scholar] [CrossRef]
- De Jong, A.; Molinari, N.; Terzi, N.; Mongardon, N.; Arnal, J.M.; Guitton, C.; Allaouchiche, B.; Paugam-Burtz, C.; Constantin, J.M.; Lefrant, J.Y.; et al. Early identification of patients at risk for difficult intubation in the intensive care unit: Development and validation of the MACOCHA score in a multicenter cohort study. Am. J. Respir. Crit. Care Med. 2013, 187, 832–839. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Austin, D.R.; Chang, M.G.; Bittner, E.A. Use of Handheld Point-of-Care Ultrasound in Emergency Airway Management. Chest 2021, 159, 1155–1165. [Google Scholar] [CrossRef] [PubMed]
- Matthews, L.J.; O’Connor, M.; Chaggar, R.S.; Vaughan, D. Airway alert bracelets: Enhancing safety in the COVID-19 era. Anesth. Analg. 2020, 131, e237–e238. [Google Scholar] [CrossRef] [PubMed]
- Shanahan, E.; Huang, J.H.C.; Chen, A.; Narsimhan, A.; Tang, R. Difficultintubationapp.com—A difficult airway electronic record. Can. J. Anaesth. 2016, 63, 1299–1300. [Google Scholar] [CrossRef]
- Difficult Airway Society Extubation Guidelines Group; Popat, M.; Mitchell, V.; Dravid, R.; Patel, A.; Swampillai, C.; Higgs, A. Difficult Airway Society guidelines for the management of tracheal extubation. Anaesthesia 2012, 67, 318–340. [Google Scholar]
- Leeuwenburg, T. Access to difficult airway equipment and training for rural GP-anaesthetists in Australia: Results of a 2012 survey. Rural Remote Health 2012, 12, 2127. [Google Scholar] [CrossRef]
- Gibbins, M.; Kelly, F.E.; Cook, T.M. Airway management equipment and practice: Time to optimise institutional, team, and personal preparedness. Br. J. Anaesth. 2020, 125, 221–224. [Google Scholar] [CrossRef]
- Schyma, B.M.; Wood, A.E.; Sothisrihari, S.; Swinton, P. Optimising remote site airway management kit dump using the SCRAM bag-a randomised controlled trial. Perioper. Med. 2020, 9, 11–16. [Google Scholar] [CrossRef]
- Wilcox, S.R.; Bittner, E.; George, E.; Buckley, V.F.; Schmidt, U.H. Improvement in emergency airway equipment transport. Respir. Care 2010, 55, 852–857. [Google Scholar]
- Gleeson, S.; Groom, P.; Mercer, S. Human factors in complex airway management. BJA Educ. 2016, 16, 191–197. [Google Scholar] [CrossRef] [Green Version]
- Schnittker, R.; Marshall, S.; Horberry, T.; Young, K.L. Human factors enablers and barriers for successful airway management—An in-depth interview study. Anaesthesia 2018, 73, 980–989. [Google Scholar] [CrossRef] [PubMed]
- Fioratou, E.; Flin, R.; Glavin, R. No simple fix for fixation errors: Cognitive processes and their clinical applications. Anaesthesia 2010, 65, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Wijesuriya, J.; Brand, J. Improving the safety of remote site emergency airway management. BMJ Qual. Improv. Rep. 2014, 2, u202785.w1275. [Google Scholar] [CrossRef]
- Harvey, R.; Foulds, L.; Housden, T.; Bennett, K.A.; Falzon, D.; McNarry, A.F.; Graham, C. The impact of didactic read-aloud action cards on the performance of cannula cricothyroidotomy in a simulated ‘can’t intubate can’t oxygenate’ scenario. Anaesthesia 2017, 72, 343–349. [Google Scholar] [CrossRef]
- Jaber, S.; Jung, B.; Corne, P.; Sebbane, M.; Muller, L.; Chanques, G.; Verzilli, D.; Jonquet, O.; Eledjam, J.-J.; Lefrant, J.-Y. An intervention to decrease complications related to endotracheal intubation in the intensive care unit: A prospective, multiple-center study. Intensiv. Care Med. 2010, 36, 248–255. [Google Scholar] [CrossRef]
- Chrimes, N. The Vortex: A universal “high-acuity implementation tool” for emergency airway management. Br. J. Anaesth. 2016, 117, i20–i27. [Google Scholar] [CrossRef] [Green Version]
- Smith, C.; McNarry, A.F. Airway Leads and Airway Response Teams: Improving Delivery of Safer Airway Management? Curr. Anesthesiol. Rep. 2020, 10, 370–377. [Google Scholar] [CrossRef]
- Brazil, V. Translational simulation: Not ‘where?’ but ‘why?’ A functional view of in situ simulation. Adv. Simul. 2017, 2, 20. [Google Scholar] [CrossRef] [Green Version]
- Munzer, B.W.; Bassin, B.S.; Peterson, W.J.; Tucker, R.V.; Doan, J.; Harvey, C.; Sefa, N.; Hsu, C.H. In-situ Simulation Use for Rapid Implementation and Process Improvement of COVID-19 Airway Management. West. J. Emerg. Med. 2020, 21, 99–106. [Google Scholar] [CrossRef]
- Iliff, H.A.; Lawson, T.; Ahmad, I. JanuAIRWAY: Providing airway education through social media. Anaesth. Rep. 2022, 10, e12174. [Google Scholar] [CrossRef]
- Baker, P.A.; Feinleib, J.; O’Sullivan, E.P. Is it time for airway management education to be mandatory? Br. J. Anaesth. 2016, 117, i13–i16. [Google Scholar] [CrossRef] [PubMed]
- Stone, A.B.; Grant, M.C.; Dasani, S.S.; Nascimben, L. The monthly operating cost of an institutional COVID-19 airway response team: A financial model and sensitivity analysis based on experience at an academic medical center. Perioper Care Oper Room Manag. 2021, 23, 100168. [Google Scholar] [CrossRef] [PubMed]
- Marshall, S.D.; Chrimes, N. Time for a breath of fresh air: Rethinking training in airway management. Anaesthesia 2016, 71, 1259–1264. [Google Scholar] [CrossRef]
- Lindkaer Jensen, N.H.; Cook, T.M.; Kelly, F.E. A national survey of practical airway training in UK anaesthetic departments: Time for a national policy? Anaesthesia 2016, 71, 1273–1279. [Google Scholar] [CrossRef] [PubMed]
- Tsai, A.C.; Krisciunas, G.P.; Brook, C.; Basa, K.; Gonzalez, M.; Crimlisk, J.; Grillone, G.A. Comprehensive Emergency Airway Response Team (EART) training and education: Impact on team effectiveness, personnel confidence, and protocol knowledge. Ann. Otol. Rhinol. Laryngol. 2016, 125, 457–463. [Google Scholar] [CrossRef]
- Weaver, S.J.; Dy, S.M.; Rosen, M.A. Team-training in healthcare: A narrative synthesis of the literature. BMJ Qual. Saf. 2014, 23, 359–372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mathieu, J.E.; Heffner, T.S.; Goodwin, G.F.; Salas, E.; Cannon-Bowers, J.A. The influence of shared mental models on team process and performance. J. Appl. Psychol. 2000, 85, 273–283. [Google Scholar] [CrossRef]
- Boet, S.; Borges, B.C.R.; Naik, V.N.; Siu, L.W.; Riem, N.; Chandra, D.; Bould, M.D.; Joo, H.S. Complex procedural skills are retained for a minimum of 1 yr after a single high-fidelity simulation training session. Br. J. Anaesth. 2011, 107, 533–539. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hubert, V.; Duwat, A.; Deransy, R.; Mahjoub, Y.; Dupont, H. Effect of Simulation Training on Compliance with Difficult Airway Management Algorithms, Technical Ability, and Skills Retention for Emergency Cricothyrotomy. Anesthesiology 2014, 120, 999–1008. [Google Scholar] [CrossRef] [Green Version]
- Kennedy, C.C.; Cannon, E.K.; Warner, D.O.; Cook, D.A. Advanced airway management simulation training in medical education: A systematic review and meta-analysis. Crit. Care Med. 2014, 42, 169–178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Groom, P.; Schofield, L.; Hettiarachchi, N.; Pickard, S.; Brown, J.; Sandars, J.; Morton, B. Performance of emergency surgical front of neck airway access by head and neck surgeons, general surgeons, or anaesthetists: An in situ simulation study. Br. J. Anaesth. 2019, 123, 696–703. [Google Scholar] [CrossRef]
- Silverio, S.A.; Wallace, H.; Gauntlett, W.; Berwick, R.; Mercer, S.; Morton, B.; Rogers, S.N.; Sandars, J.E.; Groom, P.; Brown, J.M. Becoming the temporary surgeon: A grounded theory examination of anaesthetists performing emergency front of neck access in inter-disciplinary simulation-based training. PLoS ONE 2021, 16, e0249070. [Google Scholar] [CrossRef] [PubMed]
- Sankaranarayanan, G.; Odlozil, C.A.; Hasan, S.S.; Shabbir, R.; Qi, D.; Turkseven, M.; De, S.; Funk, G.; Weddle, R.J. Training on a virtual reality cricothyroidotomy simulator improves skills and transfers to a simulated procedure. Trauma Surg. Acute Care Open 2022, 7, e000826. [Google Scholar] [CrossRef] [PubMed]
- Komasawa, N.; Berg, B.W. Interprofessional Simulation Training for Perioperative Management Team Development and Patient Safety. J. Perioper. Pract. 2016, 26, 250–253. [Google Scholar] [CrossRef] [PubMed]
- Joyce, M.F.; Berg, S.; Bittner, E.A. Practical strategies for increasing efficiency and effectiveness in critical care education. World J. Crit. Care Med. 2017, 6, 1–12. [Google Scholar] [CrossRef]
- Fent, G.; Blythe, J.; Farooq, O.; Purva, M. In situ simulation as a tool for patient safety: A systematic review identifying how it is used and its effectiveness. BMJ Simul. Technol. Enhanc. Learn. 2015, 1, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Greenland, K.B.; Bradley, W.P.L.; Chapman, G.A.; Goulding, G.; Irwin, M.G. Emergency front-of-neck access: Scalpel or cannula—And the parable of Buridan’s ass. Br. J. Anaesth. 2017, 118, 811–814. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Devore, E.K.; Redmann, A.; Howell, R.; Khosla, S. Best practices for emergency surgical airway: A systematic review. Laryngoscope 2019, 4, 602–608. [Google Scholar] [CrossRef] [PubMed]
- Eisenburger, P.; Laczika, K.; List, M.; Wilfing, A.; Losert, H.; Hofbauer, R.; Burgmann, H.; Bankl, H.; Pikula, B.; Benumof, J.L.; et al. Comparison of Conventional Surgical versus Seldinger Technique Emergency Cricothyrotomy Performed by Inexperienced Clinicians. Anesthesiology 2000, 92, 687–690. [Google Scholar] [CrossRef] [PubMed]
- Heymans, F.; Feigl, G.; Graber, S.; Courvoisier, D.S.; Weber, K.M.; Dulguerov, P. Emergency Cricothyrotomy Performed by Surgical Airway-naive Medical Personnel: A Randomized Crossover Study in Cadavers Comparing Three Commonly Used Techniques. Anesthesiology 2016, 125, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Gordon, J.; Cooper, R.M.; Parotto, M. Supraglottic airway devices: Indications, contraindications and management. Minerva Anestesiol. 2018, 84, 389–397. [Google Scholar] [CrossRef] [PubMed]
- Mort, T.C. Laryngeal Mask Airway and Bougie Intubation Failures: The Combitube as a Secondary Rescue Device for In-Hospital Emergency Airway Management. Anesth. Analg. 2006, 103, 1264–1266. [Google Scholar] [CrossRef]



| Physiologic Complications | Traumatic Complications | Procedure-Related Complications |
|---|---|---|
|
|
|
| Factors | Points |
|---|---|
| Patient-related | |
| 5 |
| 2 |
| 1 |
| 1 |
| Pathology-related | |
| 1 |
| 1 |
| Operator-related | |
| 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tankard, K.A.; Sharifpour, M.; Chang, M.G.; Bittner, E.A. Design and Implementation of Airway Response Teams to Improve the Practice of Emergency Airway Management. J. Clin. Med. 2022, 11, 6336. https://doi.org/10.3390/jcm11216336
Tankard KA, Sharifpour M, Chang MG, Bittner EA. Design and Implementation of Airway Response Teams to Improve the Practice of Emergency Airway Management. Journal of Clinical Medicine. 2022; 11(21):6336. https://doi.org/10.3390/jcm11216336
Chicago/Turabian StyleTankard, Kelly A., Milad Sharifpour, Marvin G. Chang, and Edward A. Bittner. 2022. "Design and Implementation of Airway Response Teams to Improve the Practice of Emergency Airway Management" Journal of Clinical Medicine 11, no. 21: 6336. https://doi.org/10.3390/jcm11216336







