PET Molecular Imaging in Breast Cancer: Current Applications and Future Perspectives
Abstract
1. Introduction
1.1. FDG PET/CT Applications
1.1.1. Initial Diagnosis
1.1.2. Initial Staging
Axillary Lymph Node Staging
Distant Metastasis
1.1.3. Evaluation of Response
1.1.4. Recurrence
1.2. Beyond FDG
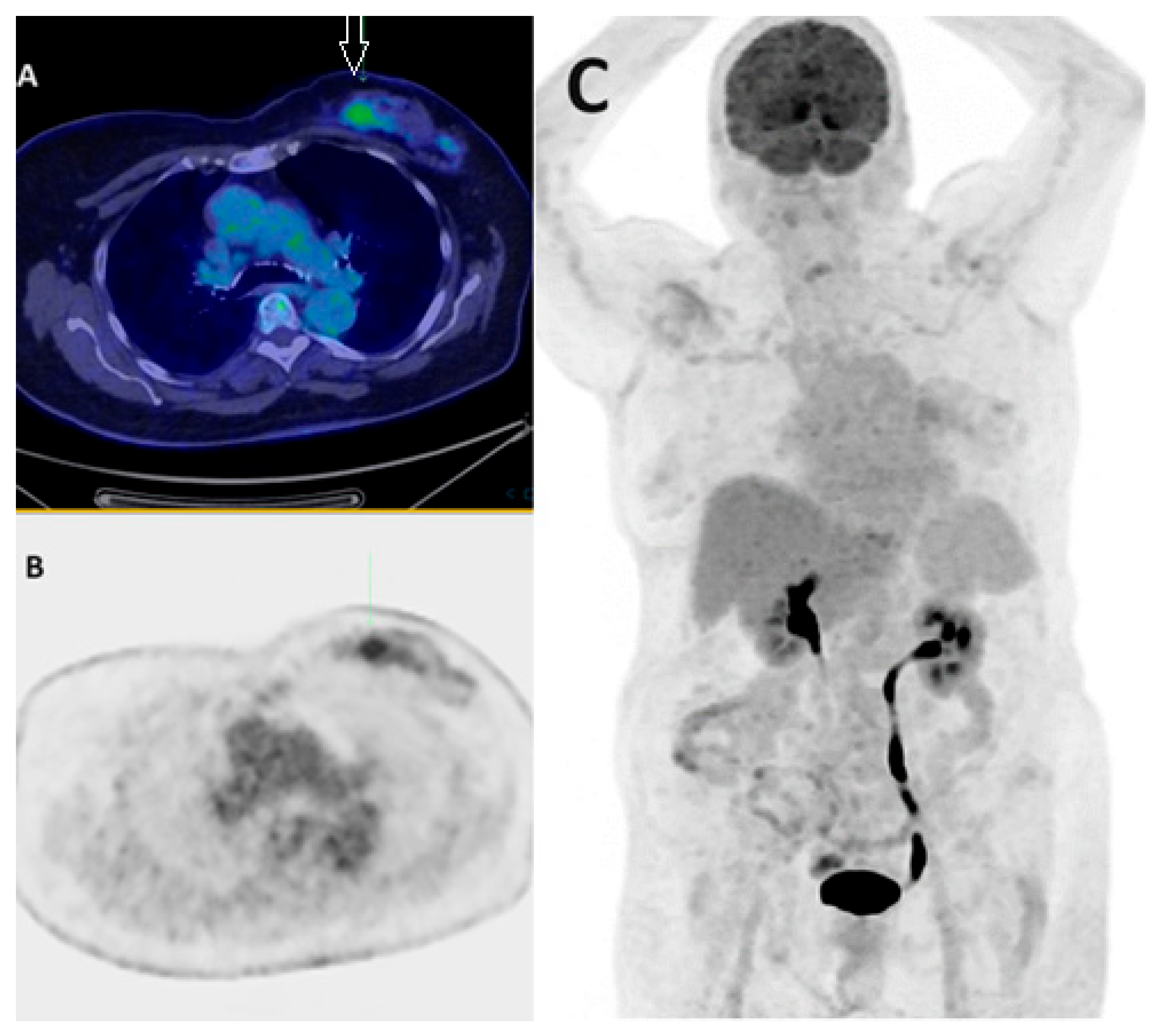
1.2.1. Fibroblast Activation Protein Inhibitor—FAPI
1.2.2. Hormone Receptor Imaging
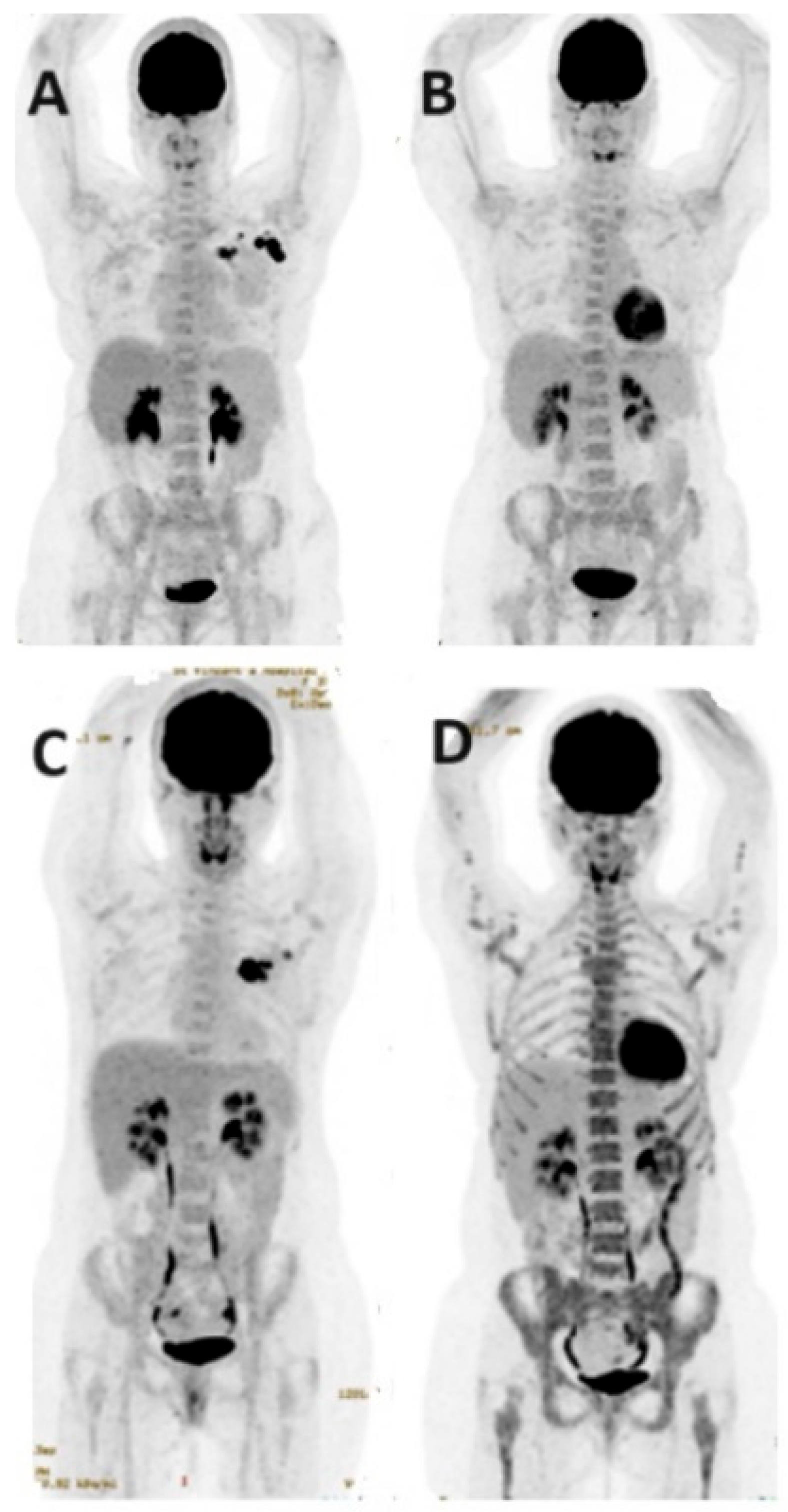
Estrogen Receptor Imaging—FES
Progesterone Receptor Imaging
1.2.3. Human Epidermal Growth Factor Receptor 2 (HER2)
1.2.4. Other Tracers
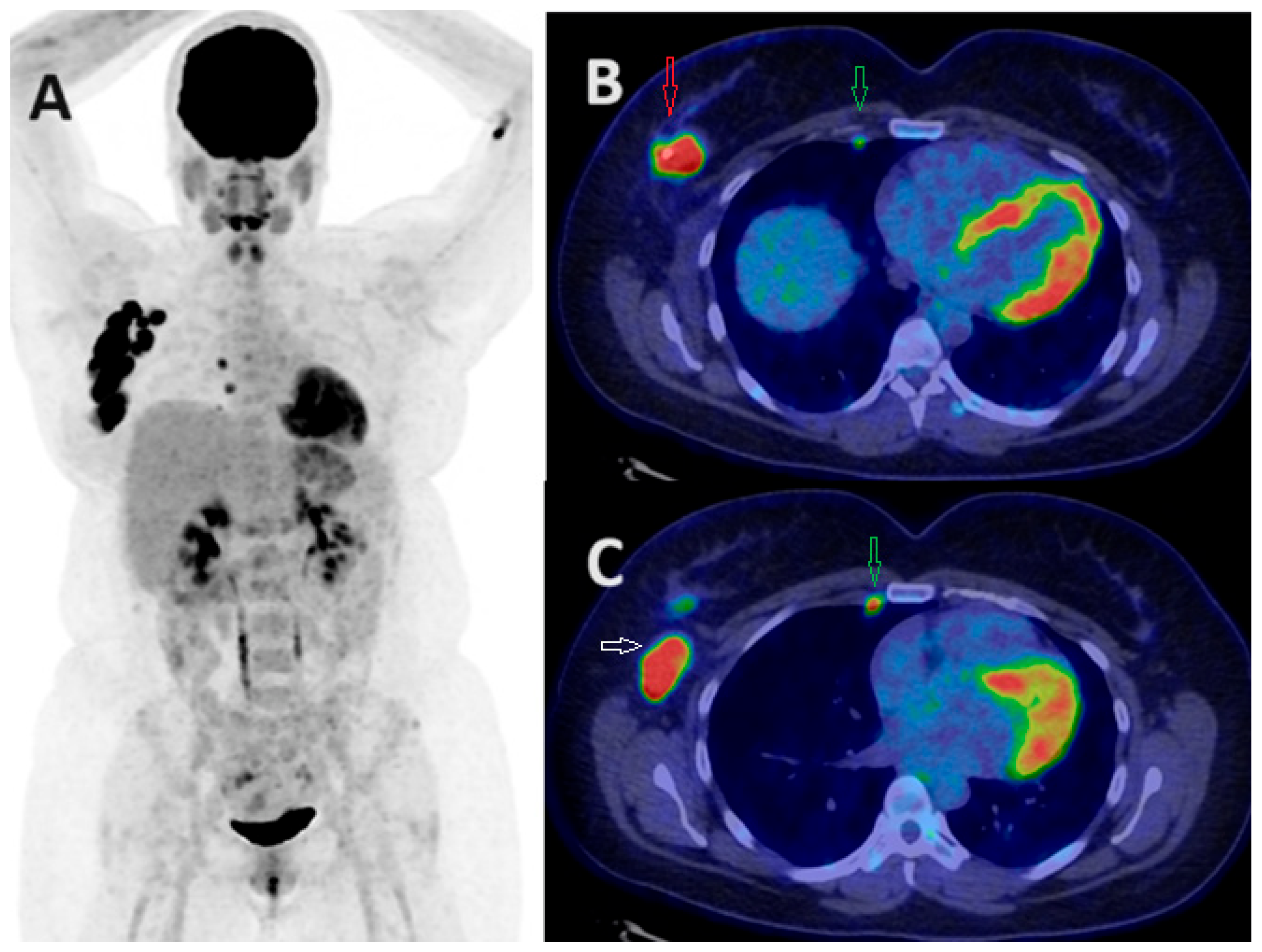
Prostate-Specific Membrane Antigen (PSMA)
Chemokine Receptor 4 (CXCR4)
Somatostatin Receptors (SSTRs)
Androgen Receptor
Others
1.3. PET/MRI Applications
1.4. Recent Advancements: Artificial Intelligence, Machine Learning, and Deep Learning
2. Conclusions
Funding
Conflicts of Interest
Abbreviations
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [PubMed]
- Giaquinto, A.N.; Sung, H.; Miller, K.D.; Kramer, J.L.; Newman, L.A.; Minihan, A.; Jemal, A.; Siegel, R.L. Breast Cancer Statistics, 2022. CA Cancer J. Clin. 2022, 72, 524–541. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.canceraustralia.gov.au/cancer-types/breast-cancer/statistics (accessed on 20 March 2024).
- Taori, K.; Dhakate, S.; Rathod, J.; Hatgaonkar, A.; Disawal, A.; Wavare, P.; Bakare, V.; Puri, R.P. Evaluation of breast masses using mammography and sonography as first line investigations. Open J. Med. Imaging 2013, 3, 40–49. [Google Scholar] [CrossRef]
- Bevers, T.B.; Niell, B.L.; Baker, J.L.; Bennett, D.L.; Bonaccio, E.; Camp, M.S.; Stehman, K. NCCN Guidelines® Insights: Breast Cancer Screening and Diagnosis, Version 1.2023. J. Natl. Compr. Cancer Netw. 2023, 21, 900–909. [Google Scholar] [CrossRef]
- Warning, K.; Hildebrandt, M.G.; Kristensen, B.; Ewertz, M. Utility of 18FDG-PET/CT in breast cancer diagnostics—A systematic review. Dan. Med. Bull. 2011, 58, A4289. [Google Scholar] [PubMed]
- Miyake, K.K.; Nakamoto, Y.; Kanao, S.; Tanaka, S.; Sugie, T.; Mikami, Y.; Toi, M.; Togashi, K. Journal Club: Diagnostic value of 18F-FDG PET/CT and MRI in predicting the clinicopathologic subtypes of invasive breast cancer. Am. J. Roentgenol. 2014, 203, 272–279. [Google Scholar] [CrossRef]
- Yoon, H.J.; Kang, K.W.; Chun, I.K.; Cho, N.; Im, S.A.; Jeong, S.; Moon, W.K. Correlation of breast cancer subtypes, based on estrogen receptor, progesterone receptor, and HER2, with functional imaging parameters from 68Ga-RGD PET/CT and 18F-FDG PET/CT. Eur. J. Nucl. Med. Mol. Imaging 2014, 41, 1534–1543. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, R.; Mammatas, L.H.; Aras, T.; Vogel, W.V.; van de Brug, T.; Oprea-Lager, D.E.; Menke-van der Houven van Oordt, C.W. Diagnostic Performance of [18F]FDG PET in Staging Grade 1-2, Estrogen Receptor Positive Breast Cancer. Diagnostics 2021, 11, 1954. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wu, F.; Han, P. The role of (18)F-FDG PET/CT in the diagnosis of breast cancer and lymph nodes metastases and micrometastases may be limited. Hell. J. Nucl. Med. 2014, 17, 177–183. [Google Scholar] [PubMed]
- de Mooij, C.M.; Ploumen, R.A.W.; Nelemans, P.J.; Mottaghy, F.M.; Smidt, M.L.; van Nijnatten, T.J.A. The influence of receptor expression and clinical subtypes on baseline [18F]FDG uptake in breast cancer: Systematic review and meta-analysis. EJNMMI Res. 2023, 13, 5. [Google Scholar] [CrossRef] [PubMed]
- Soussan, M.; Orlhac, F.; Boubaya, M.; Zelek, L.; Ziol, M.; Eder, V.; Buvat, I. Relationship between tumour heterogeneity measured on FDG-PET/CT and pathological prognostic factors in invasive breast cancer. PLoS ONE 2014, 9, e94017. [Google Scholar] [CrossRef]
- Zhang, J.; Wu, J.; Zhou, X.S.; Shi, F.; Shen, D. Recent advancements in artificial intelligence for breast cancer: Image augmentation, segmentation, diagnosis, and prognosis approaches. Semin. Cancer Biol. 2023, 96, 11–25. [Google Scholar] [CrossRef] [PubMed]
- Berg, W.A.; Madsen, K.S.; Schilling, K.; Tartar, M.; Pisano, E.D.; Larsen, L.H.; Narayanan, D.; Ozonoff, A.; Miller, J.P.; Kalinyak, J.E. Breast cancer: Comparative effectiveness of positron emission mammography and MR imaging in presurgical planning for the ipsilateral breast. Radiology 2011, 258, 59–72. [Google Scholar] [CrossRef] [PubMed]
- Krammer, J.; Schnitzer, A.; Kaiser, C.G.; Buesing, K.A.; Sperk, E.; Brade, J.; Wasser, K. (18)F-FDG PET/CT for initial staging in breast cancer patients–Is there a relevant impact on treatment planning compared to conventional staging modalities? Eur. Radiol. 2015, 25, 2460–2469. [Google Scholar] [CrossRef] [PubMed]
- Groves, A.M.; Shastry, M.; Ben-Haim, S.; Kayani, I.; Malhotra, A.; Davidson, T.; Kelleher, T.; Whittaker, D.; Meagher, M.; Holloway, B.; et al. Defining the role of PET-CT in staging early breast cancer. Oncologist 2012, 17, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Gradishar, W.J.; Moran, M.S.; Abraham, J.; Aft, R.; Agnese, D.; Allison, K.H.; Anderson, B.; Burstein, H.J.; Chew, H.; Dang, C.; et al. Breast cancer, version 3.2022, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. 2022, 20, 691–722. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Choi, J.Y. Impact of 18F-FDG PET, PET/CT, and PET/MRI on Staging and Management as an Initial Staging Modality in Breast Cancer: A Systematic Review and Meta-analysis. Clin. Nucl. Med. 2021, 46, 271–282. [Google Scholar] [CrossRef] [PubMed]
- Hadebe, B.; Harry, L.; Ebrahim, T.; Pillay, V.; Vorster, M. The Role of PET/CT in Breast Cancer. Diagnostics 2023, 13, 597. [Google Scholar] [CrossRef] [PubMed]
- Kasem, J.; Wazir, U.; Mokbel, K. Sensitivity, Specificity and the Diagnostic Accuracy of PET/CT for Axillary Staging in Patients with Stage I-III Cancer: A Systematic Review of The Literature. In Vivo 2021, 35, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Peare, R.; Staff, R.T.; Heys, S.D. The use of FDG-PET in assessing axillary lymph node status in breast cancer: A systematic review and meta-analysis of the literature. Breast Cancer Res. Treat. 2010, 123, 281–290. [Google Scholar] [CrossRef]
- Vercher-Conejero, J.L.; Pelegrí-Martinez, L.; Lopez-Aznar, D.; Cózar-Santiago Mdel, P. Positron Emission Tomography in Breast Cancer. Diagnostics 2015, 5, 61–83. [Google Scholar] [CrossRef]
- Seo, M.J.; Lee, J.J.; Kim, H.O.; Chae, S.Y.; Park, S.H.; Ryu, J.S.; Ahn, S.H.; Lee, J.W.; Son, B.H.; Gong, G.Y.; et al. Detection of internal mammary lymph node metastasis with (18)F-fluorodeoxyglucose positron emission tomography/computed tomography in patients with stage III breast cancer. Eur. J. Nucl. Med. Mol. Imaging 2014, 41, 438–445. [Google Scholar] [CrossRef] [PubMed]
- An, Y.Y.; Kim, S.H.; Kang, B.J.; Lee, A.W. Comparisons of Positron Emission Tomography/Computed Tomography and Ultrasound Imaging for Detection of Internal Mammary Lymph Node Metastases in Patients with Breast Cancer and Pathologic Correlation by Ultrasound-Guided Biopsy Procedures. J. Ultrasound Med. 2015, 34, 1385–1394. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.L.; Eissa, M.J.; Rogers, J.V.; Aravkin, A.Y.; Porter, B.A.; Beatty, J.D. (18)F-FDG PET/CT-positive internal mammary lymph nodes: Pathologic correlation by ultrasound-guided fine-needle aspiration and assessment of associated risk factors. AJR Am. J. Roentgenol. 2013, 200, 1138–1144. [Google Scholar] [CrossRef] [PubMed]
- Garcia, J.R.; Kauak, M.; Compte, A.; Bassa, P.; Llinares, E.; Valls, E.; Riera, E. Detection of internal mammary chain infiltration in breast cancer patients by [18F] FDG PET/MRI. Therapy implications. Rev. Esp. Med. Nucl. Imagen Mol. 2023, 43, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Shiner, A.; Kiss, A.; Saednia, K.; Jerzak, K.J.; Gandhi, S.; Lu, F.I.; Emmenegger, U.; Fleshner, L.; Lagree, A.; Alera, M.A.; et al. Predicting Patterns of Distant Metastasis in Breast Cancer Patients following Local Regional Therapy Using Machine Learning. Genes 2023, 14, 1768. [Google Scholar] [CrossRef] [PubMed]
- Pires, A.O.; Borges, U.S.; Lopes-Costa, P.V.; Gebrim, L.H.; da Silva, B.B. Evaluation of bone metastases from breast cancer by bone scintigraphy and positron emission tomography/computed tomography imaging. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 180, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Vogsen, M.; Jensen, J.D.; Christensen, I.Y.; Gerke, O.; Jylling, A.M.B.; Larsen, L.B.; Braad, P.-E.; Søe, K.L.; Bille, C.; Ewertz, M.; et al. FDG-PET/CT in high-risk primary breast cancer—A prospective study of stage migration and clinical impact. Breast Cancer Res. Treat. 2021, 185, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Xu, G.Z.; Li, C.Y.; Zhao, L.; He, Z.Y. Comparison of FDG whole-body PET/CT and gadolinium-enhanced whole-body MRI for distant malignancies in patients with malignant tumours: A meta-analysis. Ann. Oncol. 2013, 24, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.; Li, J.; Wang, S. 18FDG PET-CT for diagnosis of distant metastases in breast cancer patients. A meta-analysis. Surg. Oncol. 2013, 22, 139–143. [Google Scholar] [CrossRef]
- Sen, F.; Akpinar, A.T.; Ogur, U.; Duman, G.; Tamgac, F.; Alper, E. The impact of PET/CT imaging performed in the early postoperative period on the management of breast cancer patients. Nucl. Med. Commun. 2013, 34, 571–576. [Google Scholar] [CrossRef] [PubMed]
- Riedl, C.C.; Slobod, E.; Jochelson, M.; Morrow, M.; Goldman, D.A.; Gonen, M.; Weber, W.A.; Ulaner, G.A. Retrospective analysis of 18F-FDG PET/CT for staging asymptomatic breast cancer patients younger than 40 years. J. Nucl. Med. 2014, 55, 1578–1583. [Google Scholar] [CrossRef] [PubMed]
- Yararbas, U.; Avci, N.C.; Yeniay, L.; Argon, A.M. The value of 18F-FDG PET/CT imaging in breast cancer staging. Bosn. J. Basic Med. Sci. 2018, 18, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.T. Breast carcinoma: Pattern of metastasis at autopsy. J. Surg. Oncol. 1983, 23, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Yi, Y.L.; Liu, Y.; Xiong, J.P.; He, C.Z. Comparison of whole-body PET/PET-CT and conventional imaging procedures for distant metastasis staging in patients with breast cancer: A meta-analysis. Eur. J. Gynaecol. Oncol. 2015, 36, 672–676. [Google Scholar]
- Rong, J.; Wang, S.; Ding, Q.; Yun, M.; Zheng, Z.; Ye, S. Comparison of 18 FDG PET-CT and bone scintigraphy for detection of bone metastases in breast cancer patients. A meta-analysis. Surg. Oncol. 2013, 22, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Kitajima, K.; Miyoshi, Y. Present and future role of FDG-PET/CT imaging in the management of breast cancer. Jpn. J. Radiol. 2016, 34, 167–180. [Google Scholar] [CrossRef] [PubMed]
- Asaoka, M.; Gandhi, S.; Ishikawa, T.; Takabe, K. Neoadjuvant Chemotherapy for Breast Cancer: Past, Present, and Future. Breast Cancer 2020, 14, 1178223420980377. [Google Scholar] [CrossRef] [PubMed]
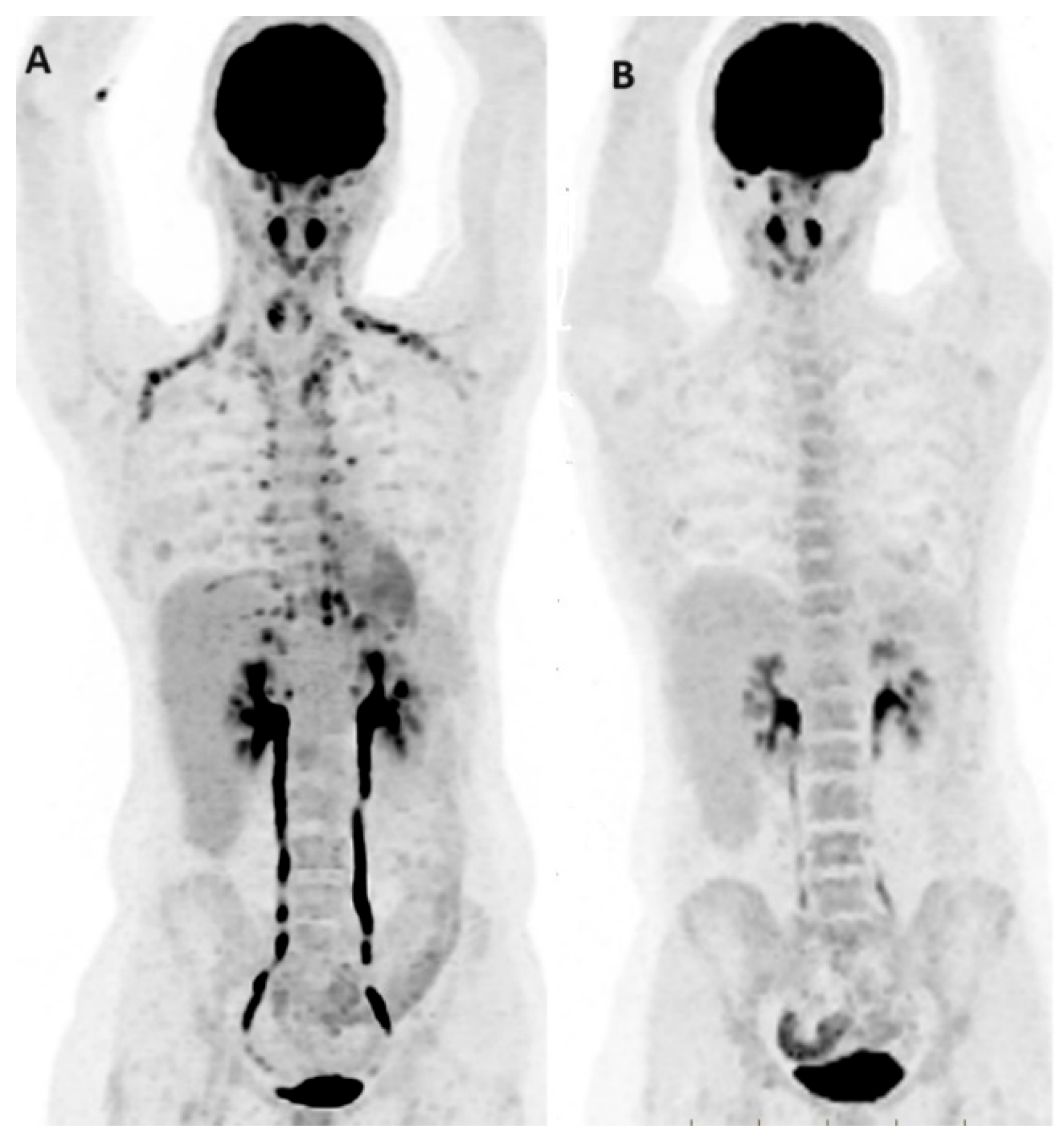
- Groheux, D.; Giacchetti, S.; Delord, M.; de Roquancourt, A.; Merlet, P.; Hamy, A.S.; Espié, M.; Hindié, E. Prognostic impact of 18F-FDG PET/CT staging and of pathological response to neoadjuvant chemotherapy in triple-negative breast cancer. Eur. J. Nucl. Med. Mol. Imaging 2015, 42, 377–385. [Google Scholar] [CrossRef] [PubMed]
- García Vicente, A.M.; Cruz Mora, M.Á.; León Martín, A.A.; Muñoz Sánchez, M.D.M.; Relea Calatayud, F.; Van Gómez López, O.; Soriano Castrejón, Á. Glycolytic activity with 18F-FDG PET/CT predicts final neoadjuvant chemotherapy response in breast cancer. Tumour Biol. 2014, 35, 11613–11620. [Google Scholar] [CrossRef] [PubMed]
- Zucchini, G.; Quercia, S.; Zamagni, C.; Santini, D.; Taffurelli, M.; Fanti, S.; Martoni, A.A. Potential utility of early metabolic response by 18F-2-fluoro-2-deoxy-D-glucose-positron emission tomography/computed tomography in a selected group of breast cancer patients receiving preoperative chemotherapy. Eur. J. Cancer 2013, 49, 1539–1545. [Google Scholar] [CrossRef]
- Mghanga, F.P.; Lan, X.; Bakari, K.H.; Li, C.; Zhang, Y. Fluorine-18 fluorodeoxyglucose positron emission tomography-computed tomography in monitoring the response of breast cancer to neoadjuvant chemotherapy: A meta-analysis. Clin. Breast Cancer 2013, 13, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Martoni, A.A.; Zamagni, C.; Quercia, S.; Rosati, M.; Cacciari, N.; Bernardi, A.; Musto, A.; Fanti, S.; Santini, D.; Taffurelli, M. Early (18)F-2-fluoro-2-deoxy-d-glucose positron emission tomography may identify a subset of patients with estrogen receptor-positive breast cancer who will not respond optimally to preoperative chemotherapy. Cancer 2010, 116, 805–813. [Google Scholar] [CrossRef] [PubMed]
- Tian, F.; Shen, G.; Deng, Y.; Diao, W.; Jia, Z. The accuracy of 18F-FDG PET/CT in predicting the pathological response to neoadjuvant chemotherapy in patients with breast cancer: A meta-analysis and systematic review. Eur. Radiol. 2017, 27, 4786–4796. [Google Scholar] [CrossRef] [PubMed]
- An, Y.Y.; Kim, S.H.; Kang, B.J.; Lee, A.W. Treatment Response Evaluation of Breast Cancer after Neoadjuvant Chemotherapy and Usefulness of the Imaging Parameters of MRI and PET/CT. J. Korean Med. Sci. 2015, 30, 808–815. [Google Scholar] [CrossRef] [PubMed]
- Hildebrandt, M.G.; Naghavi-Behzad, M.; Vogsen, M. A role of FDG-PET/CT for response evaluation in metastatic breast cancer? Semin. Nucl. Med. 2022, 52, 520–530. [Google Scholar] [CrossRef] [PubMed]
- Suto, H.; Inui, Y.; Okamura, A. Is CT or FDG-PET more useful for evaluation of the treatment response in metastatic HER2-positive breast cancer? A case report and literature review. Front. Oncol. 2023, 13, 1158797. [Google Scholar] [CrossRef] [PubMed]
- Djassemi, N.; Rampey, S.; Motiani, J. Examining the evolving utility of 18FDG-PET/CT in breast cancer recurrence. Transl. Cancer Res. 2020, 9 (Suppl. S1), S116–S121. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, G.P.; Baur-Melnyk, A.; Haug, A.; Heinemann, V.; Bauerfeind, I.; Reiser, M.F.; Schoenberg, S.O. Comprehensive imaging of tumour recurrence in breast cancer patients using whole-body MRI at 1.5 and 3 T compared to FDG-PET-CT. Eur. J. Radiol. 2008, 65, 47–58. [Google Scholar] [CrossRef] [PubMed]
- Groheux, D. FDG-PET/CT for Primary Staging and Detection of Recurrence of Breast Cancer. Semin. Nucl. Med. 2022, 52, 508–519. [Google Scholar] [CrossRef]
- Ulaner, G.A. PET/CT for Patients with Breast Cancer: Where Is the Clinical Impact? AJR Am. J. Roentgenol. 2019, 213, 254–265. [Google Scholar] [CrossRef] [PubMed]
- Cochet, A.; David, S.; Moodie, K.; Drummond, E.; Dutu, G.; MacManus, M.; Hicks, R.J. The utility of 18 F-FDG-PET/CT for suspected recurrent breast cancer: Impact and prognostic stratification. Cancer Imaging 2014, 14, 1. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.T.; Hu, C.; Chiu, Y.L.; Peng, N.J.; Liu, R.S. Role of 2-[18F] fluoro-2-deoxy-D-glucose-positron emission tomography/computed tomography in the post-therapy surveillance of breast cancer. PLoS ONE 2014, 9, e115127. [Google Scholar] [CrossRef] [PubMed]
- Pan, L.; Han, Y.; Sun, X.; Liu, J.; Gang, H. FDG-PET and other imaging modalities for the evaluation of breast cancer recurrence and metastases: A meta-analysis. J. Cancer Res. Clin. Oncol. 2010, 136, 1007–1022. [Google Scholar] [CrossRef] [PubMed]
- Pennant, M.; Takwoingi, Y.; Pennant, L.; Davenport, C.; Fry-Smith, A.; Eisinga, A.; Hyde, C. A systematic review of positron emission tomography (PET) and positron emission tomography/computed tomography (PET/CT) for the diagnosis of breast cancer recurrence. Health Technol. Assess. 2010, 14, 1–103. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; Wang, L.; Jiang, X.; She, W.; He, L.; Hu, G. Diagnostic efficacy of 18F-FDG-PET or PET/CT in breast cancer with suspected recurrence: A systematic review and meta-analysis. Nucl. Med. Commun. 2016, 37, 1180–1188. [Google Scholar] [CrossRef] [PubMed]
- Grassetto, G.; Fornasiero, A.; Otello, D.; Bonciarelli, G.; Rossi, E.; Nashimben, O.; Minicozzi, A.M.; Crepaldi, G.; Pasini, F.; Facci, E.; et al. 18F-FDG-PET/CT in patients with breast cancer and rising Ca 15-3 with negative conventional imaging: A multicentre study. Eur. J. Radiol. 2011, 80, 828–833. [Google Scholar] [CrossRef] [PubMed]
- Evangelista, L.; Cervino, A.R.; Ghiotto, C.; Al-Nahhas, A.; Rubello, D.; Muzzio, P.C. Tumour marker-guided PET in breast cancer patients-a recipe for a perfect wedding: A systematic literature review and meta-analysis. Clin. Nucl. Med. 2012, 37, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Aukema, T.S.; Rutgers, E.J.; Vogel, W.V.; Teertstra, H.J.; Oldenburg, H.S.; Peeters, M.V.; Olmos, R.V. The role of FDG PET/CT in patients with locoregional breast cancer recurrence: A comparison to conventional imaging techniques. Eur. J. Surg. Oncol. 2010, 36, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Choi, J.Y.; Park, Y.H.; Lee, J.E.; Kim, S.W.; Nam, S.J.; Cho, Y.S. Diagnostic Value of FDG PET/CT in Surveillance after Curative Resection of Breast Cancer. Cancers 2023, 15, 2646. [Google Scholar] [CrossRef] [PubMed]
- Manohar, K.; Mittal, B.R.; Senthil, R.; Kashyap, R.; Bhattacharya, A.; Singh, G. Clinical utility of F-18 FDG PET/CT in recurrent breast carcinoma. Nucl. Med. Commun. 2012, 33, 591–596. [Google Scholar] [CrossRef] [PubMed]
- Kratochwil, C.; Flechsig, P.; Lindner, T.; Abderrahim, L.; Altmann, A.; Mier, W.; Adeberg, S.; Rathke, H.; Röhrich, M.; Winter, H.; et al. 68Ga-FAPI PET/CT: Tracer Uptake in 28 Different Kinds of Cancer. J. Nucl. Med. 2019, 60, 801–805. [Google Scholar] [CrossRef] [PubMed]
- Kömek, H.; Can, C.; Güzel, Y.; Oruç, Z.; Gündoğan, C.; Yildirim, Ö.A.; Kaplan, I.; Erdur, E.; Yıldırım, M.S.; Çakabay, B. 68Ga-FAPI-04 PET/CT, a new step in breast cancer imaging: A comparative pilot study with the 18F-FDG PET/CT. Ann. Nucl. Med. 2021, 35, 744–752. [Google Scholar] [CrossRef] [PubMed]
- Lindner, T.; Loktev, A.; Altmann, A.; Giesel, F.; Kratochwil, C.; Debus, J.; Jäger, D.; Mier, W.; Haberkorn, U. Development of Quinoline-Based Theranostic Ligands for the Targeting of Fibroblast Activation Protein. J. Nucl. Med. 2018, 59, 1415–1422. [Google Scholar] [CrossRef] [PubMed]
- Elboga, U.; Sahin, E.; Kus, T.; Cayirli, Y.B.; Aktas, G.; Uzun, E.; Cinkir, H.Y.; Teker, F.; Sever, O.N.; Aytekin, A.; et al. Superiority of 68Ga-FAPI PET/CT scan in detecting additional lesions compared to 18FDG PET/CT scan in breast cancer. Ann. Nucl. Med. 2021, 35, 1321–1331. [Google Scholar] [CrossRef] [PubMed]
- Evangelista, L.; Filippi, L.; Schillaci, O. What radiolabeled FAPI pet can add in breast cancer? A systematic review from literature. Ann. Nucl. Med. 2023, 37, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Baumgarten, S.C.; Frasor, J. Minireview: Inflammation: An instigator of more aggressive estrogen receptor (ER) positive breast cancers. Mol. Endocrinol. 2012, 26, 360–371. [Google Scholar] [CrossRef] [PubMed]
- Lebron, L.; Greenspan, D.; Pandit-Taskar, N. PET Imaging of Breast Cancer: Role in Patient Management. PET Clin. 2015, 10, 159–195. [Google Scholar] [CrossRef] [PubMed]
- Dehdashti, F.; Wu, N.; Ma, C.X.; Naughton, M.J.; Katzenellenbogen, J.A.; Siegel, B.A. Association of PET-based estradiol-challenge test for breast cancer progesterone receptors with response to endocrine therapy. Nat. Commun. 2021, 12, 733. [Google Scholar] [CrossRef] [PubMed]
- Mammatas, L.H.; Venema, C.M.; Schröder, C.P.; de Vet, H.C.W.; van Kruchten, M.; Glaudemans, A.W.J.M.; Yaqub, M.M.; Verheul, H.M.W.; Boven, E.; van der Vegt, B.; et al. Visual and quantitative evaluation of [18F] FES and [18F] FDHT PET in patients with metastatic breast cancer: An interobserver variability study. EJNMMI Res. 2020, 10, 40. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, N.; Iqbal, N. Human Epidermal Growth Factor Receptor 2 (HER2) in Cancers: Overexpression and Therapeutic Implications. Mol. Biol. Int. 2014, 2014, 852748. [Google Scholar] [CrossRef] [PubMed]
- Reis-Filho, J.S.; Pusztai, L. Gene expression profiling in breast cancer: Classification, prognostication, and prediction. Lancet 2011, 378, 1812–1823. [Google Scholar] [CrossRef] [PubMed]
- Lamon, D.J.; Clark, G.M.; Wong, S.G.; Levin, W.J.; Ullrich, A.; McGuire, W.L. Human breast cancer: Correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 1987, 235, 177–182. [Google Scholar]
- Nahta, R.; Yu, D.; Hung, M.C.; Hortobagyi, G.N.; Esteva, F.J. Mechanisms of disease: Understanding resistance to HER2-targeted therapy in human breast cancer. Nat. Clin. Pract. Oncol. 2006, 3, 269–280. [Google Scholar] [CrossRef] [PubMed]
- Laforest, R.; Lapi, S.E.; Oyama, R.; Bose, R.; Tabchy, A.; Marquez-Nostra, B.V.; Burkemper, J.; Wright, B.D.; Frye, J.; Frye, S.; et al. [89Zr] Trastuzumab: Evaluation of Radiation Dosimetry, Safety, and Optimal Imaging Parameters in Women with HER2-Positive Breast Cancer. Mol. Imaging Biol. 2016, 18, 952–959. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Aboian, M.S.; Zhu, X.; Marquez-Nostra, B. Clinical Evaluation of Nuclear Imaging Agents in Breast Cancer. Cancers 2022, 14, 2103. [Google Scholar] [CrossRef] [PubMed]
- Sathekge, M.; Lengana, T.; Modiselle, M.; Vorster, M.; Zeevaart, J.; Maes, A.; Ebenhan, T.; Van de Wiele, C. 68Ga-PSMA-HBED-CC PET imaging in breast carcinoma patients. Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 689–694. [Google Scholar] [CrossRef] [PubMed]
- Lapidot, T.; Dar, A.; Kollet, O. How do stem cells find their way home? Blood 2005, 106, 1901–1910. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Suh, M.; Choi, H.; Ha, S.; Paeng, J.C.; Cheon, G.J.; Lee, D.S. A pan-cancer analysis of the clinical and genetic portraits of somatostatin receptor expressing tumour as a potential target of peptide receptor imaging and therapy. EJNMMI Res. 2020, 10, 42. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.; Fullard, K.; Sheehan-Dare, G.; Tang, R.; Chan, L.; Ho, B.; Emmett, L. Diagnostic value of 68Ga-DOTATATE PET-CT imaging for staging of ER+/PR+ HER2- breast cancer patients with metastatic disease: Comparison with conventional imaging with bone scan, diagnostic CT and 18 F-FDG PET-CT in a prospective pilot trial. J. Med. Imaging Radiat. Oncol. 2022, 66, 731–737. [Google Scholar] [CrossRef] [PubMed]
- Overmoyer, B.; Rugo, H.S.; Johnston, S.; O’Shaughnessy, J.A.; Palmieri, C.; Schwartzberg, L.S.; Johnston, M.A. First stage of an on-going phase 2, open label, international, randomized, parallel design study investigating efficacy+ safety of GTx-024 for advanced ER+/AR+ breast cancer (BC). Ann. Oncol. 2017, 28, i7–i8. [Google Scholar] [CrossRef]
- Venema, C.M.; Mammatas, L.H.; Schröder, C.P.; Van Kruchten, M.; Apollonio, G.; Glaudemans, A.W.J.M.; Bongaerts, A.H.; Hoekstra, O.S.; Verheul, H.M.; Boven, E.; et al. Androgen and Estrogen Receptor Imaging in Metastatic Breast Cancer Patients as a Surrogate for Tissue Biopsies. J. Nucl. Med. 2017, 58, 1906–1912. [Google Scholar] [CrossRef] [PubMed]
- Jacene, H.; Liu, M.; Cheng, S.C.; Abbott, A.; Dubey, S.; McCall, K.; Young, D.; Johnston, M.; Abbeele, A.D.V.D.; Overmoyer, B. Imaging Androgen Receptors in Breast Cancer with 18F-Fluoro-5α-Dihydrotestosterone PET: A Pilot Study. J. Nucl. Med. 2022, 63, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Linden, H.M.; Dehdashti, F. Novel methods and tracers for breast cancer imaging. Semin. Nucl. Med. 2013, 43, 324–329. [Google Scholar] [CrossRef] [PubMed]
- Ulaner, G.A.; Goldman, D.A.; Gönen, M.; Pham, H.; Castillo, R.; Lyashchenko, S.K.; Lewis, J.S.; Dang, C. Initial Results of a Prospective Clinical Trial of 18F-Fluciclovine PET/CT in Newly Diagnosed Invasive Ductal and Invasive Lobular Breast Cancers. J. Nucl. Med. 2016, 57, 1350–1356. [Google Scholar] [CrossRef] [PubMed]
- Sabeghi, P.; Katal, S.; Chen, M.; Taravat, F.; Werner, T.J.; Saboury, B.; Alavi, A. Update on Positron Emission Tomography/Magnetic Resonance Imaging: Cancer and Inflammation Imaging in the Clinic. Magn. Reson. Imaging Clin. 2023, 31, 517–538. [Google Scholar] [CrossRef] [PubMed]
- Ruan, D.; Sun, L. Diagnostic Performance of PET/MRI in Breast Cancer: A Systematic Review and Bayesian Bivariate Meta-analysis. Clin. Breast Cancer 2023, 23, 108–124. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.R.; Qu, M.M.; Zhai, Y.N.; Feng, W.; Gao, Y.; Lei, J.-Q. Diagnostic role of 18F-FDG PET/MRI in the TNM staging of breast cancer: A systematic review and meta-analysis. Ann. Palliat. Med. 2021, 10, 4328–4337. [Google Scholar] [CrossRef] [PubMed]
- Pinker, K.; Bogner, W.; Baltzer, P.; Karanikas, G.; Magometschnigg, H.; Brader, P.; Helbich, T.H. Improved differentiation of benign and malignant breast tumours with multiparametric 18fluorodeoxyglucose positron emission tomography magnetic resonance imaging: A feasibility study. Clin. Cancer Res. 2014, 20, 3540–3549. [Google Scholar] [CrossRef] [PubMed]
- Sawicki, L.M.; Grueneisen, J.; Schaarschmidt, B.M.; Buchbender, C.; Nagarajah, J.; Umutlu, L.; Antoch, G.; Kinner, S. Evaluation of ¹⁸F-FDG PET/MRI, ¹⁸F-FDG PET/CT, MRI, and CT in whole-body staging of recurrent breast cancer. Eur. J. Radiol. 2016, 85, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Morawitz, J.; Kirchner, J.; Martin, O.; Bruckmann, N.-M.; Dietzel, F.; Li, Y.; Rischpler, C.; Herrmann, K.; Umutlu, L.; Bittner, A.-K.; et al. Prospective Correlation of Prognostic Immunohistochemical Markers with SUV and ADC Derived from Dedicated Hybrid Breast 18F-FDG PET/MRI in Women with Newly Diagnosed Breast Cancer. Clin. Nucl. Med. 2021, 46, 201–205. [Google Scholar] [CrossRef] [PubMed]
- Incoronato, M.; Grimaldi, A.M.; Mirabelli, P.; Cavaliere, C.; Parente, C.A.; Franzese, M.; Staibano, S.; Ilardi, G.; Russo, D.; Soricelli, A.; et al. Circulating miRNAs in untreated breast cancer: An exploratory multimodality morpho-functional study. Cancers 2019, 11, 876. [Google Scholar] [CrossRef] [PubMed]
- Melsaether, A.N.; Raad, R.A.; Pujara, A.C.; Ponzo, F.D.; Pysarenko, K.M.; Jhaveri, K.; Babb, J.S.; Sigmund, E.E.; Kim, S.G.; Moy, L.A. Comparison of Whole-Body (18)F FDG PET/MR Imaging and Whole-Body (18)F FDG PET/CT in Terms of Lesion Detection and Radiation Dose in Patients with Breast Cancer. Radiology 2016, 281, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Taneja, S.; Jena, A.; Goel, R.; Sarin, R.; Kaul, S. Simultaneous whole-body 18F-FDG PET-MRI in primary staging of breast cancer: A pilot study. Eur. J. Radiol. 2014, 83, 2231–2239. [Google Scholar] [CrossRef] [PubMed]
- Najjar, R. Redefining Radiology: A Review of Artificial Intelligence Integration in Medical Imaging. Diagnostics 2023, 13, 2760. [Google Scholar] [CrossRef]
- Hosny, A.; Parmar, C.; Quackenbush, J.; Schwartz, L.H.; Aerts, H.J.W.L. Artificial intelligence in radiology. Nat. Rev. Cancer 2018, 18, 500–510. [Google Scholar] [CrossRef] [PubMed]
- Morawitz, J.; Sigl, B.; Rubbert, C.; Bruckmann, N.-M.; Dietzel, F.; Häberle, L.J.; Ting, S.; Mohrmann, S.; Ruckhäberle, E.; Bittner, A.-K.; et al. Clinical Decision Support for Axillary Lymph Node Staging in Newly Diagnosed Breast Cancer Patients Based on 18F-FDG PET/MRI and Machine Learning. J. Nucl. Med. 2023, 64, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Wang, X.; Xu, C.; Liu, C.; Zheng, C.; Fulham, M.J.; Feng, D.; Wang, L.; Song, S.; Huang, G. 18F-FDG PET/CT radiomic predictors of pathologic complete response (pCR) to neoadjuvant chemotherapy in breast cancer patients. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 1116–1126. [Google Scholar] [CrossRef] [PubMed]
- Bi, W.L.; Hosny, A.; Schabath, M.B.; Giger, M.L.; Birkbak, N.J.; Mehrtash, A.; Allison, T.; Arnaout, O.; Abbosh, C.; Dunn, I.F.; et al. Artificial intelligence in cancer imaging: Clinical challenges and applications. CA Cancer J. Clin. 2019, 69, 127–157. [Google Scholar] [CrossRef] [PubMed]
- Romeo, V.; Clauser, P.; Rasul, S.; Kapetas, P.; Gibbs, P.; Baltzer, P.A.T.; Hacker, M.; Woitek, R.; Helbich, T.H.; Pinker, K. AI-enhanced simultaneous multiparametric 18F-FDG PET/MRI for accurate breast cancer diagnosis. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 596–608. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Giger, M.L.; Huynh, B.Q.; Antropova, N.O. Deep learning in breast cancer risk assessment: Evaluation of convolutional neural networks on a clinical dataset of full-field digital mammograms. J. Med. Imaging 2017, 4, 041304. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Katal, S.; McKay, M.J.; Taubman, K. PET Molecular Imaging in Breast Cancer: Current Applications and Future Perspectives. J. Clin. Med. 2024, 13, 3459. https://doi.org/10.3390/jcm13123459
Katal S, McKay MJ, Taubman K. PET Molecular Imaging in Breast Cancer: Current Applications and Future Perspectives. Journal of Clinical Medicine. 2024; 13(12):3459. https://doi.org/10.3390/jcm13123459
Chicago/Turabian StyleKatal, Sanaz, Michael J. McKay, and Kim Taubman. 2024. "PET Molecular Imaging in Breast Cancer: Current Applications and Future Perspectives" Journal of Clinical Medicine 13, no. 12: 3459. https://doi.org/10.3390/jcm13123459
APA StyleKatal, S., McKay, M. J., & Taubman, K. (2024). PET Molecular Imaging in Breast Cancer: Current Applications and Future Perspectives. Journal of Clinical Medicine, 13(12), 3459. https://doi.org/10.3390/jcm13123459






