Functional Outcome after Direct Anterior Approach Total Hip Arthroplasty (DAA-THA) for Coxa Profunda and Protrusio Acetabuli—A Retrospective Study
Abstract
1. Introduction
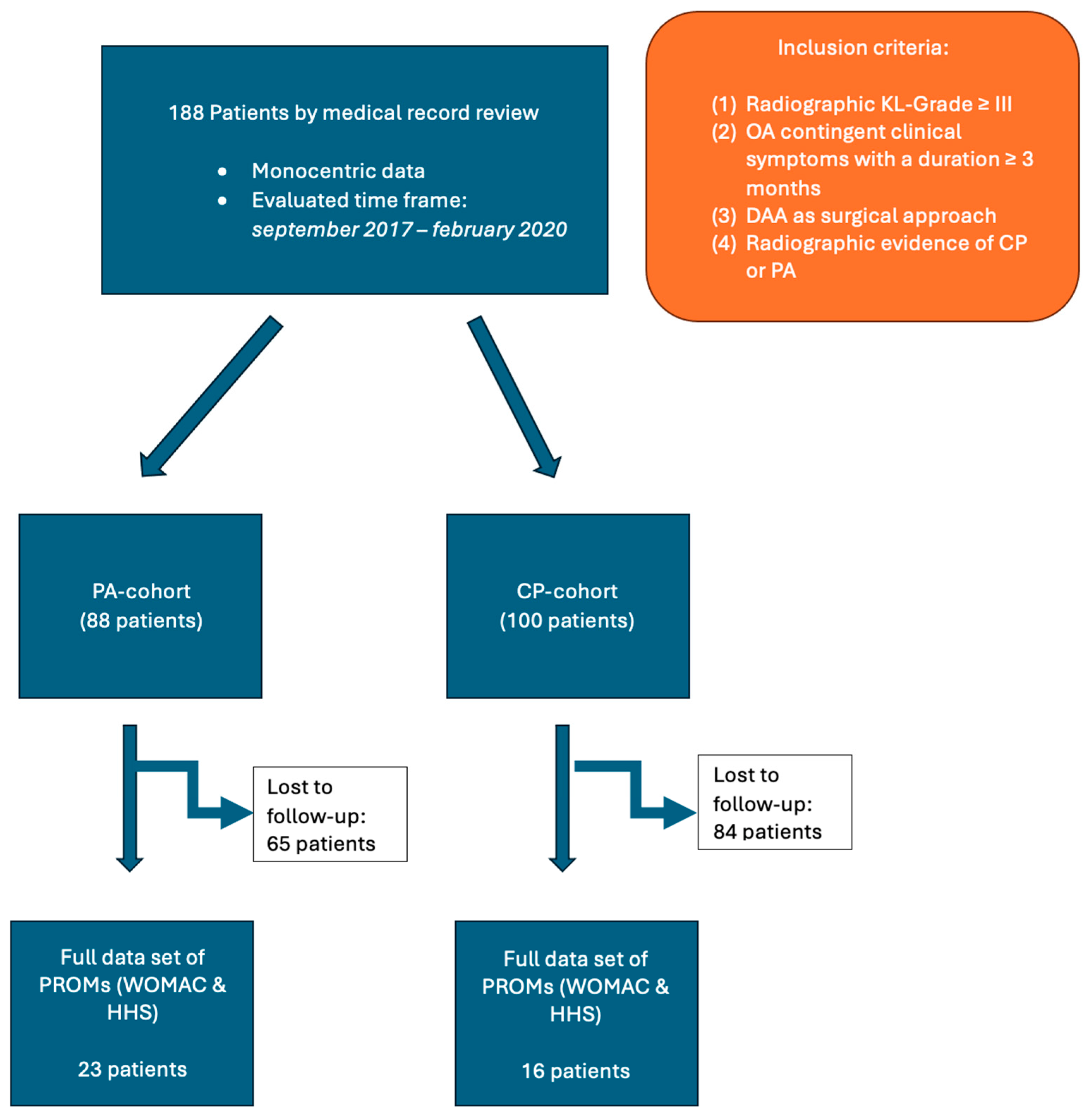
2. Materials and Methods
2.1. Study Population
2.2. Surgical Technique
2.3. Radiographic Features
2.4. Statistical Analysis
3. Results
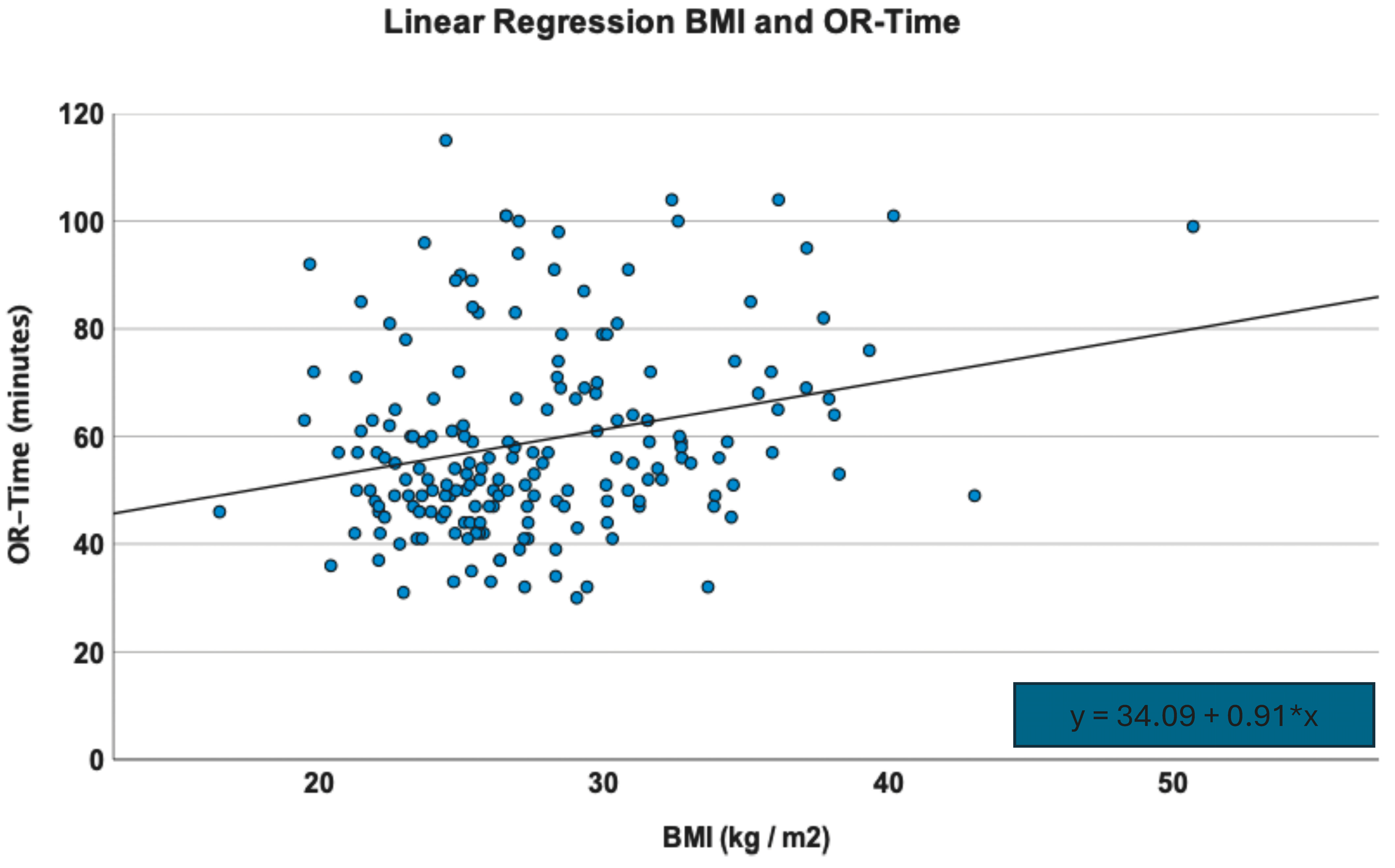
3.1. Patient Demographics
3.2. Radiographic Outcome
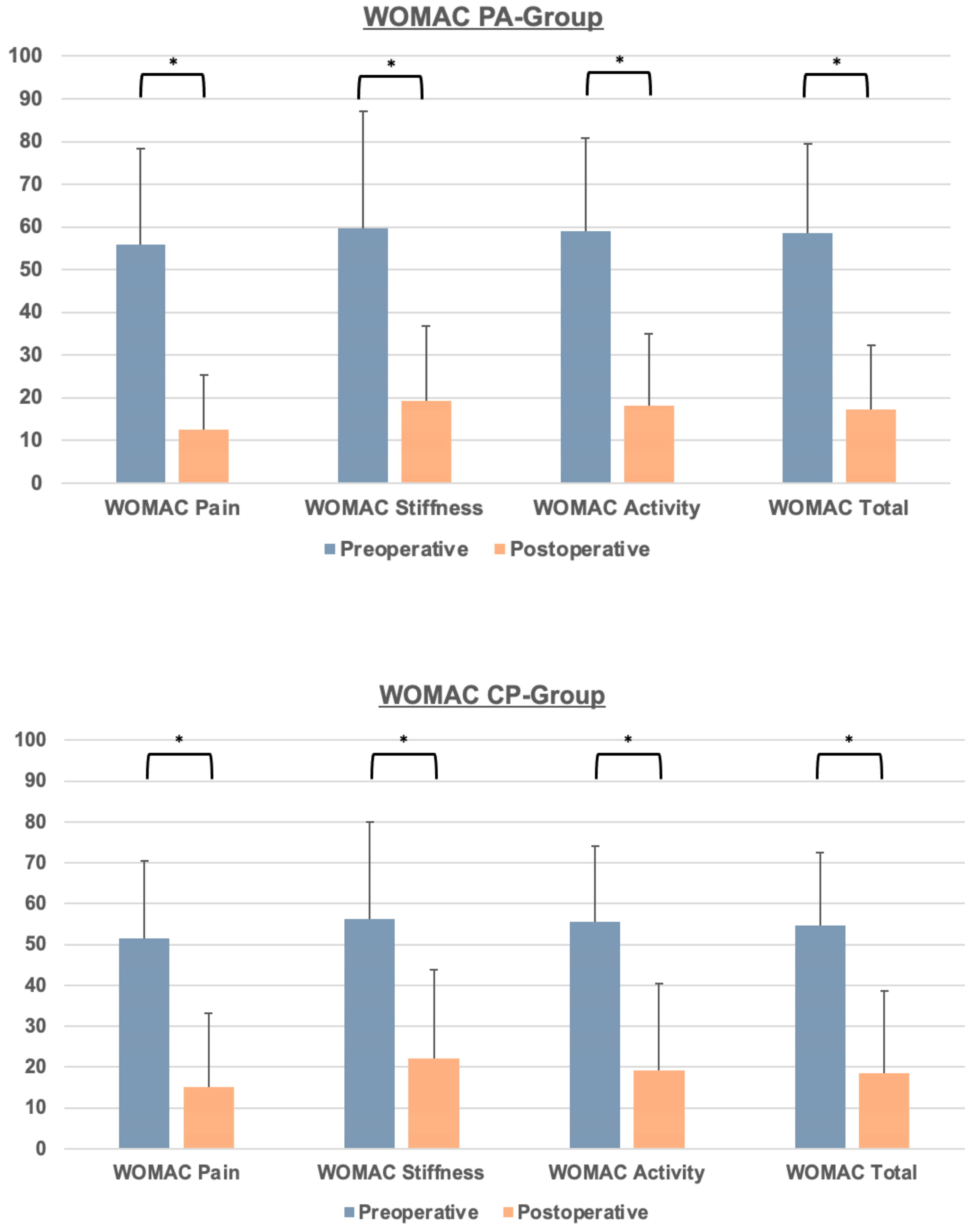
3.3. Clinical Outcome and PROMs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Learmonth, I.D.; Young, C.; Rorabeck, C. The operation of the century: Total hip replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef] [PubMed]
- Clohisy, J.C.; Carlisle, J.C.; Beaulé, P.E.; Kim, Y.J.; Trousdale, R.T.; Sierra, R.J.; Leunig, M.; Schoenecker, P.L.; Millis, M.B. A systematic approach to the plain radiographic evaluation of the young adult hip. J. Bone Jt. Surg. Am. 2008, 90 (Suppl. 4), 47–66. [Google Scholar] [CrossRef] [PubMed]
- Armbuster, T.G.; Guerra, J., Jr.; Resnick, D.; Goergen, T.G.; Feingold, M.L.; Niwayama, G.; Danzig, L.A. The adult hip: An anatomic study. Part I: The bony landmarks. Radiology 1978, 128, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Guerra, J., Jr.; Armbuster, T.G.; Resnick, D.; Goergen, T.G.; Feingold, M.L.; Niwayama, G.; Danzig, L.A. The adult hip: An anatomic study. Part II: The soft-tissue landmarks. Radiology 1978, 128, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Qiao, Y.-J.; Lou, J.-P.; Cao, G.; Chang, Y.; Zhou, S.-H. Cementless total hip arthroplasty for treatment of acetabular protrusion secondary to rheumatoid arthritis. J. Orthop. Surg. Res. 2023, 18, 282. [Google Scholar] [CrossRef] [PubMed]
- Lu, N.; Yang, Y.; Chen, H.; Li, W.; Pu, B.; Liu, L. Health-type total hip arthroplasty combined with compression bone grafting for rheumatoid arthritis with acetabular retraction. Chin. J. Reconstr. Surg. 2015, 29, 160–162. [Google Scholar]
- Zhen, P.; Li, X.; Zhou, S.; Lu, H.; Chen, H.; Liu, J. Total hip arthroplasty to treat acetabular protrusions secondary to rheumatoid arthritis. J. Orthop. Surg. Res. 2018, 13, 92. [Google Scholar] [CrossRef]
- Baghdadi, Y.M.K.; Larson, A.N.; Sierra, R.J. Long-term results of the uncemented acetabular component in a primary total hip arthroplasty performed for protrusio acetabuli: A fifteen year median follow-up. Int. Orthop. 2015, 39, 839–845. [Google Scholar] [CrossRef] [PubMed]
- McBride, M.T.; Muldoon, M.P.; Santore, R.F.; Trousdale, R.T.; Wenger, D.R. Protrusio acetabuli: Diagnosis and treatment. J. Am. Acad. Orthop. Surg. 2001, 9, 79–88. [Google Scholar] [CrossRef]
- Gilmour, J. Adolescent deformities of the acetabulum: An investigation into the nature of protrusio acetabuli. Br. J. Surg. 2005, 26, 670–699. [Google Scholar] [CrossRef]
- Alexander, C. The Aetiology of Primary Protrusio Acetabuli. Br. J. Radiol. 1965, 38, 567–580. [Google Scholar] [CrossRef]
- Hirst, P.; Esser, M.; Murphy, J.C.; Hardinge, K. Bone grafting for protrusio acetabuli during total hip replacement. A review of the Wrightington method in 61 hips. J. Bone Jt. Surg. Br. 1987, 69, 229–233. [Google Scholar] [CrossRef]
- Garcia-Cimbrelo, E.; Diaz-Martin, A.; Madero, R.; Munera, L. Loosening of the cup after low-friction arthroplasty in patients with acetabular protrusion. The importance of the position of the cup. J. Bone Jt. Surg. Br. 2000, 82, 108–115. [Google Scholar] [CrossRef]
- Welten, M.L.; Schreurs, B.W.; Buma, P.; Verdonschot, N.; Slooff, T.J. Acetabular reconstruction with impacted morcellized cancellous bone autograft and cemented primary total hip arthroplasty: A 10- to 17-year follow-up study. J. Arthroplast. 2000, 15, 819–824. [Google Scholar] [CrossRef]
- Mullaji, A.B.; Shetty, G.M. Acetabular protrusio: Surgical technique of dealing with a problem in depth. Bone Jt. J. 2013, 95-b (Suppl. A), 37–40. [Google Scholar] [CrossRef]
- Zuh, S.-G.; Zazgyva, A.; Gergely, I.; Pop, T.S. Acetabuloplasty with bone grafting in uncemented hip replacement for protrusion. Int. Orthop. 2015, 39, 1757–1763. [Google Scholar] [CrossRef] [PubMed]
- Mullaji, A.B.; Marawar, S.V. Primary total hip arthroplasty in protrusio acetabuli using impacted morsellized bone grafting and cementless cups: A medium-term radiographic review. J. Arthroplast. 2007, 22, 1143–1149. [Google Scholar] [CrossRef] [PubMed]
- Heinz, T.; Vasilev, H.; Anderson, P.M.; Stratos, I.; Jakuscheit, A.; Horas, K.; Holzapfel, B.M.; Rudert, M.; Weißenberger, M. The Direct Anterior Approach (DAA) as a Standard Approach for Total Hip Arthroplasty (THA) in Coxa Profunda and Protrusio Acetabuli? A Radiographic Analysis of 188 Cases. J. Clin. Med. 2023, 12, 3941. [Google Scholar] [CrossRef]
- Yun, A.; Qutami, M.; Carles, E. Managing Protrusio Acetabuli With a Direct Anterior Approach Total Hip Replacement. Cureus 2021, 13, e14048. [Google Scholar] [CrossRef]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13 (Suppl. 1), S31–S34. [Google Scholar] [CrossRef]
- Günther, K.P.; Deckert, S.; Lützner, C.; Lange, T.; Schmitt, J.; Postler, A. Total Hip Replacement for Osteoarthritis-Evidence-Based and Patient-Oriented Indications. Dtsch. Arztebl. Int. 2021, 118, 730–736. [Google Scholar] [CrossRef]
- Lützner, C.; Deckert, S.; Günther, K.-P.; Postler, A.E.; Lützner, J.; Schmitt, J.; Limb, D.; Lange, T. Indication Criteria for Total Hip Arthroplasty in Patients with Hip Osteoarthritis—Recommendations from a German Consensus Initiative. Medicina 2022, 58, 574. [Google Scholar] [CrossRef] [PubMed]
- Association, W.M. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Rudert, M.; Thaler, M.; Holzapfel, B.M. Primary hip arthroplasty via the direct anterior approach. Oper. Orthop. Traumatol. 2021, 33, 287. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.A.; Schleck, C.; Harmsen, S.; Lewallen, D. Clinically important improvement thresholds for Harris Hip Score and its ability to predict revision risk after primary total hip arthroplasty. BMC Musculoskelet. Disord. 2016, 17, 256. [Google Scholar] [CrossRef] [PubMed]
- MacKay, C.; Clements, N.; Wong, R.; Davis, A.M. A systematic review of estimates of the minimal clinically important difference and patient acceptable symptom state of the Western Ontario and McMaster Universities Osteoarthritis Index in patients who underwent total hip and total knee replacement. Osteoarthr. Cartil. 2019, 27, 1408–1419. [Google Scholar] [CrossRef] [PubMed]
- Hastings, D.E.; Parker, S.M. Protrusio acetabuli in rheumatoid arthritis. Clin. Orthop. Relat. Res. 1975, 108, 76–83. [Google Scholar] [CrossRef]
- Bayley, J.C.; Christie, M.J.; Ewald, F.C.; Kelley, K. Long-term results of total hip arthroplasty in protrusio acetabuli. J. Arthroplast. 1987, 2, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Salvati, E.A.; Bullough, P.; Wilson, P.D., Jr. Intrapelvic Protrusion of the Acetabular Component Following Total Hip Replacement. Clin. Orthop. Relat. Res. 1975, 111, 212–227. [Google Scholar] [CrossRef]
- Figueras Coll, G.; Salazar Fernandez de Erenchu, J.; Roca Burniol, J. Results of acetabular wiremesh and autograft in protrusio acetabuli. Hip Int. 2008, 18, 23–28. [Google Scholar] [CrossRef]
- Baghdadi, Y.M.; Larson, A.N.; Sierra, R.J. Restoration of the hip center during THA performed for protrusio acetabuli is associated with better implant survival. Clin. Orthop. Relat. Res. 2013, 471, 3251–3259. [Google Scholar] [CrossRef]
- Ansari, S.; Gupta, K.; Gupta, T.; Raja, B.S.; Pranav, J.; Kalia, R.B. Total Hip Arthroplasty in Protrusio Acetabuli: A Systematic Review. Hip Pelvis 2024, 36, 12–25. [Google Scholar] [CrossRef]
- Rosenberg, W.W.; Schreurs, B.W.; de Waal Malefijt, M.C.; Veth, R.P.; Slooff, T.J. Impacted morsellized bone grafting and cemented primary total hip arthroplasty for acetabular protrusion in patients with rheumatoid arthritis: An 8- to 18-year follow-up study of 36 hips. Acta Orthop. Scand. 2000, 71, 143–146. [Google Scholar] [CrossRef]
- Mibe, J.; Imakiire, A.; Watanabe, T.; Fujie, T. Results of total hip arthroplasty with bone graft and support ring for protrusio acetabuli in rheumatoid arthritis. J. Orthop. Sci. 2005, 10, 8–14. [Google Scholar] [CrossRef]
- Unger, A.S.; Stronach, B.M.; Bergin, P.F.; Nogler, M. Direct anterior total hip arthroplasty. Instr. Course Lect. 2014, 63, 227–238. [Google Scholar]
- Thaler, M.; Dammerer, D.; Leitner, H.; Lindtner, R.A.; Nogler, M. Mid-term Follow-up of the Direct Anterior Approach in Acetabular Revision Hip Arthroplasty Using a Reconstruction Cage With Impaction Grafting. J. Arthroplast. 2020, 35, 1339–1343. [Google Scholar] [CrossRef]
- Prodinger, P.M.; Lazic, I.; Horas, K.; Burgkart, R.; von Eisenhart-Rothe, R.; Weissenberger, M.; Rudert, M.; Holzapfel, B.M. Revision Arthroplasty Through the Direct Anterior Approach Using an Asymmetric Acetabular Component. J. Clin. Med. 2020, 9, 3031. [Google Scholar] [CrossRef]
- Abdel, M.P.; Berry, D.J. Current Practice Trends in Primary Hip and Knee Arthroplasties Among Members of the American Association of Hip and Knee Surgeons: A Long-Term Update. J. Arthroplast. 2019, 34, S24–S27. [Google Scholar] [CrossRef] [PubMed]
- Meermans, G.; Konan, S.; Das, R.; Volpin, A.; Haddad, F.S. The direct anterior approach in total hip arthroplasty. Bone Jt. J. 2017, 99-B, 732–740. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Hou, J.-Z.; Wu, C.-H.; Zhou, Y.-J.; Gu, X.-M.; Wang, H.-H.; Feng, W.; Cheng, Y.-X.; Sheng, X.; Bao, H.-W. A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. J. Orthop. Surg. Res. 2018, 13, 229. [Google Scholar] [CrossRef]
- Awad, M.E.; Farley, B.J.; Mostafa, G.; Saleh, K.J. Direct anterior approach has short-term functional benefit and higher resource requirements compared with the posterior approach in primary total hip arthroplasty. Bone Jt. J. 2021, 103-B, 1078–1087. [Google Scholar] [CrossRef]

| Type of PROM | Time of Evaluation |
|---|---|
| EQ5D | Preoperative 1 year postoperative 5 years postoperative |
| WOMAC | Preoperative 1 year postoperative 5 years postoperative |
| Harris Hip Score (HHS) | Preoperative 3 years postoperative |
| VAS | Preoperative 1 year postoperative |
| Item | PA-Group | CP-Group | |
|---|---|---|---|
| Mean (±SD), rel. frequency | p-value (CP-group vs. PA-group) | ||
| Age (years ± SD) | 71.61 ± 12.41 | 67.05 ± 10.23 | 0.01 |
| ASA | I: 1 (1.1%) II: 56 (63.6%) III: 30 (34.1%) IV: 1 (1.1%) | I: 6 (6.0%) II: 65 (65.0%) III: 28 (28.0%) IV: 1 (1.0%) | 0.31 |
| BMI (kg/m2) | 27.24 ± 4.61 | 27.91 ± 5.25 | 0.36 |
| Sex (female/male) | 75/13, 85.20%/14.80% | 82/18, 82.0%/18.0% | 0.35 |
| Hip flexion preoperative (degrees) | 82. 63 ± 17.80 | 90.20 ± 16.60 | 0.00 |
| Hip flexion postoperative (degrees) | 112.14 ± 9.17 | 101.67 ± 20.05 | 0.02 |
| Method of fixation (cementless/hybrid/fully cemented) | 72/11/5 | 94/6/0 | 0.01 |
| LOS (days ± SD) | 9.11 ± 3.58 | 8.44 ± 2.10 | 0.11 |
| CP-Group | PA-Group | p-Value (CP-Group vs. PA-Group) | |
|---|---|---|---|
| WOMAC Pain preoperative | 51.60 ± 19.00 | 55.86 + 22.39 | 0.17 |
| WOMAC Pain postoperative | 15.08 ± 18.06 | 12.60 ± 12.79 | 0.36 |
| p-value (preoperative vs. postoperative) | <0.00 | <0.00 | |
| WOMAC Stiffness preoperative | 56.16 ± 23.83 | 59.73 ± 19.21 | 0.35 |
| WOMAC Stiffness postoperative | 22.10 ± 21.70 | 19.21 ± 17.51 | 0.39 |
| p-value (preoperative vs. postoperative) | <0.00 | <0.00 | |
| WOMAC Activity preoperative | 55.61 ± 18.45 | 58.94 ± 18.12 | 0.26 |
| WOMAC Activity postoperative | 19.18 ± 21.30 | 18.16 ± 16.81 | 0.76 |
| p-value (preoperative vs. postoperative) | <0.00 | <0.00 | |
| WOMAC Total preoperative | 54.65 ± 17.83 | 58.52 ± 20.94 | 0.18 |
| WOMAC Total postoperative | 18.58 ± 20.11 | 17.15 ± 15.07 | 0.64 |
| p-value (preoperative vs. postoperative) | <0.00 | <0.00 |
| CP-Group | PA-Group | |
|---|---|---|
| Complication rates (total number n, percent %) | ||
| Postoperative anemia | 3 (3.00%) | 2 (2.27%) |
| Prolonged wound healing | 4 (4.00%) | 4 (4.54%) |
| Postoperative regional paresthesia | 2 (2.00%) | 1 (1.14%) |
| Respiratory infection | 2 (2.00%) | 2 (2.27%) |
| Intraoperative fracture (femur or acetabulum) | 1 (0.53%) | 2 (1.06%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heinz, T.; Vasilev, H.; Anderson, P.M.; Stratos, I.; Jakuscheit, A.; Horas, K.; Holzapfel, B.M.; Rudert, M.; Weißenberger, M. Functional Outcome after Direct Anterior Approach Total Hip Arthroplasty (DAA-THA) for Coxa Profunda and Protrusio Acetabuli—A Retrospective Study. J. Clin. Med. 2024, 13, 4596. https://doi.org/10.3390/jcm13164596
Heinz T, Vasilev H, Anderson PM, Stratos I, Jakuscheit A, Horas K, Holzapfel BM, Rudert M, Weißenberger M. Functional Outcome after Direct Anterior Approach Total Hip Arthroplasty (DAA-THA) for Coxa Profunda and Protrusio Acetabuli—A Retrospective Study. Journal of Clinical Medicine. 2024; 13(16):4596. https://doi.org/10.3390/jcm13164596
Chicago/Turabian StyleHeinz, Tizian, Hristo Vasilev, Philip Mark Anderson, Ioannis Stratos, Axel Jakuscheit, Konstantin Horas, Boris Michael Holzapfel, Maximilian Rudert, and Manuel Weißenberger. 2024. "Functional Outcome after Direct Anterior Approach Total Hip Arthroplasty (DAA-THA) for Coxa Profunda and Protrusio Acetabuli—A Retrospective Study" Journal of Clinical Medicine 13, no. 16: 4596. https://doi.org/10.3390/jcm13164596
APA StyleHeinz, T., Vasilev, H., Anderson, P. M., Stratos, I., Jakuscheit, A., Horas, K., Holzapfel, B. M., Rudert, M., & Weißenberger, M. (2024). Functional Outcome after Direct Anterior Approach Total Hip Arthroplasty (DAA-THA) for Coxa Profunda and Protrusio Acetabuli—A Retrospective Study. Journal of Clinical Medicine, 13(16), 4596. https://doi.org/10.3390/jcm13164596









