Effect of Graft Choice for ACL Reconstruction on Clinical Outcomes in Combined ACL and MCL Injuries: Comparison Between Bone-Patellar Tendon-Bone and Hamstring Autografts
Abstract
1. Introduction
2. Materials and Methods
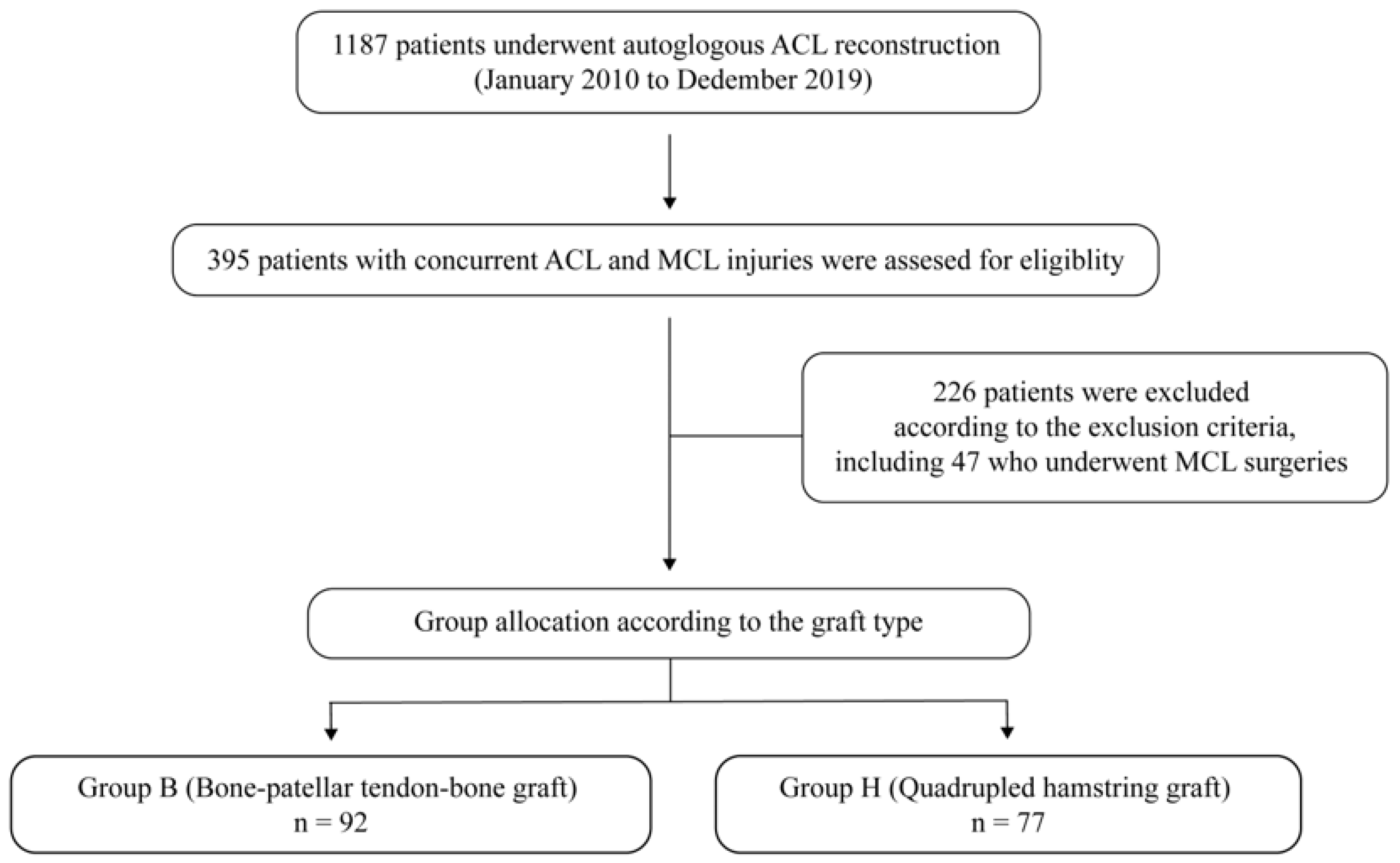
2.1. Patients
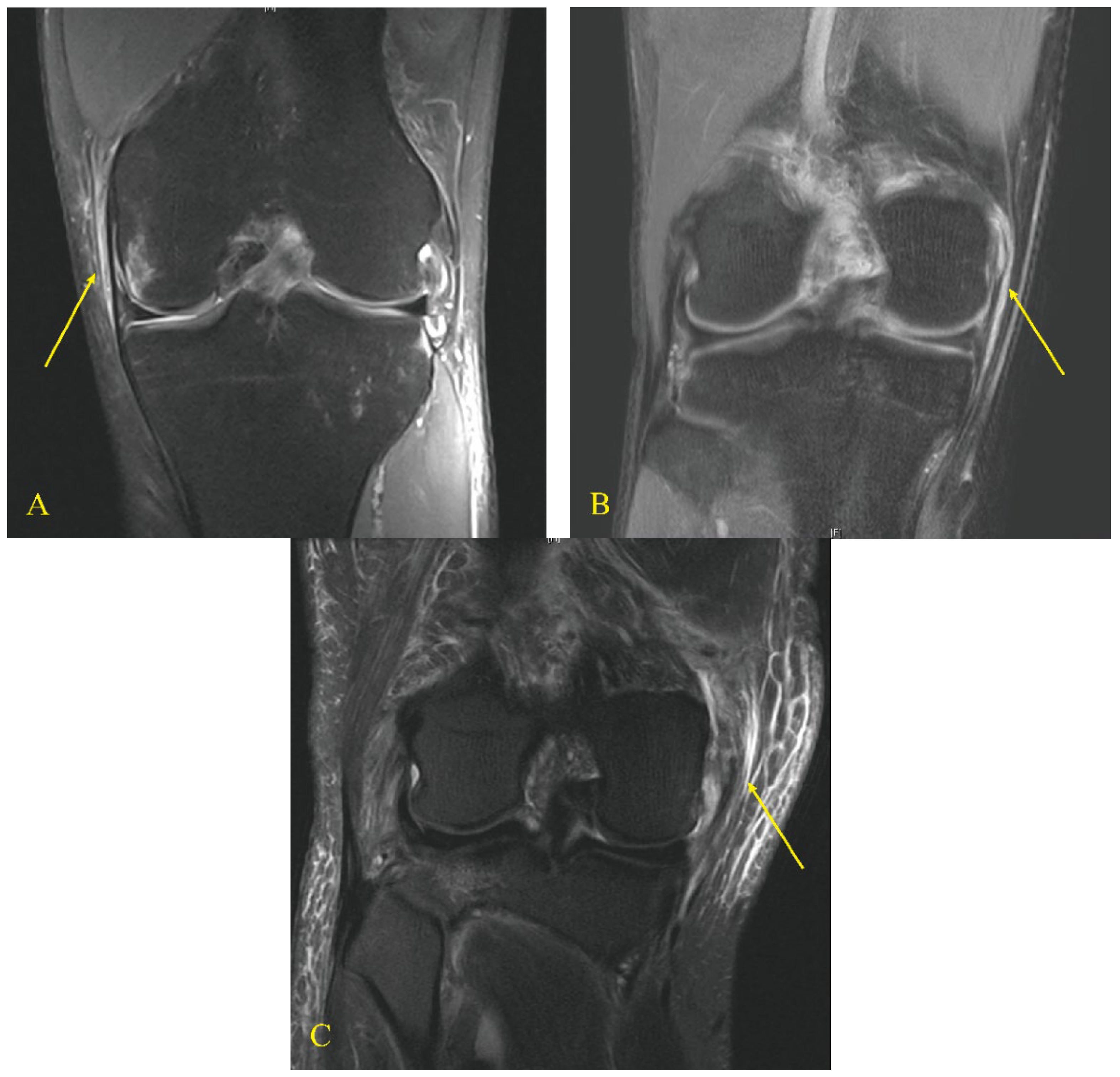
2.2. Clinical Assessments
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Duncan, J.B.; Hunter, R.; Purnell, M.; Freeman, J. Meniscal injuries associated with acute anterior cruciate ligament tears in alpine skiers. Am. J. Sports Med. 1995, 23, 170–172. [Google Scholar] [CrossRef] [PubMed]
- LaPrade, R.F.; Wentorf, F.A.; Fritts, H.; Gundry, C.; Hightower, C.D. A prospective magnetic resonance imaging study of the incidence of posterolateral and multiple ligament injuries in acute knee injuries presenting with a hemarthrosis. Arthrosc. J. Arthrosc. Relat. Surg. 2007, 23, 1341–1347. [Google Scholar] [CrossRef] [PubMed]
- Yoon, K.H.; Yoo, J.H.; Kim, K.I. Bone contusion and associated meniscal and medial collateral ligament injury in patients with anterior cruciate ligament rupture. J. Bone Jt. Surg. 2011, 93, 1510–1518. [Google Scholar] [CrossRef] [PubMed]
- Von Rehlingen-Prinz, F.; Leiderer, M.; Dehoust, J.; Dust, T.; Kowald, B.; Frosch, K.H.; Izadpanah, K.; Henes, F.O.; Krause, M. Association of medial collateral ligament complex injuries with anterior cruciate ligament ruptures based on posterolateral tibial plateau injuries. Sports Med. Open 2023, 9, 70. [Google Scholar] [CrossRef]
- Smyth, M.P.; Koh, J.L. A review of surgical and nonsurgical outcomes of medial knee injuries. Sports Med. Arthrosc. Rev. 2015, 23, e15–e22. [Google Scholar] [CrossRef]
- Tandogan, N.R.; Kayaalp, A. Surgical treatment of medial knee ligament injuries: Current indications and techniques. EFORT Open Rev. 2016, 1, 27–33. [Google Scholar] [CrossRef]
- Elkin, J.L.; Zamora, E.; Gallo, R.A. Combined anterior cruciate ligament and medial collateral ligament knee injuries: Anatomy, diagnosis, management recommendations, and return to sport. Curr. Rev. Musculoskelet. Med. 2019, 12, 239–244. [Google Scholar] [CrossRef]
- Halinen, J.; Lindahl, J.; Hirvensalo, E. Range of motion and quadriceps muscle power after early surgical treatment of acute combined anterior cruciate and grade-iii medial collateral ligament injuries. A prospective randomized study. J. Bone Jt. Surg. 2009, 91, 1305–1312. [Google Scholar] [CrossRef]
- Westermann, R.W.; Spindler, K.P.; Huston, L.J.; Wolf, B.R. Outcomes of grade iii medial collateral ligament injuries treated concurrently with anterior cruciate ligament reconstruction: A multicenter study. Arthrosc. J. Arthrosc. Relat. Surg. 2019, 35, 1466–1472. [Google Scholar] [CrossRef]
- Halinen, J.; Lindahl, J.; Hirvensalo, E.; Santavirta, S. Operative and nonoperative treatments of medial collateral ligament rupture with early anterior cruciate ligament reconstruction: A prospective randomized study. Am. J. Sports Med. 2006, 34, 1134–1140. [Google Scholar] [CrossRef]
- Noyes, F.R.; Barber-Westin, S.D. The treatment of acute combined ruptures of the anterior cruciate and medial ligaments of the knee. Am. J. Sports Med. 1995, 23, 380–389. [Google Scholar] [CrossRef] [PubMed]
- Shelbourne, K.D.; Porter, D.A. Anterior cruciate ligament-medial collateral ligament injury: Nonoperative management of medial collateral ligament tears with anterior cruciate ligament reconstruction. A preliminary report. Am. J. Sports Med. 1992, 20, 283–286. [Google Scholar] [CrossRef] [PubMed]
- Noyes, F.R.; Butler, D.L.; Grood, E.S.; Zernicke, R.F.; Hefzy, M.S. Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J. Bone Jt. Surg. 1984, 66, 344–352. [Google Scholar] [CrossRef]
- Shani, R.H.; Umpierez, E.; Nasert, M.; Hiza, E.A.; Xerogeanes, J. Biomechanical comparison of quadriceps and patellar tendon grafts in anterior cruciate ligament reconstruction. Arthrosc. J. Arthrosc. Relat. Surg. 2016, 32, 71–75. [Google Scholar] [CrossRef]
- Schimoler, P.J.; Braun, D.T.; Miller, M.C.; Akhavan, S. Quadrupled hamstring graft strength as a function of clinical sizing. Arthrosc. J. Arthrosc. Relat. Surg. 2015, 31, 1091–1096. [Google Scholar] [CrossRef]
- Wilson, T.W.; Zafuta, M.P.; Zobitz, M. A biomechanical analysis of matched bone-patellar tendon-bone and double-looped semitendinosus and gracilis tendon grafts. Am. J. Sports Med. 1999, 27, 202–207. [Google Scholar] [CrossRef]
- Freedman, K.B.; D’Amato, M.J.; Nedeff, D.D.; Kaz, A.; Bach, B.R., Jr. Arthroscopic anterior cruciate ligament reconstruction: A metaanalysis comparing patellar tendon and hamstring tendon autografts. Am. J. Sports Med. 2003, 31, 2–11. [Google Scholar] [CrossRef]
- Geib, T.M.; Shelton, W.R.; Phelps, R.A.; Clark, L. Anterior cruciate ligament reconstruction using quadriceps tendon autograft: Intermediate-term outcome. Arthrosc. J. Arthrosc. Relat. Surg. 2009, 25, 1408–1414. [Google Scholar] [CrossRef]
- Tashiro, T.; Kurosawa, H.; Kawakami, A.; Hikita, A.; Fukui, N. Influence of medial hamstring tendon harvest on knee flexor strength after anterior cruciate ligament reconstruction. A detailed evaluation with comparison of single- and double-tendon harvest. Am. J. Sports Med. 2003, 31, 522–529. [Google Scholar] [CrossRef]
- Mouarbes, D.; Menetrey, J.; Marot, V.; Courtot, L.; Berard, E.; Cavaignac, E. Anterior cruciate ligament reconstruction: A systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone-patellar tendon-bone and hamstring-tendon autografts. Am. J. Sports Med. 2019, 47, 3531–3540. [Google Scholar] [CrossRef]
- Samuelsen, B.T.; Webster, K.E.; Johnson, N.R.; Hewett, T.E.; Krych, A.J. Hamstring autograft versus patellar tendon autograft for acl reconstruction: Is there a difference in graft failure rate? A meta-analysis of 47,613 patients. Clin. Orthop. Relat. Res. 2017, 475, 2459–2468. [Google Scholar] [CrossRef] [PubMed]
- Cavaignac, E.; Coulin, B.; Tscholl, P.; Nik Mohd Fatmy, N.; Duthon, V.; Menetrey, J. Is quadriceps tendon autograft a better choice than hamstring autograft for anterior cruciate ligament reconstruction? A comparative study with a mean follow-up of 3.6 years. Am. J. Sports Med. 2017, 45, 1326–1332. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Lee, S.K.; Choi, C.H.; Kim, S.H.; Kim, S.H.; Jung, M. Graft selection in anterior cruciate ligament reconstruction for smoking patients. Am. J. Sports Med. 2014, 42, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Herbort, M.; Michel, P.; Raschke, M.J.; Vogel, N.; Schulze, M.; Zoll, A.; Fink, C.; Petersen, W.; Domnick, C. Should the ipsilateral hamstrings be used for anterior cruciate ligament reconstruction in the case of medial collateral ligament insufficiency? Biomechanical investigation regarding dynamic stabilization of the medial compartment by the hamstring muscles. Am. J. Sports Med. 2017, 45, 819–825. [Google Scholar] [CrossRef]
- Kremen, T.J.; Polakof, L.S.; Rajaee, S.S.; Nelson, T.J.; Metzger, M.F. The effect of hamstring tendon autograft harvest on the restoration of knee stability in the setting of concurrent anterior cruciate ligament and medial collateral ligament injuries. Am. J. Sports Med. 2018, 46, 163–170. [Google Scholar] [CrossRef]
- Paley, D.; Herzenberg, J.E.; Tetsworth, K.; McKie, J.; Bhave, A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop. Clin. N. Am. 1994, 25, 425–465. [Google Scholar] [CrossRef]
- Naraghi, A.M.; White, L.M. Imaging of athletic injuries of knee ligaments and menisci: Sports imaging series. Radiology 2016, 281, 23–40. [Google Scholar] [CrossRef]
- Kim, S.J.; Choi, C.H.; Kim, S.H.; Lee, S.K.; Lee, W.; Kim, T.; Jung, M. Bone-patellar tendon-bone autograft could be recommended as a superior graft to hamstring autograft for acl reconstruction in patients with generalized joint laxity: 2- and 5-year follow-up study. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 2568–2579. [Google Scholar] [CrossRef]
- Laprade, R.F.; Bernhardson, A.S.; Griffith, C.J.; Macalena, J.A.; Wijdicks, C.A. Correlation of valgus stress radiographs with medial knee ligament injuries: An in vitro biomechanical study. Am. J. Sports Med. 2010, 38, 330–338. [Google Scholar] [CrossRef]
- Lysholm, J.; Gillquist, J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am. J. Sports Med. 1982, 10, 150–154. [Google Scholar] [CrossRef]
- Hefti, F.; Muller, W.; Jakob, R.P.; Staubli, H.U. Evaluation of knee ligament injuries with the ikdc form. Knee Surg. Sports Traumatol. Arthrosc. 1993, 1, 226–234. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using g*power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Sajovic, M.; Stropnik, D.; Skaza, K. Long-term comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: A 17-year follow-up of a randomized controlled trial. Am. J. Sports Med. 2018, 46, 1800–1808. [Google Scholar] [CrossRef]
- Bjornsson, H.; Samuelsson, K.; Sundemo, D.; Desai, N.; Sernert, N.; Rostgard-Christensen, L.; Karlsson, J.; Kartus, J. A randomized controlled trial with mean 16-year follow-up comparing hamstring and patellar tendon autografts in anterior cruciate ligament reconstruction. Am. J. Sports Med. 2016, 44, 2304–2313. [Google Scholar] [CrossRef]
- Svensson, M.; Sernert, N.; Ejerhed, L.; Karlsson, J.; Kartus, J.T. A prospective comparison of bone-patellar tendon-bone and hamstring grafts for anterior cruciate ligament reconstruction in female patients. Knee Surg. Sports Traumatol. Arthrosc. 2006, 14, 278–286. [Google Scholar] [CrossRef]
- Webster, K.E.; Feller, J.A.; Hartnett, N.; Leigh, W.B.; Richmond, A.K. Comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction: A 15-year follow-up of a randomized controlled trial. Am. J. Sports Med. 2016, 44, 83–90. [Google Scholar] [CrossRef]
- Taylor, D.C.; DeBerardino, T.M.; Nelson, B.J.; Duffey, M.; Tenuta, J.; Stoneman, P.D.; Sturdivant, R.X.; Mountcastle, S. Patellar tendon versus hamstring tendon autografts for anterior cruciate ligament reconstruction: A randomized controlled trial using similar femoral and tibial fixation methods. Am. J. Sports Med. 2009, 37, 1946–1957. [Google Scholar] [CrossRef]
- Andernord, D.; Bjornsson, H.; Petzold, M.; Eriksson, B.I.; Forssblad, M.; Karlsson, J.; Samuelsson, K. Surgical predictors of early revision surgery after anterior cruciate ligament reconstruction: Results from the swedish national knee ligament register on 13,102 patients. Am. J. Sports Med. 2014, 42, 1574–1582. [Google Scholar] [CrossRef]
- Xie, X.; Liu, X.; Chen, Z.; Yu, Y.; Peng, S.; Li, Q. A meta-analysis of bone-patellar tendon-bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee 2015, 22, 100–110. [Google Scholar] [CrossRef]
- Gabler, C.M.; Jacobs, C.A.; Howard, J.S.; Mattacola, C.G.; Johnson, D.L. Comparison of graft failure rate between autografts placed via an anatomic anterior cruciate ligament reconstruction technique: A systematic review, meta-analysis, and meta-regression. Am. J. Sports Med. 2016, 44, 1069–1079. [Google Scholar] [CrossRef]
- Ciccotti, M.C.; Secrist, E.; Tjoumakaris, F.; Ciccotti, M.G.; Freedman, K.B. Anatomic anterior cruciate ligament reconstruction via independent tunnel drilling: A systematic review of randomized controlled trials comparing patellar tendon and hamstring autografts. Arthrosc. J. Arthrosc. Relat. Surg. 2017, 33, 1062–1071.e5. [Google Scholar] [CrossRef] [PubMed]
- Zaffagnini, S.; Bonanzinga, T.; Marcheggiani Muccioli, G.M.; Giordano, G.; Bruni, D.; Bignozzi, S.; Lopomo, N.; Marcacci, M. Does chronic medial collateral ligament laxity influence the outcome of anterior cruciate ligament reconstruction?: A prospective evaluation with a minimum three-year follow-up. J. Bone Jt. Surg. 2011, 93, 1060–1064. [Google Scholar] [CrossRef]
- Svantesson, E.; Hamrin Senorski, E.; Ostergaard, M.; Grassi, A.; Krupic, F.; Westin, O.; Samuelsson, K. Graft choice for anterior cruciate ligament reconstruction with a concomitant non-surgically treated medial collateral ligament injury does not influence the risk of revision. Arthrosc. J. Arthrosc. Relat. Surg. 2020, 36, 199–211. [Google Scholar] [CrossRef]
- Dijkman, B.; Kooistra, B.; Bhandari, M. How to work with a subgroup analysis. Can. J. Surg. 2009, 52, 515–522. [Google Scholar] [PubMed]
- Vermorel, P.H.; Testa, R.; Klasan, A.; Putnis, S.E.; Philippot, R.; Sonnery-Cottet, B.; Neri, T. Contribution of the medial hamstrings to valgus stability of the knee. Orthop. J. Sports Med. 2023, 11, 23259671231202767. [Google Scholar] [CrossRef] [PubMed]
- Vosoughi, F.; Rezaei Dogahe, R.; Nuri, A.; Ayati Firoozabadi, M.; Mortazavi, J. Medial collateral ligament injury of the knee: A review on current concept and management. Arch. Bone Jt. Surg. 2021, 9, 255–262. [Google Scholar]
- Irrgang, J.J.; Anderson, A.F.; Boland, A.L.; Harner, C.D.; Neyret, P.; Richmond, J.C.; Shelbourne, K.D. Responsiveness of the international knee documentation committee subjective knee form. Am. J. Sports Med. 2006, 34, 1567–1573. [Google Scholar] [CrossRef]
- Tanaka, M.; Vyas, D.; Moloney, G.; Bedi, A.; Pearle, A.D.; Musahl, V. What does it take to have a high-grade pivot shift? Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 737–742. [Google Scholar] [CrossRef]

| Variable | Group B (BPTB Graft) (n = 92) | Group H (Hamstring Graft) (n = 77) | p-Value |
|---|---|---|---|
| Age (years) a | 33.3 ± 10.3 | 31.3 ± 8.0 | 0.148 |
| Sex b | |||
| Male | 70 (76.1) | 52 (67.5) | 0.216 |
| Female | 22 (23.9) | 25 (32.5) | |
| Affected side b | |||
| Left | 41 (44.6) | 34 (44.2) | 0.957 |
| Right | 51 (55.4) | 43 (55.8) | |
| Duration from injury to operation (weeks) a | 8.2 ± 2.5 | 8.3 ± 2.4 | 0.596 |
| Additional diagnosis including meniscus and cartilage lesions b | 0.891 | ||
| Yes | 54 (58.7) | 46 (59.7) | |
| No | 38 (41.3) | 31 (40.3) |
| Variable | Group B (BPTB Graft) (n = 92) | Group H (Hamstring Graft) (n = 77) | p-Value |
|---|---|---|---|
| Lachman test b | 0.702 | ||
| I | 5 (5.4) | 5 (6.5) | |
| II | 72 (78.3) | 56 (72.7) | |
| III | 15 (16.3) | 16 (20.8) | |
| SSD of Anterior translation a,c | 7.8 ± 1.9 | 7.9 ± 2.0 | 0.798 |
| MCL injury grade b | 0.890 | ||
| Grade I | 48 (52.2) | 43 (55.8) | |
| Grade II | 32 (34.8) | 25 (32.5) | |
| Grade III | 12 (13.0) | 9 (11.7) | |
| Lysholm knee score a | 65.4 ± 17.3 | 67.8 ± 10.8 | 0.914 |
| IKDC subjective score a | 51.7 ± 14.1 | 52.7 ± 8.7 | 0.577 |
| IKDC objective grade b | 0.745 | ||
| A | 0 | 0 | |
| B | 4 (4.3) | 4 (5.2) | |
| C | 69 (75.0) | 54 (70.1) | |
| D | 19 (20.7) | 19 (24.7) | |
| IKDC radiographic grade b | >0.999 | ||
| A | 87 (94.6) | 73 (94.8) | |
| B | 5 (5.4) | 4 (5.2) | |
| C | 0 | 0 | |
| D | 0 | 0 |
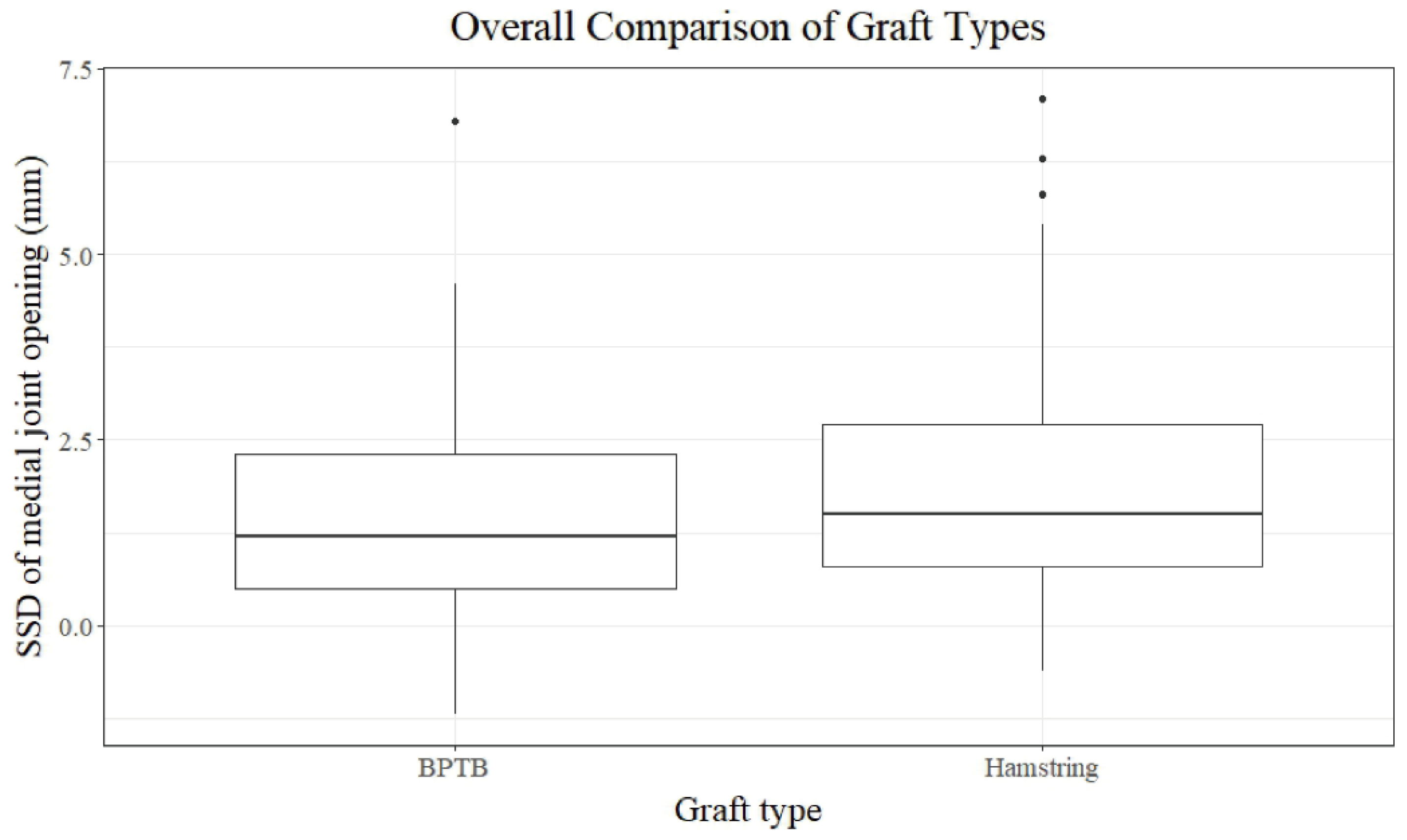
| Variable | Group B (BPTB Graft) (n = 92) | Group H (Hamstring Graft) (n = 77) | p-Value |
|---|---|---|---|
| SSD of medial joint opening a,c | 1.4 ± 1.4 | 2.0 ± 1.7 | 0.060 |
| Lachman test b | 0.949 | ||
| 0 | 71 (77.2) | 58 (75.3) | |
| I | 15 (16.3) | 14 (18.2) | |
| II | 6 (6.5) | 5 (6.5) | |
| SSD of anterior translation a,d | 2.3 ± 1.3 | 2.6 ± 1.5 | 0.317 |
| Lysholm knee score b | 85.2 ± 8.9 | 85.0 ± 7.5 | 0.576 |
| IKDC subjective score b | 83.5 ± 6.6 | 81.6 ± 8.2 | 0.110 |
| IKDC objective grade b | 0.419 | ||
| A | 68 (73.9) | 51 (66.2) | |
| B | 18 (19.6) | 17 (22.1) | |
| C | 6 (6.5) | 9 (11.7) | |
| D | 0 | 0 | |
| IKDC radiographic grade b | 0.722 | ||
| A | 81 (88.0) | 66 (85.7) | |
| B | 11 (12.0) | 10 (13.0) | |
| C | 0 | 1 (1.3) | |
| D | 0 | 0 |
| Variable | Grade I MCL Injury (n = 91) | p-Value | |
|---|---|---|---|
| BPTB (n = 48) | Hamstring (n = 43) | ||
| SSD of medial joint opening a,c | 0.9 ± 1.0 | 0.9 ± 0.8 | 0.479 |
| Lachman test b | 0.787 | ||
| 0 | 39 (81.3) | 33 (76.7) | |
| I | 7 (14.6) | 7 (16.3) | |
| II | 2 (4.2) | 3 (7.0) | |
| SSD of anterior translation a,d | 2.1 ± 1.2 | 2.4 ± 1.4 | 0.511 |
| Lysholm knee score a | 85.8 ± 9.8 | 87.2 ± 7.2 | 0.690 |
| IKDC subjective score a | 83.0 ± 6.6 | 83.7 ± 7.0 | 0.640 |
| IKDC objective grade b | 0.591 | ||
| A | 36 (75.0) | 29 (67.4) | |
| B | 10 (20.8) | 10 (23.3) | |
| C | 2 (4.2) | 4 (9.3) | |
| D | 0 | 0 | |
| IKDC radiographic grade b | >0.999 | ||
| A | 43 (89.6) | 39 (90.7) | |
| B | 5 (10.4) | 4 (9.3) | |
| C | 0 | 0 | |
| D | 0 | 0 | |
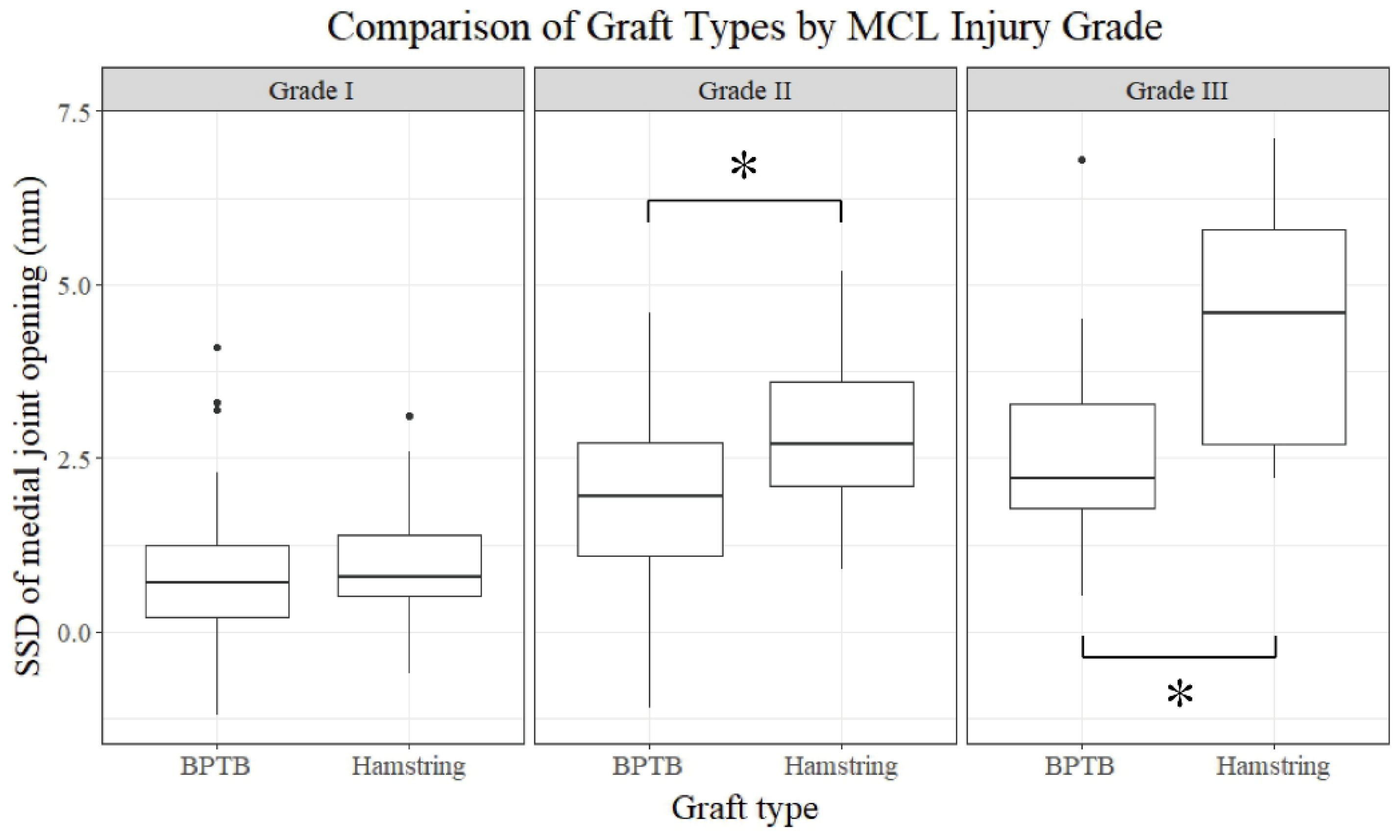
| Variable | Grade II MCL Injury (n = 57) | p-Value | |
|---|---|---|---|
| BPTB (n = 32) | Hamstring (n = 25) | ||
| SSD of medial joint opening a,c | 1.9 ± 1.4 | 2.9 ± 1.3 | 0.006 |
| Lachman test b | >0.999 | ||
| 0 | 24 (75.0) | 19 (76.0) | |
| I | 6 (18.8) | 5 (20.0) | |
| II | 2 (6.3) | 1 (4.0) | |
| SSD of anterior translation a,d | 2.2 ± 1.3 | 2.4 ± 1.4 | 0.658 |
| Lysholm knee score a | 85.1 ± 7.5 | 83.6 ± 5.9 | 0.430 |
| IKDC subjective score a | 84.4 ± 6.4 | 80.1 ± 9.3 | 0.045 |
| IKDC objective grade b | >0.999 | ||
| A | 24 (75.0) | 19 (72.0) | |
| B | 6 (18.8) | 5 (20.0) | |
| C | 2 (6.3) | 2 (8.0) | |
| D | 0 | 0 | |
| IKDC radiographic grade b | 0.720 | ||
| A | 28 (87.5) | 21 (84.0) | |
| B | 4 (12.5) | 4 (16.0) | |
| C | 0 | 0 | |
| D | 0 | 0 | |
| Variable | Grade III MCL Injury (n = 21) | p-Value | |
|---|---|---|---|
| BPTB (n = 12) | Hamstring (n = 9) | ||
| SSD of medial joint opening a,c | 2.7 ± 1.7 | 4.4 ± 1.9 | 0.039 |
| Lachman test b | >0.999 | ||
| 0 | 8 (66.7) | 6 (66.7) | |
| I | 2 (16.7) | 2 (22.2) | |
| II | 2 (16.7) | 1 (11.1) | |
| SSD of anterior translation a,d | 3.0 ± 1.5 | 3.8 ± 1.9 | 0.286 |
| Lysholm knee score a | 83.2 ± 8.6 | 78.1 ± 8.1 | 0.187 |
| IKDC subjective score a | 82.9 ± 7.3 | 75.9 ± 6.8 | 0.038 |
| IKDC objective grade b | 0.605 | ||
| A | 8 (66.7) | 4 (44.4) | |
| B | 2 (16.7) | 2 (22.2) | |
| C | 2 (16.7) | 3 (33.1) | |
| D | 0 | 0 | |
| IKDC radiographic grade b | 0.591 | ||
| A | 10 (83.3) | 6 (66.6) | |
| B | 2 (16.7) | 2 (22.2) | |
| C | 0 | 1 (11.1) | |
| D | 0 | 0 | |
| Variable | BPTB Graft (n = 92) | p-Value | ||
|---|---|---|---|---|
| Grade I Injury (n = 48) | Grade II Injury (n = 32) | Grade III Injury (n = 12) | ||
| SSD of medial joint opening a,c | 0.9 ± 1.0 | 1.9 ± 1.4 | 2.7 ± 1.7 | <0.001 |
| Lachman test b | 0.532 | |||
| 0 | 39 (81.3) | 24 (75.0) | 8 (66.7) | |
| I | 7 (14.6) | 6 (18.8) | 2 (16.7) | |
| II | 2 (4.2) | 2 (6.3) | 2 (16.7) | |
| SSD of anterior translation a,d | 2.1 ± 1.2 | 2.2 ± 1.3 | 3.0 ± 1.5 | 0.112 |
| Lysholm knee score a | 85.8 ± 9.8 | 85.1 ± 7.5 | 83.2 ± 8.6 | 0.506 |
| IKDC subjective score a | 83.0 ± 6.7 | 84.4 ± 6.4 | 82.9 ± 7.3 | 0.634 |
| IKDC objective grade b | 0.626 | |||
| A | 36 (75.0) | 24 (75.0) | 8 (66.7) | |
| B | 10 (20.8) | 6 (18.8) | 2 (16.7) | |
| C | 2 (4.2) | 2 (6.3) | 2 (16.7) | |
| D | 0 | 0 | 0 | |
| IKDC radiographic grade b | 0.743 | |||
| A | 43 (89.6) | 28 (87.5) | 10 (83.3) | |
| B | 5 (10.4) | 4 (12.5) | 2 (16.7) | |
| C | 0 | 0 | 0 | |
| D | 0 | 0 | 0 | |
| Variable | Hamstring Graft (n = 77) | p-Value | ||
|---|---|---|---|---|
| Grade I Injury (n = 43) | Grade II Injury (n = 25) | Grade III Injury (n = 9) | ||
| SSD of medial joint opening a,c | 0.9 ± 0.8 | 2.9 ± 1.3 | 4.4 ± 1.9 | <0.001 |
| Lachman test b | 0.829 | |||
| 0 | 33 (76.7) | 19 (76.0) | 6 (66.7) | |
| I | 7 (16.3) | 5 (20.0) | 2 (22.2) | |
| II | 3 (7.0) | 1 (4.0) | 1 (11.1) | |
| SSD of anterior translation a,d | 2.4 ± 1.4 | 2.4 ± 1.4 | 3.8 ± 1.9 | 0.094 |
| Lysholm knee score a | 87.2 ± 7.2 | 83.6 ± 5.9 | 78.1 ± 8.1 | 0.009 |
| IKDC subjective score a | 83.7 ± 7.0 | 80.1 ± 9.3 | 75.9 ± 6.8 | 0.015 |
| IKDC objective grade b | ||||
| A | 29 (67.4) | 18 (72.0) | 4 (44.4) | |
| B | 10 (23.3) | 5 (20.0) | 2 (22.2) | |
| C | 4 (9.3) | 2 (8.0) | 3 (33.3) | |
| D | 0 | 0 | 0 (0) | |
| IKDC radiographic grade b | 0.097 | |||
| A | 39 (90.7) | 21 (84.0) | 6 (66.7) | |
| B | 4 (9.3) | 4 (16.0) | 2 (22.2) | |
| C | 0 | 0 | 1 (11.1) | |
| D | 0 | 0 | 0 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chung, K.; Ham, H.; Kim, S.-H.; Seo, Y.-J. Effect of Graft Choice for ACL Reconstruction on Clinical Outcomes in Combined ACL and MCL Injuries: Comparison Between Bone-Patellar Tendon-Bone and Hamstring Autografts. J. Clin. Med. 2024, 13, 6316. https://doi.org/10.3390/jcm13216316
Chung K, Ham H, Kim S-H, Seo Y-J. Effect of Graft Choice for ACL Reconstruction on Clinical Outcomes in Combined ACL and MCL Injuries: Comparison Between Bone-Patellar Tendon-Bone and Hamstring Autografts. Journal of Clinical Medicine. 2024; 13(21):6316. https://doi.org/10.3390/jcm13216316
Chicago/Turabian StyleChung, Kwangho, Hyeongwon Ham, Sung-Hwan Kim, and Young-Jin Seo. 2024. "Effect of Graft Choice for ACL Reconstruction on Clinical Outcomes in Combined ACL and MCL Injuries: Comparison Between Bone-Patellar Tendon-Bone and Hamstring Autografts" Journal of Clinical Medicine 13, no. 21: 6316. https://doi.org/10.3390/jcm13216316
APA StyleChung, K., Ham, H., Kim, S.-H., & Seo, Y.-J. (2024). Effect of Graft Choice for ACL Reconstruction on Clinical Outcomes in Combined ACL and MCL Injuries: Comparison Between Bone-Patellar Tendon-Bone and Hamstring Autografts. Journal of Clinical Medicine, 13(21), 6316. https://doi.org/10.3390/jcm13216316






