Safe and Informed Use of Gadolinium-Based Contrast Agent in Body Magnetic Resonance Imaging: Where We Were and Where We Are
Abstract
1. Introduction
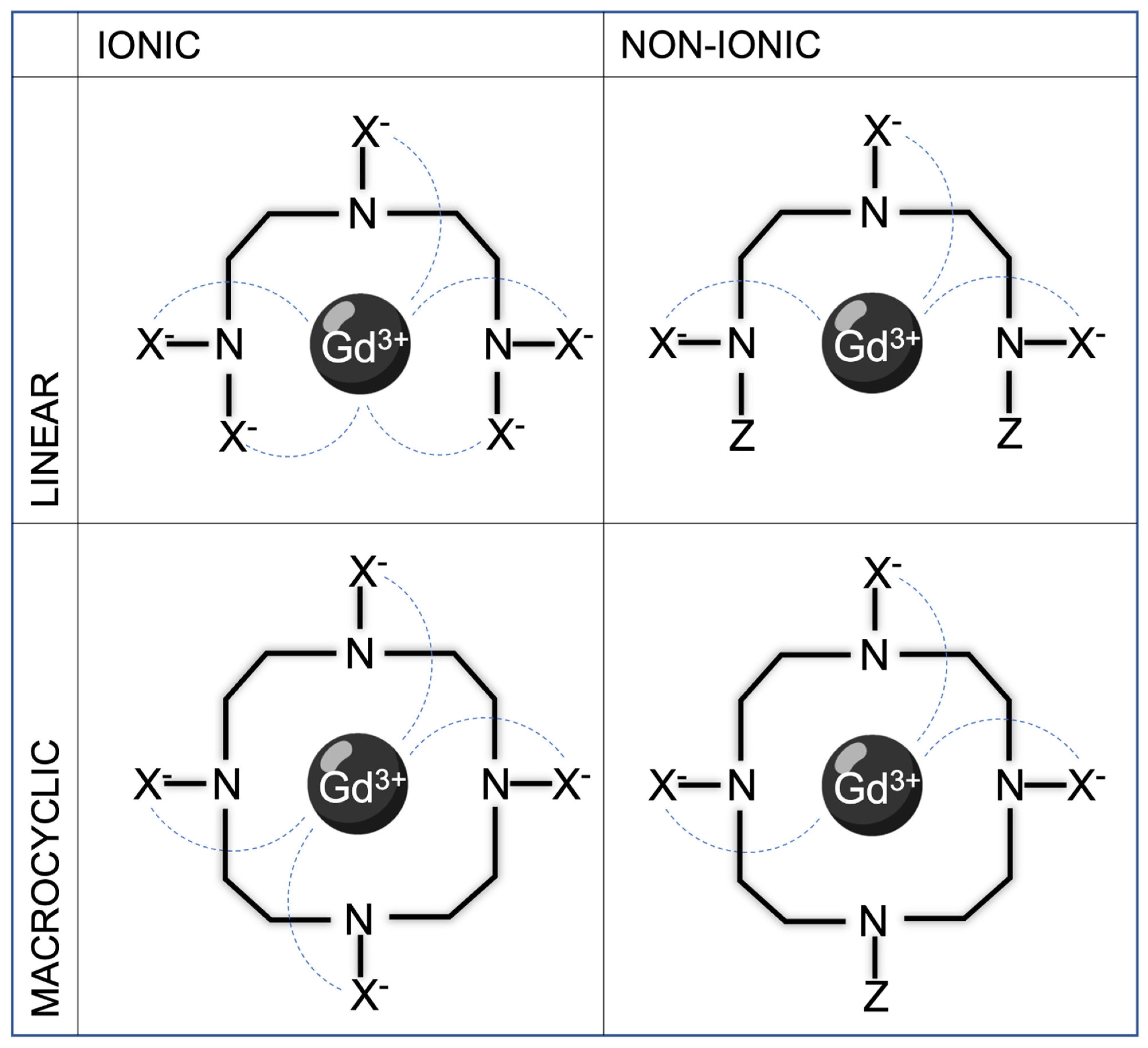
2. Gadolinium and Gadolinium-Based Contrast Media: Key Concepts
- Extracellular space agents (ECSAs): This category includes agents rapidly distributing within the extracellular space (vascular space plus interstitial space); these molecules are quickly eliminated by the kidneys (about 100% renal excretion). ECSAs are widely used for thoracic, abdominal, and/or pelvic MRI studies. This category encompasses molecules such as gadoterate meglumine, gadobutrol, gadopentetate dimeglumine, gadodiamide, gadoversetamide, gadoteridol, and gadopiclenol.
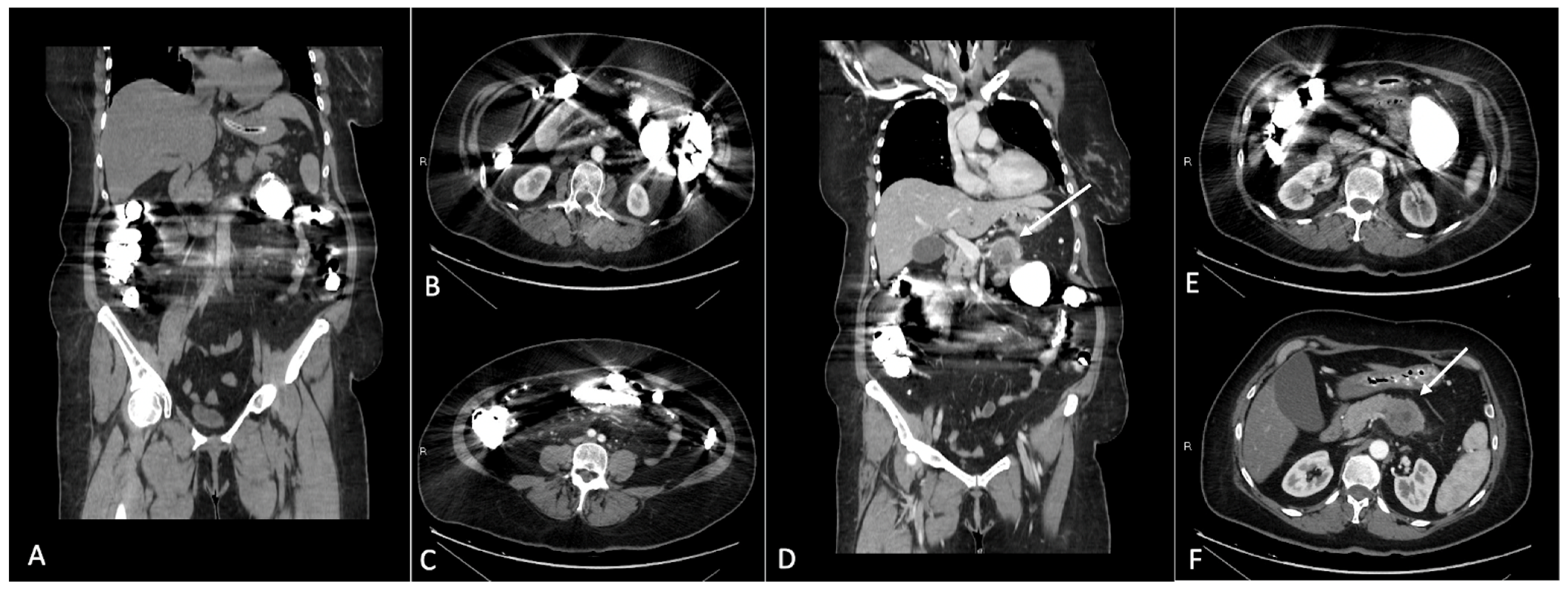
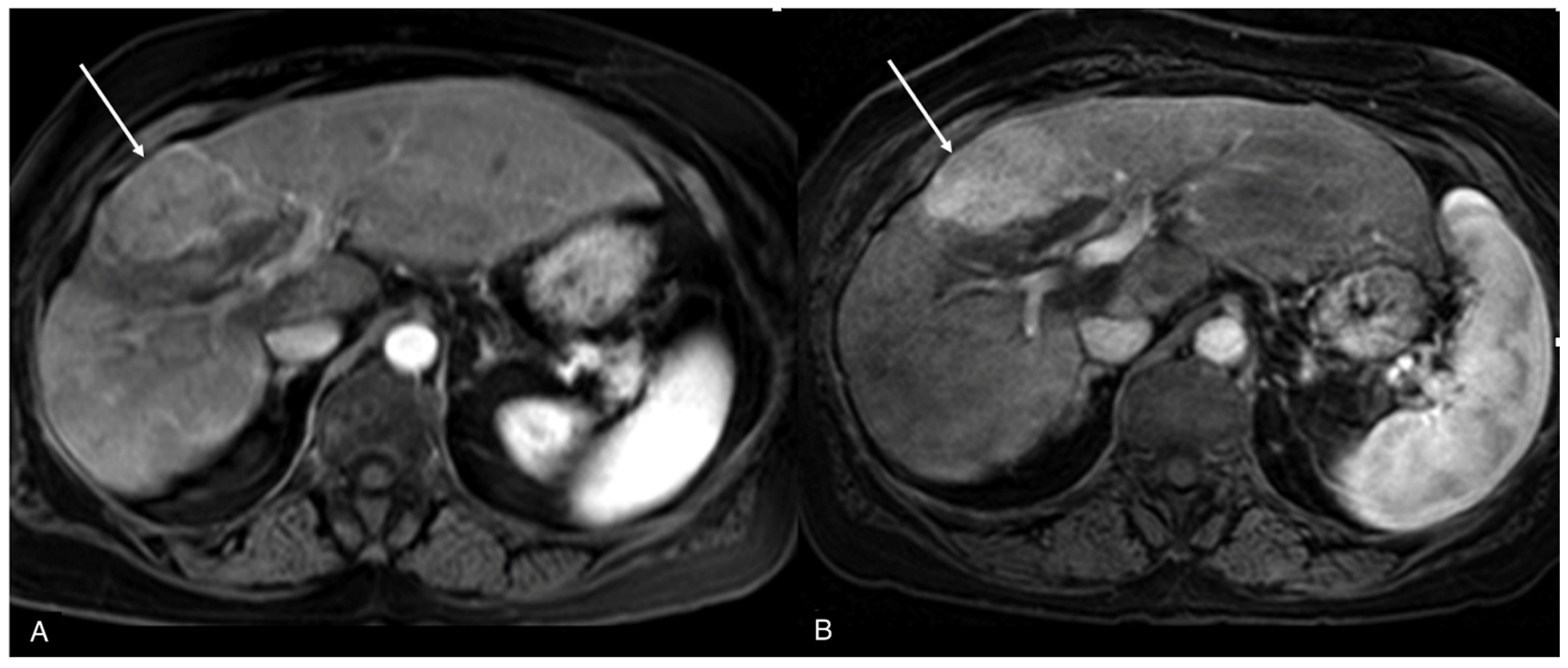
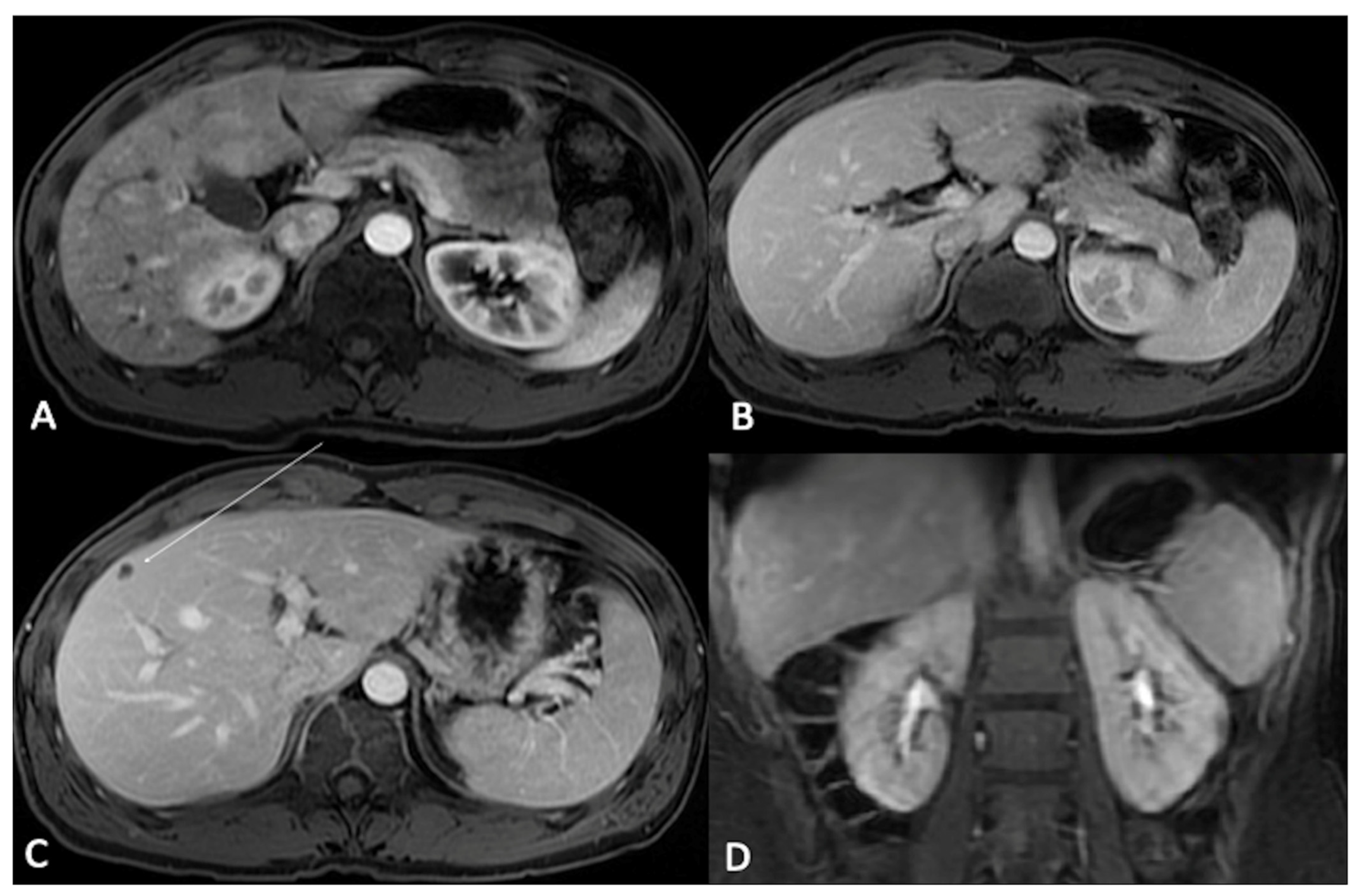
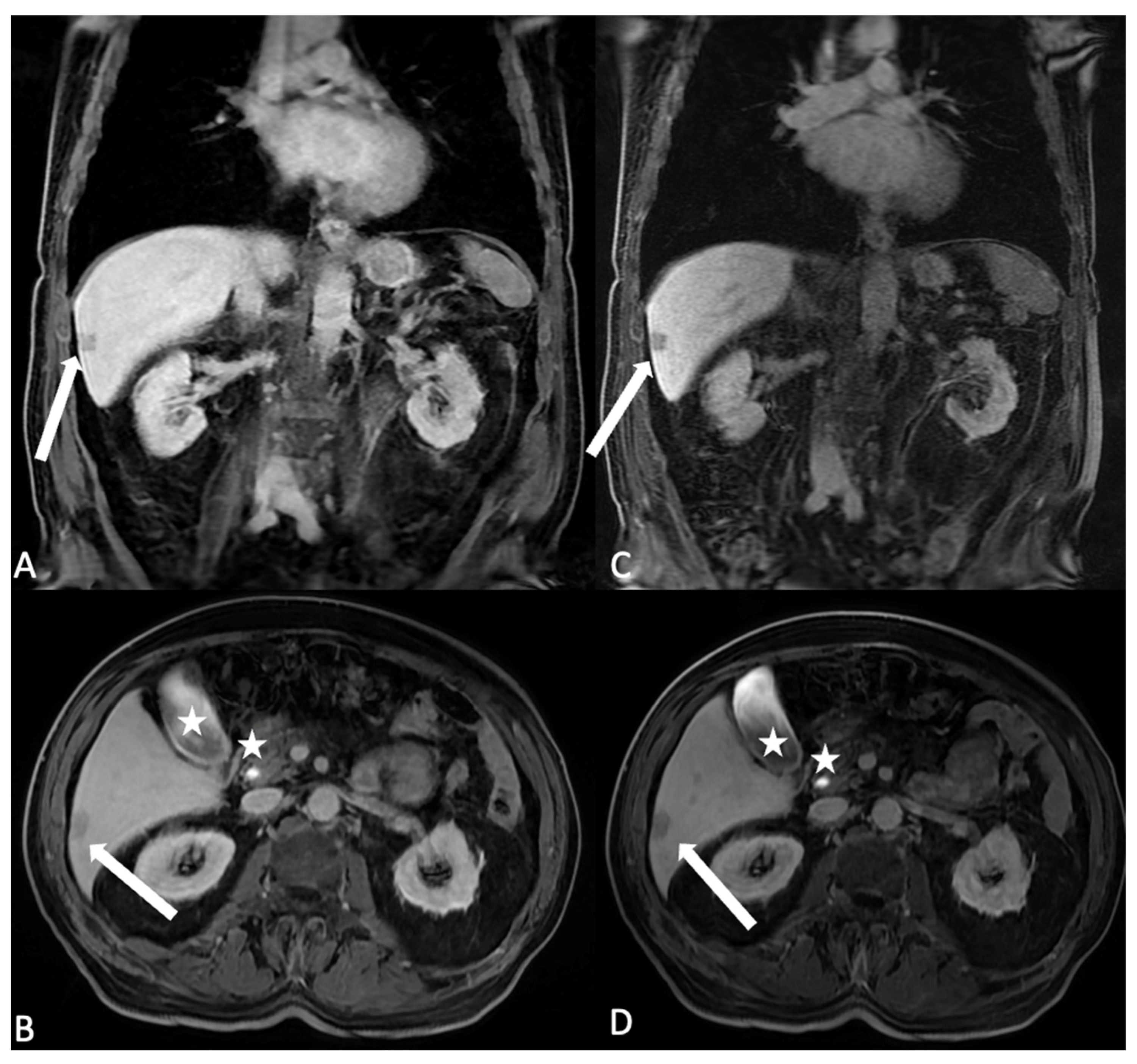
- Hepatocyte-specific contrast agents (HSCAs): Only two molecules are commercially available in this class (gadoxetate disodium and gadobenate dimeglumine); once intravenously injected, they undergo hepatocytes uptake. Their elimination is a combination of biliary and renal clearance (in particular, 50% of godoxetate disodium is excreted in the biliary system, thus with a shorter hepatocellular imaging window occurring approximately 20 min after injection and with a shorter total acquisition time compared to gadobenate dimeglumine of which just 5% is excreted in the biliary system). Due to their properties, HSCAs are mainly used for characterizing focal liver lesions, especially in chronic hepatopathies; off-label indications include bile duct imaging (both pre- or post-surgical or post-traumatic), gallbladder evaluation, and cystic duct obstructions [11,12,13].
- Blood-pool agents (BPAs): The only GBCA in this category is gadofosveset trisodium, which was discontinued after commercialization due to marketing reasons [14]; this contrast agent temporarily binds albumin, allowing the molecule to persist longer in the blood flow providing an almost selective vascular phase for up to 1 h from injection. This allows for a high-resolution three-dimensional MR angiography and MR venography; this GBCA has approximately five times the relaxivity of ECSA, which allows the first pass MR angiography to be performed with similar image quality as ECSAs but with a lower dose. Indications encompass aortoiliac occlusive disease, abdominal aortic aneurysm or dissection, pulmonary embolism, and vein thrombosis [15].
3. Gadolinium-Based Contrast Media Optimization
3.1. Dose and Concentration
3.2. Choice and Timing of Post-Contrast MRI Sequences
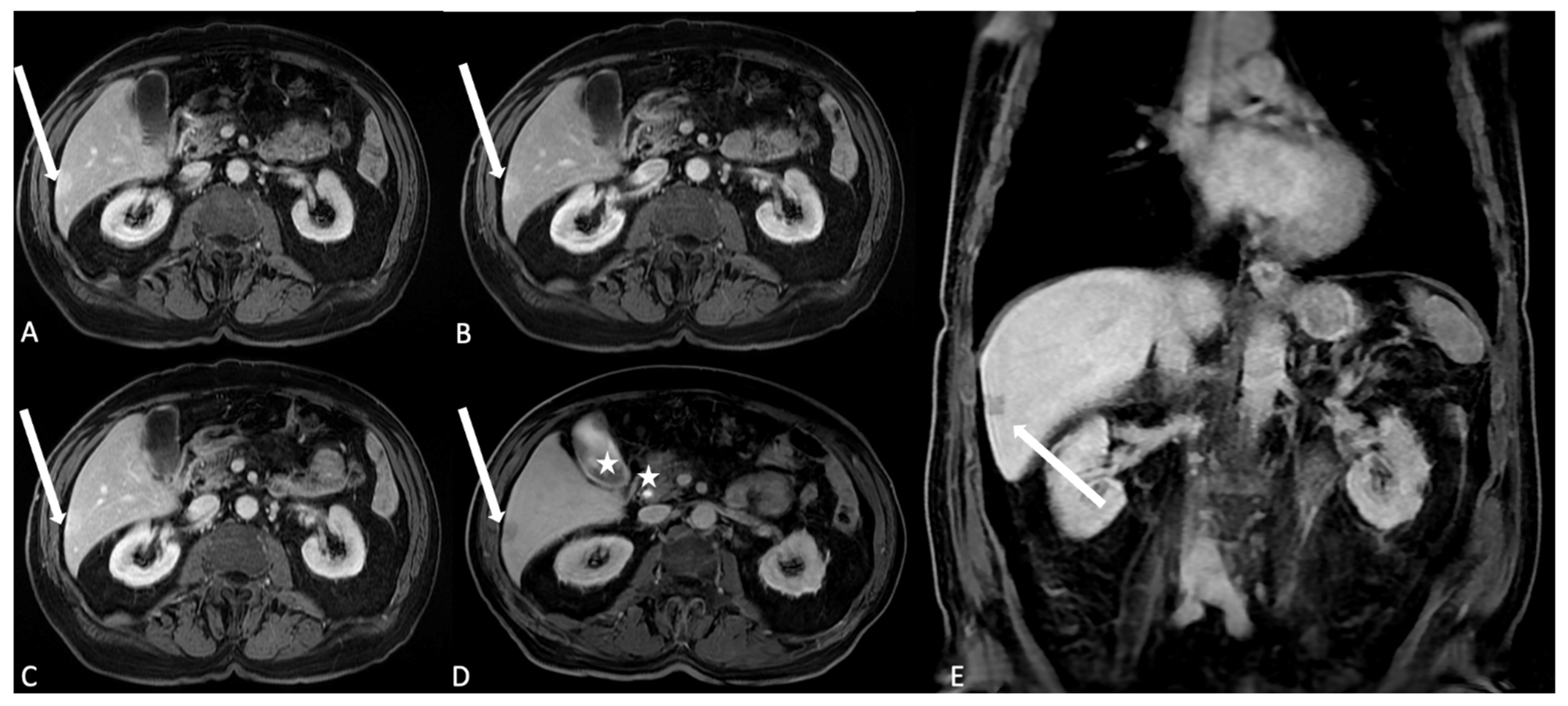
- When using ECSAs, in the early arterial phase, arterial structures are enhanced, while in the late arterial phase, hypervascular tissues (including normal parenchymas such as the pancreas, spleen, or renal cortex) are visible. The venous phase allows for the best liver enhancement. In the delayed/equilibrium phase (occurring between 3 and 5 min from contrast injection), interstitial and extracellular spaces are finally enhanced (Figure 4).
- When using BPAs, despite at present being withdrawn from the market, BPAs presented with a first-pass angiographic phase like ESCAs but offered a very long steady-state phase (up to 1 h from injection) to accurately depict blood vessels; timing should, however, be tuned according to the specific clinical indication for MRI examination (arteries vs. veins imaging).
- Pulse sequences that may benefit from previous GBCA injection:
- −
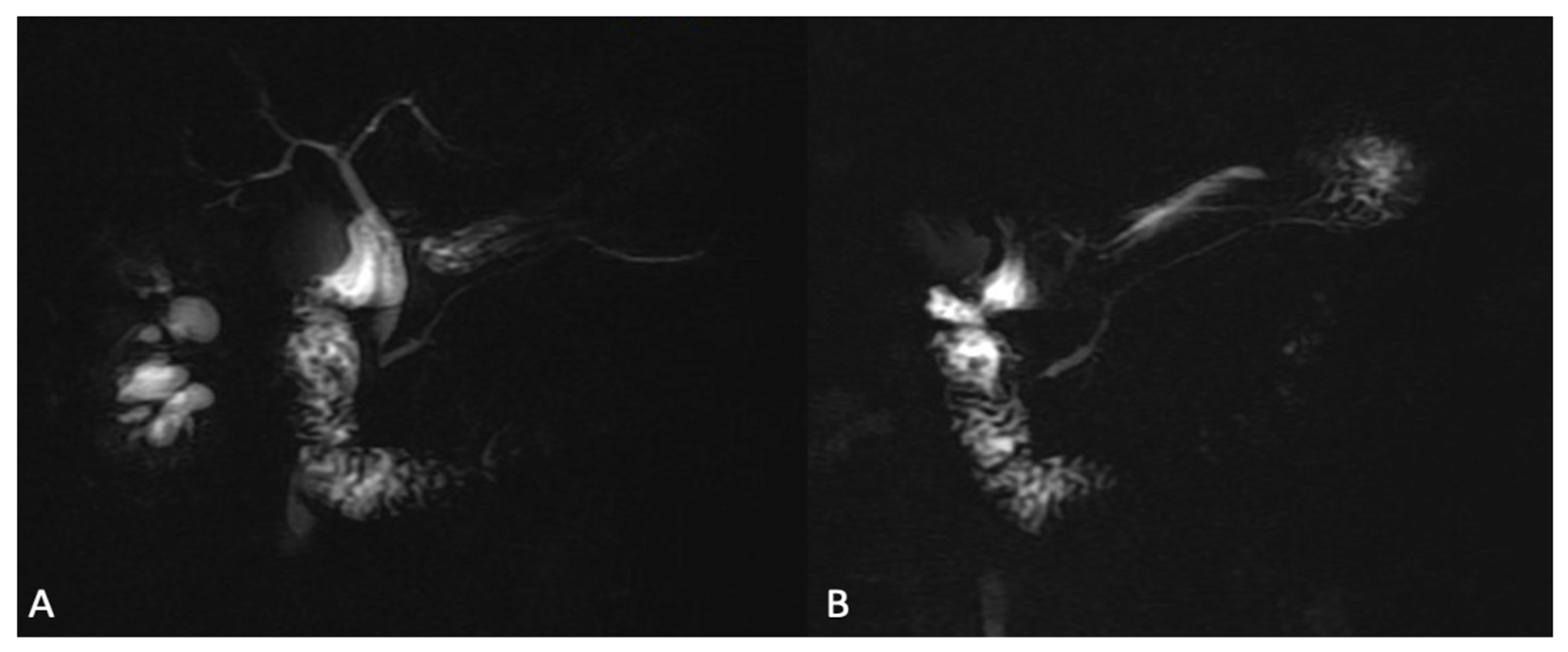
- Two-dimensional radial slab MR cholangiopancreatography after ECSA, as gadolinium reduces the signal intensity of the kidneys and renal collecting systems, which may improve the visualization of the biliary tract and pancreatic ducts (Figure 7);
- −
- Short tau inversion recovery (STIR) after gadoxetate disodium, as contrast-induced T1 shortening of hepatic parenchyma causes suppression of background liver signal, accentuating contrast between normal liver and focal hepatic lesions;
- −
- Moderately T2-weighted fat-suppressed (reducing signal of kidneys and urinary system, and slightly reducing signal of other abdominal organs);
- −
- 2D GRE series (increased signal intensity of blood vessels).
- Pulse sequences not significantly influenced by GBCA injection:
- −
- Balanced steady-state free-precession (Figure 8);
- −
- Diffusion-weighted images (paying attention to possible susceptibility artifacts from gadolinium in the urinary system).
- Pulse sequences negatively influenced by GBCA injection:
- −
- Dual GRE in-phase and out-of-phase (interferes with the evaluation of fatty liver or fat-containing lesions);
- −
- Two-dimensional radial slab MR cholangiopancreatography/high-resolution 3D MR cholangiopancreatography after HSCAs (the biliary excretion may darken the bile ducts and degrade biliary duct visualization, potentially rendering these images nondiagnostic);
- −
- STIR images after ECSA administration;
- −
- Single-shot fast-spin echo (SSFSE) heavily T2-weighted sequences (interference due to the T2 shortening effect of GBCA).
4. GBCA-Related Adverse Reactions and Secondary Effects
4.1. Local Undesired Events: Injection Site Reactions and GBCAs Extravasation
4.2. Systemic Adverse Events: Acute and Late Reactions
4.3. Nephrogenic Systemic Fibrosis
4.4. Accumulation in Human Tissues
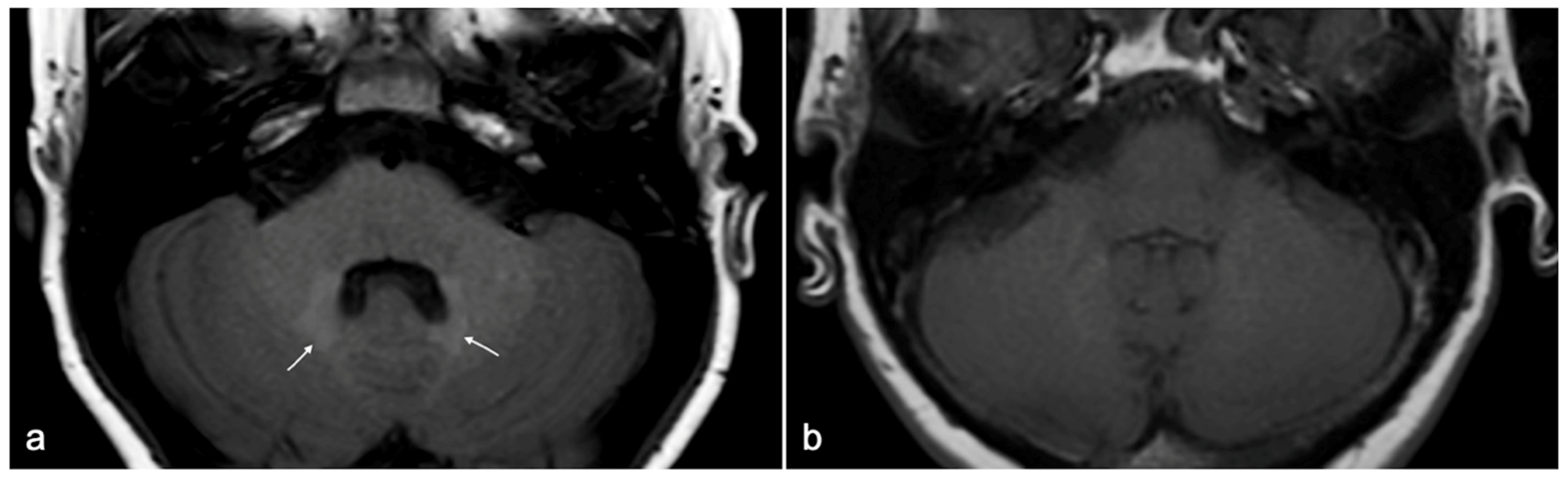
5. Gadolinium-Based Contrast Agents and at-Risk Categories
5.1. GBCAs and Dialyzed Patients
5.2. GBCAs and Patients with Sickle Cell Disease
5.3. GBCAs and Interaction with Other Drugs
5.4. GBCAs during Pregnancy
5.5. GBCAs in Women Who Are Breast-Feeding
6. GBCAs in Children
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rogosnitzky, M.; Branch, S. Gadolinium-based contrast agent toxicity: A review of known and proposed mechanisms. Biometals 2016, 29, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Davies, J.; Siebenhandl-Wolff, P.; Tranquart, F.; Jones, P.; Evans, P. Gadolinium: Pharmacokinetics and toxicity in humans and laboratory animals following contrast agent administration. Arch. Toxicol. 2022, 96, 403–429. [Google Scholar] [CrossRef] [PubMed]
- Caravan, P.; Farrar, C.T.; Frullano, L.; Uppal, R. Influence of molecular parameters and increasing magnetic field strength on relaxivity of gadolinium- and manganese-based T 1 contrast agents. Radiology 2016, 34, 89–100. [Google Scholar] [CrossRef] [PubMed]
- Robic, C.; Port, M.; Rousseaux, O.; Louguet, S.; Fretellier, N.; Catoen, S.; Factor, C.; Le Greneur, S.; Medina, C.; Bourrinet, P.; et al. Physicochemical and Pharmacokinetic Profiles of Gadopiclenol: A New Macrocyclic Gadolinium Chelate with High T1 Relaxivity. Investig. Radiol. 2019, 54, 475–484. [Google Scholar] [CrossRef] [PubMed]
- Rohrer, M.; Bauer, H.; Mintorovitch, J.; Requardt, M.; Weinmann, H.-J. Comparison of Magnetic Properties of MRI Contrast Media Solutions at Different Magnetic Field Strengths. Investig. Radiol. 2005, 40, 715–724. [Google Scholar] [CrossRef] [PubMed]
- Elster, A.D. How much contrast is enough? Dependence of enhancement on field strength and MR pulse sequence. Eur. Radiol. 1997, 7, S276–S280. [Google Scholar] [CrossRef] [PubMed]
- Rinck, P.A.; Muller, R.N. Field strength and dose dependence of contrast enhancement by gadolinium-based MR contrast agents. Eur. Radiol. 1999, 9, 998–1004. [Google Scholar] [CrossRef]
- Chang, K.J.; Kamel, I.R.; Macura, K.J.; Bluemke, D.A. 3.0-T MR Imaging of the Abdomen: Comparison with 1.5 T. Radiographics 2008, 28, 1983–1998. [Google Scholar] [CrossRef]
- Endler, C.H.-J.; Kukuk, G.M.; Peeters, J.M.; Beck, G.M.; Isaak, A.; Faron, A.; Mesropyan, N.; Luetkens, J.A.; Attenberger, U.I.; Kupczyk, P.A. Dynamic Liver Magnetic Resonance Imaging During Free Breathing. Investig. Radiol. 2022, 57, 470–477. [Google Scholar] [CrossRef]
- Laurent, S.; Elst, L.V.; Muller, R.N. Comparative study of the physicochemical properties of six clinical low molecular weight gadolinium contrast agents. Contrast Media Mol. Imaging 2006, 1, 128–137. [Google Scholar] [CrossRef]
- Seale, M.K.; Catalano, O.A.; Saini, S.; Hahn, P.F.; Sahani, D.V. Hepatobiliary-specific MR Contrast Agents: Role in Imaging the Liver and Biliary Tree. Radiographics 2009, 29, 1725–1748. [Google Scholar] [CrossRef] [PubMed]
- Iacobellis, F.; Di Serafino, M.; Brillantino, A.; Mottola, A.; Del Giudice, S.; Stavolo, C.; Festa, P.; Patlas, M.N.; Scaglione, M.; Romano, L. Role of MRI in early follow-up of patients with solid organ injuries: How and why we do it? Radiol. Med. 2021, 126, 1328–1334. [Google Scholar] [CrossRef] [PubMed]
- Di Serafino, M.; Iacobellis, F.; Ronza, R.; Martino, A.; Grimaldi, D.; Rinaldo, C.; Caruso, M.; Orabona, G.D.; Barbuto, L.; Verde, F.; et al. Hepatobiliary-specific magnetic resonance contrast agents: Role in biliary trauma. Gland Surg. 2023, 12, 1425–1433. [Google Scholar] [CrossRef] [PubMed]
- Gadofosveset Trisodium. Reference Article, Radiopaedia.org. 2024. Available online: https://radiopaedia.org/articles/mri-contrast-agents (accessed on 9 March 2024).
- Oliveira, I.S.; Hedgire, S.S.; Li, W.; Ganguli, S.; Prabhakar, A.M. Blood pool contrast agents for venous magnetic resonance imaging. Cardiovasc. Diagn. Ther. 2016, 6, 508–518. [Google Scholar] [CrossRef] [PubMed]
- Baroni, R.H.; Bauab, T.; Bittencourt, L.K.; D’ippolito, G.; Goldman, S.M.; Hohgraefe Neto, G.; Manzella, A.; Rocha, A.J.; Sonoda, L.A.; Takeda, F.S. Practical recommendations for the safe use of gadolinium in magnetic resonance imaging: A delphi expert panel study. Radiol. Bras. 2020, 53, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Scott, L.J. Gadobutrol: A Review in Contrast-Enhanced MRI and MRA. Clin. Drug Investig. 2018, 38, 773–784. [Google Scholar] [CrossRef] [PubMed]
- Loevner, L.A.; Kolumban, B.; Hutóczki, G.; Dziadziuszko, K.; Bereczki, D.; Bago, A.; Pichiecchio, A. Efficacy and Safety of Gadopiclenol for Contrast-Enhanced MRI of the Central Nervous System. Investig. Radiol. 2023, 58, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Bendszus, M.; Roberts, D.; Kolumban, B.; Meza, J.A.; Bereczki, D.; San-Juan, D.; Liu, B.P.; Anzalone, N.; Maravilla, K. Dose Finding Study of Gadopiclenol, a New Macrocyclic Contrast Agent, in MRI of Central Nervous System. Investig. Radiol. 2020, 55, 129–137. [Google Scholar] [CrossRef]
- Jurkiewicz, E.; Tsvetkova, S.; Grinberg, A.; Pasquiers, B. Pharmacokinetics, Safety, and Efficacy of Gadopiclenol in Pediatric Patients Aged 2 to 17 Years. Investig. Radiol. 2022, 57, 510–516. [Google Scholar] [CrossRef]
- Hadizadeh, D.R.; Gieseke, J.; Lohmaier, S.H.; Wilhelm, K.; Boschewitz, J.; Verrel, F.; Schild, H.H.; Willinek, W.A. Peripheral MR angiography with blood pool contrast agent: Prospective intraindividual comparative study of high-spatial-resolution steady-state MR angiography versus standard-resolution first-pass MR angiography and DSA. Radiology 2008, 249, 701–711. [Google Scholar] [CrossRef][Green Version]
- Gandhi, S.N.; Brown, M.A.; Wong, J.G.; Aguirre, D.A.; Sirlin, C.B. MR Contrast Agents for Liver Imaging: What, When, How. Radiographics 2006, 26, 1621–1636. [Google Scholar] [CrossRef] [PubMed]
- Guglielmo, F.F.; Mitchell, D.G.; Gupta, S. Gadolinium contrast agent selection and optimal use for body MR imaging. Radiol. Clin. N. Am. 2014, 52, 637–656. [Google Scholar] [CrossRef] [PubMed]
- Iacobellis, F.; Reginelli, A.; Berritto, D.; Gagliardi, G.; Laporta, A.; Brillantino, A.; Renzi, A.; Scaglione, M.; Masselli, G.; Barile, A.; et al. Pelvic floor dysfunctions: How to image patients? Jpn. J. Radiol. 2020, 38, 47–63. [Google Scholar] [CrossRef] [PubMed]
- Di Serafino, M.; Pucci, L.; Iacobellis, F.; Fasbender Jacobitti, M.; Ronza, R.; Sabatino, V.; De Luca, L.; Iossa, V.; Langella, N.A.; Persico, F.; et al. MRI-Cavernosography: A New Diagnostic Tool for Erectile Dysfunction Due to Venous Leakage: A Diagnostic Chance. Diagnostics 2023, 13, 2178. [Google Scholar] [CrossRef]
- Odedra, D.; Scaglione, M.; Basilico, R.; Patlas, M.N. Magnetic resonance imaging in abdominal trauma—More relevant than ever. Can. Assoc. Radiol. J. 2022, 73, 612–613. [Google Scholar] [CrossRef] [PubMed]
- Iacobellis, F.; Di Serafino, M.; Caruso, M.; Dell’Aversano Orabona, G.; Rinaldo, C.; Grimaldi, D.; Verde, F.; Sabatino, V.; Schillirò, M.L.; Giacobbe, G.; et al. Non-Operative Management of Polytraumatized Patients: Body Imaging beyond CT. Diagnostics 2023, 13, 1347. [Google Scholar] [CrossRef] [PubMed]
- Costello, J.R.; Kalb, B.; Martin, D.R. Incidence and risk factors for gadolinium-based contrast agent immediate reactions. Top. Magn. Reson. Imaging 2016, 25, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Gracia Bara, M.T.; Gallardo-Higueras, A.; Moreno, E.M.; Laffond, E.; Muñoz Bellido, F.J.; Martin, C.; Sobrino, M.; Macias, E.; Arriba-Méndez, S.; Castillo, R.; et al. Hypersensitivity to Gadolinium-Based Contrast Media. Front. Allergy 2022, 3, 813927. [Google Scholar] [CrossRef] [PubMed]
- Prince, M.R.; Zhang, H.; Zou, Z.; Staron, R.B.; Brill, P.W. Incidence of immediate gadolinium contrast media reactions. Am. J. Roentgenol. 2011, 196, 138–143. [Google Scholar] [CrossRef]
- Xiao, Y.D.; Paudel, R.; Liu, J.; Ma, C.; Zhang, Z.S.; Zhou, S.K. MRI contrast agents: Classification and application (Review). Int. J. Mol. Med. 2016, 38, 1319–1326. [Google Scholar] [CrossRef]
- Ramalho, J.; Semelka, R.C.; Ramalho, M.; Nunes, R.H.; AlObaidy, M.; Castillo, M. Gadolinium-based contrast agent accumulation and toxicity: An update. Am. J. Neuroradiol. 2016, 37, 1192–1198. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, H.S.; Webb, J. The Lalli and Weber effects and the incidence of acute non-renal adverse reactions to contrast media. Acta Radiol. 2012, 53, 953–954. [Google Scholar] [CrossRef] [PubMed]
- Granata, V.; Cascella, M.; Fusco, R.; Dell’Aprovitola, N.; Catalano, O.; Filice, S.; Schiavone, V.; Izzo, F.; Cuomo, A.; Petrillo, A. Immediate adverse reactions to gadolinium-based MR contrast media: A retrospective analysis on 10,608 examinations. Biomed. Res. Int. 2016, 2016, 3918292. [Google Scholar] [CrossRef] [PubMed]
- Shaqdan, K.; Aran, S.; Thrall, J.; Abujudeh, H. Incidence of contrast medium extravasation for CT and MRI in a large academic medical centre: A report on 502,391 injections. Clin. Radiol. 2014, 69, 1264–1272. [Google Scholar] [CrossRef] [PubMed]
- Heshmatzadeh Behzadi, A.; Farooq, Z.; Newhouse, J.H.; Prince, M.R. MRI and CT contrast media extravasation: A systematic review. Medicine 2018, 97, e0055. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.T.; Park, J.Y.; Lee, H.J.; Cheon, Y.J. Guidelines for the management of extravasation. J. Educ. Eval. Health Prof. 2020, 17, 21. [Google Scholar] [CrossRef] [PubMed]
- Roditi, G.; Khan, N.; van der Molen, A.J.; Bellin, M.-F.; Bertolotto, M.; Brismar, T.; Correas, J.-M.; Dekkers, I.A.; Geenen, R.W.F.; Heinz-Peer, G.; et al. Intravenous contrast medium extravasation: Systematic review and updated ESUR Contrast Media Safety Committee Guidelines. Eur. Radiol. 2022, 32, 3056–3066. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.W.; Kang, H.R.; Kim, M.H.; Lee, W.; Min, K.U.; Han, M.H.; Cho, S.H. Immediate hypersensitivity reaction to gadolinium-based MR contrast media. Radiology 2012, 264, 414–422. [Google Scholar] [CrossRef] [PubMed]
- Forghani, R. Adverse Effects of Gadolinium-Based Contrast Agents: Changes in Practice Patterns. Top. Magn. Reson. Imaging 2016, 25, 163–169. [Google Scholar] [CrossRef]
- Contrast Media Safety Committee. ESUR Guidelines on Contrast Agents v10.0; European Society of Urogenital Radiology: Vienna, Austria, 2018; pp. 1–45. [Google Scholar]
- ACR Committee on Drugs and Contrast Media. ACR Manual on Contrast Media; ACR Headquarters Office: Reston, VA, USA, 2013; Volume 105, ISBN 9781559030502. [Google Scholar]
- Neeman, Z.; abu Ata, M.; Touma, E.; Saliba, W.; Barnett-Griness, O.; Gralnek, I.M.; Rock, W.; Bisharat, N. Is fasting still necessary prior to contrast-enhanced computed tomography? A randomized clinical study. Eur. Radiol. 2021, 31, 1451–1459. [Google Scholar] [CrossRef]
- Kaewlai, R.; Abujudeh, H. Nephrogenic systemic fibrosis. Am. J. Roentgenol. 2012, 199, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Wertman, R.; Altun, E.; Martin, D.R.; Mitchell, D.G.; Leyendecker, J.R.; O’Malley, R.B.; Parsons, D.J.; Fuller, E.R.; Semelka, R.C. Risk of nephrogenic systemic fibrosis: Evaluation of gadolinium chelate contrast agents at four american universities. Radiology 2008, 248, 799–806. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, H.S. Nephrogenic Systemic Fibrosis: History and Epidemiology. Radiol. Clin. N. Am. 2009, 47, 827–831. [Google Scholar] [CrossRef] [PubMed]
- Khawaja, A.Z.; Cassidy, D.B.; Al Shakarchi, J.; McGrogan, D.G.; Inston, N.G.; Jones, R.G. Revisiting the risks of MRI with Gadolinium based contrast agents—Review of literature and guidelines. Insights Imaging 2015, 6, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Weinreb, J.C.; Rodby, R.A.; Yee, J.; Wang, C.L.; Fine, D.; McDonald, R.J.; Perazella, M.A.; Dillman, J.R.; Davenport, M.S. Use of intravenous gadolinium-based contrast media in patients with kidney disease: Consensus statements from the American college of radiology and the national kidney foundation. Radiology 2021, 298, 28–35. [Google Scholar] [CrossRef]
- Schieda, N.; Blaichman, J.I.; Costa, A.F.; Glikstein, R.; Hurrell, C.; James, M.; Jabehdar Maralani, P.; Shabana, W.; Tang, A.; Tsampalieros, A.; et al. Gadolinium-Based Contrast Agents in Kidney Disease: Comprehensive Review and Clinical Practice Guideline Issued by the Canadian Association of Radiologists. Can. Assoc. Radiol. J. 2018, 69, 136–150. [Google Scholar] [CrossRef] [PubMed]
- Dekkers, I.A.; Roos, R.; van der Molen, A.J. Gadolinium retention after administration of contrast agents based on linear chelators and the recommendations of the European Medicines Agency. Eur. Radiol. 2018, 28, 1579–1584. [Google Scholar] [CrossRef] [PubMed]
- Radbruch, A. Are some agents less likely to deposit gadolinium in the brain? Magn. Reson. Imaging 2016, 34, 1351–1354. [Google Scholar] [CrossRef] [PubMed]
- Quattrocchi, C.C.; Van Der Molen, A.J. Gadolinium retention in the body and brain: Is it time for an international joint research effort? Radiology 2017, 282, 12–16. [Google Scholar] [CrossRef]
- Cheong, B.Y.C.; Wilson, J.M.; Preventza, O.A.; Muthupillai, R. Gadolinium-Based Contrast Agents: Updates and Answers to Typical Questions Regarding Gadolinium Use. Tex. Hear. Inst. J. 2022, 49, e217680. [Google Scholar] [CrossRef]
- Murata, N.; Murata, K.; Gonzalez-Cuyar, L.F.; Maravilla, K.R. Gadolinium tissue deposition in brain and bone. Magn. Reson. Imaging 2016, 34, 1359–1365. [Google Scholar] [CrossRef] [PubMed]
- Tedeschi, E.; Caranci, F.; Giordano, F.; Angelini, V.; Cocozza, S.; Brunetti, A. Gadolinium retention in the body: What we know and what we can do. Radiol. Med. 2017, 122, 589–600. [Google Scholar] [CrossRef] [PubMed]
- Kanda, T.; Nakai, Y.; Oba, H.; Toyoda, K.; Kitajima, K.; Furui, S. Gadolinium deposition in the brain. Magn. Reson. Imaging 2016, 34, 1346–1350. [Google Scholar] [CrossRef] [PubMed]
- McDonald, R.J.; McDonald, J.S.; Kallmes, D.F.; Jentoft, M.E.; Murray, D.L.; Thielen, K.R.; Williamson, E.E.; Eckel, L.J. Intracranial Gadolinium Deposition after Contrast-enhanced MR Imaging. Radiology 2015, 275, 772–782. [Google Scholar] [CrossRef] [PubMed]
- Gulani, V.; Calamante, F.; Shellock, F.G.; Kanal, E.; Reeder, S.B. Gadolinium deposition in the brain: Summary of evidence and recommendations. Lancet Neurol. 2017, 16, 564–570. [Google Scholar] [CrossRef]
- Cocozza, S.; Pontillo, G.; Lanzillo, R.; Russo, C.; Petracca, M.; Di Stasi, M.; Paolella, C.; Vola, E.A.; Criscuolo, C.; Moccia, M.; et al. MRI features suggestive of gadolinium retention do not correlate with Expanded Disability Status Scale worsening in Multiple Sclerosis. Neuroradiology 2019, 61, 155–162. [Google Scholar] [CrossRef]
- Scaravilli, A.; Tranfa, M.; Pontillo, G.; Falco, F.; Criscuolo, C.; Moccia, M.; Monti, S.; Lanzillo, R.; Brescia Morra, V.; Palma, G.; et al. MR Imaging Signs of Gadolinium Retention Are Not Associated with Long-Term Motor and Cognitive Outcomes in Multiple Sclerosis. Am. J. Neuroradiol. 2023, 44, 396–402. [Google Scholar] [CrossRef] [PubMed]
- Ayers-Ringler, J.; McDonald, J.S.; Connors, M.A.; Fisher, C.R.; Han, S.; Jakaitis, D.R.; Scherer, B.; Tutor, G.; Wininger, K.M.; Dai, D.; et al. Neurologic Effects of Gadolinium Retention in the Brain after Gadolinium-based Contrast Agent Administration. Radiology 2022, 302, 676–683. [Google Scholar] [CrossRef] [PubMed]
- Okada, S.; Katagiri, K.; Kumazaki, T.; Yokoyama, H. Safety of gadolinium contrast agent in hemodialysis patients. Acta Radiol. 2001, 42, 339–341. [Google Scholar] [CrossRef]
- Yee, J. Prophylactic Hemodialysis for Protection Against Gadolinium-Induced Nephrogenic Systemic Fibrosis: A Doll’s House. Adv. Chronic Kidney Dis. 2017, 24, 133–135. [Google Scholar] [CrossRef]
- Dillman, J.R.; Ellis, J.H.; Cohan, R.H.; Caoili, E.M.; Hussain, H.K.; Campbell, A.D.; Strouse, P.J. Safety of gadolinium-based contrast material in sickle cell disease. J. Magn. Reson. Imaging 2011, 34, 917–920. [Google Scholar] [CrossRef]
- Zimmerman, R.A. MRI/MRA evaluation of sickle cell disease of the brain. Pediatr. Radiol. 2005, 35, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Westwood, M.A.; Shah, F.; Anderson, L.J.; Strange, J.W.; Tanner, M.A.; Maceira, A.M.; Howard, J.; Porter, J.B.; Walker, J.M.; Wonke, B.; et al. Myocardial tissue characterization and the role of chronic anemia in sickle cell cardiomyopathy. J. Magn. Reson. Imaging 2007, 26, 564–568. [Google Scholar] [CrossRef]
- Morcos, S.K.; Thomsen, H.S.; Exley, C.M.; Almén, T.; Aspelin, P.; Bellin, M.F.; Flaten, H.; Jakobsen, J.Å.; Löwe, A.; Oyen, R.; et al. Contrast media: Interactions with other drugs and clinical tests. Eur. Radiol. 2005, 15, 1463–1468. [Google Scholar] [CrossRef] [PubMed]
- Panigel, M.; Wolf, G.; Zeleznick, A. Magnetic resonance imaging of the placenta in rhesus monkeys, Macaca mulatta. J. Med. Primatol. 1988, 17, 3–18. [Google Scholar] [CrossRef] [PubMed]
- Ray, J.G.; Vermeulen, M.J.; Bharatha, A.; Montanera, W.J.; Park, A.L. Association between MRI exposure during pregnancy and fetal and childhood outcomes. JAMA—J. Am. Med. Assoc. 2016, 316, 952–961. [Google Scholar] [CrossRef]
- Bird, S.T.; Gelperin, K.; Sahin, L.; Bleich, K.B.; Fazio-Eynullayeva, E.; Woods, C.; Radden, E.; Greene, P.; McCloskey, C.; Johnson, T.; et al. First-trimester exposure to gadolinium-based contrast agents: A utilization study of 4.6 Million U.S. Pregnancies. Radiology 2019, 293, 193–200. [Google Scholar] [CrossRef]
- Sachs, H.C. The transfer of drugs and therapeutics into human breast milk: An update on selected topics. Pediatrics 2013, 132, e796–e809. [Google Scholar] [CrossRef]
- McDonald, J.S.; Larson, N.B.; Kolbe, A.B.; Hunt, C.H.; Schmitz, J.J.; Kallmes, D.F.; McDonald, R.J. Acute Reactions to Gadolinium-Based Contrast Agents in a Pediatric Cohort: A Retrospective Study of 16,237 Injections. Am. J. Roentgenol. 2021, 216, 1363–1369. [Google Scholar] [CrossRef]
- Rozenfeld, M.N.; Podberesky, D.J. Gadolinium-based contrast agents in children. Pediatr. Radiol. 2018, 48, 1188–1196. [Google Scholar] [CrossRef]
- Nardone, B.; Saddleton, E.; Laumann, A.E.; Edwards, B.J.; Raisch, D.W.; McKoy, J.M.; Belknap, S.M.; Bull, C.; Haryani, A.; Cowper, S.E.; et al. Pediatric nephrogenic systemic fibrosis is rarely reported: A RADAR report. Pediatr. Radiol. 2014, 44, 173–180. [Google Scholar] [CrossRef] [PubMed]

| Active Principle | Commercial | Manufacturer | Structure | Charge | Distribution | EMA | FDA |
|---|---|---|---|---|---|---|---|
| Gadoterate meglumine | Dotarem® Clariscan® | Guerbet, Aulnay-sous-Bois, France | Cyclic | Ionic | ECSA | Approved | Approved |
| Gadobutrol | Gadavist® Gadovist® | Bayer, Milano, Italy | Cyclic | Non-Ionic | ECSA | Approved | Approved |
| Gadopentetate dimeglumine | Magnevist® | Bayer Pharma, Leverkusen, Germany | Linear | Ionic | ECSA | Suspended | Approved |
| Gadodiamide | Omniscan® | GE Healthcare, Milano, Italy | Linear | Non-Ionic | ECSA | Suspended | Approved |
| Gadoversetamide | Optimark® | Mallinckrodt Deutschland GmbH, Hennef, Germany | Linear | Non-Ionic | ECSA | Suspended | Approved |
| Gadoteridol | ProHance® | Bracco, Hennef, Germany | Cyclic | Non-Ionic | ECSA | Approved | Approved |
| Gadopiclenol | Vueway® Elucirem® | Bracco, Raleigh, NC, USA | Cyclic | Non-Ionic | ECSA | Approved | Approved |
| Gadoxetate disodium | Eovist® Primovist® | Bayer, Milano, Italy | Linear | Ionic | HSCA | Restricted | Approved |
| Gadobenate diemglumine | MultiHance® | Bracco, Colleretto, Italy | Linear | Ionic | HSCA | Restricted | Approved |
| Gadofosveset trisodium | Ablavar® Vasovist® | Bayer Pharma, Berlin, Germany | Linear | Ionic | BPA | Withdrawn | Withdrawn |
| Type | Active Principle | Commercial | Concentration | Dose mmol/kg | Dose mL/kg | T1 rel | Notes |
|---|---|---|---|---|---|---|---|
| ECSA | Gadoterate meglumine | Dotarem® Clariscan® | 0.5 M | 0.1 | 0.2 | 3.6 | Adults and pediatric patients (including term neonates). |
| Gadobutrol | Gadavist® Gadovist® | 1 M | 0.1 | 0.1 | 5.2 | Adults and pediatric patients (including term neonates). | |
| Gadopentetate dimeglumine | Magnevist® | 0.5 M | 0.1 | 0.2 | 4.1 | Suspended by EMA for intravenous use. According to FDA: adults and pediatric patients (including term neonates). | |
| Gadodiamide | Omniscan® | 0.5 M | 0.1 | 0.2 | 4.3 | Suspended by EMA. According to FDA: adults and pediatric patients aged 2 years and older; for imaging the kidney, halving the dose (0.05 mmol/kg) is recommended. | |
| Gadoversetamide | Optimark® | 0.5 M | 0.1 | 0.2 | 4.7 | Suspended by EMA. According to FDA: contraindicated up to 4w, not recommended up to 2 y of age. | |
| Gadoteridol | ProHance® | 0.5 M | 0.1 | 0.2 | 4.1 | Adults and pediatric patients (including term neonates). According to FDA: supplementary dose (0.2 mmol/kg) may be given up to 30 min after the first dose in adults without renal impairment if poorly visualized CNS lesions or equivocal MR scan. | |
| Gadopiclenol | Vueway® Elucirem® | 0.5 M | 0.05 | 0.1 | 12.8 | Approved by EMA and FDA: adults and pediatric patients aged 2 y and older. | |
| HSCA | Gadoxetate disodium | Eovist® Primovist® | 0.25 M | 0.025 | 0.1 | 6.9 | Not recommended for use in children below 18 y. According to EMA: approved for hepatobiliary imaging only; organ-specific imaging of liver at 0.025 mmol/kg. According to FDA: allowed up to 0.05 mmol/kg, but at present recommended at 0.025 mmol/kg for hepatobiliary imaging only. |
| Gadobenate diemglumine | MultiHance® | 0.5 M | 0.05–0.1 | 0.1 | 6.3 | According to EMA: approved for hepatobiliary imaging only; organ-specific imaging of liver at 0.05 mmol/kg. According to FDA: no restriction (i.e., also indicated for CNS imaging and MR angiography); recommended dose 0.1 mmol/kg in adults and pediatric patients aged 2 y and older; halving the dose in pediatric patients aged less than 2 y. | |
| BPA | Gadofosveset trisodium | Ablavar® Vasovist® | 0.25 M | 0.03 | 0.12 | 19 | Production discontinued due to poor sales. |
| GBCA | ESUR | ACR * |
|---|---|---|
| Gadodiamide, linear (Omniscan®) | High-risk for NSF; suspended by EMA. | Group I: patients’ stratification based on eGFR required, contraindicated if CKD stage 4–5 and AKI. |
| Gadoversetamide, linear (Optimark®) | High-risk for NSF; suspended by EMA. | Group I: patients’ stratification based on eGFR required, contraindicated if CKD stage 4–5 and AKI. |
| Gadopentetic acid, linear (Magnevist®) | High-risk for NSF; suspended by EMA for intravenous use; only allowed for intra-articular administration in arthrography MRI. | Group I: patients’ stratification based on eGFR required, contraindicated if CKD stage 4–5 and AKI. |
| Gadobenic acid, linear (MultiHance®) | Intermediate-risk for NSF; approved by EMA for hepatobiliary imaging only. | Group II: recommended for patients with chronic kidney disease; assessment of renal function optional prior to intravenous administration. |
| Gadoxetic acid, linear (Eovist®, Primovist®) | Intermediate-risk for NSF; approved by EMA for hepatobiliary imaging only. | Group III (data regarding NSF risk remains limited despite an alternative hepatobiliary excretion pathway): patients’ stratification based on eGFR required. |
| Gadobutrol, cyclic (Gadavist®, Gadovist®) | Low-risk for NSF; assessment of renal function not mandatory prior to intravenous administration; caution in patients with eGFR < 30 mL/min (at least 7 days between two injections). | Group II: recommended for patients with chronic kidney disease; assessment of renal function optional prior to intravenous administration. |
| Gadoteridol, cyclic (Prohance®) | Low-risk for NSF; assessment of renal function not mandatory prior to intravenous administration; caution in patients with eGFR < 30 mL/min (at least 7 days between two injections). | Group II: recommended for patients with chronic kidney disease; assessment of renal function optional prior to intravenous administration. |
| Gadoteric acid (Dotarem®, Artirem®, Clariscan®) | Low-risk for NSF; assessment of renal function not mandatory prior to intravenous administration; caution in patients with eGFR < 30 mL/min (at least 7 days between two injections). | Group II: recommended for patients with chronic kidney disease; assessment of renal function optional prior to intravenous administration. |
| ESUR | ACR | |
|---|---|---|
| Pregnant women with preserved renal function | Smallest quantity of macrocyclic GBCAs only; very strong clinical indication to contrast enhanced MRI | Smallest quantity of macrocyclic GBCAs only; very strong clinical indication to contrast enhanced MRI |
| Pregnant women with impaired renal function | GBCAs formally contraindicated | Same safety measures as in non-pregnant women |
| Lactating women with preserved renal function | No breast-feeding interruption formally required | No breast-feeding interruption formally required |
| Lactating women with impaired renal function | GBCAs formally contraindicated | Same safety measures as in non-pregnant women |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iacobellis, F.; Di Serafino, M.; Russo, C.; Ronza, R.; Caruso, M.; Dell’Aversano Orabona, G.; Camillo, C.; Sabatino, V.; Grimaldi, D.; Rinaldo, C.; et al. Safe and Informed Use of Gadolinium-Based Contrast Agent in Body Magnetic Resonance Imaging: Where We Were and Where We Are. J. Clin. Med. 2024, 13, 2193. https://doi.org/10.3390/jcm13082193
Iacobellis F, Di Serafino M, Russo C, Ronza R, Caruso M, Dell’Aversano Orabona G, Camillo C, Sabatino V, Grimaldi D, Rinaldo C, et al. Safe and Informed Use of Gadolinium-Based Contrast Agent in Body Magnetic Resonance Imaging: Where We Were and Where We Are. Journal of Clinical Medicine. 2024; 13(8):2193. https://doi.org/10.3390/jcm13082193
Chicago/Turabian StyleIacobellis, Francesca, Marco Di Serafino, Camilla Russo, Roberto Ronza, Martina Caruso, Giuseppina Dell’Aversano Orabona, Costanza Camillo, Vittorio Sabatino, Dario Grimaldi, Chiara Rinaldo, and et al. 2024. "Safe and Informed Use of Gadolinium-Based Contrast Agent in Body Magnetic Resonance Imaging: Where We Were and Where We Are" Journal of Clinical Medicine 13, no. 8: 2193. https://doi.org/10.3390/jcm13082193
APA StyleIacobellis, F., Di Serafino, M., Russo, C., Ronza, R., Caruso, M., Dell’Aversano Orabona, G., Camillo, C., Sabatino, V., Grimaldi, D., Rinaldo, C., Barbuto, L., Verde, F., Giacobbe, G., Schillirò, M. L., Scarano, E., & Romano, L. (2024). Safe and Informed Use of Gadolinium-Based Contrast Agent in Body Magnetic Resonance Imaging: Where We Were and Where We Are. Journal of Clinical Medicine, 13(8), 2193. https://doi.org/10.3390/jcm13082193






