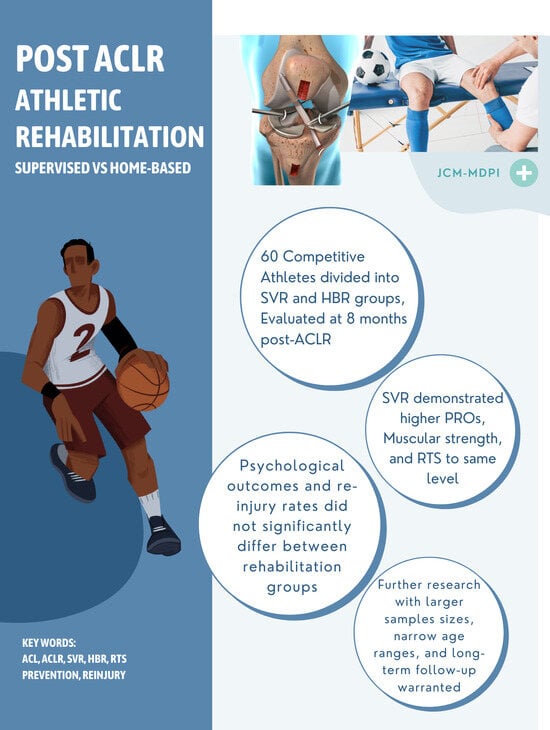
Comparative Effectiveness of Supervised and Home-Based Rehabilitation after Anterior Cruciate Ligament Reconstruction in Competitive Athletes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Patient Enrollment
2.3. Surgical Technique
2.4. Rehabilitation Protocols
2.5. Outcome Measures
2.6. Assessment of Muscle Strength and Neuromuscular Control
2.7. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Patient-Reported Questionnaires
3.3. Comparison of Muscle Strength and Neuromuscular Control Parameters
3.4. Return to Sport
3.5. ACL Re-Injury
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Griffin, L.Y.; Agel, J.; Albohm, M.J.; Arendt, E.A.; Dick, R.W.; Garrett, W.E.; Garrick, J.G.; Hewett, T.E.; Huston, L.; Ireland, M.L.; et al. Noncontact anterior cruciate ligament injuries: Risk factors and prevention strategies. J. Am. Acad. Orthop. Surg. 2000, 8, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Lee, D.H.; Park, J.H.; Suh, D.W.; Kim, E.; Jang, K.M. Poorer dynamic postural stability in patients with anterior cruciate ligament rupture combined with lateral meniscus tear than in those with medial meniscus tear. Knee Surg. Relat. Res. 2020, 32, 8. [Google Scholar] [CrossRef] [PubMed]
- Andrade, R.; Pereira, R.; van Cingel, R.; Staal, J.B.; Espregueira-Mendes, J. How should clinicians rehabilitate patients after ACL reconstruction? A systematic review of clinical practice guidelines (CPGs) with a focus on quality appraisal (AGREE II). Br. J. Sports Med. 2020, 54, 512–519. [Google Scholar] [CrossRef] [PubMed]
- Brinlee, A.W.; Dickenson, S.B.; Hunter-Giordano, A.; Snyder-Mackler, L. ACL Reconstruction Rehabilitation: Clinical Data, Biologic Healing, and Criterion-Based Milestones to Inform a Return-to-Sport Guideline. Sports Health 2022, 14, 770–779. [Google Scholar] [CrossRef] [PubMed]
- Uchino, S.; Saito, H.; Okura, K.; Kitagawa, T.; Sato, S. Effectiveness of a supervised rehabilitation compared with a home-based rehabilitation following anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Phys. Ther. Sport 2022, 55, 296–304. [Google Scholar] [CrossRef]
- Hohmann, E.; Tetsworth, K.; Bryant, A. Physiotherapy-guided versus home-based, unsupervised rehabilitation in isolated anterior cruciate injuries following surgical reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 1158–1167. [Google Scholar] [CrossRef] [PubMed]
- Feller, J.A.; Webster, K.E.; Taylor, N.F.; Payne, R.; Pizzari, T. Effect of physiotherapy attendance on outcome after anterior cruciate ligament reconstruction: A pilot study. Br. J. Sports Med. 2004, 38, 74–77. [Google Scholar] [CrossRef]
- Grant, J.A.; Mohtadi, N.G.; Maitland, M.E.; Zernicke, R.F. Comparison of home versus physical therapy- supervised rehabilitationprograms after anterior cruciate ligament reconstruction: A randomized clinical trial. Am. J. Sports Med. 2005, 33, 1288–1297. [Google Scholar] [CrossRef]
- Ugutmen, E.; Ozkan, K.; Kilincoglu, V.; Ozkan, F.U.; Toker, S.; Eceviz, E.; Altintas, F. Anterior cruciate ligament reconstruction by using otogenous [correction of otogeneous] hamstring tendons with home-based rehabilitation. J. Int. Med. Res. 2008, 36, 253–259. [Google Scholar] [CrossRef]
- Rhim, H.C.; Lee, J.H.; Lee, S.J.; Jeon, J.S.; Kim, G.; Lee, K.Y.; Jang, K.M. Supervised Rehabilitation May Lead to Better Outcome than Home-Based Rehabilitation Up to 1 Year after Anterior Cruciate Ligament Reconstruction. Medicina 2020, 57, 19. [Google Scholar] [CrossRef]
- Glattke, K.E.; Tummala, S.V.; Chhabra, A. Anterior Cruciate Ligament Reconstruction Recovery and Rehabilitation: A Systematic Review. J. Bone Jt. Surg. 2022, 104, 739–754. [Google Scholar] [CrossRef] [PubMed]
- Forster, M.C.; Forster, I.W. Patellar tendon or four-strand hamstring? A systematic review of autografts for anterior cruciate ligament reconstruction. Knee 2005, 12, 225–230. [Google Scholar] [CrossRef]
- Ardern, C.L.; Webster, K.E.; Taylor, N.F.; Feller, J.A. Return to sport following anterior cruciate ligament reconstruction surgery: A systematic review and meta-analysis of the state of play. Br. J. Sports Med. 2011, 45, 596–606. [Google Scholar] [CrossRef]
- Ebert, J.R.; Edwards, P.; Yi, L.; Joss, B.; Ackland, T.; Carey-Smith, R.; Buelow, J.U.; Hewitt, B. Strength and functional symmetry is associated with post-operative rehabilitation in patients following anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 2353–2361. [Google Scholar] [CrossRef] [PubMed]
- Kotsifaki, R.; Korakakis, V.; King, E.; Barbosa, O.; Maree, D.; Pantouveris, M.; Bjerregaard, A.; Luomajoki, J.; Wilhelmsen, J.; Whiteley, R. Aspetar clinical practice guideline on rehabilitation after anterior cruciate ligament reconstruction. Br. J. Sports Med. 2023, 57, 500–514. [Google Scholar] [CrossRef]
- Grindem, H.; Snyder-Mackler, L.; Moksnes, H.; Engebretsen, L.; Risberg, M.A. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: The Delaware-Oslo ACL cohort study. Br. J. Sports Med. 2016, 50, 804–808. [Google Scholar] [CrossRef] [PubMed]
- Hewett, T.E.; Di Stasi, S.L.; Myer, G.D. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am. J. Sports Med. 2013, 41, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Wiggins, A.J.; Grandhi, R.K.; Schneider, D.K.; Stanfield, D.; Webster, K.E.; Myer, G.D. Risk of Secondary Injury in Younger Athletes after Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2016, 44, 1861–1876. [Google Scholar] [CrossRef]
- Papalia, R.; Vasta, S.; Tecame, A.; D’Adamio, S.; Maffulli, N.; Denaro, V. Home-based vs supervised rehabilitation programs following knee surgery: A systematic review. Br. Med. Bull. 2013, 108, 55–72. [Google Scholar] [CrossRef]
- Kyritsis, P.; Bahr, R.; Landreau, P.; Miladi, R.; Witvrouw, E. Likelihood of ACL graft rupture: Not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br. J. Sports Med. 2016, 50, 946–951. [Google Scholar] [CrossRef]
- Ardern, C.L.; Österberg, A.; Tagesson, S.; Gauffin, H.; Webster, K.E.; Kvist, J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br. J. Sports Med. 2014, 48, 1613–1619. [Google Scholar] [CrossRef]
- Sadeqi, M.; Klouche, S.; Bohu, Y.; Herman, S.; Lefevre, N.; Gerometta, A. Progression of the Psychological ACL- RSI Score and Return to Sport after Anterior Cruciate Ligament Reconstruction: A Prospective 2-Year Follow-up Study from the French Prospective Anterior Cruciate Ligament Reconstruction Cohort Study (FAST). Orthop. J. Sports Med. 2018, 6, 2325967118812819. [Google Scholar] [CrossRef] [PubMed]
- Webster, K.E.; Feller, J.A.; Lambros, C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys. Ther. Sport 2008, 9, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Maron, B.J.; Zipes, D.P.; Kovacs, R.J. Eligibility and Disqualification Recommendations for Competitive Athletes with Cardiovascular Abnormalities: Preamble, Principles, and General Considerations: A Scientific Statement From the American Heart Association and American College of Cardiology. J. Am. Coll. Cardiol. 2015, 66, 2343–2349. [Google Scholar] [CrossRef] [PubMed]
- Filbay, S.R.; Grindem, H. Evidence-based recommendations for the management of anterior cruciate ligament (ACL) rupture. Best Pract. Res. Clin. Rheumatol. 2019, 33, 33–47. [Google Scholar] [CrossRef]
- Costa, S.N.; Boiko Ferreira, L.H.; Barauce Bento, P.C. The effects of supervision on three different exercises modalities (supervised vs. home vs. supervised+home) in older adults: Randomized controlled trial protocol. PLoS ONE 2021, 16, e0259827. [Google Scholar] [CrossRef]
- Müller, U.; Krüger-Franke, M.; Schmidt, M.; Rosemeyer, B. Predictive parameters for return to pre-injury level of sport 6 months following anterior cruciate ligament reconstruction surgery. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 3623–3631. [Google Scholar] [CrossRef]
- Joreitz, R.; Lynch, A.; Popchak, A.; Irrgang, J. Criterion-Based Rehabilitation Program with Return to Sport Testing Following Acl Reconstruction: A Case Series. Int. J. Sports Phys. Ther. 2020, 15, 1151–1173. [Google Scholar] [CrossRef]
- Canale, S.T.; Beaty, J.H. Campbell’s Operative Orthopaedics E-Book; Elsevier: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Podlog, L.; Dimmock, J.; Miller, J. A review of return to sport concerns following injury rehabilitation: Practitioner strategies for enhancing recovery outcomes. Phys. Ther. Sport 2011, 12, 36–42. [Google Scholar] [CrossRef]
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Whitehead, T.S.; Webster, K.E. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am. J. Sports Med. 2013, 41, 1549–1558. [Google Scholar] [CrossRef]
- Ardern, C.L.; Webster, K.E.; Taylor, N.F.; Feller, J.A. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: Two-thirds of patients have not returned by 12 months after surgery. Am. J. Sports Med. 2011, 39, 538–543. [Google Scholar] [CrossRef]
- Webster, K.E.; Nagelli, C.V.; Hewett, T.E.; Feller, J.A. Factors Associated with Psychological Readiness to Return to Sport after Anterior Cruciate Ligament Reconstruction Surgery. Am. J. Sports Med. 2018, 46, 1545–1550. [Google Scholar] [CrossRef] [PubMed]
- Kvist, J.; Ek, A.; Sporrstedt, K.; Good, L. Fear of re-injury: A hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2005, 13, 393–397. [Google Scholar] [CrossRef] [PubMed]
- Han, F.; Banerjee, A.; Shen, L.; Krishna, L. Increased Compliance with Supervised Rehabilitation Improves Functional Outcome and Return to Sport after Anterior Cruciate Ligament Reconstruction in Recreational Athletes. Orthop. J. Sports Med. 2015, 3, 2325967115620770. [Google Scholar] [CrossRef] [PubMed]
- Chung, K.S.; Ha, J.K.; Yeom, C.H.; Ra, H.J.; Lim, J.W.; Kwon, M.S.; Kim, J.G. Are Muscle Strength and Function of the Uninjured Lower Limb Weakened after Anterior Cruciate Ligament Injury? Two-Year Follow-up after Reconstruction. Am. J. Sports Med. 2015, 43, 3013–3021. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, D.; Myer, G.D.; McKeon, J.M.; Hewett, T.E. Evaluation of the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: A critical review of relative risk reduction and numbers-needed-to-treat analyses. Br. J. Sports Med. 2012, 46, 979–988. [Google Scholar] [CrossRef] [PubMed]
- Adams, D.; Logerstedt, D.S.; Hunter-Giordano, A.; Axe, M.J.; Snyder-Mackler, L. Current concepts for anterior cruciate ligament reconstruction: A criterion-based rehabilitation progression. J. Orthop. Sports Phys. Ther. 2012, 42, 601–614. [Google Scholar] [CrossRef] [PubMed]
- Faleide, A.G.H.; Magnussen, L.H.; Strand, T.; Bogen, B.E.; Moe-Nilssen, R.; Mo, I.F.; Vervaat, W.; Inderhaug, E. The Role of Psychological Readiness in Return to Sport Assessment after Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2021, 49, 1236–1243. [Google Scholar] [CrossRef]
- van Melick, N.; van Cingel, R.E.; Brooijmans, F.; Neeter, C.; van Tienen, T.; Hullegie, W.; Nijhuis-van der Sanden, M.W. Evidence-based clinical practice update: Practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br. J. Sports Med. 2016, 50, 1506–1515. [Google Scholar] [CrossRef]


| Baseline Characteristics | SVR (n = 30) | HBR (n = 30) | p |
|---|---|---|---|
| Gender (male/female) | 15/15 | 15/15 | |
| Age (years) | 22.43 ± 6.34 | 24.96 ± 7.93 | 0.199 |
| Height (cm) | 174.78 ± 9.59 | 172 ± 9.81 | 0.302 |
| Weight (kg) | 71.11 ± 12.90 | 77.23 ± 20.41 | 0.196 |
| Follow-up time (months) | 8.62 ± 7.32 | 8.48 ± 7.68 | 0.950 |
| BMI (Male) | 22.19 ± 2.02 | 23.93 ± 2.75 | 0.070 |
| BMI (Female) | 24.23 ± 2.52 | 25.53 ± 3.66 | 0.327 |
| Measurement Procedure | Group | Mean | SD | p | Effect Size | Power |
|---|---|---|---|---|---|---|
| 30 deg Max Isometric Quadricep Strength (kg) O | SVR | 54.614 | 16.295 | 0.077 | ||
| HBR | 44.810 | 18.607 | ||||
| 30 deg Max Isometric Quadricep Strength (kg) NO | SVR | 68.957 | 16.720 | 0.035 * | 0.664 | 0.689 |
| HBR | 57.323 | 18.257 | ||||
| 30 deg Quadricep Asymmetry (%) | SVR | 21.519 | 11.708 | 0.969 | ||
| HBR | 21.352 | 15.479 | ||||
| 30 deg Max Isometric Hamstring Strength (kg) O | SVR | 21.514 | 6.237 | 0.224 | ||
| HBR | 19.217 | 6.091 | ||||
| 30 deg Max Isometric Hamstring Strength (kg) NO | SVR | 24.686 | 6.528 | 0.730 | ||
| HBR | 25.465 | 8.194 | ||||
| 30 deg Hamstring Asymmetry (%) | SVR | 17.490 | 10.564 | 0.042 * | 0.633 | 0.662 |
| HBR | 24.970 | 12.832 | ||||
| 30 deg H/Q Ratio (%) O | SVR | 38.462 | 11.329 | 0.218 | ||
| HBR | 43.979 | 16.704 | ||||
| 30 deg H/Q Ratio (%) NO | SVR | 34.664 | 7.189 | 0.018 * | 0.752 | 0.782 |
| HBR | 43.412 | 14.672 | ||||
| 45 deg Max Isometric Quadricep Strength (kg) O | SVR | 58.252 | 15.364 | 0.214 | ||
| HBR | 51.448 | 19.344 | ||||
| 45 deg Max Isometric Quadricep Strength (kg) NO | SVR | 71.233 | 17.792 | 0.155 | ||
| HBR | 62.868 | 19.986 | ||||
| 45 deg Quadricep Asymmetry (%) | SVR | 21.019 | 11.199 | 0.781 | ||
| HBR | 19.895 | 14.650 | ||||
| 45 deg Max Isometric Hamstring Strength (kg) O | SVR | 20.233 | 6.684 | 0.031 * | 0.673 | 0.691 |
| HBR | 16.304 | 4.953 | ||||
| 45.deg Max Isometric Hamstring Strength (kg) NO | SVR | 24.233 | 6.163 | 0.981 | ||
| HBR | 24.183 | 7.993 | ||||
| 45 deg Hamstring Asymmetry (%) | SVR | 19.967 | 13.815 | 0.010 * | 0.81 | 0.84 |
| HBR | 31.696 | 15.057 | ||||
| 45 deg H/Q Ratio (%) O | SVR | 34.025 | 10.749 | 0.786 | ||
| HBR | 33.066 | 11.922 | ||||
| 45 deg H/Q Ratio (%) NO | SVR | 33.790 | 7.743 | 0.131 | ||
| HBR | 38.528 | 11.878 | ||||
| Isokinetic Leg Extension 240° (Kg) O | SVR | 20.850 | 6.716 | 0.007 * | 1.183 | 0.885 |
| HBR | 13.809 | 4.781 | ||||
| Isokinetic Leg Extension 240° (Kg) NO | SVR | 25.114 | 6.431 | 0.010 * | 1.133 | 0.86 |
| HBR | 17.664 | 6.763 |
| Measurement Procedure | Group | Mean | SD | p |
|---|---|---|---|---|
| Max Isometric Hip Adductor Strength at 60. Knee Flexion (N) O | SVR | 379.837 | 96.169 | 0.164 |
| HBR | 339.609 | 89.725 | ||
| Max Isometric Hip Adductor Strength at 60. Knee Flexion (N) NO | SVR | 387.188 | 90.290 | 0.160 |
| HBR | 348.174 | 88.023 | ||
| Hip Adductor Asymmetry (%) | SVR | 5.633 | 3.356 | 0.956 |
| HBR | 5.694 | 3.760 | ||
| Max Isometric Hip Abductor Strength at 60. Knee Flexion (N) O | SVR | 354.967 | 87.474 | 0.127 |
| HBR | 315.326 | 79.593 | ||
| Max Isometric Hip Abductor Strength at 60. Knee Flexion (N) NO | SVR | 352.650 | 76.089 | 0.163 |
| HBR | 318.630 | 80.340 | ||
| Hip Abductor Asymmetry (%) | SVR | 7.759 | 5.368 | 0.854 |
| HBR | 8.076 | 5.814 | ||
| Hip ABD/ADD Ratio (%) O | SVR | 94.480 | 15.259 | 0.958 |
| HBR | 94.752 | 18.359 | ||
| Hip ABD/ADD Ratio (%) NO | SVR | 92.825 | 18.038 | 0.931 |
| HBR | 92.400 | 13.792 | ||
| Stance Evaluation Weight Distribution (%) O | SVR | 49.757 | 3.667 | 0.408 |
| HBR | 48.870 | 3.371 | ||
| Stance Evaluation Weight Distribution (%) NO | SVR | 50.243 | 3.667 | 0.408 |
| HBR | 51.130 | 3.371 | ||
| Squat Analysis Average Weight Distribution (%) O | SVR | 48.433 | 2.765 | 0.961 |
| HBR | 48.395 | 2.338 | ||
| Squat Analysis Average Weight Distribution (%) NO | SVR | 51.567 | 2.765 | 0.961 |
| HBR | 51.605 | 2.338 |
| RTS | SVR Group | HBR Group |
|---|---|---|
| Same level | 23 (76.6%) | 16 (53.3%) |
| Lower level | 5 (16.6%) | 9 (30%) |
| No return | 2 (6.6%) | 5 (16.6%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Syed, R.I.B.; Hangody, L.R.; Frischmann, G.; Kós, P.; Kopper, B.; Berkes, I. Comparative Effectiveness of Supervised and Home-Based Rehabilitation after Anterior Cruciate Ligament Reconstruction in Competitive Athletes. J. Clin. Med. 2024, 13, 2245. https://doi.org/10.3390/jcm13082245
Syed RIB, Hangody LR, Frischmann G, Kós P, Kopper B, Berkes I. Comparative Effectiveness of Supervised and Home-Based Rehabilitation after Anterior Cruciate Ligament Reconstruction in Competitive Athletes. Journal of Clinical Medicine. 2024; 13(8):2245. https://doi.org/10.3390/jcm13082245
Chicago/Turabian StyleSyed, Rehan Iftikhar Bukhari, Laszlo Rudolf Hangody, Gergely Frischmann, Petra Kós, Bence Kopper, and István Berkes. 2024. "Comparative Effectiveness of Supervised and Home-Based Rehabilitation after Anterior Cruciate Ligament Reconstruction in Competitive Athletes" Journal of Clinical Medicine 13, no. 8: 2245. https://doi.org/10.3390/jcm13082245