The Mechanical and Clinical Properties of Customized Orthodontic Bracket Systems—A Comprehensive Review
Abstract
:1. Introduction
2. Materials and Methods
3. CAD/CAM Customized Bracket Properties
3.1. CAD/CAM Customized Lingual Brackets
| Bracket System (Brands) | CAD/CAM Customized Lingual (Incognito; Harmony) | CAD/CAM Customized Labial (Insignia) | |
|---|---|---|---|
| Mechanical Properties | Fracture Toughness | - | - |
| Hardness | - | - | |
| Modulus of Elasticity | - | - | |
| Frictional Resistance | Higher (compared to both TMB and TML) [28] | - | |
| Slot Accuracy | Higher (Incognito compared to TML) [29] | - | |
| Torque Momentum | Higher (Incognito compared to TMB) [30] | - | |
| Shear Bond Strength | Lower (Incognito and Harmony compared to TMB and Insignia) [31] | Higher (compared to TMB, Incognito, and Harmony) More brackets debond (compared to TMB) [31,32] | |
| Clinical Properties | Treatment Outcome | Less effective in vertical and anteroposterior corrections (Incognito compared to TMB) [33] | Inconsistent conclusions from different studies (compared to TMB) |
| Chair Time | Shorter (Harmony compared to TMB) [34] | - | |
| Treatment Duration | - | Inconsistent conclusions from different studies (compared to TMB) | |
| Color Stability | - | - | |
| Discomfort | Less (compared to TML) [35,36] | Inconsistent conclusions from different studies (compared to TMB) | |
| Cost | Higher (compared to TMB) [37] | Higher (compared to TMB) [38] | |
| White Spot Lesions | Fewer (compared to TMB placed buccally) [39] | - | |
3.1.1. Mechanical Properties
3.1.2. Clinical Properties
3.1.3. Summary
3.2. CAD/CAM Customized Labial Brackets
3.2.1. Mechanical Properties
3.2.2. Clinical Properties
3.2.3. Summary
4. 3D-Printed Customized Bracket Properties
4.1. 3D-Printed Customized Brackets: Metal
| Bracket System | 3D-Printed Metal | |
|---|---|---|
| Mechanical Properties | Fracture Toughness | - |
| Hardness | - | |
| Modulus of Elasticity | - | |
| Frictional Resistance | - | |
| Slot Accuracy | Higher (compared to TMB); minor bumps found on slot surface [60] | |
| Torque Momentum | - | |
| Shear Bond Strength | Lower (compared to TMB) [60] | |
| Clinical Properties | Treatment Outcome | - |
| Chair Time | - | |
| Treatment Duration | - | |
| Color Stability | - | |
| Discomfort | - | |
| Cost | $7 per bracket and 90 min to print both arches [60] | |
| White Spot Lesions | - | |
4.1.1. Mechanical Properties
4.1.2. Clinical Properties
4.1.3. Summary
4.2. 3D-Printed Customized Brackets: Ceramic
| Bracket System | 3D-Printed Ceramic | |||
|---|---|---|---|---|
| Polycrystalline Alumina | Lithium Disilicate | Zirconia | ||
| Mechanical Properties | Fracture Toughness | Lower (compared to TPCB) [65] | - | Higher (compared to TPCB and 3D-printed alumina) [65] |
| Hardness | Lower (compared to TPCB) Higher (compared to 3D-printed zirconia) [65,66] | - | Lower (compared to TPCB and 3D-printed alumina) [65,67] | |
| Modulus of Elasticity | - | - | - | |
| Frictional Resistance | - | Lower (compared to TPCB) Higher (compared to TMCB) [68] | - | |
| Slot Accuracy | - | No obvious defects (compared to TPCB) [68] | - | |
| Torque Momentum | - | - | - | |
| Shear Bond Strength | - | Similar (compared to TMB) Lower (compared to TPCB) [68] | - | |
| Clinical Properties | Treatment Outcome | Fewer loose brackets and superior final tooth alignment (compared to TMB) [69] | - | - |
| Chair Time | - | - | - | |
| Treatment Duration | Shorter (compared to TMB) [69] | - | - | |
| Color Stability | - | Less (compared to TPCB) [68] | - | |
| Discomfort | - | - | - | |
| Cost | Higher (compared to TMB) [69] | - | $1000 per 1 L slurry (1.5 mL required per 24 brackets) [21,26] | |
| White Spot Lesions | - | - | - | |
4.2.1. 3D-Printed Customized Ceramic Brackets: Polycrystalline Alumina
Mechanical Properties
Clinical Properties
Summary
4.2.2. D-Printed Customized Ceramic Brackets: Lithium Disilicate
Mechanical Properties
Clinical Properties
Summary
4.2.3. 3D-Printed Customized Ceramic Brackets: Zirconia
Mechanical Properties
Summary
4.3. 3D-Printed Customized Brackets: Plastic/Resin
4.3.1. Mechanical Properties
| Bracket System | 3D-Printed Plastic/Resin | |||||||
|---|---|---|---|---|---|---|---|---|
| Permanent Crown Resin | Temporary Crown Resin | SG Resin | LT Resin | Shark SL | Sheraprint Ortho PLus | GR-10/GR-17.1 Guide Resin | ||
| Mechanical Properties | Fracture Toughness | Higher (compared to TPCB) [84] | - | - | - | - | Lower (compared to TMB) [1] | - |
| Hardness | Lower (compared to TMB and TPCB) Higher (compared to TPB) [65,85] | Lower (compared to TMB and TPCB) Higher (compared to TPB) [65,85] | - | - | - | - | - | |
| Modulus of Elasticity | Lower (compared to TMB and TPCB) [85] | Lower (compared to TMB and TPCB) [85] | - | - | - | - | - | |
| Frictional Resistance | - | - | - | - | Lower (compared to TMB and TPCB) [86,87] | - | - | |
| Slot Accuracy | Higher (compared to TPB and TMB) [88] | - | - | - | - | - | - | |
| Torque Momentum | Clinically sufficient (compared to TMB and TPCB) [84] | - | - | - | - | - | - | |
| Shear Bond Strength | - | - | Clinically sufficient (compared to TMB and TPB) [89] | Clinically sufficient (compared to TMB and TPB) [89] | - | - | - | |
| Clinical Properties | Treatment Outcome | - | - | - | - | - | - | - |
| Chair Time | - | - | - | - | - | - | - | |
| Treatment Duration | - | - | - | - | - | - | - | |
| Color Stability | - | - | Less (compared to LT Resin) [90] | Higher (compared to SG Resin) [90] | - | - | Unstable [91] | |
| Discomfort | - | - | - | - | - | - | - | |
| Cost | $790 per 0.7 L [92] | $499 per 0.7 L [93] | $249 per 1 L [94] | $349 per 1 L [95] | - | - | - | |
| White Spot Lesions | - | - | - | - | - | - | - | |
4.3.2. Clinical Properties
4.3.3. Summary
5. Conclusions and Future Directions
- (1)
- CAD/CAM customized lingual brackets: CAD/CAM customized lingual brackets stand out in modern orthodontics because they are discreet and fit each patient’s anatomy precisely. They offer significant improvements in comfort and treatment effectiveness, but it is important to fully understand their biomechanical impacts before use.
- (2)
- CAD/CAM customized labial brackets: Evaluating the mechanical and clinical properties of CAD/CAM customized labial brackets is still in its infancy. Contradictory results about treatment duration and its effectiveness indicate that more research is needed.
- (3)
- 3D-printed metal brackets: 3D-printed metal brackets could possibly blend customization with the efficient properties of the traditional metal bracket. Increased slot accuracy is a promising property, but the evidence is limited.
- (4)
- 3D-Printed Polycrystalline alumina ceramic brackets: The concept behind 3D-printed alumina ceramic brackets is compelling, but they are currently characterized by brittleness and fracture susceptibility. Current research suggests that they speed up orthodontic treatment compared to traditional systems.
- (5)
- 3D-printed lithium disilicate brackets: 3D-printed lithium disilicate brackets may be superior to traditional ceramic brackets given that they have lower frictional resistance. However, the lower color stability compromises the aesthetics—the key feature of ceramic brackets.
- (6)
- 3D-Printed Zirconia brackets: 3D-printed zirconia brackets require extensive research to fully grasp their clinical implications. Initial research points to promising fracture resistance, which minimizes wing fractures, and low hardness, which prevents enamel abrasion compared to conventional ceramics.
- (7)
- 3D-Printed Resin/plastic brackets: Multiple types of resin have been used for 3D-printed resin brackets. But the evaluation of the properties of each type of 3D-printed resin brackets is minimum. Currently, brackets printed with permanent crown resin may hold good clinical potential due to their high fracture toughness, low hardness, high slot accuracy, and clinically sufficient torque momentum.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Krey, K.F.; Darkazanly, N.; Kühnert, R.; Ruge, S. 3D-printed orthodontic brackets-proof of concept. Int. J. Comput. Dent. 2016, 19, 351–362. [Google Scholar] [PubMed]
- Khan, S.U. Comparative assessment of customized (insignia) and non-customized bracket systems (Damon Q) for clinical effectiveness and efficiency—A clinical study. IP Indian J. Orthod. Dentofac. Res. (IJODR) 2022, 8, 94–103. [Google Scholar] [CrossRef]
- Alrejaye, N.; Pober, R.; Giordano Ii, R. Torsional strength of computer-aided design/computer-aided manufacturing-fabricated esthetic orthodontic brackets. Angle Orthod. 2017, 87, 125–130. [Google Scholar] [CrossRef]
- Andrews, L.F. The six keys to normal occlusion. Am. J. Orthod. 1972, 62, 296–309. [Google Scholar] [CrossRef]
- Brown, M.W.; Koroluk, L.; Ko, C.C.; Zhang, K.; Chen, M.; Nguyen, T. Effectiveness and efficiency of a CAD/CAM orthodontic bracket system. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 1067–1074. [Google Scholar] [CrossRef]
- Gange, P. The evolution of bonding in orthodontics. Am. J. Orthod. Dentofac. Orthop. 2015, 147, S56–S63. [Google Scholar] [CrossRef]
- Koo, B.C.; Chung, C.H.; Vanarsdall, R.L. Comparison of the accuracy of bracket placement between direct and indirect bonding techniques. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 346–351. [Google Scholar] [CrossRef]
- Hodge, T.M.; Dhopatkar, A.A.; Rock, W.P.; Spary, D.J. A randomized clinical trial comparing the accuracy of direct versus indirect bracket placement. J. Orthod. 2004, 31, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Miethke, R.R.; Melsen, B. Effect of variation in tooth morphology and bracket position on first and third order correction with preadjusted appliances. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 329–335. [Google Scholar] [CrossRef]
- Alexopoulou, E.; Polychronis, G.; Konstantonis, D.; Sifakakis, I.; Zinelis, S.; Eliades, T. A study of the mechanical properties of as-received and intraorally exposed single-crystal and polycrystalline orthodontic ceramic brackets. Eur. J. Orthod. 2020, 42, 72–77. [Google Scholar] [CrossRef]
- Iwasaki, T.; Nagata, S.; Ishikawa, T.; Tanimoto, Y. Mechanical characterization of aesthetic orthodontic brackets by the dynamic indentation method. Dent. Mater. J. 2022, 41, 860–867. [Google Scholar] [CrossRef] [PubMed]
- Bhat, K.R.R.; Ahmed, N.; Joseph, R.; Younus, A.A. Comparative Evaluation of Frictional Resistance between Different Types of Ceramic Brackets and Stainless Steel Brackets with Teflon-Coated Stainless Steel and Stainless Steel Archwires: An In-Vitro Study. Cureus J. Med. Sci. 2022, 14, e24161. [Google Scholar] [CrossRef] [PubMed]
- Stasinopoulos, D.; Papageorgiou, S.N.; Kirsch, F.; Daratsianos, N.; Jäger, A.; Bourauel, C. Failure patterns of different bracket systems and their influence on treatment duration: A retrospective cohort study. Angle Orthod. 2018, 88, 338–347. [Google Scholar] [CrossRef] [PubMed]
- Arash, V.; Rabiee, M.; Rakhshan, V.; Khorasani, S.; Sobouti, F. In vitro evaluation of frictional forces of two ceramic orthodontic brackets versus a stainless steel bracket in combination with two types of archwires. J. Orthod. Sci. 2015, 4, 42–46. [Google Scholar] [CrossRef]
- Williams, C.L.; Khalaf, K. Frictional resistance of three types of ceramic brackets. J. Oral Maxillofac. Res. 2013, 4, e3. [Google Scholar] [CrossRef]
- Malkiewicz, K.; Jastrzebska, A.; Janas-Naze, A.; Bartczak, J. Assessment of the Susceptibility of Aesthetic Orthodontic Brackets to Discoloration. Coatings 2022, 12, 1080. [Google Scholar] [CrossRef]
- Larson, N. Mechanical Stability of 3D-Printed Orthodontic Brackets. Master’s Thesis, The University of Texas School of Dentistry at Houston, Houston, TX, USA, 2019. [Google Scholar]
- Wiechmann, D. A new bracket system for lingual orthodontic treatment. Part 1: Theoretical background and development. J. Orofac. Orthop. 2002, 63, 234–245. [Google Scholar] [CrossRef]
- Wiechmann, D. A new bracket system for lingual orthodontic treatment. Part 2: First clinical experiences and further development. J. Orofac. Orthop. 2003, 64, 372–388. [Google Scholar] [CrossRef]
- Wiechmann, D.; Rummel, V.; Thalheim, A.; Simon, J.S.; Wiechmann, L. Customized brackets and archwires for lingual orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 593–599. [Google Scholar] [CrossRef]
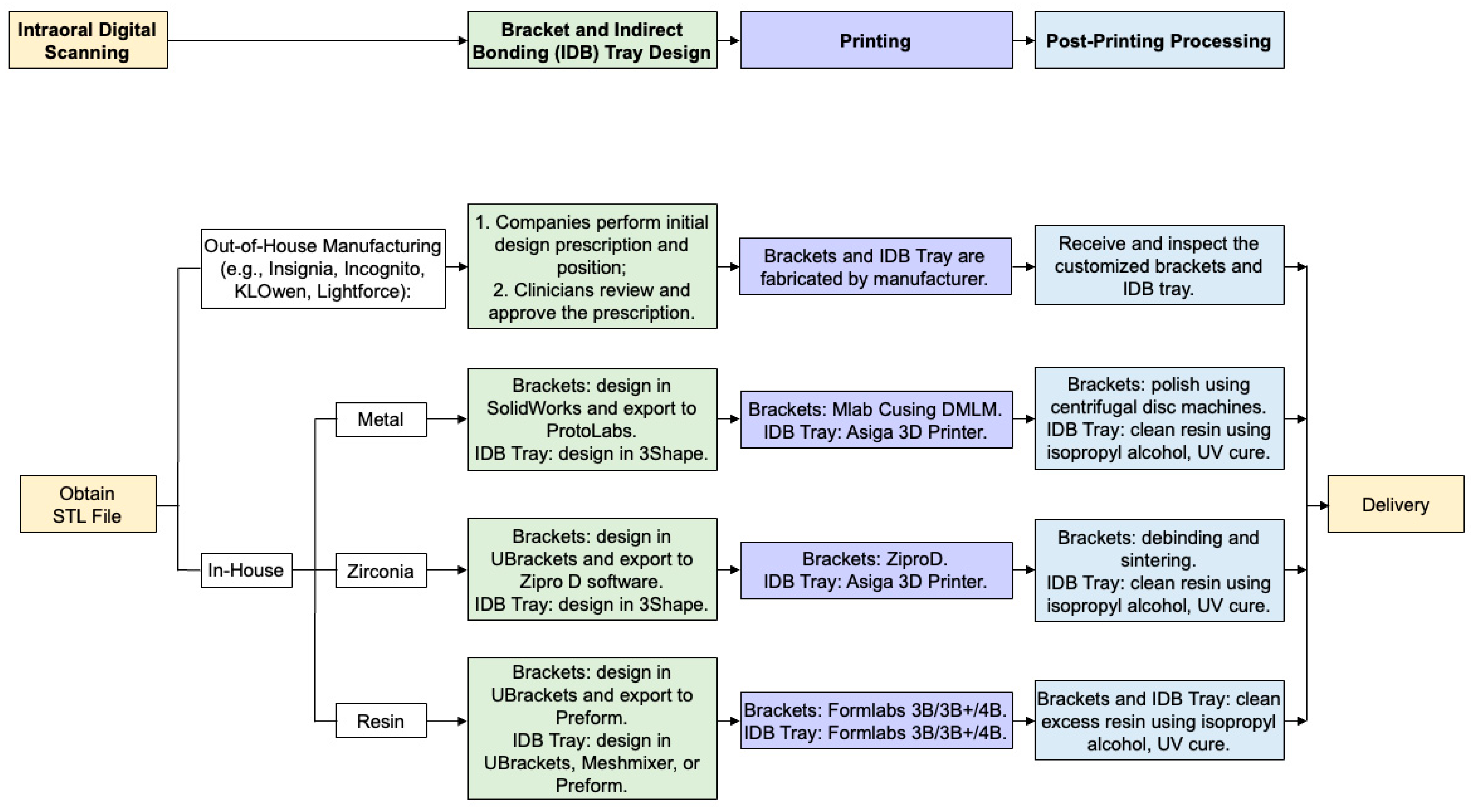
- Panayi, N.C. In-house three-dimensional designing and printing customized brackets. J. World Fed. Orthod. 2022, 11, 190–196. [Google Scholar] [CrossRef]
- Kodama, H. A scheme for three-dimensional display by automatic fabrication of three-dimensional model. J. IEICE 1981, 52, 1770. [Google Scholar] [CrossRef]
- Panayi, N.C. In-office Customized Brackets: Aligning with the Future. Turk. J. Orthod. 2023, 36, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Shannon, T.; Groth, C. Be your own manufacturer: 3D printing intraoral appliances. Semin. Orthod. 2021, 27, 184–188. [Google Scholar] [CrossRef]
- Jasen, S. Applicability of CAD/CAM Technology in Orthodontics. Stud. Comput. Intell. 2022, 1010, 69–76. [Google Scholar] [CrossRef]
- Panayi, N.C. 3D Printing of in Office Custom-Made Brackets: Concept, Design, Production and Evidence. Semin. Orthod. 2023, 29, 11–16. [Google Scholar] [CrossRef]
- Huang, G.; Wu, L.; Hu, J.; Zhou, X.; He, F.; Wan, L.; Pan, S.T. Main Applications and Recent Research Progresses of Additive Manufacturing in Dentistry. Biomed. Res. Int. 2022, 2022, 5530188. [Google Scholar] [CrossRef]
- Albertini, P.; Franciosi, F.; Palone, M.; Mollica, F.; Cremonini, F. Comparative Analysis of Sliding Resistance of Different Lingual Systems. Pesqui. Bras. Odontopediatria Clín. Integr. 2021, 21, e210025. [Google Scholar] [CrossRef]
- Demling, A.; Dittmer, M.P.; Schwestka-Polly, R. Comparative analysis of slot dimension in lingual bracket systems. Head Face Med. 2009, 5, 27. [Google Scholar] [CrossRef]
- Sifakakis, I.; Pandis, N.; Makou, M.; Eliades, T.; Katsaros, C.; Bourauel, C. A comparative assessment of torque generated by lingual and conventional brackets. Eur. J. Orthod. 2013, 35, 375–380. [Google Scholar] [CrossRef]
- Sha, H.N.; Choi, S.H.; Yu, H.S.; Hwang, C.J.; Cha, J.Y.; Kim, K.M. Debonding force and shear bond strength of an array of CAD/CAM-based customized orthodontic brackets, placed by indirect bonding—An in vitro study. PLoS ONE 2018, 13, e0202952. [Google Scholar] [CrossRef]
- Joseph, R.; Ahmed, N.; Younus, A.A.; Bhat, K.R.R. Evaluation of Shear Bond Strength of a Primer Incorporated Orthodontic Composite Resin: An In-Vitro Study. Cureus 2022, 14, e24088. [Google Scholar] [CrossRef] [PubMed]
- Alobeid, A.; El-Bialy, T.; Reimann, S.; Keilig, L.; Cornelius, D.; Jäger, A.; Bourauel, C. Comparison of the efficacy of tooth alignment among lingual and labial brackets: An in vitro study. Eur. J. Orthod. 2018, 40, 660–665. [Google Scholar] [CrossRef]
- Dalessandri, D.; Lazzaroni, E.; Migliorati, M.; Piancino, M.; Tonni, I.; Bonetti, S. Self-ligating fully customized lingual appliance and chair-time reduction: A typodont study followed by a randomized clinical trial. Eur. J. Orthod. 2013, 35, 758–765. [Google Scholar] [CrossRef] [PubMed]
- Stamm, T.; Hohoff, A.; Ehmer, U. A subjective comparison of two lingual bracket systems. Eur. J. Orthod. 2005, 27, 420–426. [Google Scholar] [CrossRef]
- Wiechmann, D.; Gerss, J.; Stamm, T.; Hohoff, A. Prediction of oral discomfort and dysfunction in lingual orthodontics: A preliminary report. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 359–364; quiz 476.e351. [Google Scholar] [CrossRef]
- Fuck, L.-M.; Wiechmann, D.; Drescher, D. Comparison of the Initial Orthodontic Force Systems Produced by a New Lingual Bracket System and a Straight-Wire Appliance. J. Orofac. Orthop./Fortschritte Kieferorthopädie 2005, 66, 363–376. [Google Scholar] [CrossRef]
- Ormco. INSIGNIATM Advanced Digital Orthodontic Solution. Available online: https://ormco.com/en-us/insignia-advantage (accessed on 22 July 2024).
- van der Veen, M.H.; Attin, R.; Schwestka-Polly, R.; Wiechmann, D. Caries outcomes after orthodontic treatment with fixed appliances: Do lingual brackets make a difference? Eur. J. Oral Sci. 2010, 118, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Kaptac, M.; Unuvar, Y.A. Customized lingual brackets vs. conventional labial brackets for initial alignment A randomized clinical trial. J. Orofac. Orthop.-Fortschritte Kieferorthopadie 2022, 83, 307–317. [Google Scholar] [CrossRef]
- Reis, A.; Santos, J.E.d.; Loguercio, A.D.; de Oliveira Bauer, J.R. Eighteen-month bracket survival rate: Conventional versus self-etch adhesive. Eur. J. Orthod. 2008, 30, 94–99. [Google Scholar] [CrossRef]
- Kachoei, M.; Mohammadi, A.; Esmaili Moghaddam, M.; Rikhtegaran, S.; Pourghaznein, M.; Shirazi, S. Comparison of multiple rebond shear strengths of debonded brackets after preparation with sandblasting and CO2 laser. J. Dent. Res. Dent. Clin. Dent. Prospect. 2016, 10, 148–154. [Google Scholar] [CrossRef]
- Jung, M.H.; Shon, W.J.; Park, Y.S.; Chung, S.H. Effects of silanation time on shear bond strength between a gold alloy surface and metal bracket. Korean J. Orthod. 2013, 43, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Geron, S.; Romano, R.; Brosh, T. Vertical forces in labial and lingual orthodontics applied on maxillary incisors—A theoretical approach. Angle Orthod. 2004, 74, 195–201. [Google Scholar] [CrossRef]
- Sifakakis, I.; Pandis, N.; Makou, M.; Katsaros, C.; Eliades, T.; Bourauel, C. A comparative assessment of forces and moments generated by lingual and conventional brackets. Eur. J. Orthod. 2011, 35, 82–86. [Google Scholar] [CrossRef]
- Wiechmann, D.; Klang, E.; Helms, H.J.; Knösel, M. Lingual appliances reduce the incidence of white spot lesions during orthodontic multibracket treatment. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 414–422. [Google Scholar] [CrossRef]
- Perri, A.; Gracco, A.; Siviero, L.; Parenti, I.S.; Ippolito, D.R. Customized orthodontics: The Insignia System. Int. J. Orthod. Milwaukee 2014, 25, 17–20. [Google Scholar]
- Gracco, A.; Tracey, S. The insignia system of customized orthodontics. J. Clin. Orthod. 2011, 45, 442–451; quiz 467–448. [Google Scholar] [PubMed]
- Liu, F.; Liu, L.; Wang, Y.H. Evaluation of the effect of Insignia system in customized orthodontic treatment. Shanghai Kou Qiang Yi Xue [Shanghai J. Stomatol.] 2022, 31, 96–99. [Google Scholar]
- Klocke, A.; Kahl-Nieke, B. Influence of force location in orthodontic shear bond strength testing. Dent. Mater. 2005, 21, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Papakostopoulou, M.; Hurst, D. Customised fixed appliance systems and treatment duration. Evid.-Based Dent. 2018, 19, 50. [Google Scholar] [CrossRef]
- Penning, E.; Peerlings, R.; Govers, J.; Rischen, R.; Zinad, K.; Bronkhorst, E.; Breuning, K.; Kuijpers-Jagtman, A. Orthodontics with Customized versus Noncustomized Appliances: A Randomized Controlled Clinical Trial. J. Dent. Res. 2017, 96, 1498–1504. [Google Scholar] [CrossRef]
- Weber, D.J., 2nd; Koroluk, L.D.; Phillips, C.; Nguyen, T.; Proffit, W.R. Clinical effectiveness and efficiency of customized vs. conventional preadjusted bracket systems. J. Clin. Orthod. 2013, 47, 261–266; quiz 268. [Google Scholar] [PubMed]
- Hegele, J.; Seitz, L.; Claussen, C.; Baumert, U.; Sabbagh, H.; Wichelhaus, A. Clinical effects with customized brackets and CAD/CAM technology: A prospective controlled study. Prog. Orthod. 2021, 22, 40. [Google Scholar] [CrossRef]
- Choi, E.A.; Park, J.H.; Erdenebat, T.; Hwang, C.J.; Cha, J.Y. Surgical treatment of a skeletal Class III patient using customized brackets based on the CAD/CAM virtual orthodontic system. Angle Orthod. 2021, 91, 692–704. [Google Scholar] [CrossRef]
- Jackers, N.; Maes, N.; Lambert, F.; Albert, A.; Charavet, C. Standard vs computer-aided design/computer-aided manufacturing customized self-ligating systems using indirect bonding with both: A comparative study. Angle Orthod. 2021, 91, 74–80. [Google Scholar] [CrossRef]
- Tsai, M.J.; Wu, C.T.; Chen, C.Y. Custome-Made Brackets Fabrication by an Additive Manufacturing Process for Orthodontic Treatment. Biomed. Eng.-Appl. Basis Commun. 2011, 23, 493–500. [Google Scholar] [CrossRef]
- Prinz, F. Processing, thermal, and mechanical issues in shape deposition manufacturing. Eng. Mater. Sci. 1995. [Google Scholar] [CrossRef]
- Kravitz, N.D. Introduction. Semin. Orthod. 2021, 27, 173–174. [Google Scholar] [CrossRef]
- Jackson, C. Accuracy and Performance of a Novel 3D Metal Printed Orthodontic Bracket. Master’s Thesis, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA, 2017. [Google Scholar]
- Cash, A.C.; Good, S.A.; Curtis, R.V.; McDonald, F. An evaluation of slot size in orthodontic brackets—Are standards as expected? Angle Orthod. 2004, 74, 450–453. [Google Scholar] [CrossRef] [PubMed]
- Kusy, R.P.; Whitley, J.Q. Assessment of second-order clearances between orthodontic archwires and bracket slots via the critical contact angle for binding. Angle Orthod. 1999, 69, 71–80. [Google Scholar] [CrossRef]
- Garrett, A.; Alghilan, M.A.; Ash, S.; Awawdeh, M.; Singh, P. An Evaluation of the Accuracy and Precision of Ceramic Orthodontic Bracket Slot Dimensions Utilizing Micro-Computed Tomography (Micro-CT). Tomography 2023, 9, 1369–1380. [Google Scholar] [CrossRef]
- Owen, B. Analog to digital conversion for all orthodontic patients. Semin. Orthod. 2021, 27, 196–200. [Google Scholar] [CrossRef]
- Polychronis, G.; Papageorgiou, S.N.; Riollo, C.S.; Panayi, N.; Zinelis, S.; Eliades, T. Fracture toughness and hardness of in-office, 3D-printed ceramic brackets. Orthod. Craniofacial Res. 2023, 26, 476–480. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.B. Fracture Resistance of Tie Wings of Ceramic Brackets Under Loading. Ph.D. Thesis, University of Alabama at Birmingham School of Dentistry, Birmingham, AL, USA, 2020. [Google Scholar]
- Kruzic, J.J.; Kim, D.K.; Koester, K.J.; Ritchie, R.O. Indentation techniques for evaluating the fracture toughness of biomaterials and hard tissues. J. Mech. Behav. Biomed. Mater. 2009, 2, 384–395. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Yin, G.; Liao, X.; Yin, X.; Ye, N. A novel customized ceramic bracket for esthetic orthodontics: In vitro study. Prog. Orthod. 2019, 20, 39. [Google Scholar] [CrossRef]
- Waldman, A.; Garvan, C.S.; Yang, J.; Wheeler, T.T. Clinical efficiency of LightForce 3D-printed custom brackets. J. Clin. Orthod. 2023, 57, 274–282. [Google Scholar]
- Griffin, A.C. Ceramic Processing for the Direct Manufacture of Customized Labial and Lingual Orthodontic Brackets. US10241499B1, 26 March 2019. [Google Scholar]
- Meling, T.R.; Odegaard, J.; Meling, E.O. On mechanical properties of square and rectangular stainless steel wires tested in torsion. Am. J. Orthod. Dentofac. Orthop. 1997, 111, 310–320. [Google Scholar] [CrossRef]
- Lefebvre, C.; Saadaoui, H.; Olive, J.M.; Renaudin, S.; Jordana, F. Variability of slot size in orthodontic brackets. Clin. Exp. Dent. Res. 2019, 5, 528–533. [Google Scholar] [CrossRef]
- Kwon, S.J.; Lawson, N.C.; McLaren, E.E.; Nejat, A.H.; Burgess, J.O. Comparison of the mechanical properties of translucent zirconia and lithium disilicate. J. Prosthet. Dent. 2018, 120, 132–137. [Google Scholar] [CrossRef]
- Motro, P.F.; Kursoglu, P.; Kazazoglu, E. Effects of different surface treatments on stainability of ceramics. J. Prosthet. Dent. 2012, 108, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Kelly, J.R. Dental Ceramics for Restoration and Metal Veneering. Dent. Clin. N. Am. 2017, 61, 797–819. [Google Scholar] [CrossRef]
- Read-Ward, G.E.; Jones, S.P.; Davies, E.H. A comparison of self-ligating and conventional orthodontic bracket systems. Br. J. Orthod. 1997, 24, 309–317. [Google Scholar] [CrossRef]
- Chen, H.Y.; Su, M.Z.; Chang, H.F.; Chen, Y.J.; Lan, W.H.; Lin, C.P. Effects of different debonding techniques on the debonding forces and failure modes of ceramic brackets in simulated clinical set-ups. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 680–686. [Google Scholar] [CrossRef] [PubMed]
- Söderholm, K.J.M.; Shang, S.W. Molecular Orientation of Silane at the Surface of Colloidal Silica. J. Dent. Res. 1993, 72, 1050–1054. [Google Scholar] [CrossRef] [PubMed]
- RETIEF, D.H. Failure at the dental adhesive—Etched enamel interface. J. Oral Rehabil. 1974, 1, 265–284. [Google Scholar] [CrossRef] [PubMed]
- Panayi, N.C.; Tsolakis, A.I. In-house computer-aided design and 3-dimensional printing of customized orthodontic brackets using hybrid ceramic resin: Is it the time for the orthodontist to take over? AJO-DO Clin. Companion 2021, 1, 187–193. [Google Scholar] [CrossRef]
- Johnson, G.; Walker, M.P.; Kula, K. Fracture strength of ceramic bracket tie wings subjected to tension. Angle Orthod. 2005, 75, 95–100. [Google Scholar] [CrossRef]
- Eliades, G.; Grímsdóttir, M.R.; Hensten-Pettersen, A.; Jacobsen, N.; Johnston, W.M.; Kakaboura, A.; Litsky, A.S.; Messersmith, M.L.; Øgaard, B.; Papazoglou, E.; et al. Orthodontic Materials. Sci. Clin. Asp. 2001. [Google Scholar] [CrossRef]
- Iijima, M.; Muguruma, T.; Brantley, W.A.; Mizoguchi, I. Comparisons of nanoindentation, 3-point bending, and tension tests for orthodontic wires. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 65–71. [Google Scholar] [CrossRef]
- Bauer, C.A.J.; Scheurer, M.; Bourauel, C.; Kretzer, J.P.; Roser, C.J.; Lux, C.J.; Hodecker, L.D. Precision of slot widths and torque transmission of in-office 3D printed brackets: An in vitro study. J. Orofac. Orthop. 2024, 85, 327–339. [Google Scholar] [CrossRef]
- Papageorgiou, S.N.; Polychronis, G.; Panayi, N.; Zinelis, S.; Eliades, T. New aesthetic in-house 3D-printed brackets: Proof of concept and fundamental mechanical properties. Prog. Orthod. 2022, 23, 6. [Google Scholar] [CrossRef]
- Hodecker, L.; Bourauel, C.; Braumann, B.; Kruse, T.; Christ, H.; Scharf, S. Comparative in vitro analysis of the sliding resistance of a modern 3D-printed polymer bracket in combination with different archwire types. Clin. Oral Investig. 2022, 26, 4049–4057. [Google Scholar] [CrossRef]
- Hodecker, L.; Bourauel, C.; Braumann, B.; Kruse, T.; Christ, H.; Scharf, S. Sliding behaviour and surface quality after static air polishing of conventional and modern bracket materials: In vitro analysis. J. Orofac. Orthop. 2023, 84, 110–124. [Google Scholar] [CrossRef] [PubMed]
- Brucculeri, L.; Carpanese, C.; Palone, M.; Lombardo, L. In-House 3D-Printed vs. Conventional Bracket: An In Vitro Comparative Analysis of Real and Nominal Bracket Slot Heights. Appl. Sci. 2022, 12, 10120. [Google Scholar] [CrossRef]
- Hanson, M.S.; Ontiveros, J.C.; English, J.D.; Wirthlin, J.O.; Cozad, B.E.; Harrington, D.A.; Kasper, F.K. Effect of Material and Pad Abrasion on Shear Bond Strength of 3D-Printed Orthodontic Brackets. Orthod. Craniofacial Res. 2023, 26, 171–179. [Google Scholar] [CrossRef]
- Haynie, A.S.; English, J.D.; Paravina, R.D.; Moon, A.; Hanigan, J.; Abu Al Tamn, M.A.; Kasper, F.K. Colour stability of 3D-printed resin orthodontic brackets. J. Orthod. 2021, 48, 241–249. [Google Scholar] [CrossRef]
- Wallach, R.; English, J.D.; Moon, A.; Brock, R.A.; Paravina, R.D.; Kasper, F.K. Colour stability of 3D-Printed orthodontic brackets using filled resins. Orthod. Craniofacial Res. 2023, 26, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Formlabs. Permanent Crown Resin. Available online: https://dental.formlabs.com/store/materials/permanent-crown-resin-us/ (accessed on 7 August 2024).
- Formlabs. Temporary Crown Resin. Available online: https://dental.formlabs.com/store/materials/temporary-cb-resin-us/ (accessed on 7 August 2024).
- Formlabs. SG Resin. Available online: https://dental.formlabs.com/store/materials/temporary-cb-resin-us/ (accessed on 7 August 2024).
- Formlabs. LT Resin. Available online: https://dental.formlabs.com/store/materials/temporary-cb-resin-us/ (accessed on 7 August 2024).
- Matsui, S.; Umezaki, E.; Komazawa, D.; Otsuka, Y.; Suda, N. Evaluation of mechanical properties of esthetic brackets. J. Dent. Biomech. 2015, 6, 1758736015574401. [Google Scholar] [CrossRef]
- Bourauel, C.; Drescher, D.; Thier, M. An experimental apparatus for the simulation of three-dimensional movements in orthodontics. J. Biomed. Eng. 1992, 14, 371–378. [Google Scholar] [CrossRef]
- Maijer, R.; Smith, D.C. Variables influencing the bond strength of metal orthodontic bracket bases. Am. J. Orthod. 1981, 79, 20–34. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elabed, I.; Zheng, Z.; Zhang, Y.; Chung, C.-H.; Li, C. The Mechanical and Clinical Properties of Customized Orthodontic Bracket Systems—A Comprehensive Review. J. Funct. Biomater. 2024, 15, 299. https://doi.org/10.3390/jfb15100299
Elabed I, Zheng Z, Zhang Y, Chung C-H, Li C. The Mechanical and Clinical Properties of Customized Orthodontic Bracket Systems—A Comprehensive Review. Journal of Functional Biomaterials. 2024; 15(10):299. https://doi.org/10.3390/jfb15100299
Chicago/Turabian StyleElabed, Issa, Zhong Zheng, Yu Zhang, Chun-Hsi Chung, and Chenshuang Li. 2024. "The Mechanical and Clinical Properties of Customized Orthodontic Bracket Systems—A Comprehensive Review" Journal of Functional Biomaterials 15, no. 10: 299. https://doi.org/10.3390/jfb15100299
APA StyleElabed, I., Zheng, Z., Zhang, Y., Chung, C.-H., & Li, C. (2024). The Mechanical and Clinical Properties of Customized Orthodontic Bracket Systems—A Comprehensive Review. Journal of Functional Biomaterials, 15(10), 299. https://doi.org/10.3390/jfb15100299










