Natural Bred ε2-Phages Have an Improved Host Range and Virulence against Uropathogenic Escherichia coli over Their Ancestor Phages
Abstract
1. Introduction
2. Results
2.1. Isolation of Phages from Waste Water Reveales 28 Novel Phages
2.2. The Plaquing Host Range Does Not Correlate with the Ability of Phages to Control Growth in Suspension
2.3. Breeding of Myoviridae Phages Improves Their Kinetic Host Range against Uropathogenic E. coli
2.4. Myoviridae ε2-Phages Are More Virulent than Their Ancestors
2.5. The Genomes of ε2-Phages Are Intercrossed from Up to 3 Ancestors
3. Discussion
4. Materials and Methods
4.1. Bacterial Strains
4.2. Phage Collection and Propagation
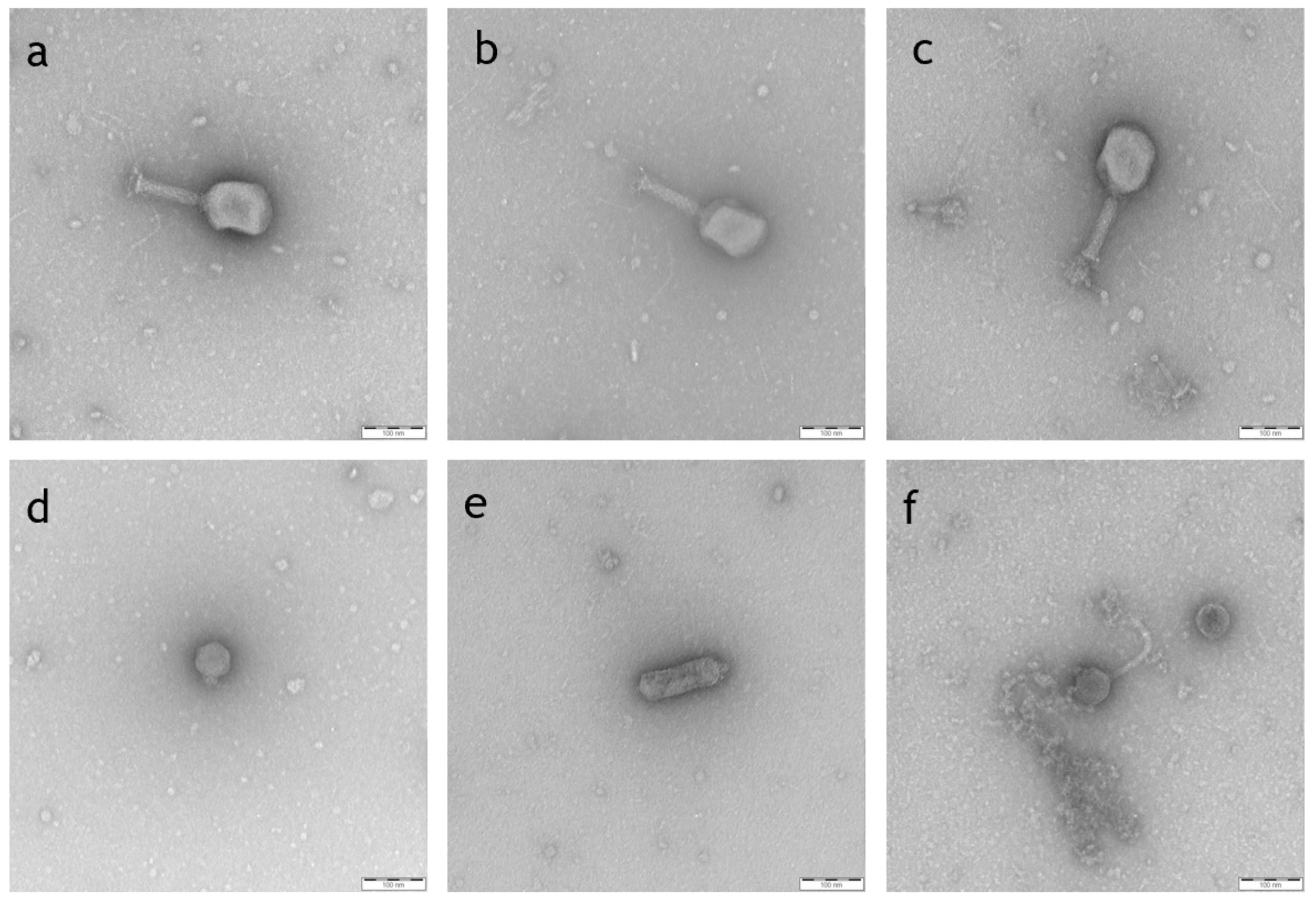
4.3. Transmission Electron Microscopy (TEM)
4.4. Plaquing Host Range (PHR) and Efficiency of Plaquing (EOP)
4.5. Kinetic Host Range (KHR)
4.6. Phage DNA Isolation
4.7. Library Preparation, Whole Genome Sequencing and Genomic Analysis
4.8. Breeding of Phages
4.9. Determination of Phage Efficiency
4.10. Statistics
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wagenlehner, F.; Pilatz, A.; Naber, K.; Weidner, W. Urinary tract infections. Aktuelle Urol. 2014, 45, 135–146. [Google Scholar]
- Abo Basha, J.; Kiel, M.; Görlich, D.; Schütte-Nütgen, K.; Witten, A.; Pavenstädt, H.; Kahl, B.C.; Dobrindt, U.; Reuter, S. Phenotypic and Genotypic Characterization of Escherichia coli Causing Urinary Tract Infections in Kidney-Transplanted Patients. J. Clin. Med. 2019, 8, 988. [Google Scholar] [CrossRef] [PubMed]
- Alghoribi, M.F.; Gibreel, T.M.; Farnham, G.; al Johani, S.M.; Balkhy, H.H.; Upton, M. Antibiotic-resistant ST38, ST131 and ST405 strains are the leading uropathogenic Escherichia coli clones in Riyadh, Saudi Arabia. J. Antimicrob. Chemother. 2015, 70, 2757–2762. [Google Scholar] [CrossRef] [PubMed]
- Croxall, G.; Hale, J.; Weston, V.; Manning, G.; Cheetham, P.; Achtman, M.; McNally, A. Molecular epidemiology of extraintestinal pathogenic Escherichia coli isolates from a regional cohort of elderly patients highlights the prevalence of ST131 strains with increased antimicrobial resistance in both community and hospital care settings. J. Antimicrob. Chemother. 2011, 66, 2501–2508. [Google Scholar] [CrossRef]
- Ismail, M.D.; Ali, I.; Hatt, S.; Salzman, E.A.; Cronenwett, A.W.; Marrs, C.F.; Rickard, A.H.; Foxman, B. Association of Escherichia coli ST131 lineage with risk of urinary tract infection recurrence among young women. J. Glob. Antimicrob. Resist. 2018, 13, 81–84. [Google Scholar] [CrossRef]
- Kudinha, T.; Johnson, J.R.; Andrew, S.D.; Kong, F.; Anderson, P.; Gilbert, G.L. Escherichia coli Sequence Type 131 as a Prominent Cause of Antibiotic Resistance among Urinary Escherichia coli Isolates from Reproductive-Age Women. J. Clin. Microbiol. 2013, 51, 3270–3276. [Google Scholar] [CrossRef]
- Matsukawa, M.; Igarashi, M.; Watanabe, H.; Qin, L.; Ohnishi, M.; Terajima, J.; Iyoda, S.; Morita-Ishihara, T.; Tateda, K.; Ishii, Y.; et al. Epidemiology and genotypic characterisation of dissemination patterns of uropathogenic Escherichia coli in a community. Epidemiol. Infect. 2019, 147, e148. [Google Scholar] [CrossRef] [PubMed]
- Rogers, B.; Sidjabat, H.E.; Paterson, D.L. Escherichia coli O25b-ST131: A pandemic, multiresistant, community-associated strain. J. Antimicrob. Chemother. 2010, 66, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Kranz, J.; Schmidt, S.; Lebert, C.; Schneidewind, L.; Vahlensieck, W.; Sester, U.; Fünfstück, R.; Helbig, S.; Hofmann, W.; Hummers, E.; et al. Epidemiology, diagnostics, therapy, prevention and management of uncomplicated bacterial outpatient acquired urinary tract infections in adult patients: Update 2017 of the interdisciplinary AWMF S3 guideline. Der. Urol. 2017, 56, 746–758. [Google Scholar] [CrossRef]
- Dalhoff, A. Global Fluoroquinolone Resistance Epidemiology and Implictions for Clinical Use. Interdiscip. Perspect. Infect. Dis. 2012, 2012, 1–37. [Google Scholar] [CrossRef]
- Van Driel, A.A.; Notermans, D.W.; Meima, A.; Mulder, M.; Donker, G.A.; Stobberingh, E.E.; Verbon, A. Antibiotic resistance of Escherichia coli isolated from uncomplicated UTI in general practice patients over a 10-year period. Eur. J. Clin. Microbiol. Infect. Dis. 2019, 38, 2151–2158. [Google Scholar] [CrossRef] [PubMed]
- Summers, W.C. The strange history of phage therapy. Bacteriophage 2012, 2, 130–133. [Google Scholar] [CrossRef]
- García, P.; Martínez, B.; Obeso, J.; Rodriguez, A. Bacteriophages and their application in food safety. Lett. Appl. Microbiol. 2008, 47, 479–485. [Google Scholar] [CrossRef] [PubMed]
- Abedon, S.T.; Kuhl, S.J.; Blasdel, B.G.; Kutter, E.M. Phage treatment of human infections. Bacteriophage 2011, 1, 66–85. [Google Scholar] [CrossRef] [PubMed]
- Kortright, K.E.; Chan, B.K.; Koff, J.L.; Turner, P.E. Phage Therapy: A Renewed Approach to Combat Antibiotic-Resistant Bacteria. Cell Host Microbe 2019, 25, 219–232. [Google Scholar] [CrossRef]
- Storms, Z.J.; Teel, M.R.; Mercurio, K.; Sauvageau, D. The Virulence Index: A Metric for Quantitative Analysis of Phage Virulence. PHAGE 2020, 1, 27–36. [Google Scholar] [CrossRef]
- Levin, B.R.; Bull, J.J. Population and evolutionary dynamics of phage therapy. Nat. Rev. Genet. 2004, 2, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Roach, D.R.; Leung, C.Y.; Henry, M.; Morello, E.; Singh, D.; Di Santo, J.P.; Weitz, J.S.; Debarbieux, L. Synergy between the Host Immune System and Bacteriophage Is Essential for Successful Phage Therapy against an Acute Respiratory Pathogen. Cell Host Microbe 2017, 22, 38–47. [Google Scholar] [CrossRef]
- Pires, D.P.; Cleto, S.; Sillankorva, S.; Azeredo, J.; Lu, T.K. Genetically Engineered Phages: A Review of Advances over the Last Decade. Microbiol. Mol. Biol. Rev. 2016, 80, 523–543. [Google Scholar] [CrossRef]
- Yehl, K.; Lemire, S.; Yang, A.C.; Ando, H.; Mimee, M.; Torres, M.D.T.; de la Fuente-Nunez, C.; Lu, T.K. Engineering Phage Host-Range and Suppressing Bacterial Resistance through Phage Tail Fiber Mutagenesis. Cell 2019, 179, 459–469.e9. [Google Scholar] [CrossRef] [PubMed]
- Selle, K.; Fletcher, J.R.; Tuson, H.; Schmitt, D.S.; McMillan, L.; Vridhambal, G.S.; Rivera, A.J.; Montgomery, S.A.; Fortier, L.-C.; Barrangou, R.; et al. In Vivo Targeting of Clostridioides difficile Using Phage-Delivered CRISPR-Cas3 Antimicrobials. mBio 2020, 11. [Google Scholar] [CrossRef]
- Hatfull, G.F.; Hendrix, R.W. Bacteriophages and their genomes. Curr. Opin. Virol. 2011, 1, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Burrowes, B.H.; Molineux, I.J.; Fralick, J.A. Directed in Vitro Evolution of Therapeutic Bacteriophages: The Appelmans Protocol. Viruses 2019, 11, 241. [Google Scholar] [CrossRef]
- Rohde, C.; Resch, G.; Pirnay, J.-P.; Blasdel, B.G.; Debarbieux, L.; Gelman, D.; Górski, A.; Hazan, R.; Huys, I.; Kakabadze, E.; et al. Expert Opinion on Three Phage Therapy Related Topics: Bacterial Phage Resistance, Phage Training and Prophages in Bacterial Production Strains. Viruses 2018, 10, 178. [Google Scholar] [CrossRef] [PubMed]
- Hershey, A.D.; Rotman, R. Genetic recombination between host-range and plaque-type mutants of bacteriophage in single bacterial cells. Genetics 1949, 34, 44–71. [Google Scholar] [CrossRef]
- Dion, M.B.; Oechslin, F.; Moineau, S. Phage diversity, genomics and phylogeny. Nat. Rev. Microbiol. 2020, 18, 125–138. [Google Scholar] [CrossRef] [PubMed]
- Gibson, S.B.; Green, S.I.; Liu, C.G.; Salazar, K.C.; Clark, J.R.; Terwilliger, A.L.; Kaplan, H.B.; Maresso, A.W.; Trautner, B.W.; Ramig, R.F. Constructing and Characterizing Bacteriophage Libraries for Phage Therapy of Human Infections. Front. Microbiol. 2019, 10, 1–17. [Google Scholar] [CrossRef]
- Mapes, A.C.; Trautner, B.W.; Liao, K.S.; Ramig, R.F. Development of expanded host range phage active on biofilms of multi-drug resistantPseudomonas aeruginosa. Bacteriophage 2016, 6, e1096995. [Google Scholar] [CrossRef]
- Moreno, D.S.; Visram, Z.; Mutti, M.; Restrepo-Córdoba, M.; Hartmann, S.; Kremers, A.; Tišáková, L.; Schertler, S.; Wittmann, J.; Kalali, B.; et al. ε2-Phages Are Naturally Bred and Have a Vastly Improved Host Range in Staphylococcus aureus over Wild Type Phages. Pharmaceuticals 2021, 14, 325. [Google Scholar] [CrossRef] [PubMed]
- Korf, I.H.E.; Meier-Kolthoff, J.P.; Adriaenssens, E.M.; Kropinski, A.M.; Nimtz, M.; Rohde, M.; Van Raaij, M.J.; Wittmann, J. Still Something to Discover: Novel Insights into Escherichia coli Phage Diversity and Taxonomy. Viruses 2019, 11, 454. [Google Scholar] [CrossRef]
- Perepanova, T.; Darbeeva, O.S.; Kotliarova, G.A.; Kondrat’eva, E.M.; Maĭskaia, L.M.; Malysheva, V.; Baĭguzina, F.A.; Grishkova, N.V. The efficacy of bacteriophage preparations in treating inflammatory urologic diseases. Urologiia i Nefrologiia 1995, 1995, 14–17. [Google Scholar]
- Nishikawa, H.; Yasuda, M.; Uchiyama, J.; Rashel, M.; Maeda, Y.; Takemura, I.; Sugihara, S.; Ujihara, T.; Shimizu, Y.; Shuin, T.; et al. T-even-related bacteriophages as candidates for treatment of Escherichia coli urinary tract infections. Arch. Virol. 2008, 153, 507–515. [Google Scholar] [CrossRef]
- Ujmajuridze, A.; Chanishvili, N.; Goderdzishvili, M.; Leitner, L.; Mehnert, U.; Chkhotua, A.; Kessler, T.M.; Sybesma, W. Adapted Bacteriophages for Treating Urinary Tract Infections. Front. Microbiol. 2018, 9, 1832. [Google Scholar] [CrossRef] [PubMed]
- Sybesma, W.; Zbinden, R.; Chanishvili, N.; Kutateladze, M.; Chkhotua, A.; Ujmajuridze, A.; Mehnert, U.; Kessler, T.M. Bacteriophages as Potential Treatment for Urinary Tract Infections. Front. Microbiol. 2016, 7, 465. [Google Scholar] [CrossRef]
- Mutti, M.; Corsini, L. Robust Approaches for the Production of Active Ingredient and Drug Product for Human Phage Therapy. Front. Microbiol. 2019, 10, 2289. [Google Scholar] [CrossRef]
- Borin, J.M.; Avrani, S.; Barrick, J.E.; Petrie, K.L.; Meyer, J.R. Coevolutionary phage training leads to greater bacterial suppression and delays the evolution of phage resistance. Proc. Natl. Acad. Sci. USA 2021, 118, e2104592118. [Google Scholar] [CrossRef] [PubMed]
- Holtzman, T.; Globus, R.; Molshanski-Mor, S.; Ben-Shem, A.; Yosef, I.; Qimron, U. A continuous evolution system for contracting the host range of bacteriophage T7. Sci. Rep. 2020, 10, 1–8. [Google Scholar] [CrossRef]
- Morona, R.; Henning, U. Host range mutants of bacteriophage Ox2 can use two different outer membrane proteins of Escherichia coli K-12 as receptors. J. Bacteriol. 1984, 159, 579–582. [Google Scholar] [CrossRef]
- Tétart, F.; Repoila, F.; Monod, C.; Krisch, H. Bacteriophage T4 Host Range is Expanded by Duplications of a Small Domain of the Tail Fiber Adhesin. J. Mol. Biol. 1996, 258, 726–731. [Google Scholar] [CrossRef]
- Kunisaki, H.; Tanji, Y. Intercrossing of phage genomes in a phage cocktail and stable coexistence with Escherichia coli O157:H7 in anaerobic continuous culture. Appl. Microbiol. Biotechnol. 2009, 85, 1533–1540. [Google Scholar] [CrossRef]
- Nóbrega, F.; Vlot, M.; de Jonge, P.A.; Dreesens, L.L.; Beaumont, H.J.E.; Lavigne, R.; Dutilh, B.E.; Brouns, S.J.J. Targeting mechanisms of tailed bacteriophages. Nat. Rev. Genet. 2018, 16, 760–773. [Google Scholar] [CrossRef] [PubMed]
- Clermont, O.; Lavollay, M.; Vimont, S.; Deschamps, C.; Forestier, C.; Branger, C.; Denamur, E.; Arlet, G. The CTX-M-15-producing Escherichia coli diffusing clone belongs to a highly virulent B2 phylogenetic subgroup. J. Antimicrob. Chemother. 2008, 61, 1024–1028. [Google Scholar] [CrossRef]
- Dufour, N.; Clermont, O.; La Combe, B.; Messika, J.; Dion, S.; Khanna, V.; Denamur, E.; Ricard, J.D.; Debarbieux, L.; ColoColi Group. Bacteriophage LM33_P1, a fast-acting weapon against the pandemic ST131-O25b: H4 Escherichia coli clonal complex. J. Antimicrob. Chemother. 2016, 71, 3072–3080. [Google Scholar] [CrossRef] [PubMed]
- O’Flynn, G.; Coffey, A.; Fitzgerald, G.; Ross, R. The newly isolated lytic bacteriophages st104a and st104b are highly virulent against Salmonella enterica. J. Appl. Microbiol. 2006, 101, 251–259. [Google Scholar] [CrossRef]
- De Melo, A.C.C.; Gomes, A.D.M.; Melo, F.L.; Ardisson-Araújo, D.M.P.; De Vargas, A.P.C.; Ely, V.L.; Kitajima, E.W.; Ribeiro, B.M.; Wolff, J.L.C. Characterization of a bacteriophage with broad host range against strains of Pseudomonas aeruginosa isolated from domestic animals. BMC Microbiol. 2019, 19, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Pirnay, J.-P.; Verbeken, G.; Ceyssens, P.-J.; Huys, I.; de Vos, D.; Ameloot, C.; Fauconnier, A.; Pirnay, J.-P.; Verbeken, G.; Ceyssens, P.-J.; et al. The Magistral Phage. Viruses 2018, 10, 64. [Google Scholar] [CrossRef]
- Aslam, S.; Lampley, E.; Wooten, D.; Karris, M.; Benson, C.; Strathdee, S.; Schooley, R.T. Lessons Learned From the First 10 Consecutive Cases of Intravenous Bacteriophage Therapy to Treat Multidrug-Resistant Bacterial Infections at a Single Center in the United States. Open Forum Infect. Dis. 2020, 7. [Google Scholar] [CrossRef]
- Picard, B.; Garcia, J.S.; Gouriou, S.; Duriez, P.; Brahimi, N.; Bingen, E.; Elion, J.; Denamur, E. The Link between Phylogeny and Virulence in Escherichia coli Extraintestinal Infection. Infect. Immun. 1999, 67, 546–553. [Google Scholar] [CrossRef]
- Chen, M.; Zhang, L.; Abdelgader, S.A.; Yu, L.; Xu, J.; Yao, H.; Lu, C.; Zhang, W. Alterations in gp37 Expand the Host Range of a T4-Like Phage. Appl. Environ. Microbiol. 2017, 83, e01576-17. [Google Scholar] [CrossRef]
- Chattopadhyay, S.; Paul, S.; Kisiela, D.I.; Linardopoulou, E.V.; Sokurenko, E.V. Convergent Molecular Evolution of Genomic Cores in Salmonella enterica and Escherichia coli. J. Bacteriol. 2012, 194, 5002–5011. [Google Scholar] [CrossRef][Green Version]
- Hendrickson, H. Order and Disorder during Escherichia coli Divergence. PLoS Genet. 2009, 5, e1000335. [Google Scholar] [CrossRef][Green Version]
- Yang, Z.; Luo, H.; Zhang, Y.; Wang, B.; Gao, F. Pan-genomic analysis provides novel insights into the association of E.coli with human host and its minimal genome. Bioinformatics 2018, 35, 1987–1991. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, S.; Mehlan, H.; Bernhardt, J.; Hennig, A.; Michalik, S.; Surmann, K.; Pané-Farré, J.; Giese, A.; Weiss, S.; Backert, L.; et al. AureoWiki ̵ The repository of the Staphylococcus aureus research and annotation community. Int. J. Med. Microbiol. 2018, 308, 558–568. [Google Scholar] [CrossRef] [PubMed]
- Mutalik, V.K.; Adler, B.A.; Rishi, H.S.; Piya, D.; Zhong, C.; Koskella, B.; Kutter, E.M.; Calendar, R.; Novichkov, P.S.; Price, M.N.; et al. High-troughput mapping of the phage resistance landscape in E. coli. PLoS Biol. 2020, 18, e3000877. [Google Scholar] [CrossRef] [PubMed]
- Altamirano, F.L.G.; Barr, J.J. Unlocking the next generation of phage therapy: The key is in the receptors. Curr. Opin. Biotechnol. 2020, 68, 115–123. [Google Scholar] [CrossRef]
- Stickler, D.J.; Morris, N.S.; Winters, C. Simple physical model to study formation and physiology of biofilms on urethral catheters. Methods Enzymol. 1999, 310, 494–501. [Google Scholar] [CrossRef]
- Dreiseikelmann, B.; Bunk, B.; Spröer, C.; Rohde, M.; Nimtz, M.; Wittmann, J. Characterization and genome comparisons of three Achromobacter phages of the family Siphoviridae. Arch. Virol. 2017, 162, 2191–2201. [Google Scholar] [CrossRef]
- Ackermann, H.-W. Frequency of morphological phage descriptions in the year 2000. Arch. Virol. 2001, 146, 843–857. [Google Scholar] [CrossRef]
- Yamamoto, K.R.; Alberts, B.M.; Benzinger, R.; Lawhorne, L.; Treiber, G. Rapid bacteriophage sedimentation in the presence of polyethylene glycol and its application to large-scale virus purification. Virology 1970, 40, 734–744. [Google Scholar] [CrossRef]
- Schmieder, R.; Edwards, R. Quality control and preprocessing of metagenomic datasets. Bioinformatics 2011, 27, 863–864. [Google Scholar] [CrossRef]
- Andrews, S. FastQC: A Quality Control Tool for High Throughput Sequence Data. 2010. Available online: http://www.bioinformatics.babraham.ac.uk/projects/fastqc/ (accessed on 13 April 2021).
- Bankevich, A.; Nurk, S.; Antipov, D.; Gurevich, A.A.; Dvorkin, M.; Kulikov, A.S.; Lesin, V.M.; Nikolenko, S.I.; Pham, S.; Prjibelski, A.D.; et al. SPAdes: A new genome assembly algorithm and its applications to single-cell sequencing. J. Comput. Biol. 2012, 19, 455–477. [Google Scholar] [CrossRef]
- Seemann, T. Prokka: Rapid prokaryotic genome annotation. Bioinformatics 2014, 30, 2068–2069. [Google Scholar] [CrossRef] [PubMed]
- McNair, K.; Bailey, B.A.; Edwards, R.A. PHACTS, a computational approach to classifying the lifestyle of phages. Bioinformatics 2012, 28, 614–618. [Google Scholar] [CrossRef]
- Bortolaia, V.; Kaas, R.S.; Ruppe, E.; Roberts, M.C.; Schwarz, S.; Cattoir, V.; Philippon, A.; Allesoe, R.L.; Rebelo, A.R.; Florensa, A.F.; et al. ResFinder 4.0 for predictions of phenotypes from genotypes. J. Antimicrob. Chemother. 2020, 75, 3491–3500. [Google Scholar] [CrossRef] [PubMed]
- Alcock, B.P.; Raphenya, A.R.; Lau, T.T.Y.; Tsang, K.K.; Bouchard, M.; Edalatmand, A.; Huynh, W.; Nguyen, A.-L.V.; A Cheng, A.; Liu, S.; et al. CARD 2020: Antibiotic resistome surveillance with the comprehensive antibiotic resistance database. Nucleic Acids Res. 2019, 48, D517–D525. [Google Scholar] [CrossRef]
- Joensen, K.G.; Scheutz, F.; Lund, O.; Hasman, H.; Kaas, R.S.; Nielsen, E.M.; Aarestrup, F.M. Real-Time Whole-Genome Sequencing for Routine Typing, Surveillance, and Outbreak Detection of Verotoxigenic Escherichia coli. J. Clin. Microbiol. 2014, 52, 1501–1510. [Google Scholar] [CrossRef] [PubMed]
- Tetzschner, A.M.M.; Johnson, J.R.; Johnston, B.D.; Lund, O.; Scheutz, F. In Silico Genotyping of Escherichia coli Isolates for Extraintestinal Virulence Genes by Use of Whole-Genome Sequencing Data. J. Clin. Microbiol. 2020, 58, e01269-20. [Google Scholar] [CrossRef]





| Order | Family | Subfamily | Genus | Phage Name | Genome Length bp | Host Strain: E. coli # | Accession Number | HR * [%] |
|---|---|---|---|---|---|---|---|---|
| Caudovirales | Autographiviridae | Molineuxvirinae | Vectrevirus | 101101UKE1 | 44450 | DSM101101 | MZ234012 | 19 |
| UTI89UKE2 | 44293 | UTI89 | MZ234049 | 3 | ||||
| UTI89UKE3 | 44294 | UTI89 | MZ234050 | 4 | ||||
| unspecified | 101117UKE2 | 44526 | DSM101117 | MZ234019 | 8 | |||
| 101118B1 | 44526 | DSM101118 | MZ234020 | 51 | ||||
| Studiervirinae | Kayfunavirus | 101118UKE1 | 40233 | DSM101118 | MZ234021 | 41 | ||
| 101120B1-2 | 39845 | DSM101120 | MZ234022 | 19 | ||||
| 101120B2 | 39899 | DSM101120 | MZ234023 | 34 | ||||
| 101136BS1 | 39375 | DSM101136 | MZ234024 | 44 | ||||
| 22664BS1 | 39133 | DSM22664 | MZ234009 | 42 | ||||
| 22664UKE3-2 | 40482 | DSM22664 | MZ234011 | 61 | ||||
| Myoviridae | Tevenvirinae | Mosigvirus | 172859UKE1 | 168667 | 172859 | MZ234025 | 4 | |
| Tequatrovirus | 101112UKE3-1 | 169555 | DSM101112 | MZ234013 | 37 | |||
| 101117BS1 | 167080 | DSM101117 | MZ234018 | 23 | ||||
| CHD16UKE1 | 168543 | CHD16 | MZ234030 | 42 | ||||
| CHD2BS1 | 168577 | CHD2 | MZ234027 | 13 | ||||
| CHD94UKE2 | 167922 | CHD94 | MZ234031 | 29 | ||||
| G3G7 | 168649 | CHD16 | MZ234040 | n.d. | ||||
| Podo-viridae | [x] | Kuravirus | 101114BS3 | 75747 | DSM101114 | MZ234015 | 53 | |
| 101114UKE3 | 75747 | DSM101114 | MZ234017 | 32 | ||||
| CHD5UKE1 | 77359 | CHD5 | MZ234028 | 1 | ||||
| Siphoviridae | [x] | Dhillonvirus | 101114B2 | 44971 | DSM101114 | MZ234014 | 38 | |
| 101114BS4 | 45251 | DSM101114 | MZ234016 | 27 | ||||
| 22664B1 | 45019 | DSM22664 | MZ234008 | 41 | ||||
| CHD2B1 | 45144 | CHD2 | MZ234026 | 15 | ||||
| CHD5UKE2 | 45243 | CHD5 | MZ234029 | 24 | ||||
| UTI89UKE1 | 41265 | UTI89 | MZ234048 | 1 | ||||
| Guernseyvirinae | Kagunavirus | 22664BS2 | 45176 | DSM22664 | MZ234010 | 43 |
| Sequence Type | Phylogenetic Group | Number of Isolates Used in This Study | % of Total Strains in This Study | Literature a Range % of Strains |
|---|---|---|---|---|
| ST131 | B2 | 6 | 13% | 7.7–29 |
| ST95 | B2 | 1 | 2% | 3–28.9 |
| ST73 | B2 | 3 | 6% | 8.8–11 |
| ST69 | D | 3 | 6% | 3–9 |
| ST38 | D | 1 | 2% | 1.2–7 |
| ST10 | A | 2 | 4% | 1.8–6.4 |
| ST127 | B2 | 1 | 2% | 0.6–5.9 |
| ST141 | B2 | 1 | 2% | 4.4 |
| ST12 | B2 | 1 | 2% | 1.2–3.8 |
| ST405 | D | 1 | 2% | 0.6–3 |
| ST624 | D | 2 | 4% | 1.5 |
| ST23 | A | 1 | 2% | 1.5 |
| ST93 | A | 1 | 2% | 1,2 |
| ST101 | B1 | 1 | 2% | 1 |
| ST167 | A | 1 | 2% | 1 |
| ST162 | AxB1 | 1 | 2% | 0.6–1 |
| ST2020 | n.d. | 1 | 2% | 0.5 |
| ST90 | A | 1 | 2% | n.d. |
| ST399 | A (AxB1) | 1 | 2% | n.d. |
| ST226 | A0 | 1 | 2% | n.d. |
| ST453 | ABD | 1 | 2% | n.d. |
| ST446 | B1 | 1 | 2% | n.d. |
| ST126 | B2 | 1 | 2% | n.d. |
| ST135 | B2 | 1 | 2% | n.d. |
| ST5640 | B2 | 1 | 2% | n.d. |
| ST648 | D/F | 1 | 2% | n.d. |
| ST117 | F (B1/D) | 1 | 2% | n.d. |
| ST1007 | n.d. | 1 | 2% | n.d. |
| ST1064 | n.d. | 1 | 2% | n.d. |
| ST1851 | n.d. | 1 | 2% | n.d. |
| ST3077 | n.d. | 1 | 2% | n.d. |
| Not determined | n.d. | 5 | 11% | n.d. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Loose, M.; Sáez Moreno, D.; Mutti, M.; Hitzenhammer, E.; Visram, Z.; Dippel, D.; Schertler, S.; Tišáková, L.P.; Wittmann, J.; Corsini, L.; et al. Natural Bred ε2-Phages Have an Improved Host Range and Virulence against Uropathogenic Escherichia coli over Their Ancestor Phages. Antibiotics 2021, 10, 1337. https://doi.org/10.3390/antibiotics10111337
Loose M, Sáez Moreno D, Mutti M, Hitzenhammer E, Visram Z, Dippel D, Schertler S, Tišáková LP, Wittmann J, Corsini L, et al. Natural Bred ε2-Phages Have an Improved Host Range and Virulence against Uropathogenic Escherichia coli over Their Ancestor Phages. Antibiotics. 2021; 10(11):1337. https://doi.org/10.3390/antibiotics10111337
Chicago/Turabian StyleLoose, Maria, David Sáez Moreno, Michele Mutti, Eva Hitzenhammer, Zehra Visram, David Dippel, Susanne Schertler, Lenka Podpera Tišáková, Johannes Wittmann, Lorenzo Corsini, and et al. 2021. "Natural Bred ε2-Phages Have an Improved Host Range and Virulence against Uropathogenic Escherichia coli over Their Ancestor Phages" Antibiotics 10, no. 11: 1337. https://doi.org/10.3390/antibiotics10111337
APA StyleLoose, M., Sáez Moreno, D., Mutti, M., Hitzenhammer, E., Visram, Z., Dippel, D., Schertler, S., Tišáková, L. P., Wittmann, J., Corsini, L., & Wagenlehner, F. (2021). Natural Bred ε2-Phages Have an Improved Host Range and Virulence against Uropathogenic Escherichia coli over Their Ancestor Phages. Antibiotics, 10(11), 1337. https://doi.org/10.3390/antibiotics10111337






