Increased Susceptibility of Mycobacterium tuberculosis to Ethionamide by Expressing PPs-Induced Rv0560c
Abstract
1. Introduction
2. Results
2.1. Exploring PPs-Induced Alterations of Gene Expression in M. tuberculosis
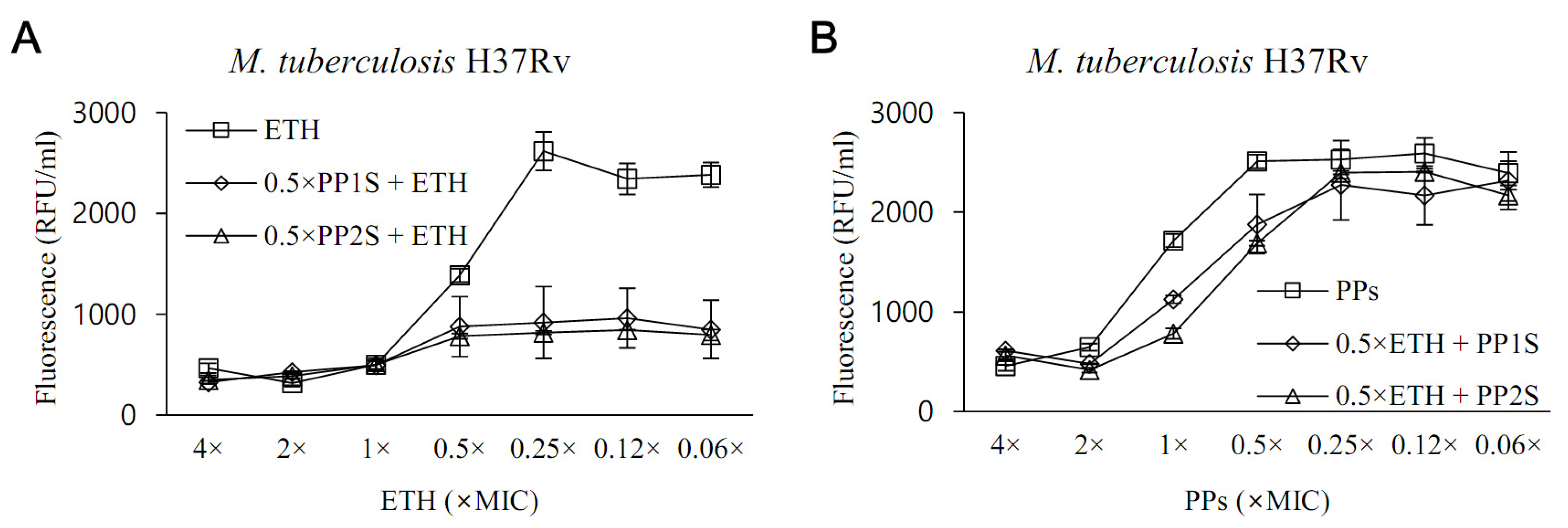
2.2. ETH-Boosting Activity of PPs
2.3. Interaction between Rv2887, a Repressor of Rv0560c, and PPs
3. Discussion
4. Method
4.1. M. tuberculosis Strains
4.2. Drugs
4.3. Exploration of Gene Expression of M. tuberculosis Changed by Drugs
4.4. Microarray
4.5. 2DE
4.6. Confirmation of Overexpression of Rv0560c Gene Using Real-Time PCR and Western Blot
4.7. Protein Microarray
4.8. In Silico Protein Modeling and Docking
4.9. SPR Analysis
4.10. In Vitro Evaluation of the Synergistic Anti-Tuberculosis Effect
4.11. Evaluation of ETH-Boosting Effect in a Pulmonary Tuberculosis Mouse Model
4.12. Synthesis of Proteins and Preparation of Polyclonal Antisera
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Global Tuberculosis Report 2021; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Hameed, H.M.A.; Islam, M.M.; Chhotaray, C.; Wang, C.; Liu, Y.; Tan, Y.; Li, X.; Tan, S.; Delorme, V.; Yew, W.W.; et al. Molecular Targets Related Drug Resistance Mechanisms in MDR-, XDR-, and TDR-Mycobacterium tuberculosis Strains. Front. Cell. Infect. Microbiol. 2018, 8, 114. [Google Scholar] [CrossRef]
- Antituberculosis Agents. In LiverTox: Clinical and Research Information on Drug-Induced Liver Injury; National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda, MD, USA, 2012.
- Shehzad, A.; Rehman, G.; Ul-Islam, M.; Khattak, W.A.; Lee, Y.S. Challenges in the development of drugs for the treatment of tuberculosis. Braz. J. Infect. Dis. 2013, 17, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Perveen, S.; Kumari, D.; Singh, K.; Sharma, R. Tuberculosis drug discovery: Progression and future interventions in the wake of emerging resistance. Eur. J. Med. Chem. 2022, 229, 114066. [Google Scholar] [CrossRef] [PubMed]
- Seo, H.; Kim, S.; Mahmud, H.A.; Islam, M.I.; Yoon, Y.; Cho, H.D.; Nam, K.W.; Choi, J.; Gil, Y.S.; Lee, B.E.; et al. A novel class of antimicrobial drugs selectively targets a Mycobacterium tuberculosis PE-PGRS protein. PLoS Biol. 2022, 20, e3001648. [Google Scholar] [CrossRef] [PubMed]
- Pepperell, C.S. Evolution of Tuberculosis Pathogenesis. Ann. Rev. Microbiol. 2022, 76, 661–680. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Cheng, S.J.; Zhang, H.; Zhang, Y. Salicylate uniquely induces a 27-kDa protein in tubercle bacillus. FEMS Microbiol. Lett. 2001, 203, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Schuessler, D.L.; Parish, T. The promoter of Rv0560c is induced by salicylate and structurally-related compounds in Mycobacterium tuberculosis. PLoS ONE 2012, 7, e34471. [Google Scholar] [CrossRef]
- Engohang-Ndong, J.; Baillat, D.; Aumercier, M.; Bellefontaine, F.; Besra, G.S.; Locht, C.; Baulard, A.R. EthR, a repressor of the TetR/CamR family implicated in ethionamide resistance in mycobacteria, octamerizes cooperatively on its operator. Mol. Microbiol. 2004, 51, 175–188. [Google Scholar] [CrossRef] [PubMed]
- Flipo, M.; Desroses, M.; Lecat-Guillet, N.; Dirie, B.; Carette, X.; Leroux, F.; Piveteau, C.; Demirkaya, F.; Lens, Z.; Rucktooa, P.; et al. Ethionamide boosters: Synthesis, biological activity, and structure-activity relationships of a series of 1,2,4-oxadiazole EthR inhibitors. J. Med. Chem. 2011, 54, 2994–3010. [Google Scholar] [CrossRef] [PubMed]
- Katawera, V.; Siedner, M.; Boum, Y., 2nd. Evaluation of the modified colorimetric resazurin microtiter plate-based antibacterial assay for rapid and reliable tuberculosis drug susceptibility testing. BMC Microbiol. 2014, 14, 259. [Google Scholar] [CrossRef] [PubMed]
- Minch, K.J.; Rustad, T.R.; Peterson, E.J.; Winkler, J.; Reiss, D.J.; Ma, S.; Hickey, M.; Brabant, W.; Morrison, B.; Turkarslan, S.; et al. The DNA-binding network of Mycobacterium tuberculosis. Nat. Commun. 2015, 6, 5829. [Google Scholar] [CrossRef]
- Winglee, K.; Lun, S.; Pieroni, M.; Kozikowski, A.; Bishai, W. Mutation of Rv2887, a marR-like gene, confers Mycobacterium tuberculosis resistance to an imidazopyridine-based agent. Antimicrob. Agents Chemother. 2015, 59, 6873–6881. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.R.; Li, D.F.; Fleming, J.; Zhou, Y.F.; Liu, Y.; Deng, J.Y.; Zhou, L.; Zhou, J.; Zhu, G.F.; Zhang, X.E.; et al. Structural analysis of the regulatory mechanism of MarR protein Rv2887 in M. tuberculosis. Sci. Rep. 2017, 7, 6471. [Google Scholar] [CrossRef]
- Baulard, A.R.; Betts, J.C.; Engohang-Ndong, J.; Quan, S.; McAdam, R.A.; Brennan, P.J.; Locht, C.; Besra, G.S. Activation of the pro-drug ethionamide is regulated in mycobaeteria. J. Biol. Chem. 2000, 275, 28326–28331. [Google Scholar] [CrossRef] [PubMed]
- Willand, N.; Dirie, B.; Carette, X.; Bifani, P.; Singhal, A.; Desroses, M.; Leroux, F.; Willery, E.; Mathys, V.; Deprez-Poulain, R.; et al. Synthetic EthR inhibitors boost antituberculous activity of ethionamide. Nat. Med. 2009, 15, 537–544. [Google Scholar] [CrossRef]
- Blondiaux, N.; Moune, M.; Desroses, M.; Frita, R.; Flipo, M.; Mathys, V.; Soetaert, K.; Kiass, M.; Delorme, V.; Djaout, K.; et al. Reversion of antibiotic resistance in Mycobacterium tuberculosis by spiroisoxazoline SMARt-420. Science 2017, 355, 1206–1211. [Google Scholar] [CrossRef] [PubMed]
- Rahim, M.A.; Seo, H.; Kim, S.; Jeong, Y.K.; Tajdozian, H.; Kim, M.; Lee, S.; Song, H.Y. A Clinical Trial to Evaluate the Efficacy of alpha-Viniferin in Staphylococcus aureus—Specific Decolonization without Depleting the Normal Microbiota of Nares. Pol. J. Microbiol. 2021, 70, 117–130. [Google Scholar] [CrossRef] [PubMed]
- Cole, S.T.; Brosch, R.; Parkhill, J.; Garnier, T.; Churcher, C.; Harris, D.; Gordon, S.V.; Eiglmeier, K.; Gas, S.; Barry, C.E., 3rd; et al. Deciphering the biology of Mycobacterium tuberculosis from the complete genome sequence. Nature 1998, 393, 537–544. [Google Scholar] [CrossRef]
- Tavazoie, S.; Hughes, J.D.; Campbell, M.J.; Cho, R.J.; Church, G.M. Systematic determination of genetic network architecture. Nat. Genet. 1999, 22, 281–285. [Google Scholar] [CrossRef] [PubMed]
- Boldrick, J.C.; Alizadeh, A.A.; Diehn, M.; Dudoit, S.; Liu, C.L.; Belcher, C.E.; Botstein, D.; Staudt, L.M.; Brown, P.O.; Relman, D.A. Stereotyped and specific gene expression programs in human innate immune responses to bacteria. Proc. Natl. Acad. Sci. USA 2002, 99, 972–977. [Google Scholar] [CrossRef] [PubMed]
- Bahk, Y.Y.; Kim, S.A.; Kim, J.S.; Euh, H.J.; Bai, G.H.; Cho, S.N.; Kim, Y.S. Antigens secreted from Mycobacterium tuberculosis: Identification by proteomics approach and test for diagnostic marker. Proteomics 2004, 4, 3299–3307. [Google Scholar] [CrossRef]
- Gobom, J.; Nordhoff, E.; Mirgorodskaya, E.; Ekman, R.; Roepstorff, P. Sample purification and preparation technique based on nano-scale reversed-phase columns for the sensitive analysis of complex peptide mixtures by matrix-assisted laser desorption/ionization mass spectrometry. J. Mass Spectrom. 1999, 34, 105–116. [Google Scholar] [CrossRef]
- Kim, S.; Seo, H.; Al Mahmud, H.; Islam, M.I.; Kim, Y.S.; Lyu, J.W.; Nam, K.W.; Lee, B.E.; Lee, K.I.; Song, H.Y. In Vitro Effect of DFC-2 on Mycolic Acid Biosynthesis in Mycobacterium tuberculosis. J. Microbiol. Biotechnol. 2017, 27, 1932–1941. [Google Scholar] [CrossRef]
- Zerin, T.; Lee, M.; Jang, W.S.; Nam, K.W.; Song, H.Y. Ursolic Acid Reduces Mycobacterium tuberculosis-Induced Nitric Oxide Release in Human Alveolar A549 cells. Mol. Cells 2015, 38, 610–615. [Google Scholar] [CrossRef]
- Hurdle, J.G.; Lee, R.B.; Budha, N.R.; Carson, E.I.; Qi, J.; Scherman, M.S.; Cho, S.H.; McNeil, M.R.; Lenaerts, A.J.; Franzblau, S.G.; et al. A microbiological assessment of novel nitrofuranylamides as anti-tuberculosis agents. J. Antimicrob. Chemother. 2008, 62, 1037–1045. [Google Scholar] [CrossRef]
- Islam, M.I.; Han, C.M.; Seo, H.; Kim, S.; Al Mahmud, H.; Nam, K.W.; Lee, B.E.; Sadu, V.S.; Lee, K.I.; Song, H.Y. In vitro activity of DNF-3 against drug-resistant Mycobacterium tuberculosis. Int. J. Antimicrob. Agents 2019, 54, 69–74. [Google Scholar] [CrossRef]




| Organism a | Antibiotic b Combination | FICA c | FICB c | FIC d |
|---|---|---|---|---|
| M. tuberculosis H37Rv | PP1S + INH | 1 | 1 | 2 |
| PP1S + RIF | 0.125 | 1 | 1.125 | |
| PP1S + STR | 1 | 0.125 | 1.125 | |
| PP1S + PZA | 1 | 1 | 2 | |
| PP1S + EMB | 1 | 1 | 2 | |
| PP2S + INH | 0.5 | 1 | 1.5 | |
| PP2S + RIF | 0.125 | 1 | 1.125 | |
| PP2S + STR | 1 | 0.125 | 1.125 | |
| PP2S + PZA | 0.5 | 1 | 1.5 | |
| PP2S + EMB | 1 | 1 | 2 | |
| XDR M. tuberculosis | PP1S + INH | 0.06 | 1 | 1.06 |
| PP1S + RIF | 0.5 | 1 | 1.5 | |
| PP1S + STR | 0.125 | 1 | 1.125 | |
| PP1S + PZA | 0.5 | 1 | 1.5 | |
| PP1S + EMB | 1 | 1 | 2 | |
| PP2S + INH | 0.25 | 1 | 1.25 | |
| PP2S + RIF | 1 | 1 | 2 | |
| PP2S + STR | 1 | 0.06 | 1.06 | |
| PP2S + PZA | 1 | 1 | 2 | |
| PP2S + EMB | 0.5 | 1 | 1.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seo, H.; Kim, S.; Mahmud, H.A.; Sultana, O.F.; Lee, Y.; Yoon, Y.; Rahim, M.A.; Jo, S.; Choi, J.; Lee, S.; et al. Increased Susceptibility of Mycobacterium tuberculosis to Ethionamide by Expressing PPs-Induced Rv0560c. Antibiotics 2022, 11, 1349. https://doi.org/10.3390/antibiotics11101349
Seo H, Kim S, Mahmud HA, Sultana OF, Lee Y, Yoon Y, Rahim MA, Jo S, Choi J, Lee S, et al. Increased Susceptibility of Mycobacterium tuberculosis to Ethionamide by Expressing PPs-Induced Rv0560c. Antibiotics. 2022; 11(10):1349. https://doi.org/10.3390/antibiotics11101349
Chicago/Turabian StyleSeo, Hoonhee, Sukyung Kim, Hafij Al Mahmud, Omme Fatema Sultana, Youngkyoung Lee, Youjin Yoon, Md Abdur Rahim, Sujin Jo, Jiwon Choi, Saebim Lee, and et al. 2022. "Increased Susceptibility of Mycobacterium tuberculosis to Ethionamide by Expressing PPs-Induced Rv0560c" Antibiotics 11, no. 10: 1349. https://doi.org/10.3390/antibiotics11101349
APA StyleSeo, H., Kim, S., Mahmud, H. A., Sultana, O. F., Lee, Y., Yoon, Y., Rahim, M. A., Jo, S., Choi, J., Lee, S., & Song, H.-Y. (2022). Increased Susceptibility of Mycobacterium tuberculosis to Ethionamide by Expressing PPs-Induced Rv0560c. Antibiotics, 11(10), 1349. https://doi.org/10.3390/antibiotics11101349








