Cisplatin-Induced Kidney Toxicity: Potential Roles of Major NAD+-Dependent Enzymes and Plant-Derived Natural Products
Abstract
:1. Introduction
2. Methods
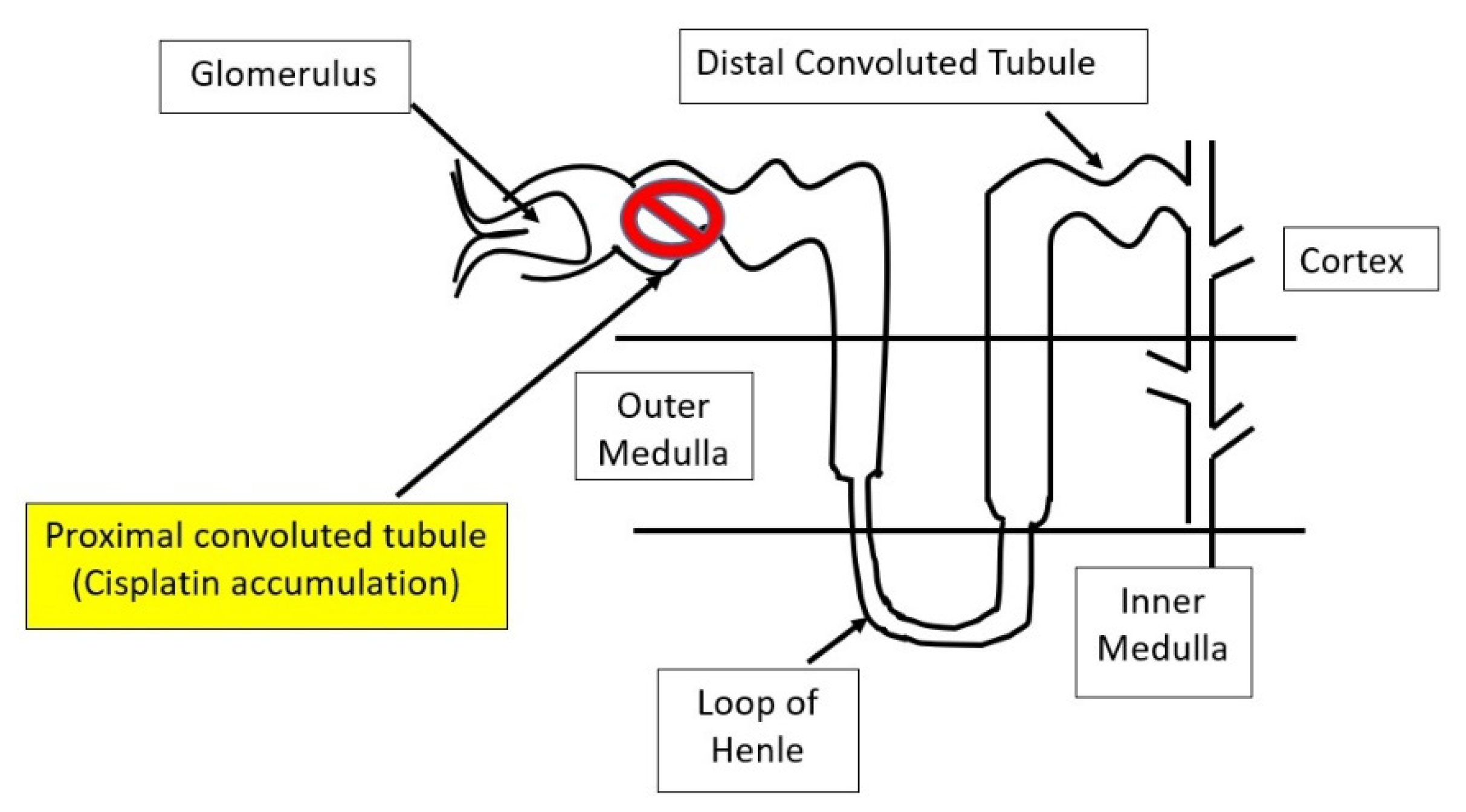
3. Major Molecular Mechanisms of Cisplatin-Induced Kidney Injury
4. Rodent Models of Cisplatin-Induced Kidney Injury
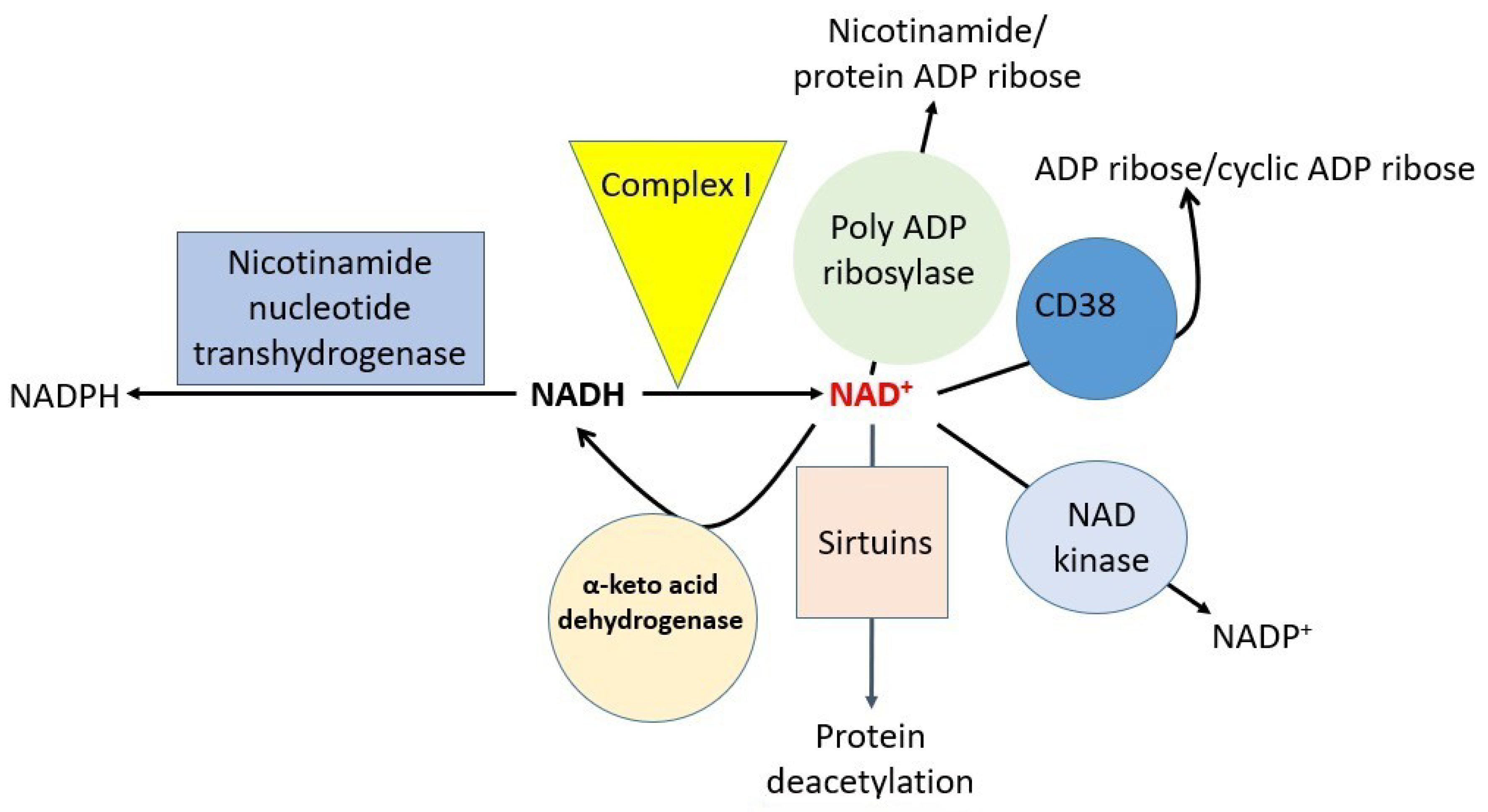
5. Effects of Cisplatin on Major Individual NAD+-Dependent Redox Enzymes
6. Counteracting Effects of Natural Products Derived from Plants
7. Other Factors That Can Modulate Cisplatin-Induced Kidney Injury
8. Summary
Author Contributions
Funding
Conflicts of Interest
References
- Zhang, J.; Ye, Z.W.; Tew, K.D.; Townsend, D.M. Cisplatin chemotherapy and renal function. Adv. Cancer Res. 2021, 152, 305–327. [Google Scholar] [PubMed]
- Dasari, S.; Tchounwou, P.B. Cisplatin in cancer therapy: Molecular mechanisms of action. Eur. J. Pharmacol. 2014, 740, 364–378. [Google Scholar] [CrossRef] [PubMed]
- Ashrafi, F.; Mortazavi, M.; Nematbakhsh, M. The prevention of cisplatin-induced nephrotoxicity: A general consensus statement of a group of oncologist-hematologists, adult and pediatric nephrologists, radiation oncologists, clinical pathologists, clinical pharmacologists, and renal physiologists on cisplatin therapy in cancer patients. Int. J. Prev. Med. 2022, 13, 21. [Google Scholar] [PubMed]
- Wang, D.; Lippard, S.J. Cellular processing of platinum anticancer drugs. Nat. Rev. Drug Discov. 2005, 4, 307–320. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.M.; Lippard, S.J. Cisplatin: From DNA damage to cancer chemotherapy. Prog. Nucleic Acid Res. Mol. Biol. 2001, 67, 93–130. [Google Scholar]
- Zazuli, Z.; Op’t Hoog, C.J.P.; Vijverberg, S.J.H.; Masereeuw, R.; Rassekh, S.R.; Medeiros, M.; Rivas-Ruiz, R.; Maitland-van der Zee, A.H.; Carleton, B.C. Cisplatin-induced nephrotoxicity in childhood cancer: Comparison between two countries. Pediatr. Nephrol. 2022. [Google Scholar] [CrossRef]
- Huang, G.; Zhang, Q.; Xu, C.; Chen, L.; Zhang, H. Mechanism of kidney injury induced by cisplatin. Toxicol. Res. 2022, 11, 385–390. [Google Scholar] [CrossRef]
- Pabla, N.; Dong, Z. Cisplatin nephrotoxicity: Mechanisms and renoprotective strategies. Kidney Int. 2008, 73, 994–1007. [Google Scholar] [CrossRef]
- Dong, G.; Luo, J.; Kumar, V.; Dong, Z. Inhibitors of histone deacetylases suppress cisplatin-induced p53 activation and apoptosis in renal tubular cells. Am. J. Physiol. Ren. Physiol. 2010, 298, F293–F300. [Google Scholar] [CrossRef]
- Nematbakhsh, M.; Ashrafi, F.; Nasri, H.; Talebi, A.; Pezeshki, Z.; Eshraghi, F.; Haghighi, M. A model for prediction of cisplatin induced nephrotoxicity by kidney weight in experimental rats. J. Res. Med. Sci. 2013, 18, 370–373. [Google Scholar]
- dos Santos, N.A.; Carvalho Rodrigues, M.A.; Martins, N.M.; dos Santos, A.C. Cisplatin-induced nephrotoxicity and targets of nephroprotection: An update. Arch. Toxicol. 2012, 86, 1233–1250. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.P.; Tadagavadi, R.K.; Ramesh, G.; Reeves, W.B. Mechanisms of cisplatin nephrotoxicity. Toxins 2010, 2, 2490–2518. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Shen, Y.; Fan, J.; Zeng, X.; Zhang, X.; Luan, J.; Wang, Y.; Zhang, J.; Fang, S.; Mei, X.; et al. Il-22-mediated renal metabolic reprogramming via pfkfb3 to treat kidney injury. Clin. Transl. Med. 2021, 11, e324. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Xiao, C.; Zheng, S.; Wang, Q.; Zhu, H.; Zhang, Y.; Wang, R. Microrna-214-3p aggravates ferroptosis by targeting gpx4 in cisplatin-induced acute kidney injury. Cell Stress Chaperones 2022, 27, 325–336. [Google Scholar] [CrossRef]
- Skinner, R.; Parry, A.; Price, L.; Cole, M.; Craft, A.W.; Pearson, A.D. Persistent nephrotoxicity during 10-year follow-up after cisplatin or carboplatin treatment in childhood: Relevance of age and dose as risk factors. Eur. J. Cancer 2009, 45, 3213–3219. [Google Scholar] [CrossRef] [PubMed]
- Sears, S.; Siskind, L. Potential therapeutic targets for cisplatin-induced kidney injury: Lessons from other models of aki and fibrosis. J. Am. Soc. Nephrol. 2021, 32, 1559–1567. [Google Scholar] [CrossRef]
- McSweeney, K.R.; Gadanec, L.K.; Qaradakhi, T.; Ali, B.A.; Zulli, A.; Apostolopoulos, V. Mechanisms of cisplatin-induced acute kidney injury: Pathological mechanisms, pharmacological interventions, and genetic mitigations. Cancers 2021, 13, 1572. [Google Scholar] [CrossRef] [PubMed]
- Oh, G.S.; Kim, H.J.; Shen, A.; Lee, S.B.; Yang, S.H.; Shim, H.; Cho, E.Y.; Kwon, K.B.; Kwak, T.H.; So, H.S. New therapeutic concept of nad redox balance for cisplatin nephrotoxicity. Biomed Res. Int. 2016, 2016, 4048390. [Google Scholar] [CrossRef] [PubMed]
- Mapuskar, K.A.; Wen, H.; Holanda, D.G.; Rastogi, P.; Steinbach, E.; Han, R.; Coleman, M.C.; Attanasio, M.; Riley, D.P.; Spitz, D.R.; et al. Persistent increase in mitochondrial superoxide mediates cisplatin-induced chronic kidney disease. Redox Biol. 2019, 20, 98–106. [Google Scholar] [CrossRef]
- Mapuskar, K.A.; Steinbach, E.J.; Zaher, A.; Riley, D.P.; Beardsley, R.A.; Keene, J.L.; Holmlund, J.T.; Anderson, C.M.; Zepeda-Orozco, D.; Buatti, J.M.; et al. Mitochondrial superoxide dismutase in cisplatin-induced kidney injury. Antioxidants 2021, 10, 1329. [Google Scholar] [CrossRef]
- Santos, N.A.; Catao, C.S.; Martins, N.M.; Curti, C.; Bianchi, M.L.; Santos, A.C. Cisplatin-induced nephrotoxicity is associated with oxidative stress, redox state unbalance, impairment of energetic metabolism and apoptosis in rat kidney mitochondria. Arch. Toxicol. 2007, 81, 495–504. [Google Scholar] [CrossRef] [PubMed]
- Hajian, S.; Rafieian-Kopaei, M.; Nasri, H. Renoprotective effects of antioxidants against cisplatin nephrotoxicity. J. Nephropharmacol. 2014, 3, 39–42. [Google Scholar] [PubMed]
- Fang, C.Y.; Lou, D.Y.; Zhou, L.Q.; Wang, J.C.; Yang, B.; He, Q.J.; Wang, J.J.; Weng, Q.J. Natural products: Potential treatments for cisplatin-induced nephrotoxicity. Acta Pharmacol. Sin. 2021, 42, 1951–1969. [Google Scholar] [CrossRef]
- Eslamifar, Z.; Moridnia, A.; Sabbagh, S.; Ghaffaripour, R.; Jafaripour, L.; Behzadifard, M. Ameliorative effects of gallic acid on cisplatin-induced nephrotoxicity in rat variations of biochemistry, histopathology, and gene expression. Biomed Res. Int. 2021, 2021, 2195238. [Google Scholar] [CrossRef]
- Shalby, A.B.; Assaf, N.; Ahmed, H.H. Possible mechanisms for n-acetyl cysteine and taurine in ameliorating acute renal failure induced by cisplatin in rats. Toxicol. Mech. Methods 2011, 21, 538–546. [Google Scholar] [CrossRef] [PubMed]
- Rattanavich, R.; Plagov, A.; Kumar, D.; Rai, P.; Lederman, R.; Salhan, D.; Vashistha, H.; Malhotra, A.; Meggs, L.G.; Singhal, P.C. Deficit of p66shca restores redox-sensitive stress response program in cisplatin-induced acute kidney injury. Exp. Mol. Pathol. 2013, 94, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Hosohata, K. Role of oxidative stress in drug-induced kidney injury. Int. J. Mol. Sci. 2016, 17, 1826. [Google Scholar] [CrossRef]
- Kim, D.H.; Choi, H.I.; Park, J.S.; Kim, C.S.; Bae, E.H.; Ma, S.K.; Kim, S.W. Farnesoid x receptor protects against cisplatin-induced acute kidney injury by regulating the transcription of ferroptosis-related genes. Redox Biol. 2022, 54, 102382. [Google Scholar] [CrossRef]
- Yin, M.; Li, N.; Makinde, E.A.; Olatunji, O.J.; Ni, Z. N6-2-hydroxyethyl-adenosine ameliorate cisplatin induced acute kidney injury in mice. All Life 2020, 13, 244–251. [Google Scholar] [CrossRef]
- Guo, P.; Zhang, N.; Li, J.; Liu, Y.; Li, Y.; Wang, X.; Wang, J.; Wang, Y.; Wang, A. Protective effects of low-temperature plasma on cisplatin-induced nephrotoxicity. Life Sci. 2022, 289, 120230. [Google Scholar] [CrossRef]
- Wang, X.L.; Wang, L.; Lin, F.L.; Li, S.S.; Lin, T.X.; Jiang, R.W. Protective effect of penetratin analogue-tagged sod1 on cisplatin-induced nephrotoxicity through inhibiting oxidative stress and jnk/p38 mapk signaling pathway. Oxid. Med. Cell. Longev. 2021, 2021, 5526053. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Wen, X.; Huang, Q.; Zhu, M.; Lu, J. Selenium status in diet affects nephrotoxicity induced by cisplatin in mice. Antioxidants 2022, 11, 1141. [Google Scholar] [CrossRef] [PubMed]
- Williams, R.M.; Shah, J.; Mercer, E.; Tian, H.S.; Thompson, V.; Cheung, J.M.; Dorso, M.; Kubala, J.M.; Gudas, L.J.; de Stanchina, E.; et al. Kidney-targeted redox scavenger therapy prevents cisplatin-induced acute kidney injury. Front. Pharmacol. 2021, 12, 790913. [Google Scholar] [CrossRef] [PubMed]
- Black, L.M.; Lever, J.M.; Traylor, A.M.; Chen, B.; Yang, Z.; Esman, S.K.; Jiang, Y.; Cutter, G.R.; Boddu, R.; George, J.F.; et al. Divergent effects of aki to ckd models on inflammation and fibrosis. Am. J. Physiol. Ren. Physiol. 2018, 315, F1107–F1118. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Li, K.Y.; Wang, P.J.; Huang, H.W.; Chen, M.J. Alleviating chronic kidney disease progression through modulating the critical genus of gut microbiota in a cisplatin-induced lanyu pig model. J. Food Drug Anal. 2020, 28, 103–114. [Google Scholar] [CrossRef]
- Younis, N.N.; Elsherbiny, N.M.; Shaheen, M.A.; Elseweidy, M.M. Modulation of nadph oxidase and nrf2/ho-1 pathway by vanillin in cisplatin-induced nephrotoxicity in rats. J. Pharm. Pharmacol. 2020, 72, 1546–1555. [Google Scholar] [CrossRef]
- Al Za’abi, M.; Al Salam, S.; Al Suleimani, Y.; Ashique, M.; Manoj, P.; Nemmar, A.; Ali, B.H. Effects of repeated increasing doses of cisplatin as models of acute kidney injury and chronic kidney disease in rats. Naunyn Schmiedeberg’s Arch. Pharmacol. 2021, 394, 249–259. [Google Scholar] [CrossRef]
- Hsiao, Y.P.; Chen, H.L.; Tsai, J.N.; Lin, M.Y.; Liao, J.W.; Wei, M.S.; Ko, J.L.; Ou, C.C. Administration of lactobacillus reuteri combined with clostridium butyricum attenuates cisplatin-induced renal damage by gut microbiota reconstitution, increasing butyric acid production, and suppressing renal inflammation. Nutrients 2021, 13, 2792. [Google Scholar] [CrossRef]
- Tsai, Y.S.; Chen, Y.P.; Lin, S.W.; Chen, Y.L.; Chen, C.C.; Huang, G.J. Lactobacillus rhamnosus gklc1 ameliorates cisplatin-induced chronic nephrotoxicity by inhibiting cell inflammation and apoptosis. Biomed. Pharmacother. 2022, 147, 112701. [Google Scholar] [CrossRef]
- Li, M.; Li, C.M.; Ye, Z.C.; Huang, J.; Li, Y.; Lai, W.; Peng, H.; Lou, T.Q. Sirt3 modulates fatty acid oxidation and attenuates cisplatin-induced aki in mice. J. Cell. Mol. Med. 2020, 24, 5109–5121. [Google Scholar] [CrossRef]
- Singh, M.P.; Chauhan, A.K.; Kang, S.C. Morin hydrate ameliorates cisplatin-induced er stress, inflammation and autophagy in hek-293 cells and mice kidney via parp-1 regulation. Int. Immunopharmacol. 2018, 56, 156–167. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Lu, M.; Xiong, L.; Fan, J.; Zhou, Y.; Li, H.; Peng, X.; Zhong, Z.; Wang, Y.; Huang, F.; et al. Drp1-mediated mitochondrial fission promotes renal fibroblast activation and fibrogenesis. Cell Death Dis. 2020, 11, 29. [Google Scholar] [CrossRef] [PubMed]
- Ayanga, B.A.; Badal, S.S.; Wang, Y.; Galvan, D.L.; Chang, B.H.; Schumacker, P.T.; Danesh, F.R. Dynamin-related protein 1 deficiency improves mitochondrial fitness and protects against progression of diabetic nephropathy. J. Am. Soc. Nephrol. 2016, 27, 2733–2747. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Tang, C.; Cai, J.; Chen, G.; Zhang, D.; Zhang, Z.; Dong, Z. Pink1/parkin-mediated mitophagy is activated in cisplatin nephrotoxicity to protect against kidney injury. Cell Death Dis. 2018, 9, 1113. [Google Scholar] [CrossRef] [PubMed]
- Wu, R.; Li, J.; Tu, G.; Su, Y.; Zhang, X.; Luo, Z.; Rong, R.; Zhang, Y. Comprehensive molecular and cellular characterization of acute kidney injury progression to renal fibrosis. Front. Immunol. 2021, 12, 699192. [Google Scholar] [CrossRef]
- Sears, S.M.; Orwick, A.; Siskind, L.J. Modeling cisplatin-induced kidney injury to increase translational potential. Nephron 2022, 1–4. [Google Scholar] [CrossRef]
- Yan, L.J. Folic acid-induced animal model of kidney disease. Anim. Models Exp. Med. 2021, 4, 329–342. [Google Scholar] [CrossRef]
- Shi, M.; McMillan, K.L.; Wu, J.; Gillings, N.; Flores, B.; Moe, O.W.; Hu, M.C. Cisplatin nephrotoxicity as a model of chronic kidney disease. Lab. Investig. 2018, 98, 1105–1121. [Google Scholar] [CrossRef]
- Perse, M. Cisplatin mouse models: Treatment, toxicity and translatability. Biomedicines 2021, 9, 1406. [Google Scholar] [CrossRef]
- Fu, Y.; Tang, C.; Cai, J.; Chen, G.; Zhang, D.; Dong, Z. Rodent models of aki-ckd transition. Am. J. Physiol. Ren. Physiol. 2018, 315, F1098–F1106. [Google Scholar] [CrossRef]
- Fu, Y.; Xiang, Y.; Wu, W.; Cai, J.; Tang, C.; Dong, Z. Persistent activation of autophagy after cisplatin nephrotoxicity promotes renal fibrosis and chronic kidney disease. Front. Pharmacol. 2022, 13, 918732. [Google Scholar] [CrossRef] [PubMed]
- Fu, S.; Hu, X.; Ma, Z.; Wei, Q.; Xiang, X.; Li, S.; Wen, L.; Liang, Y.; Dong, Z. P53 in proximal tubules mediates chronic kidney problems after cisplatin treatment. Cells 2022, 11, 712. [Google Scholar] [CrossRef] [PubMed]
- Bufi, R.; Korstanje, R. The impact of genetic background on mouse models of kidney disease. Kidney Int. 2022, 102, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Usami, M.; Okada, A.; Taguchi, K.; Hamamoto, S.; Kohri, K.; Yasui, T. Genetic differences in c57bl/6 mouse substrains affect kidney crystal deposition. Urolithiasis 2018, 46, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Navarro, C.D.C.; Figueira, T.R.; Francisco, A.; Dal’Bo, G.A.; Ronchi, J.A.; Rovani, J.C.; Escanhoela, C.A.F.; Oliveira, H.C.F.; Castilho, R.F.; Vercesi, A.E. Redox imbalance due to the loss of mitochondrial nad(p)-transhydrogenase markedly aggravates high fat diet-induced fatty liver disease in mice. Free Radic. Biol. Med. 2017, 113, 190–202. [Google Scholar] [CrossRef]
- Dogar, I.; Dixon, S.; Gill, R.; Young, A.; Mallay, S.; Oldford, C.; Mailloux, R.J. C57bl/6j mice upregulate catalase to maintain the hydrogen peroxide buffering capacity of liver mitochondria. Free Radic. Biol. Med. 2020, 146, 59–69. [Google Scholar] [CrossRef]
- Ronchi, J.A.; Figueira, T.R.; Ravagnani, F.G.; Oliveira, H.C.; Vercesi, A.E.; Castilho, R.F. A spontaneous mutation in the nicotinamide nucleotide transhydrogenase gene of c57bl/6j mice results in mitochondrial redox abnormalities. Free Radic. Biol. Med. 2013, 63, 446–456. [Google Scholar] [CrossRef]
- Kunath, A.; Heiker, J.T.; Kern, M.; Kosacka, J.; Flehmig, G.; Stumvoll, M.; Kovacs, P.; Bluher, M.; Kloting, N. Nicotinamide nucleotide transhydrogenase (nnt) is related to obesity in mice. Horm. Metab. Res. 2020, 52, 877–881. [Google Scholar] [CrossRef]
- Close, A.F.; Chae, H.; Jonas, J.C. The lack of functional nicotinamide nucleotide transhydrogenase only moderately contributes to the impairment of glucose tolerance and glucose-stimulated insulin secretion in c57bl/6j vs c57bl/6n mice. Diabetologia 2021, 64, 2550–2561. [Google Scholar] [CrossRef]
- Oh, G.S.; Kim, H.J.; Choi, J.H.; Shen, A.; Choe, S.K.; Karna, A.; Lee, S.H.; Jo, H.J.; Yang, S.H.; Kwak, T.H.; et al. Pharmacological activation of nqo1 increases nad(+) levels and attenuates cisplatin-mediated acute kidney injury in mice. Kidney Int. 2014, 85, 547–560. [Google Scholar] [CrossRef]
- Adhikari, A.; Mondal, S.; Chatterjee, T.; Das, M.; Biswas, P.; Ghosh, R.; Darbar, S.; Alessa, H.; Althakafy, J.T.; Sayqal, A.; et al. Redox nanomedicine ameliorates chronic kidney disease (ckd) by mitochondrial reconditioning in mice. Commun. Biol. 2021, 4, 1013. [Google Scholar] [CrossRef] [PubMed]
- Zager, R.A.; Johnson, A.C.M. Early loss of glutathione-s-transferase (gst) activity during diverse forms of acute renal tubular injury. Physiol. Rep. 2022, 10, e15352. [Google Scholar] [CrossRef] [PubMed]
- Gang, G.T.; Kim, Y.H.; Noh, J.R.; Kim, K.S.; Jung, J.Y.; Shong, M.; Hwang, J.H.; Lee, C.H. Protective role of nad(p)h:Quinone oxidoreductase 1 (nqo1) in cisplatin-induced nephrotoxicity. Toxicol. Lett. 2013, 221, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Nazari Soltan Ahmad, S.; Rashtchizadeh, N.; Argani, H.; Roshangar, L.; Ghorbani Haghjo, A.; Sanajou, D.; Panah, F.; Ashrafi Jigheh, Z.; Dastmalchi, S.; Mesgari-Abbasi, M. Dunnione protects against experimental cisplatin-induced nephrotoxicity by modulating nqo1 and nad(+) levels. Free Radic. Res. 2018, 52, 808–817. [Google Scholar] [CrossRef] [PubMed]
- Hirst, J.; King, M.S.; Pryde, K.R. The production of reactive oxygen species by complex i. Biochem. Soc. Trans. 2008, 36, 976–980. [Google Scholar] [CrossRef] [PubMed]
- Cooper, J.M.; Mann, V.M.; Krige, D.; Schapira, A.H. Human mitochondrial complex i dysfunction. Biochim. Biophys. Acta 1992, 1101, 198–203. [Google Scholar] [CrossRef]
- Morris, B.J. Seven sirtuins for seven deadly diseases of aging. Free Radic. Biol. Med. 2013, 56, 133–171. [Google Scholar] [CrossRef]
- Sauve, A.A. Sirtuin chemical mechanisms. Biochim. Biophys. Acta 2010, 1804, 1591–1603. [Google Scholar] [CrossRef]
- Yan, L.J.; Sumien, N.; Thangthaeng, N.; Forster, M.J. Reversible inactivation of dihydrolipoamide dehydrogenase by mitochondrial hydrogen peroxide. Free Radic. Res. 2013, 47, 123–133. [Google Scholar] [CrossRef]
- Hoxhaj, G.; Ben-Sahra, I.; Lockwood, S.E.; Timson, R.C.; Byles, V.; Henning, G.T.; Gao, P.; Selfors, L.M.; Asara, J.M.; Manning, B.D. Direct stimulation of nadp(+) synthesis through akt-mediated phosphorylation of nad kinase. Science 2019, 363, 1088–1092. [Google Scholar] [CrossRef]
- Tedeschi, P.M.; Bansal, N.; Kerrigan, J.E.; Abali, E.E.; Scotto, K.W.; Bertino, J.R. Nad+ kinase as a therapeutic target in cancer. Clin. Cancer Res. 2016, 22, 5189–5195. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Kim, H.; Fu, Z.; Qiu, Y.; Yang, Z.; Wang, J.; Zhang, D.; Tong, X.; Yin, L.; Li, J.; et al. Deficiency of the mitochondrial nad kinase causes stress-induced hepatic steatosis in mice. Gastroenterology 2018, 154, 224–237. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R. Mnadk, a long-awaited human mitochondrion-localized nad kinase. J. Cell. Physiol. 2015, 230, 1697–1701. [Google Scholar] [CrossRef] [PubMed]
- Benzi, A.; Sturla, L.; Heine, M.; Fischer, A.W.; Spinelli, S.; Magnone, M.; Sociali, G.; Parodi, A.; Fenoglio, D.; Emionite, L.; et al. Cd38 downregulation modulates nad(+) and nadp(h) levels in thermogenic adipose tissues. Biochim. Biophys. Acta Mol. Cell. Biol. Lipids 2021, 1866, 158819. [Google Scholar] [CrossRef]
- Braidy, N.; Berg, J.; Clement, J.; Khorshidi, F.; Poljak, A.; Jayasena, T.; Grant, R.; Sachdev, P. Role of nicotinamide adenine dinucleotide and related precursors as therapeutic targets for age-related degenerative diseases: Rationale, biochemistry, pharmacokinetics, and outcomes. Antioxid. Redox Signal. 2019, 30, 251–294. [Google Scholar] [CrossRef]
- Camacho-Pereira, J.; Tarrago, M.G.; Chini, C.C.; Nin, V.; Escande, C.; Warner, G.M.; Puranik, A.S.; Schoon, R.A.; Reid, J.M.; Galina, A.; et al. Cd38 dictates age-related nad decline and mitochondrial dysfunction through an sirt3-dependent mechanism. Cell Metab. 2016, 23, 1127–1139. [Google Scholar] [CrossRef]
- Devalaraja-Narashimha, K.; Singaravelu, K.; Padanilam, B.J. Poly(adp-ribose) polymerase-mediated cell injury in acute renal failure. Pharmacol. Res. 2005, 52, 44–59. [Google Scholar] [CrossRef]
- Alemasova, E.E.; Lavrik, O.I. Poly(adp-ribosyl)ation by parp1: Reaction mechanism and regulatory proteins. Nucleic Acids Res. 2019, 47, 3811–3827. [Google Scholar] [CrossRef]
- Butepage, M.; Eckei, L.; Verheugd, P.; Luscher, B. Intracellular mono-adp-ribosylation in signaling and disease. Cells 2015, 4, 569–595. [Google Scholar] [CrossRef]
- Ronchi, J.A.; Francisco, A.; Passos, L.A.; Figueira, T.R.; Castilho, R.F. The contribution of nicotinamide nucleotide transhydrogenase to peroxide detoxification is dependent on the respiratory state and counterbalanced by other sources of nadph in liver mitochondria. J. Biol. Chem. 2016, 291, 20173–20187. [Google Scholar] [CrossRef]
- Santos, L.R.B.; Muller, C.; de Souza, A.H.; Takahashi, H.K.; Spegel, P.; Sweet, I.R.; Chae, H.; Mulder, H.; Jonas, J.C. Nnt reverse mode of operation mediates glucose control of mitochondrial nadph and glutathione redox state in mouse pancreatic beta-cells. Mol. Metab. 2017, 6, 535–547. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Yang, C.; Amorim, T.; Maqbool, M.; Lin, J.; Li, C.; Fang, C.; Xue, L.; Kwart, A.; Fang, H.; et al. Cisplatin-mediated upregulation of ape2 binding to myh9 provokes mitochondrial fragmentation and acute kidney injury. Cancer Res. 2021, 81, 713–723. [Google Scholar] [CrossRef] [PubMed]
- Hama, T.; Nagesh, P.K.; Chowdhury, P.; Moore, B.M., 2nd; Yallapu, M.M.; Regner, K.R.; Park, F. DNA damage is overcome by trip13 overexpression during cisplatin nephrotoxicity. JCI Insight 2021, 6, e139092. [Google Scholar] [CrossRef]
- Yan, L.J.; Lodge, J.K.; Traber, M.G.; Matsugo, S.; Packer, L. Comparison between copper-mediated and hypochlorite-mediated modifications of human low density lipoproteins evaluated by protein carbonyl formation. J. Lipid Res. 1997, 38, 992–1001. [Google Scholar] [CrossRef]
- Yang, Y.; Fu, Y.; Wang, P.; Liu, S.; Sha, Y.; Zhang, Y.; Zhang, A.; Jia, Z.; Ding, G.; Huang, S. Intervention of mitochondrial activity attenuates cisplatin-induced acute kidney injury. Int. Urol. Nephrol. 2019, 51, 1207–1218. [Google Scholar] [CrossRef] [PubMed]
- Kruidering, M.; Van de Water, B.; de Heer, E.; Mulder, G.J.; Nagelkerke, J.F. Cisplatin-induced nephrotoxicity in porcine proximal tubular cells: Mitochondrial dysfunction by inhibition of complexes i to iv of the respiratory chain. J. Pharmacol. Exp. Ther. 1997, 280, 638–649. [Google Scholar]
- El-Hamoly, T.; El-Sharawy, D.M.; El Refaye, M.S.; Abd El-Rahman, S.S. L-thyroxine modifies nephrotoxicity by regulating the apoptotic pathway: The possible role of cd38/adp-ribosyl cyclase-mediated calcium mobilization. PLoS ONE 2017, 12, e0184157. [Google Scholar] [CrossRef]
- Kim, M.J.; Moon, D.; Jung, S.; Lee, J.; Kim, J. Cisplatin nephrotoxicity is induced via poly(adp-ribose) polymerase activation in adult zebrafish and mice. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2020, 318, R843–R854. [Google Scholar] [CrossRef]
- Zhang, Y.; Tao, X.; Yin, L.; Xu, L.; Xu, Y.; Qi, Y.; Han, X.; Song, S.; Zhao, Y.; Lin, Y.; et al. Protective effects of dioscin against cisplatin-induced nephrotoxicity via the microrna-34a/sirtuin 1 signalling pathway. Br. J. Pharmacol. 2017, 174, 2512–2527. [Google Scholar] [CrossRef]
- Lu, C.Y. Beta-lapachone ameliorates murine cisplatin nephrotoxicity: Nad(+), nqo1, and sirt1 at the crossroads of metabolism, injury, and inflammation. Kidney Int. 2014, 85, 496–498. [Google Scholar] [CrossRef]
- Ozkok, A.; Edelstein, C.L. Pathophysiology of cisplatin-induced acute kidney injury. Biomed Res. Int. 2014, 2014, 967826. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Long, K.E.; Tang, K.; Padanilam, B.J. Poly(adp-ribose) polymerase 1 activation is required for cisplatin nephrotoxicity. Kidney Int. 2012, 82, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Ramesh, G.; Uematsu, S.; Akira, S.; Reeves, W.B. Tlr4 signaling mediates inflammation and tissue injury in nephrotoxicity. J. Am. Soc. Nephrol. 2008, 19, 923–932. [Google Scholar] [CrossRef] [PubMed]
- Ramesh, G.; Zhang, B.; Uematsu, S.; Akira, S.; Reeves, W.B. Endotoxin and cisplatin synergistically induce renal dysfunction and cytokine production in mice. Am. J. Physiol. Ren. Physiol. 2007, 293, F325–F332. [Google Scholar] [CrossRef] [PubMed]
- Habib, R. Multifaceted roles of toll-like receptors in acute kidney injury. Heliyon 2021, 7, e06441. [Google Scholar] [CrossRef]
- Santos, N.A.; Bezerra, C.S.; Martins, N.M.; Curti, C.; Bianchi, M.L.; Santos, A.C. Hydroxyl radical scavenger ameliorates cisplatin-induced nephrotoxicity by preventing oxidative stress, redox state unbalance, impairment of energetic metabolism and apoptosis in rat kidney mitochondria. Cancer Chemother. Pharmacol. 2008, 61, 145–155. [Google Scholar] [CrossRef]
- Fernandez-Rojas, B.; Rodriguez-Rangel, D.S.; Granados-Castro, L.F.; Negrette-Guzman, M.; Leon-Contreras, J.C.; Hernandez-Pando, R.; Molina-Jijon, E.; Reyes, J.L.; Zazueta, C.; Pedraza-Chaverri, J. C-phycocyanin prevents cisplatin-induced mitochondrial dysfunction and oxidative stress. Mol. Cell. Biochem. 2015, 406, 183–197. [Google Scholar] [CrossRef]
- Shen, J.; Wang, W.; Shao, X.; Wu, J.; Li, S.; Che, X.; Ni, Z. Integrated analysis of m6a methylome in cisplatin-induced acute kidney injury and berberine alleviation in mouse. Front. Genet. 2020, 11, 584460. [Google Scholar] [CrossRef]
- Kuo, H.L.; Mong, M.C.; Chen, H.C.; Wang, Z.H.; Yin, M.C. S-ethyl cysteine, an amino acid derivative, attenuated cisplatin induced nephrotoxicity. Amino Acids 2020, 52, 1181–1190. [Google Scholar] [CrossRef]
- Yang, F.; Jia, M.; Deng, C.; Xiao, B.; Dai, R.; Xiang, Y. Silibinin ameliorates cisplatin-induced acute kidney injury via activating nfe2l1-mediated antioxidative response to suppress the ros/mapk signaling pathway. J. Mol. Histol. 2022, 1–12. [Google Scholar] [CrossRef]
- Mohamed, M.E.; Abduldaium, Y.S.; Younis, N.S. Ameliorative effect of linalool in cisplatin-induced nephrotoxicity: The role of hmgb1/tlr4/nf-kappab and nrf2/ho1 pathways. Biomolecules 2020, 10, 1488. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.; Dong, H.; Wang, Q.; Bai, J.; Li, Y.N.; Zhao, J.J.; Li, J.Z. Danshensu attenuates cisplatin-induced nephrotoxicity through activation of nrf2 pathway and inhibition of nf-kappab. Biomed. Pharmacother. 2021, 142, 111995. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Ma, Z.; Wen, L.; Li, S.; Dong, Z. Autophagy in cisplatin nephrotoxicity during cancer therapy. Cancers 2021, 13, 5618. [Google Scholar] [CrossRef]
- Bhatia, D.; Choi, M.E. Autophagy in kidney disease: Advances and therapeutic potential. Prog. Mol. Biol. Transl. Sci. 2020, 172, 107–133. [Google Scholar] [PubMed]
- Tang, Y.; Luo, H.; Xiao, Q.; Li, L.; Zhong, X.; Zhang, J.; Wang, F.; Li, G.; Wang, L.; Li, Y. Isoliquiritigenin attenuates septic acute kidney injury by regulating ferritinophagy-mediated ferroptosis. Ren. Fail. 2021, 43, 1551–1560. [Google Scholar] [CrossRef] [PubMed]
- Qi, J.; Xue, Q.; Kuang, L.; Xie, L.; Luo, R.; Nie, X. Berberine alleviates cisplatin-induced acute kidney injury by regulating mitophagy via pink 1/parkin pathway. Transl. Androl. Urol. 2020, 9, 1712–1724. [Google Scholar] [CrossRef]
- Ma, N.; Wei, Z.; Hu, J.; Gu, W.; Ci, X. Farrerol ameliorated cisplatin-induced chronic kidney disease through mitophagy induction via nrf2/pink1 pathway. Front. Pharmacol. 2021, 12, 768700. [Google Scholar] [CrossRef]
- Nazari, A.; Mirian, M.; Aghaei, M.; Aliomrani, M. 4-hydroxyhalcone effects on cisplatin-induced genotoxicity model. Toxicol. Res. 2021, 10, 11–17. [Google Scholar] [CrossRef]
- Gwon, M.G.; Gu, H.; Leem, J.; Park, K.K. Protective effects of 6-shogaol, an active compound of ginger, in a murine model of cisplatin-induced acute kidney injury. Molecules 2021, 26, 5931. [Google Scholar] [CrossRef]
- Elseweidy, M.M.; Zaghloul, M.S.; Younis, N.N. 10-dhgd ameliorates cisplatin-induced nephrotoxicity in rats. Biomed. Pharmacother. 2016, 83, 241–246. [Google Scholar] [CrossRef]
- Afsar, T.; Razak, S.; Aldisi, D.; Shabbir, M.; Almajwal, A.; Al Kheraif, A.A.; Arshad, M. Acacia hydaspica r. Parker ethyl-acetate extract abrogates cisplatin-induced nephrotoxicity by targeting ros and inflammatory cytokines. Sci. Rep. 2021, 11, 17248. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, M.O.; Ahmed, M.M.; Arshad, S.; Javaid, U.; Khan, I.A.; Manzoor, M.; Andleeb, S.; Riaz, R.; Munawar, S.H.; Manzoor, Z.; et al. Nephroprotective effects of alhagi camelorum against cisplatin-induced nephrotoxicity in albino wistar rats. Molecules 2022, 27, 941. [Google Scholar] [CrossRef] [PubMed]
- Adeoye, B.O.; Asenuga, E.R.; Oyagbemi, A.A.; Omobowale, T.O.; Adedapo, A.A. The protective effect of the ethanol leaf extract of andrographis paniculata on cisplatin-induced acute kidney injury in rats through nrf2/kim-1 signalling pathway. Drug Res. 2018, 68, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Park, J.Y.; Lee, D.; Jang, H.J.; Jang, D.S.; Kwon, H.C.; Kim, K.H.; Kim, S.N.; Hwang, G.S.; Kang, K.S.; Eom, D.W. Protective effect of artemisia asiatica extract and its active compound eupatilin against cisplatin-induced renal damage. Evid. Based Complement. Alternat. Med. 2015, 2015, 483980. [Google Scholar] [CrossRef]
- Ibrahim, A.; Al-Hizab, F.A.; Abushouk, A.I.; Abdel-Daim, M.M. Nephroprotective effects of benzyl isothiocyanate and resveratrol against cisplatin-induced oxidative stress and inflammation. Front. Pharmacol. 2018, 9, 1268. [Google Scholar] [CrossRef]
- Gholampour, F.; Masoudi, R.; Khaledi, M.; Rooyeh, M.M.; Farzad, S.H.; Ataellahi, F.; Abtahi, S.L.; Owji, S.M. Berberis integerrima hydro-alcoholic root extract and its constituent berberine protect against cisplatin-induced nephro- and hepato-toxicity. Am. J. Med. Sci. 2022, 364, 76–87. [Google Scholar] [CrossRef]
- Zaaba, N.E.; Beegam, S.; Elzaki, O.; Yasin, J.; Nemmar, B.M.; Ali, B.H.; Adeghate, E.; Nemmar, A. The nephroprotective effects of alpha-bisabolol in cisplatin-induced acute kidney injury in mice. Biomedicines 2022, 10, 842. [Google Scholar] [CrossRef]
- Widowati, W.; Prahastuti, S.; Hidayat, M.; Hasianna, S.T.; Wahyudianingsih, R.; Eltania, T.F.; Azizah, A.M.; Aviani, J.K.; Subangkit, M.; Handayani, R.A.S.; et al. Detam 1 black soybean against cisplatin-induced acute ren failure on rat model via antioxidant, antiinflammatory and antiapoptosis potential. J. Tradit. Complement. Med. 2022, 12, 426–435. [Google Scholar] [CrossRef]
- Eltamany, E.E.; Elhady, S.S.; Nafie, M.S.; Ahmed, H.A.; Abo-Elmatty, D.M.; Ahmed, S.A.; Badr, J.M.; Abdel-Hamed, A.R. The antioxidant carrichtera annua dc. Ethanolic extract counteracts cisplatin triggered hepatic and renal toxicities. Antioxidants 2021, 10, 825. [Google Scholar] [CrossRef]
- Ragab, T.I.M.; Zoheir, K.M.A.; Mohamed, N.A.; El Gendy, A.E.G.; Abd-ElGawad, A.M.; Abdelhameed, M.F.; Farrag, A.R.H.; Elshamy, A.I. Cytoprotective potentialities of carvacrol and its nanoemulsion against cisplatin-induced nephrotoxicity in rats: Development of nano-encasulation form. Heliyon 2022, 8, e09198. [Google Scholar] [CrossRef]
- Zhang, J.; Zhao, T.; Wang, C.; Meng, Q.; Huo, X.; Wang, C.; Sun, P.; Sun, H.; Ma, X.; Wu, J.; et al. Catalpol-induced ampk activation alleviates cisplatin-induced nephrotoxicity through the mitochondrial-dependent pathway without compromising its anticancer properties. Oxid. Med. Cell. Longev. 2021, 2021, 7467156. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Chen, Q.Y.; He, Y.; Liu, Y.H.; Meng, X.M.; Liu, M.M. Discovery of a chalcone derivative as potent necroptosis inhibitor for the treatment of acute kidney injury. Clin. Exp. Pharmacol. Physiol. 2022, 49, 824–835. [Google Scholar] [CrossRef] [PubMed]
- Adeyemi, O.O.; Ishola, I.O.; Ajani, I.D. Citrullus colocynthis linn. Fruit extract ameliorates cisplatin-induced hepato-renal toxicity in rats. J. Complement. Integr. Med. 2017, 15. [Google Scholar] [CrossRef]
- Wang, R.; Hassan, W.; Ahmad, F.U.D.; Jabeen, Q.; Ahmed, H.; Iqbal, O. Citrus aurantium ameliorates cisplatin-induced nephrotoxicity. Biomed Res. Int. 2019, 2019, 3960908. [Google Scholar] [CrossRef] [PubMed]
- Mahmod, I.I.; Ismail, I.S.; Alitheen, N.B.; Normi, Y.M.; Abas, F.; Khatib, A.; Rudiyanto; Latip, J. Nmr and lcms analytical platforms exhibited the nephroprotective effect of clinacanthus nutans in cisplatin-induced nephrotoxicity in the in vitro condition. BMC Complement. Med. Ther. 2020, 20, 320. [Google Scholar] [CrossRef] [PubMed]
- Sahrial, I.; Solfaine, R. Coleus amboinicus extract increases transforming growth factor-1beta expression in wistar rats with cisplatin-induced nephropathy. Vet. World 2019, 12, 1346–1351. [Google Scholar] [CrossRef]
- Ueki, M.; Ueno, M.; Morishita, J.; Maekawa, N. Curcumin ameliorates cisplatin-induced nephrotoxicity by inhibiting renal inflammation in mice. J. Biosci. Bioeng. 2013, 115, 547–551. [Google Scholar] [CrossRef]
- Sen, Z.; Jie, M.; Jingzhi, Y.; Dongjie, W.; Dongming, Z.; Xiaoguang, C. Total coumarins from hydrangea paniculata protect against cisplatin-induced acute kidney damage in mice by suppressing renal inflammation and apoptosis. Evid. Based Complement. Alternat. Med. 2017, 2017, 5350161. [Google Scholar] [CrossRef]
- Miyawaki, Y.; Ueki, M.; Ueno, M.; Asaga, T.; Tokuda, M.; Shirakami, G. D-allose ameliorates cisplatin-induced nephrotoxicity in mice. Tohoku J. Exp. Med. 2012, 228, 215–221. [Google Scholar] [CrossRef]
- Meng, H.; Fu, G.; Shen, J.; Shen, K.; Xu, Z.; Wang, Y.; Jin, B.; Pan, H. Ameliorative effect of daidzein on cisplatin-induced nephrotoxicity in mice via modulation of inflammation, oxidative stress, and cell death. Oxid. Med. Cell. Longev. 2017, 2017, 3140680. [Google Scholar] [CrossRef]
- Cao, S.S.; Yan, M.; Hou, Z.Y.; Chen, Y.; Jiang, Y.S.; Fan, X.R.; Fang, P.F.; Zhang, B.K. Danshen modulates nrf2-mediated signaling pathway in cisplatin-induced renal injury. J. Huazhong Univ. Sci. Technol. Med. Sci. 2017, 37, 761–765. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, M.O.; Sial, A.S.; Akhtar, I.; Naeem, M.; Hazafa, A.; Ansari, R.A.; Rizvi, S.A.A. The nephroprotective effects of daucus carota and eclipta prostrata against cisplatin-induced nephrotoxicity in rats. Bioengineered 2021, 12, 12702–12721. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.J.; Kim, K.S.; Park, J.H.; Lee, S.H.; Kim, H.R.; Lee, S.H.; Choi, H.B.; Cao, S.; Kumar, V.; Kwak, J.H.; et al. Protective effects of dendropanoxide isolated from dendropanax morbifera against cisplatin-induced acute kidney injury via the ampk/mtor signaling pathway. Food Chem. Toxicol. 2020, 145, 111605. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Gu, L.B.; Tu, Y.; Hu, H.; Huang, Y.R.; Sun, W. Emodin ameliorates cisplatin-induced apoptosis of rat renal tubular cells in vitro by activating autophagy. Acta Pharmacol. Sin. 2016, 37, 235–245. [Google Scholar] [CrossRef]
- Sioud, F.; Ben Toumia, I.; Lahmer, A.; Khlifi, R.; Dhaouefi, Z.; Maatouk, M.; Ghedira, K.; Chekir-Ghedira, L. Methanolic extract of ephedra alata ameliorates cisplatin-induced nephrotoxicity and hepatotoxicity through reducing oxidative stress and genotoxicity. Environ. Sci. Pollut. Res. Int. 2020, 27, 12792–12801. [Google Scholar] [CrossRef]
- Sharma, S.; Modi, A.; Narayan, G.; Hemalatha, S. Protective effect of exacum lawii on cisplatin-induced oxidative renal damage in rats. Pharmacogn. Mag. 2018, 13, S807–S816. [Google Scholar]
- El-Sayed, S.M.; El-Naggar, M.E.; Hussein, J.; Medhat, D.; El-Banna, M. Effect of ficus carica l. Leaves extract loaded gold nanoparticles against cisplatin-induced acute kidney injury. Colloids Surf. B Biointerfaces 2019, 184, 110465. [Google Scholar] [CrossRef]
- Katanic, J.; Matic, S.; Pferschy-Wenzig, E.M.; Kretschmer, N.; Boroja, T.; Mihailovic, V.; Stankovic, V.; Stankovic, N.; Mladenovic, M.; Stanic, S.; et al. Filipendula ulmaria extracts attenuate cisplatin-induced liver and kidney oxidative stress in rats: In vivo investigation and lc-ms analysis. Food Chem. Toxicol. 2017, 99, 86–102. [Google Scholar] [CrossRef]
- Hao, Y.; Miao, J.; Liu, W.; Peng, L.; Chen, Y.; Zhong, Q. Formononetin protects against cisplatininduced acute kidney injury through activation of the pparalpha/nrf2/ho1/nqo1 pathway. Int. J. Mol. Med. 2021, 47, 511–522. [Google Scholar] [CrossRef]
- El-Naga, R.N. Forskolin alleviates cisplatin-induced acute renal toxicity in rats. J. Pharm. Pharmacol. 2022, 74, 1051–1060. [Google Scholar] [CrossRef]
- Huang, Y.C.; Tsai, M.S.; Hsieh, P.C.; Shih, J.H.; Wang, T.S.; Wang, Y.C.; Lin, T.H.; Wang, S.H. Galangin ameliorates cisplatin-induced nephrotoxicity by attenuating oxidative stress, inflammation and cell death in mice through inhibition of erk and nf-kappab signaling. Toxicol. Appl. Pharmacol. 2017, 329, 128–139. [Google Scholar] [CrossRef] [PubMed]
- Geng, X.; Zhong, D.; Su, L.; Lin, Z.; Yang, B. Preventive and therapeutic effect of ganoderma lucidum on kidney injuries and diseases. Adv. Pharmacol. 2020, 87, 257–276. [Google Scholar] [PubMed]
- Nasr, A.Y. Protective effect of aged garlic extract against the oxidative stress induced by cisplatin on blood cells parameters and hepatic antioxidant enzymes in rats. Toxicol. Rep. 2014, 1, 682–691. [Google Scholar] [CrossRef] [PubMed]
- Sung, M.J.; Kim, D.H.; Jung, Y.J.; Kang, K.P.; Lee, A.S.; Lee, S.; Kim, W.; Davaatseren, M.; Hwang, J.T.; Kim, H.J.; et al. Genistein protects the kidney from cisplatin-induced injury. Kidney Int. 2008, 74, 1538–1547. [Google Scholar] [CrossRef]
- Wei, C.; Zhang, Y.; Zhong, X.; Lu, S.; Zou, X.; Yang, Y.; Huang, S.; Huang, Z. Ginkgo biloba leaf extract mitigates cisplatin-induced chronic renal interstitial fibrosis by inhibiting the epithelial-mesenchymal transition of renal tubular epithelial cells mediated by the smad3/tgf-beta1 and smad3/p38 mapk pathways. Chin. Med. 2022, 17, 25. [Google Scholar] [CrossRef]
- Zhai, J.; Gao, H.; Wang, S.; Zhang, S.; Qu, X.; Zhang, Y.; Tao, L.; Sun, J.; Song, Y.; Fu, L. Ginsenoside rg3 attenuates cisplatin-induced kidney injury through inhibition of apoptosis and autophagy-inhibited nlrp3. J. Biochem. Mol. Toxicol. 2021, 35, e22896. [Google Scholar] [CrossRef]
- Leta, B.; Kenenisa, C.; Wondimnew, T.; Sime, T. Evaluation of renoprotective effects of our locally grown green coffee beans against cisplatin-induced nephrotoxicity in swiss albino mice. Int. J. Nephrol. 2021, 2021, 2805068. [Google Scholar] [CrossRef]
- Fang, L.; Zhang, Y.; Wang, Q.; Zang, Y.; Li, Z.; Duan, Z.; Ren, J.; Xu, Z. A polysaccharide from huaier ameliorates cisplatin nephrotoxicity by decreasing oxidative stress and apoptosis via pi3k/akt signaling. Int. J. Biol. Macromol. 2019, 139, 932–943. [Google Scholar] [CrossRef]
- Sen, S.; De, B.; Devanna, N.; Chakraborty, R. Cisplatin-induced nephrotoxicity in mice: Protective role of leea asiatica leaves. Ren. Fail. 2013, 35, 1412–1417. [Google Scholar] [CrossRef]
- Mao, R.W.; He, S.P.; Lan, J.G.; Zhu, W.Z. Honokiol ameliorates cisplatin-induced acute kidney injury via inhibition of mitochondrial fission. Br. J. Pharmacol. 2022, 179, 3886–3904. [Google Scholar] [CrossRef]
- Ju, S.M.; Kim, M.S.; Jo, Y.S.; Jeon, Y.M.; Bae, J.S.; Pae, H.O.; Jeon, B.H. Licorice and its active compound glycyrrhizic acid ameliorates cisplatin-induced nephrotoxicity through inactivation of p53 by scavenging ros and overexpression of p21 in human renal proximal tubular epithelial cells. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 890–899. [Google Scholar] [PubMed]
- Zhou, M.; Dai, Y.; Ma, Y.; Yan, Y.; Hua, M.; Gao, Q.; Geng, X.; Zhou, Q. Protective effects of liquiritigenin against cisplatin-induced nephrotoxicity via nrf2/sirt3-mediated improvement of mitochondrial function. Molecules 2022, 27, 3823. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Sierra, T.; Medina-Campos, O.N.; Solano, J.D.; Ibarra-Rubio, M.E.; Pedraza-Chaverri, J. Isoliquiritigenin pretreatment induces endoplasmic reticulum stress-mediated hormesis and attenuates cisplatin-induced oxidative stress and damage in llc-pk1 cells. Molecules 2020, 25, 4442. [Google Scholar] [CrossRef] [PubMed]
- Omer Iqbal, M.; Bashir Yahya, E.; Andleeb, S.; Masood Ahmed, M.; Umar Javaid, M.; Shakeel, W.; Iqbal, I. In vivo assessment of reversing cisplatin-induced nephrotoxicity using jatropha mollissima crude extract and its potential cytotoxicity. Saudi J. Biol. Sci. 2021, 28, 7373–7378. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Jo, J.; Leem, J.; Park, K.K. Kahweol ameliorates cisplatin-induced acute kidney injury through pleiotropic effects in mice. Biomedicines 2020, 8, 572. [Google Scholar] [CrossRef] [PubMed]
- Masuda, Y.; Inoue, M.; Miyata, A.; Mizuno, S.; Nanba, H. Maitake beta-glucan enhances therapeutic effect and reduces myelosupression and nephrotoxicity of cisplatin in mice. Int. Immunopharmacol. 2009, 9, 620–626. [Google Scholar] [CrossRef]
- Yuan, L.; Yang, J.; Li, Y.; Yuan, L.; Liu, F.; Yuan, Y.; Tang, X. Matrine alleviates cisplatin-induced acute kidney injury by inhibiting mitochondrial dysfunction and inflammation via sirt3/opa1 pathway. J. Cell. Mol. Med. 2022, 26, 3702–3715. [Google Scholar] [CrossRef]
- Jain, A.; Singhai, A.K. Nephroprotective activity of momordica dioica roxb. In cisplatin-induced nephrotoxicity. Nat. Prod. Res. 2010, 24, 846–854. [Google Scholar] [CrossRef]
- Nematbakhsh, M.; Hajhashemi, V.; Ghannadi, A.; Talebi, A.; Nikahd, M. Protective effects of the morus alba l. Leaf extracts on cisplatin-induced nephrotoxicity in rat. Res. Pharm. Sci. 2013, 8, 71–77. [Google Scholar]
- el Daly, E.S. Protective effect of cysteine and vitamin e, crocus sativus and nigella sativa extracts on cisplatin-induced toxicity in rats. J. Pharm. Belg. 1998, 53, 87–93. [Google Scholar]
- Okur, M.E.; Ayla, S.; Karadag, A.E.; Cicek Polat, D.; Demirci, S.; Seckin, I. Opuntia ficus indica fruits ameliorate cisplatin-induced nephrotoxicity in mice. Biol. Pharm. Bull. 2020, 43, 831–838. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.R.; Lee, D.; Lee, H.J.; Noh, H.J.; Jung, K.; Kang, K.S.; Kim, K.H. Renoprotective chemical constituents from an edible mushroom, pleurotus cornucopiae in cisplatin-induced nephrotoxicity. Bioorg. Chem. 2017, 71, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Rajakrishnan, R.; Lekshmi, R.; Benil, P.B.; Thomas, J.; AlFarhan, A.H.; Rakesh, V.; Khalaf, S. Phytochemical evaluation of roots of plumbago zeylanica l. And assessment of its potential as a nephroprotective agent. Saudi J. Biol. Sci. 2017, 24, 760–766. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Yu, P.; Wang, T.T.; Du, Y.W.; Chen, Y.; Li, Z.; He, M.L.; Feng, L.; Li, H.R.; Han, X.; et al. Polydatin attenuates cisplatin-induced acute kidney injury by inhibiting ferroptosis. Oxid. Med. Cell. Longev. 2022, 2022, 9947191. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.J.; Leng, B.; Wu, Z.Y.; Bian, J.S. Polysulfide and hydrogen sulfide ameliorate cisplatin-induced nephrotoxicity and renal inflammation through persulfidating stat3 and ikkbeta. Int. J. Mol. Sci. 2020, 21, 7805. [Google Scholar] [CrossRef]
- Karwasra, R.; Kalra, P.; Gupta, Y.K.; Saini, D.; Kumar, A.; Singh, S. Antioxidant and anti-inflammatory potential of pomegranate rind extract to ameliorate cisplatin-induced acute kidney injury. Food Funct. 2016, 7, 3091–3101. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Li, C.; Li, Q.; Li, J.; Lu, X. Puerarin alleviates cisplatin-induced acute renal damage and upregulates microrna-31-related signaling. Exp. Ther. Med. 2020, 20, 3122–3129. [Google Scholar] [CrossRef]
- Aladaileh, S.H.; Al-Swailmi, F.K.; Abukhalil, M.H.; Ahmeda, A.F.; Mahmoud, A.M. Punicalagin prevents cisplatin-induced nephrotoxicity by attenuating oxidative stress, inflammatory response, and apoptosis in rats. Life Sci. 2021, 286, 120071. [Google Scholar] [CrossRef]
- Hasan, M.M.; Tasmin, M.S.; El-Shehawi, A.M.; Elseehy, M.M.; Reza, M.A.; Haque, A.R. Vesicarius l. Exerts nephroprotective effect against cisplatin-induced oxidative stress. BMC Complement. Med. Ther. 2021, 21, 225. [Google Scholar] [CrossRef]
- Kim, Y.J.; Lee, M.Y.; Son, H.Y.; Park, B.K.; Ryu, S.Y.; Jung, J.Y. Red ginseng ameliorates acute cisplatin-induced nephropathy. Planta Med. 2014, 80, 645–654. [Google Scholar] [CrossRef]
- Osman, A.M.; Telity, S.A.; Telity, S.A.; Damanhouri, Z.A.; Al-Harthy, S.E.; Al-Kreathy, H.M.; Ramadan, W.S.; Elshal, M.F.; Khan, L.M.; Kamel, F. Chemosensitizing and nephroprotective effect of resveratrol in cisplatin -treated animals. Cancer Cell Int. 2015, 15, 6. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, A.; Fanoudi, S.; Mollazadeh, H.; Aghaei, A.; Boroushaki, M.T. Protective effect of rheum turkestanicum against cisplatin by reducing oxidative stress in kidney tissue. J. Pharm. Bioallied Sci. 2018, 10, 66–71. [Google Scholar] [PubMed]
- Tlili, N.; Feriani, A.; Allagui, M.S.; Saadoui, E.; Khaldi, A.; Nasri, N. Effects of rhus tripartitum fruit extract on ccl4-induced hepatotoxicity and cisplatin-induced nephrotoxicity in rats. Can. J. Physiol. Pharmacol. 2016, 94, 801–807. [Google Scholar] [CrossRef] [PubMed]
- Tilyek, A.; Chai, C.; Hou, X.; Zhou, B.; Zhang, C.; Cao, Z.; Yu, B. The protective effects of ribes diacanthum pall on cisplatin-induced nephrotoxicity in mice. J. Ethnopharmacol. 2016, 178, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Radwan, R.R.; Abdel Fattah, S.M. Mechanisms involved in the possible nephroprotective effect of rutin and low dose gamma irradiation against cisplatin-induced nephropathy in rats. J. Photochem. Photobiol. B 2017, 169, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Park, C.H.; Lee, A.Y.; Kim, J.H.; Seong, S.H.; Jang, G.Y.; Cho, E.J.; Choi, J.S.; Kwon, J.; Kim, Y.O.; Lee, S.W.; et al. Protective effect of safflower seed on cisplatin-induced renal damage in mice via oxidative stress and apoptosis-mediated pathways. Am. J. Chin. Med. 2018, 46, 157–174. [Google Scholar] [CrossRef]
- Park, C.H.; Kim, M.J.; Yang, C.Y.; Yokozawa, T.; Shin, Y.S. Safflower seed extract synergizes the therapeutic effect of cisplatin and reduces cisplatin-induced nephrotoxicity in human colorectal carcinoma rko cells and rko-transplanted mice. Drug Discov. Ther. 2019, 13, 328–334. [Google Scholar] [CrossRef]
- Sohail, N.; Hira, K.; Kori, J.A.; Farhat, H.; Urooj, F.; Khan, W.; Sultana, V.; Ali, M.S.; Ehteshamul-Haque, S. Nephroprotective effect of ethanol extract and fractions of a sea lettuce, ulva fasciata against cisplatin-induced kidney injury in rats. Environ. Sci. Pollut. Res. Int. 2021, 28, 9448–9461. [Google Scholar] [CrossRef]
- Ali, B.H.; Al Salam, S.; Al Suleimani, Y.; Al Za’abi, M.; Ashique, M.; Manoj, P.; Sudhadevi, M.; Al Tobi, M.; Nemmar, A. Ameliorative effect of sesamin in cisplatin-induced nephrotoxicity in rats by suppressing inflammation, oxidative/nitrosative stress, and cellular damage. Physiol. Res. 2020, 69, 61–72. [Google Scholar] [CrossRef]
- Ikeda, Y.; Funamoto, M.; Kishi, S.; Imanishi, M.; Aihara, K.I.; Kashiwada, Y.; Tsuchiya, K. The novel preventive effect of a japanese ethical kampo extract formulation tj-90 (seihaito) against cisplatin-induced nephrotoxicity. Phytomedicine 2022, 103, 154213. [Google Scholar] [CrossRef]
- Elhady, S.S.; Abdelhameed, R.F.A.; Mehanna, E.T.; Wahba, A.S.; Elfaky, M.A.; Koshak, A.E.; Noor, A.O.; Bogari, H.A.; Malatani, R.T.; Goda, M.S. Metabolic profiling, chemical composition, antioxidant capacity, and in vivo hepato- and nephroprotective effects of sonchus cornutus in mice exposed to cisplatin. Antioxidants 2022, 11, 819. [Google Scholar] [CrossRef] [PubMed]
- Ademiluyi, A.O.; Oboh, G.; Agbebi, O.J.; Oyeleye, S.I. Dietary inclusion of sorghum (sorghum bicolour) straw dye protects against cisplatin-induced nephrotoxicity and oxidative stress in rats. Pharm. Biol. 2014, 52, 829–834. [Google Scholar] [CrossRef]
- Sadeghi, H.; Mansourian, M.; Panahi Kokhdan, E.; Salehpour, Z.; Sadati, I.; Abbaszadeh-Goudarzi, K.; Asfaram, A.; Doustimotlagh, A.H. Antioxidant and protective effect of stachys pilifera benth against nephrotoxicity induced by cisplatin in rats. J. Food Biochem. 2020, 44, e13190. [Google Scholar] [CrossRef] [PubMed]
- Potocnjak, I.; Broznic, D.; Kindl, M.; Kropek, M.; Vladimir-Knezevic, S.; Domitrovic, R. Stevia and stevioside protect against cisplatin nephrotoxicity through inhibition of erk1/2, stat3, and nf-kappab activation. Food Chem. Toxicol. 2017, 107, 215–225. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.; Kim, Y.J.; Han, I.H.; Lee, D.; Ham, J.; Kang, K.S.; Lee, J.W. The synthesis of sulforaphane analogues and their protection effect against cisplatin induced cytotoxicity in kidney cells. Bioorg. Med. Chem. Lett. 2015, 25, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Vu-Huynh, K.L.; Le, T.H.V.; Nguyen, H.T.; Kim, H.M.; Kang, K.S.; Park, J.H.; Nguyen, M.D. Increase in protective effect of panax vietnamensis by heat processing on cisplatin-induced kidney cell toxicity. Molecules 2019, 24, 4627. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, Y.H.; Tang, Y.R.; Lan, J.; Huang, Z.Y.; Tian, W.; Huang, Q.; Peng, Y.; Gao, Y.; Hu, Y.Q.; et al. Protective effects of tanshinone against cisplatin-induced nephrotoxicity in mice. Iran. J. Basic Med. Sci. 2022, 25, 414–418. [Google Scholar]
- Kalra, P.; Karwasra, R.; Gupta, Y.K.; Ray, S.B.; Singh, S. Terminalia chebula supplementation attenuates cisplatin-induced nephrotoxicity in wistar rats through modulation of apoptotic pathway. Nat. Prod. Res. 2019, 33, 1641–1645. [Google Scholar] [CrossRef]
- Song, K.I.; Park, J.Y.; Lee, S.; Lee, D.; Jang, H.J.; Kim, S.N.; Ko, H.; Kim, H.Y.; Lee, J.W.; Hwang, G.S.; et al. Protective effect of tetrahydrocurcumin against cisplatin-induced renal damage: In vitro and in vivo studies. Planta Med. 2015, 81, 286–291. [Google Scholar] [CrossRef]
- Guan, T.; Zheng, Y.; Jin, S.; Wang, S.; Hu, M.; Liu, X.; Huang, S.; Liu, Y. Troxerutin alleviates kidney injury in rats via pi3k/akt pathway by enhancing map4 expression. Food Nutr. Res. 2022, 66. [Google Scholar] [CrossRef]
- Naushad, M.; Urooj, M.; Ahmad, T.; Husain, G.M.; Kazmi, M.H.; Zakir, M. Nephroprotective effect of apium graveolens l. Against cisplatin-induced nephrotoxicity. J. Ayurveda Integr. Med. 2021, 12, 607–615. [Google Scholar] [CrossRef] [PubMed]
- Eren, H.; Aydin, H.R.; Tumkaya, L.; Kazaz, I.O.; Kalkan, Y.; Kazaz, S.N.; Mercantepe, T.; Horsanali, M.O.; Yilmaz, A. Whortleberry protects kidney against the cisplatin-induced nephrotoxicity: An experimental study. Ren. Fail. 2018, 40, 466–474. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Joshi, A.; Hemalatha, S. Protective effect of withania coagulans fruit extract on cisplatin-induced nephrotoxicity in rats. Pharmacogn. Res. 2017, 9, 354–361. [Google Scholar]
- Kandemir, F.M.; Yildirim, S.; Caglayan, C.; Kucukler, S.; Eser, G. Protective effects of zingerone on cisplatin-induced nephrotoxicity in female rats. Environ. Sci. Pollut. Res. Int. 2019, 26, 22562–22574. [Google Scholar] [CrossRef] [PubMed]
- Kensler, T.W.; Wakabayashi, N.; Biswal, S. Cell survival responses to environmental stresses via the keap1-nrf2-are pathway. Annu. Rev. Pharmacol. Toxicol. 2007, 47, 89–116. [Google Scholar] [CrossRef]
- Jaiswal, A.K. Nrf2 signaling in coordinated activation of antioxidant gene expression. Free Radic. Biol. Med. 2004, 36, 1199–1207. [Google Scholar] [CrossRef]
- Guerrero-Hue, M.; Rayego-Mateos, S.; Vazquez-Carballo, C.; Palomino-Antolin, A.; Garcia-Caballero, C.; Opazo-Rios, L.; Morgado-Pascual, J.L.; Herencia, C.; Mas, S.; Ortiz, A.; et al. Protective role of nrf2 in renal disease. Antioxidants 2020, 10, 39. [Google Scholar] [CrossRef]
- Wu, J.; Li, R.; Li, W.; Ren, M.; Thangthaeng, N.; Sumien, N.; Liu, R.; Yang, S.; Simpkins, J.W.; Forster, M.J.; et al. Administration of 5-methoxyindole-2-carboxylic acid that potentially targets mitochondrial dihydrolipoamide dehydrogenase confers cerebral preconditioning against ischemic stroke injury. Free Radic. Biol. Med. 2017, 113, 244–254. [Google Scholar] [CrossRef]
- Ali, F.E.M.; Hassanein, E.H.M.; El-Bahrawy, A.H.; Omar, Z.M.M.; Rashwan, E.K.; Abdel-Wahab, B.A.; Abd-Elhamid, T.H. Nephroprotective effect of umbelliferone against cisplatin-induced kidney damage is mediated by regulation of nrf2, cytoglobin, sirt1/foxo-3, and nf- kb-p65 signaling pathways. J. Biochem. Mol. Toxicol. 2021, 35, e22738. [Google Scholar] [CrossRef]
- Mahran, Y.F. New insights into the protection of growth hormone in cisplatin-induced nephrotoxicity: The impact of igf-1 on the keap1-nrf2/ho-1 signaling. Life Sci. 2020, 253, 117581. [Google Scholar] [CrossRef]
- El-Sayed, R.M.; Abo El Gheit, R.E.; Badawi, G.A. Vincamine protects against cisplatin induced nephrotoxicity via activation of nrf2/ho-1 and hindering tlr4/ ifn-gamma/cd44 cells inflammatory cascade. Life Sci. 2021, 272, 119224. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Cai, F.; Zhou, N.; Liu, S.; Wang, P.; Zhang, S.; Zhang, Y.; Zhang, A.; Jia, Z.; Huang, S. Dimethyl fumarate prevents ferroptosis to attenuate acute kidney injury by acting on nrf2. Clin. Transl. Med. 2021, 11, e382. [Google Scholar] [CrossRef] [PubMed]
- Barakat, N.; Barakat, L.A.A.; Zakaria, M.M.; Khirallah, S.M. Diacerein ameliorates kidney injury induced by cisplatin in rats by activation of nrf2/ho-1 pathway and bax down-regulation. Saudi J. Biol. Sci. 2021, 28, 7219–7226. [Google Scholar] [CrossRef] [PubMed]
- Hosoya, T.; Maruyama, A.; Kang, M.I.; Kawatani, Y.; Shibata, T.; Uchida, K.; Warabi, E.; Noguchi, N.; Itoh, K.; Yamamoto, M. Differential responses of the nrf2-keap1 system to laminar and oscillatory shear stresses in endothelial cells. J. Biol. Chem. 2005, 280, 27244–27250. [Google Scholar] [CrossRef]
- Motohashi, H.; Yamamoto, M. Nrf2-keap1 defines a physiologically important stress response mechanism. Trends Mol. Med. 2004, 10, 549–557. [Google Scholar] [CrossRef]
- Villeneuve, N.F.; Lau, A.; Zhang, D.D. Regulation of the nrf2-keap1 antioxidant response by the ubiquitin proteasome system: An insight into cullin-ring ubiquitin ligases. Antioxid. Redox Signal. 2011, 13, 1699–1712. [Google Scholar] [CrossRef]
- Wang, X.Y.; Wang, Z.Y.; Zhu, Y.S.; Zhu, S.M.; Fan, R.F.; Wang, L. Alleviation of cadmium-induced oxidative stress by trehalose via inhibiting the nrf2-keap1 signaling pathway in primary rat proximal tubular cells. J. Biochem. Mol. Toxicol. 2018, 32, e22011. [Google Scholar] [CrossRef]
- Yan, W.; Xu, Y.; Yuan, Y.; Tian, L.; Wang, Q.; Xie, Y.; Shao, X.; Zhang, M.; Ni, Z.; Mou, S. Renoprotective mechanisms of astragaloside iv in cisplatin-induced acute kidney injury. Free Radic. Res. 2017, 51, 669–683. [Google Scholar] [CrossRef]
- Ning, Y.C.; Cai, G.Y.; Zhuo, L.; Gao, J.J.; Dong, D.; Cui, S.Y.; Shi, S.Z.; Feng, Z.; Zhang, L.; Sun, X.F.; et al. Beneficial effects of short-term calorie restriction against cisplatin-induced acute renal injury in aged rats. Nephron Exp. Nephrol. 2013, 124, 19–27. [Google Scholar] [CrossRef]
- Estrela, G.R.; Wasinski, F.; Batista, R.O.; Hiyane, M.I.; Felizardo, R.J.; Cunha, F.; de Almeida, D.C.; Malheiros, D.M.; Camara, N.O.; Barros, C.C.; et al. Caloric restriction is more efficient than physical exercise to protect from cisplatin nephrotoxicity via ppar-alpha activation. Front. Physiol. 2017, 8, 116. [Google Scholar] [CrossRef]
- Mikami, D.; Kobayashi, M.; Uwada, J.; Yazawa, T.; Kamiyama, K.; Nishimori, K.; Nishikawa, Y.; Morikawa, Y.; Yokoi, S.; Takahashi, N.; et al. Beta-hydroxybutyrate, a ketone body, reduces the cytotoxic effect of cisplatin via activation of hdac5 in human renal cortical epithelial cells. Life Sci. 2019, 222, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Duan, Z.Y.; Liu, J.Q.; Yin, P.; Li, J.J.; Cai, G.Y.; Chen, X.M. Impact of aging on the risk of platinum-related renal toxicity: A systematic review and meta-analysis. Cancer Treat. Rev. 2018, 69, 243–253. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Han, Y.K.; Kong, M.J.; Park, K.M. Short-term control of diet affects cisplatin-induced acute kidney injury through modulation of mitochondrial dynamics and mitochondrial gsh. Physiol. Rep. 2022, 10, e15348. [Google Scholar] [CrossRef] [PubMed]
- Duan, Z.; Cai, G.; Li, J.; Chen, X. Cisplatin-induced renal toxicity in elderly people. Ther. Adv. Med. Oncol. 2020, 12, 1758835920923430. [Google Scholar] [CrossRef]
- Guan, Y.; Wang, S.R.; Huang, X.Z.; Xie, Q.H.; Xu, Y.Y.; Shang, D.; Hao, C.M. Nicotinamide mononucleotide, an nad(+) precursor, rescues age-associated susceptibility to aki in a sirtuin 1-dependent manner. J. Am. Soc. Nephrol. 2017, 28, 2337–2352. [Google Scholar] [CrossRef]
- Barinda, A.J.; Arozal, W.; Sandhiutami, N.M.D.; Louisa, M.; Arfian, N.; Sandora, N.; Yusuf, M. Curcumin prevents epithelial-to mesenchymal transition-mediated ovarian cancer progression through nrf2/etbr/et-1 axis and preserves mitochondria biogenesis in kidney after cisplatin administration. Adv. Pharm. Bull. 2022, 12, 128–141. [Google Scholar] [CrossRef]
- Ko, J.W.; Shin, N.R.; Jung, T.Y.; Shin, I.S.; Moon, C.; Kim, S.H.; Lee, I.C.; Kim, S.H.; Yun, W.K.; Kim, H.C.; et al. Melatonin attenuates cisplatin-induced acute kidney injury in rats via induction of anti-aging protein, klotho. Food Chem. Toxicol. 2019, 129, 201–210. [Google Scholar] [CrossRef]



| Natural Product | Rodent Model | Mechanism | Reference |
|---|---|---|---|
| 4-hydroxyhalcone | HEK293 cell | Inhibiting ROS production | [108] |
| 6-shogaol | Mouse | Anti-oxidative stress | [109] |
| 10-dehydrogingerdione | Rat | Increasing GSH content | [110] |
| Acacia hydaspica R. Parker | Rat | Anti-oxidative damage | [111] |
| Alhagi camelorum | Rat | Increasing antioxidant activities | [112] |
| Andrographis Paniculata | Rat | Nrf2 signaling | [113] |
| Artemisia asiatica | LLC-PK1 cells | Anti-oxidative stress | [114] |
| Benzyl Isothiocyanate | Mouse | Anti-oxidative stress | [115] |
| Berberis integerrima | Rat | Anti-oxidative damage | [116] |
| Bisabolol | Mouse | Mitigating oxidative stress | [117] |
| Black bean extract | Rat | Anti-oxidation and anti-inflammation | [118] |
| β-lapachone | Mouse | Increasing NAD levels | [60] |
| Carrichtera annua DC | Rat | Anti-oxidative stress | [119] |
| Carvacrol | Rat | Anti-oxidative stress | [120] |
| Catapol | Mouse | Anti-oxidative stress | [121] |
| Chalcone | Mouse | Inhibiting necroptosis | [122] |
| Citrullus colocynthis Linn | Rat | Anti-oxidative stress | [123] |
| Citrus aurantium | Rat | Not determined | [124] |
| Clinacanthus nutans | NRK-52E cells | various protective effects | [125] |
| Coleus amboinicus extract | Rat | Increasing TGF-1β | [126] |
| Curcumin | Mouse | Anti-inflammation | [127] |
| Coumarins | Mouse | Suppressing renal inflammation | [128] |
| D-allose | Mouse | Suppressing renal inflammation | [129] |
| Daidzein | Mouse | Anti-oxidative stress | [130] |
| Danshen | Mouse | Nrf2 signaling | [131] |
| Daucus carota | Rat | Not determined | [132] |
| Dendropanoxide | Rat | AMPK/mTOR pathway | [133] |
| Dioscin | Rat/Mouse | Maintaining redox balance | [89] |
| Emodin | Rat tubular cells | Activating autophagy | [134] |
| Ephedra alata extract | Mouse | Reducing oxidative stress | [135] |
| Exacum lawii extract | Rat | Anti-oxidative damage | [136] |
| Ficus carica L. leaves | Rat | Anti-oxidative stress | [137] |
| Filipendula ulmaria extract | Rat | Anti-oxidative stress | [138] |
| Formononetin | Rat | Activation of Nrf2 pathway | [139] |
| Forskolin | Rat | Anti-oxidation and anti-inflammation | [140] |
| Galangin | Mouse | Attenuating oxidative stress | [141] |
| Ganoderma lucidum | Mouse/rat | Antioxidation | [142] |
| Garlic extract | Rat | Anti-oxidative stress | [143] |
| Genistein | Mouse | Decreasing ROS production | [144] |
| Ginkgo biloba | Rat | Inhibiting renal fibrosis | [145] |
| Ginsenoside Rg3 | Mouse | Attenuating apoptosis | [146] |
| Green coffee beans extract | Mouse | Not determined | [147] |
| Huaier polysaccharide | Mouse | Anti-oxidative stress | [148] |
| Leea asiatica leaves | Mouse | Inhibiting lipid peroxidation | [149] |
| Honokiol | Mouse | Inhibiting mitochondrial fission | [150] |
| Licorice | HK-2 cells | Scavenging ROS | [151] |
| Liquiritigenin | Mouse | Nrf2/Sirt3 signaling pathways | [152] |
| Iosliquiritigenin | LLC-PK1 cells | Anti-oxidative stress | [153] |
| Jatropha mollissima extract | Rat | Anti-oxidative stress | [154] |
| Kahweol | Mouse | Suppressing inflammation | [155] |
| Maitake beta-glucan | Mouce | Anti-apoptosis | [156] |
| Matrine | Mouse | SIT3/OPA1 pathway | [157] |
| Momordica dioica Roxb. | Mouse | Anti-oxidative damage | [158] |
| Morus alba L extract | Rat | Anti-oxidative stress | [159] |
| Nigella sativa seed extract | Rat | Anti-oxidative damage | [160] |
| Opuntia ficus indica | Mouse | Anti-oxidative stress | [161] |
| Pleurotus cornucopiae | LLC-PK1 cells | Not determined | [162] |
| Plumbago zeylanica L | Mouse | Anti-oxidative stress | [163] |
| Polydatin | Mouse | Anti-oxidative stress | [164] |
| Polysulfide | Mouse | Anti-inflammation | [165] |
| Pomegranate rind extract | Rat | Anti-apoptosis | [166] |
| Puerarin | Rat | Upregulating microRNA-31 | [167] |
| Punicalagin | Rat | Anti-oxidative stress | [168] |
| R. vesicarius L extract | Mouse | Anti-oxidative stress | [169] |
| Red ginseng | Rat | Anti-lipid peroxidation | [170] |
| Resveratrol | Rat | Anti-oxidative damage | [171] |
| Rheum turkestanicum | Rat | Decreasing oxidative damage | [172] |
| Rhus tripartitum extract | Rat | Increasing antioxidant potential | [173] |
| Ribes diacanthum Pall | Mouse | Enhancing antioxidant potential | [174] |
| Rutin | Rat | Anti-oxidative stress | [175] |
| Safflower seed extract | Mouse | Anti-oxidative stress | [176,177] |
| Sea lettuce extract | Rat | Anti-oxidative stress | [178] |
| Sesamin | Rat | Anti-oxidative stress | [179] |
| Seihaito (TJ-90) | Mouse | Anti-oxidative stress | [180] |
| Sonchus cornutus | Mouse | Anti-oxidative stress | [181] |
| Sorghum straw dye | Rat | Anti-oxidative stress | [182] |
| Stachys pilifera benth | Rat | Anti-oxidative damage | [183] |
| Stevia | Mouse | Anti-oxidative stress | [184] |
| Sulforaphane analogues | LLC-PK1 cells | Anti-apoptosis | [185] |
| Vietnamese Ginseng | LLC-PK1 cells | Improving kidney function | [186] |
| Tanshinone I | Mouse | Increasing antioxidant enzymes | [187] |
| Terminalia chebula | Rat | Anti-apoptosis | [188] |
| Tetrahydrocurcumin | Rat | Decreasing oxidative damage | [189] |
| Troxerutin | Rat | PI3K/AKT pathway | [190] |
| Tukhm-e-karafs | Rat | Reducing ROS production | [191] |
| Whortleberry | Rat | Antioxidation | [192] |
| WIthania coagulans extract | Rat | Anti-oxidative stress | [193] |
| Zingerone | Rat | Inhibiting oxidative stress | [194] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iskander, A.; Yan, L.-J. Cisplatin-Induced Kidney Toxicity: Potential Roles of Major NAD+-Dependent Enzymes and Plant-Derived Natural Products. Biomolecules 2022, 12, 1078. https://doi.org/10.3390/biom12081078
Iskander A, Yan L-J. Cisplatin-Induced Kidney Toxicity: Potential Roles of Major NAD+-Dependent Enzymes and Plant-Derived Natural Products. Biomolecules. 2022; 12(8):1078. https://doi.org/10.3390/biom12081078
Chicago/Turabian StyleIskander, Amany, and Liang-Jun Yan. 2022. "Cisplatin-Induced Kidney Toxicity: Potential Roles of Major NAD+-Dependent Enzymes and Plant-Derived Natural Products" Biomolecules 12, no. 8: 1078. https://doi.org/10.3390/biom12081078
APA StyleIskander, A., & Yan, L.-J. (2022). Cisplatin-Induced Kidney Toxicity: Potential Roles of Major NAD+-Dependent Enzymes and Plant-Derived Natural Products. Biomolecules, 12(8), 1078. https://doi.org/10.3390/biom12081078







