Current Perspectives on Taxanes: Focus on Their Bioactivity, Delivery and Combination Therapy
Abstract
1. Introduction
1.1. Natural Sources of Paclitaxel and Isolation Processes
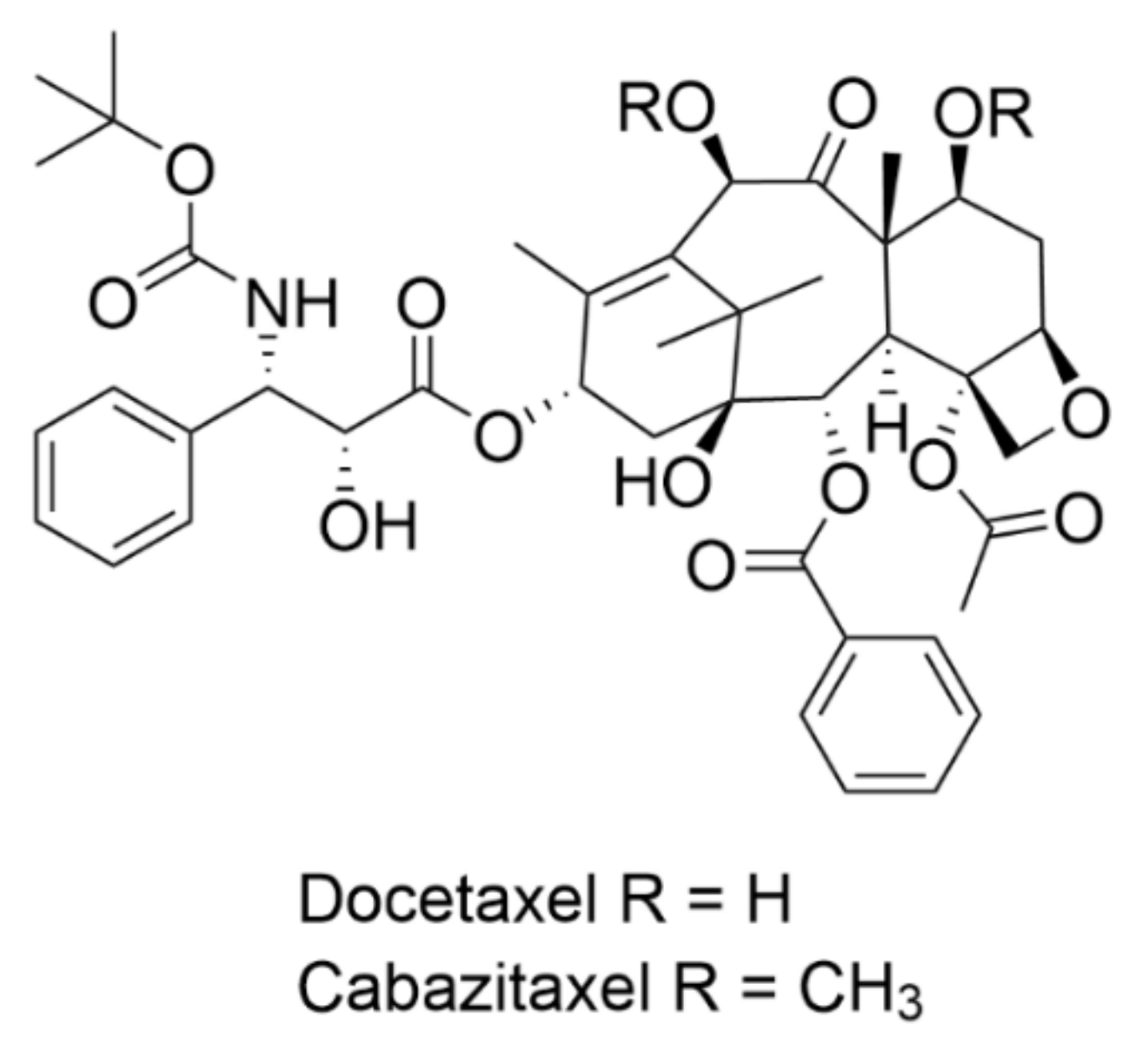
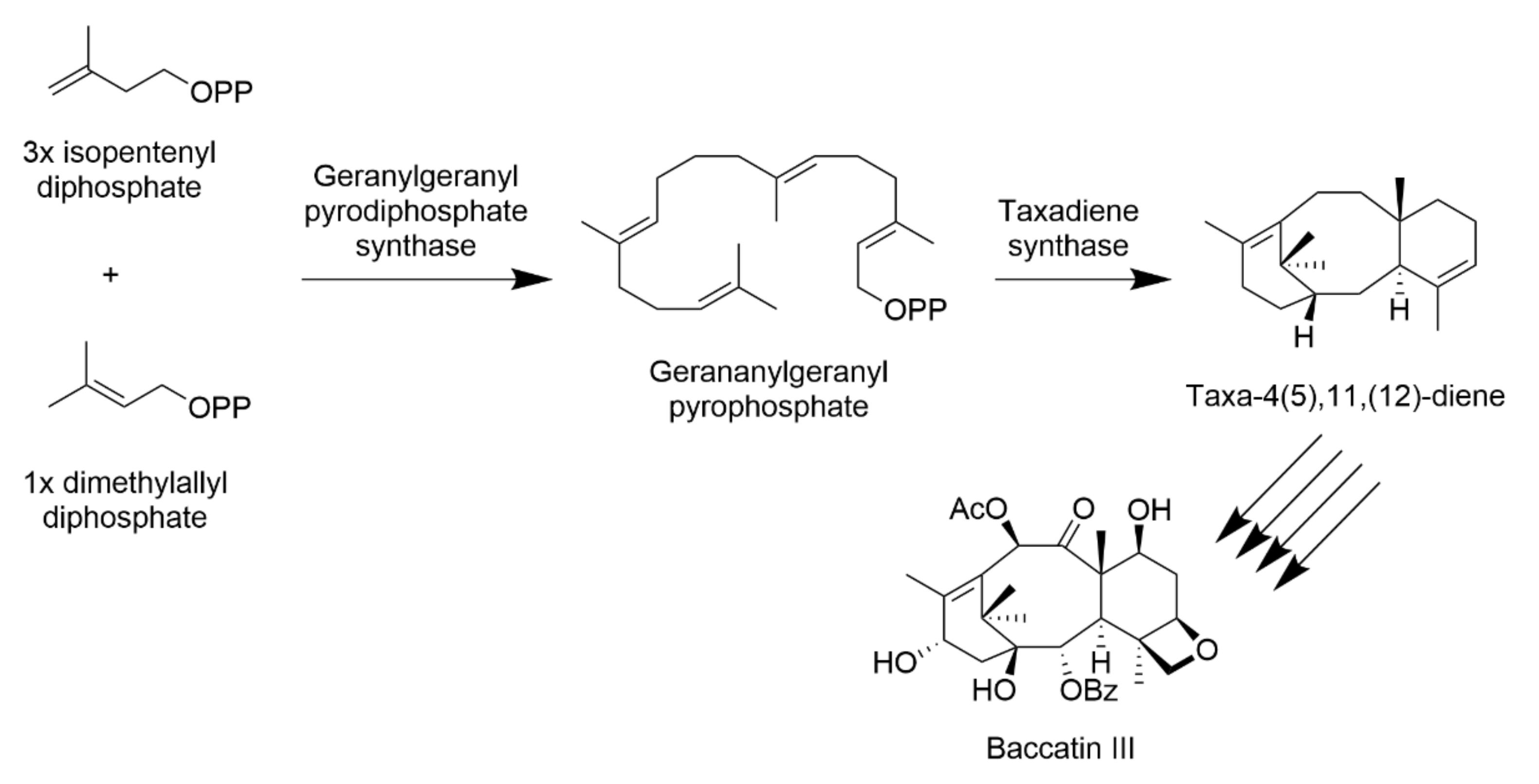
1.2. Biosynthesis, Synthesis, and Semisynthesis of Taxanes
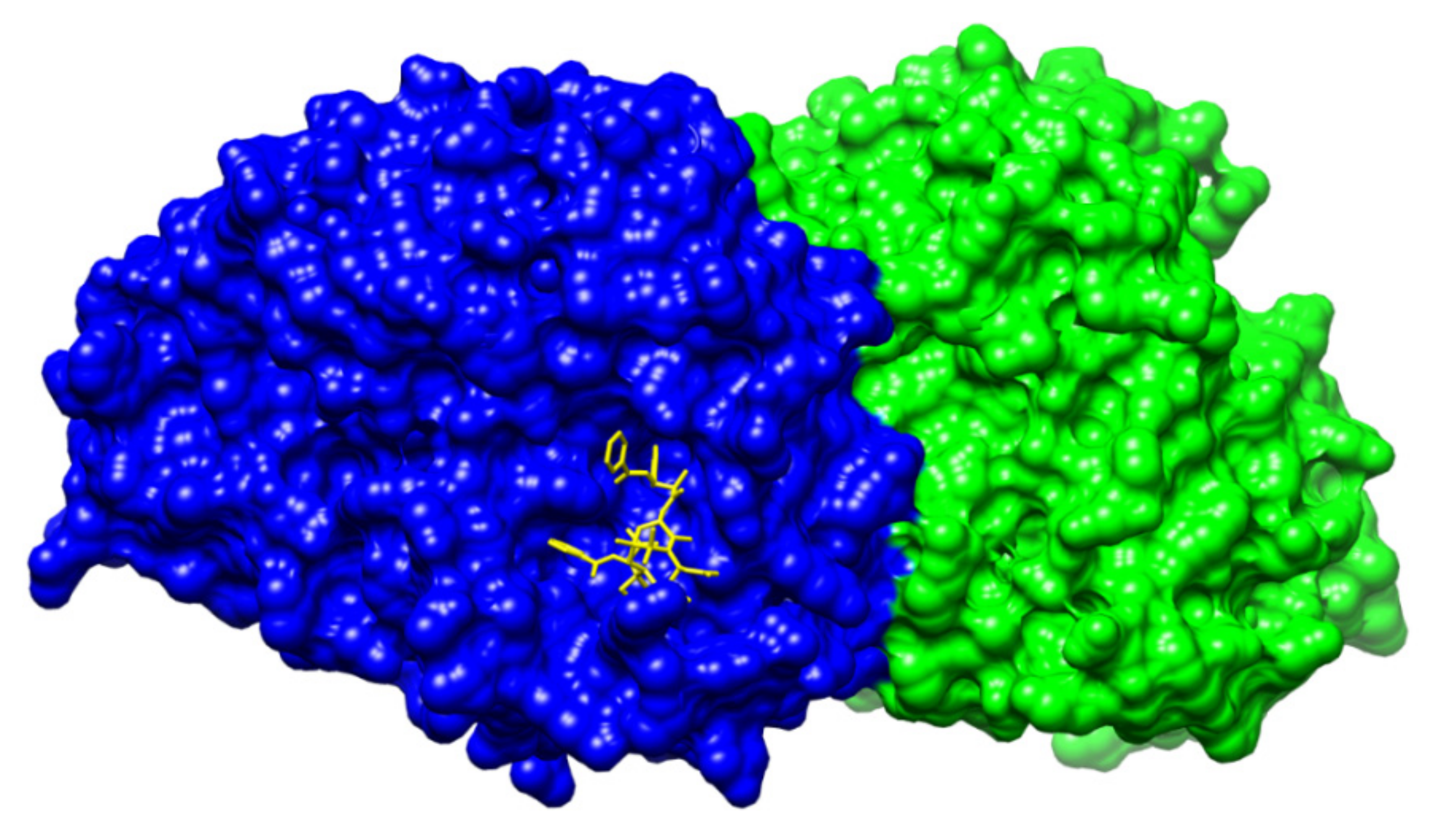
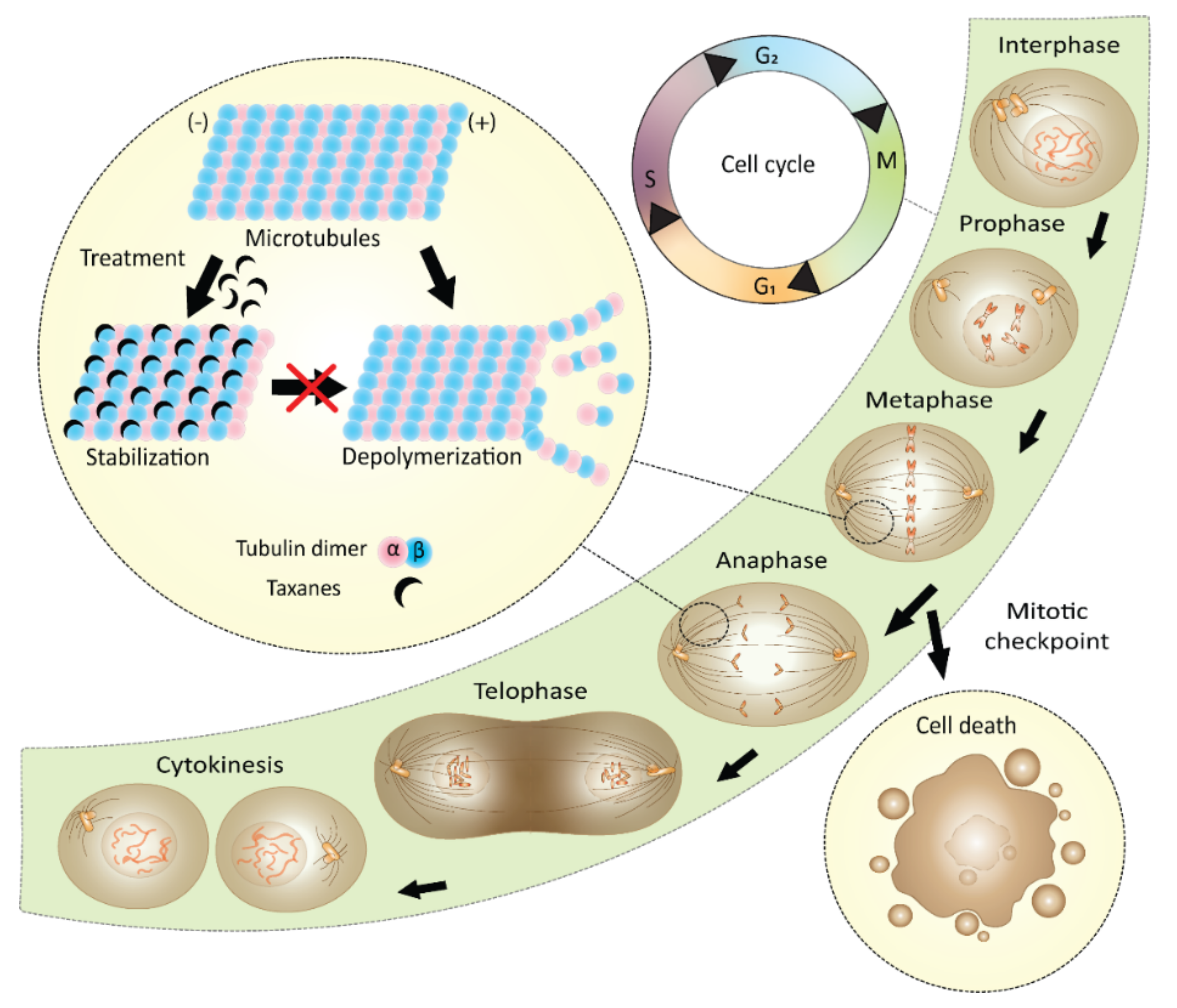
1.3. Mechanism of Action of Paclitaxel
1.4. Taxane Formulations for Improved Solubility and Tumor Delivery
1.4.1. Liposomes and Polymeric Micelles Containing Taxanes
1.4.2. Hydrogel Formulations of Taxanes
1.4.3. Formulations for Targeted Delivery of Taxanes
1.4.4. Derivatives of Taxanes for Improved Tumor Targeting
1.5. Mechanisms of Cancer Cell Resistance to Taxanes
- One of the most commonly known apoptotic factors linked to cancer cell resistance to paclitaxel is Bcl-2 protein, a proton-efflux pump acting as a pro-survival factor. Interestingly, this protein contains a paclitaxel-binding domain like in the β-tubulin and, therefore, it is strongly bound by paclitaxel. For sure, in nature, nothing is just a coincidence. Therefore, a naturally occurring ligand of both of these proteins must exist. Interestingly, this ligand has already been identified and it is the nerve growth factor IB (Nur77 or also NGFIB). Nur77 physiologically participates in cell death signaling by translocation from the nucleus to mitochondria and binding to Bcl-2, thus changing its properties from anti-apoptotic to pro-apoptotic [102]. Given the anti-apoptotic properties of Bcl-2, upregulation of this factor is often linked to cancer cell resistance to paclitaxel. To overcome this resistance, Wang et al. [103] suggested a co-delivery of paclitaxel with plasmid deoxyribonucleic acid (pDNA) for Nur77 in cationic polymeric micelles. This approach significantly increased the sensitivity of resistant cancer cell lines to taxane treatment. Besides Nur77, there are also further possibilities to regulate the Bcl-2 family of proteins, reviewed in ref. [104]. Bcl-2 proteins are not the only pump proteins playing a role in cell resistance to taxanes.
- A significant contribution to cancer cell resistance to taxanes is made by drug efflux pumps, which are responsible for decreasing the effective concentration of a drug in a cell. One of the most common pumps is P-gp, which belongs to the ATP-binding cassette (ABC) transporters. Proteins such as P-gp are commonly overexpressed in multidrug-resistant cancer cells. So far, several approaches to avoid cell efflux of paclitaxel have been explored. Mainly, the option of paclitaxel administration in combination with diverse P-gp inhibitors such as quinines, verapamil, and curcumin have been examined [105,106,107]. The subgroup of ABCs mostly involved in cancer cell resistance to taxanes is ABCB1. Zhong et al. [108] suggested that ABCB1 polymorphisms could be used for predicting the effectiveness of taxane treatment. In their study on patients with non-small cell lung carcinoma, they identified two sites in the ABCB1 gene, the mutations of which significantly correlated with enhanced cytotoxicity after taxane treatment. Generally, individuals with the wild-type genes had a longer progression-free survival rate. However, the study was conducted on a very specific and not very large group of Chinese patients and, therefore, it is not possible to make a general conclusion based on these results. Nevertheless, it has been shown that a correlation between the expression of particular ABC types and taxane treatment effectiveness exists; thus, further studies in this field are desirable.
- Cancer cell resistance to taxanes may also consist of decreased cell uptake of the drugs. Taxanes, based on their hydrophobicity, enter cells rapidly via passive diffusion. Logically, changes in cell membrane composition may impede this process, mainly increased volume of cholesterol in the membrane. Taxanes also use specific transporters in the membranes to access cells. One of such transporters, organic anion transporting polypeptide 1B3, is often downregulated in chemoresistant cancer cells. Several chemoresistance mechanisms linked to decreased drug uptake were described in the case of paclitaxel nanoformulations, see Section 1.6. The lipophilic nanoformulations use the endocytic pathway to move paclitaxel into cells; thus, malfunctions of endocytosis may influence paclitaxel’s ability to enter cells. For example, modifications of the actin protein playing a crucial role in micropinocytosis, often correlating with cell resistance to taxane treatment. Besides actin, plastin-3 is another protein playing a role in endocytosis. Its downregulation significantly increases paclitaxel sensitivity. Cell chemoresistance caused by decreased drug uptake might be overcome by derivatization of the drug or by creating novel formulations. For example, mimicking low-density lipoproteins, as cholesterol-bound paclitaxel nanocarriers, might be a possible way to go [109].
- An interesting cause of cancer cell resistance to taxane treatment is hypoxia. Hypoxic microenvironments are present in solid tumors, in which there is a reduced amount of blood vessels since tumor growth does not always correlate with the level of angiogenesis. When administered intravenously, the lack of vessels means that the opportunity for the drug to enter the tumor site is significantly reduced. At the same time, the rapidly proliferating tumor cells lacking blood vessels are promptly depleted in oxygen. Hypoxia triggers several signaling pathways leading to cell chemoresistance. The starting process of these pathways is the translocation of hypoxia-inducible factor 1 (HIF-1) into the cell nucleus and subsequent dimerization and, thus, induction of expression of genes involved in hypoxic response. Several studies confirm that silencing the gene expression of HIF-1 in cancer cells increases cell sensitivity to paclitaxel. Besides HIF-1 regulated pathways, during the hypoxic response, for example, the aforementioned ABCB1 is also overexpressed, or autophagy, which inhibits paclitaxel activity, occurs, illustrating the complexity of hypoxia’s contribution to cell resistance to taxanes. Zeng et al. also reported a certain correlation between HIF levels and changes in the morphology of tubulin. That would explain the increased resistance to paclitaxel in HIF-expressing cells [110,111,112].
- Recent studies reveal that miRNAs play also a noticeable role in cell resistance to taxanes. The cellular function of miRNAs is to regulate gene expression by binding to messenger-RNAs (mRNAs). The most recent study discussing their role in cell resistance to taxanes was performed by Chen et al. [113], who identified two miRNAs, miR-335-5p and hsa-let-7c-5p, and their gene targets, chemokine (C-X-C motif) ligand 9, C-C chemokine receptor type 7, and suppressor of cytokine signaling 1, which are all linked to cell resistance to taxanes. Certain miRNA profiles are typical for paclitaxel-sensitive or chemoresistant tumors; these molecules could be used in the initial screening preceding the personalized treatment of cancer patients [114].
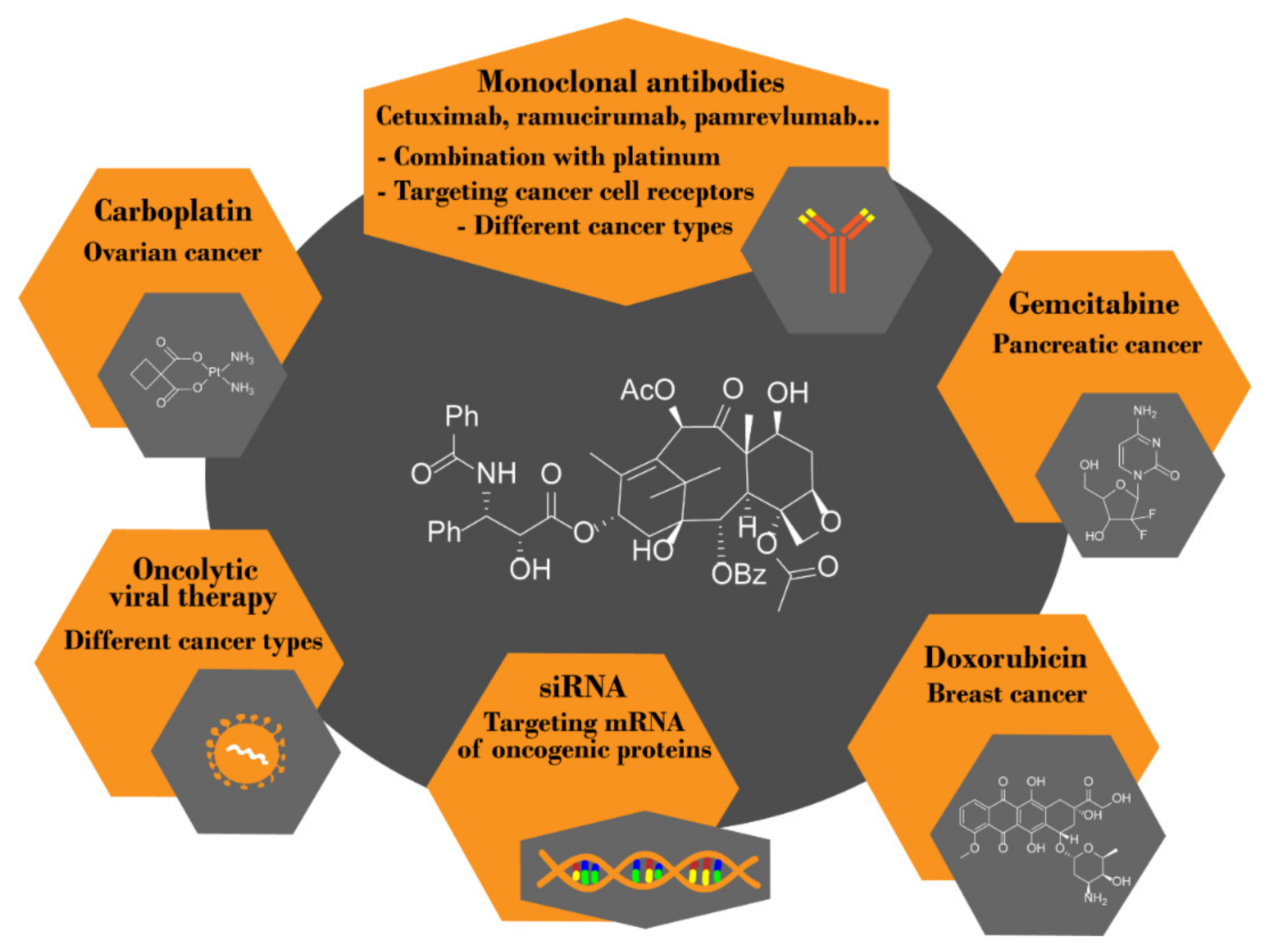
1.6. Combination Therapy with Taxanes
1.6.1. Combination of Paclitaxel and Immunotherapy
1.6.2. Combination of Paclitaxel with Diverse Low-Molecular Inhibitors
1.6.3. Other Therapeutical Combinations of Paclitaxel
2. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviation
| 10-DAB | 10-deacetyl baccatin III |
| ABC | ATP-binding cassette transporters |
| AUC | Area under curve |
| Bcl-2 | B-cell lymphoma 2 |
| CD | Cluster of differenciation |
| CSC | cancer stem cells |
| DNA | deoxyribonucleic acid |
| EGFR | the epidermal growth factor receptor |
| EMA | European Medicines Agency |
| FDA | U.S. Food and Drug Administration |
| GGPP | geranylgeranyl pyrophosphate |
| HIF-1 | hypoxia-inducible factor 1 |
| IL-6 | interleukin 6 |
| IL-20 | interleukin 20 |
| mAbs | monoclonal antibodies |
| miRNAs | microRNAs |
| mPEG | poly(ethylene glycol) methyl ether |
| Nur77 | nerve growth factor IB |
| p53 | the cellular tumor antigen p53 |
| P-gp | P-glycoprotein |
| PI3K/Akt | phosphatidylinositol 3-kinase/protein kinase B |
| PDLLA | monomethoxy poly(ethylene glycol)-block-poly(D,L-lactide) |
| PIPN | paclitaxel-induced peripheral neuropathy |
| PLGA | polylactic-co-glycolic acid |
| siRNA | short interfering RNAs |
| TRAF6 | tumor necrosis factor receptor-associated factor 6 |
| TUBB3 | class III β-tubulin |
| VEGF | vascular endothelial growth factor |
References
- Wani, M.C.; Taylor, H.L.; Wall, M.E.; Coggon, P.; McPhail, A.T. Plant antitumor agents. VI. Isolation and structure of taxol, a novel antileukemic and antitumor agent from Taxus brevifolia. J. Am. Chem. Soc. 1971, 93, 2325–2327. [Google Scholar] [CrossRef]
- Menzin, A.W.; King, S.A.; Aikins, J.K.; Mikuta, J.J.; Rubin, S.C. Taxol (paclitaxel) was approved by FDA for the treatment of patients with recurrent ovarian cancer. Gynecol. Oncol. 1994, 54, 103. [Google Scholar] [PubMed]
- Leo, C.P.; Hentschel, B.; Szucs, T.D.; Leo, C. FDA and EMA Approvals of new breast cancer drugs—A comparative regulatory analysis. Cancers 2020, 12, 437. [Google Scholar] [CrossRef]
- Paller, C.J.; Antonarakis, E.S. Cabazitaxel: A novel second-line treatment for metastatic castration-resistant prostate cancer. Drug Des. Dev. Ther. 2011, 5, 117–124. [Google Scholar] [CrossRef]
- Cope, E.A. Taxaceae: The genera and cultivated species. Bot. Rev. 1998, 64, 291–322. [Google Scholar] [CrossRef]
- World Botanical. Available online: http://www.worldbotanical.com/TAXNA.HTM (accessed on 9 March 2021).
- Bui-Khac, T.; Potier, M. Process for Isolation and Purification of Paclitaxel from Natural Sources. U.S. Patent No 6,759,539, 6 July 2004. Available online: https://patentimages.storage.googleapis.com/44/e6/98/decc6a00219616/us6759539.pdf (accessed on 22 January 2020).
- Sadeghi-aliabadi, H.; Asghari, G.; Mostafavi, S.A.; Esmaeili, A. Solvent optimization on Taxol extraction from Taxus baccata L., using HPLC and LC-MS. Daru 2009, 17, 192–198. [Google Scholar]
- Kim, G.J.; Kim, J.H. Enhancement of extraction efficiency of paclitaxel from biomass using ionic liquid-methanol co-solvents under acidic conditions. Process Biochem. 2015, 50, 989–996. [Google Scholar] [CrossRef]
- Kawamura, F.; Kikuchi, Y.; Ohira, T.; Yatagai, M. Accelerated solvent extraction of paclitaxel and related compounds from the bark of Taxus cuspidata. J. Nat. Prod. 1999, 62, 244–247. [Google Scholar] [CrossRef]
- Lee, S.H.; Kim, J.H. Kinetic and thermodynamic characteristics of microwave-assisted extraction for the recovery of paclitaxel from Taxus chinensis. Process Biochem. 2019, 76, 187–193. [Google Scholar] [CrossRef]
- Naik, B.S. Developments in taxol production through endophytic fungal biotechnology: A review. Orient. Pharm. Exp. Med. 2019, 19, 1–13. [Google Scholar] [CrossRef]
- El-Sayed, E.R.; Zaki, A.G.; Ahmed, A.S.; Ismaiel, A.A. Production of the anticancer drug taxol by the endophytic fungus Epicoccum nigrum TXB502: Enhanced production by gamma irradiation mutagenesis and immobilization technique. Appl. Microbiol. Biotechnol. 2020, 104, 6991–7003. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Singh, B.; Thakur, V.; Thakur, A.; Thakur, N.; Pandey, D.; Chanda, D. Hyper-production of taxol from Aspergillus fumigatus, an endophytic fungus isolated from Taxus sp. of the Northern Himalayan region. Biotechnol. Rep. (Amst.) 2019, 24, e00395. [Google Scholar] [CrossRef]
- Badi, H.N.; Abdoosi, V.; Farzin, N. New approach to improve taxol biosynthetic. Trakia J. Sci. 2015, 2, 115–124. [Google Scholar] [CrossRef]
- Subban, K.; Subramani, R.; Srinivasan, V.P.M.; Johnpaul, M.; Chelliah, J. Salicylic acid as an effective elicitor for improved taxol production in endophytic fungus Pestalotiopsis microspora. PLoS ONE 2019, 14, e0212736. [Google Scholar] [CrossRef]
- Sabzehzari, M.; Zeinali, M.; Naghavia, M.R. Alternative sources and metabolic engineering of Taxol: Advances and future perspectives. Biotech. Adv. 2020, 43, 107569. [Google Scholar] [CrossRef]
- Chakravarthi, B.V.S.K.; Singh, S.; Kamalraj, S.; Gupta, V.K.; Jayabaskaran, C. Evaluation of spore inoculum and confirmation of pathway genetic blueprint of T13αH and DBAT from a Taxol-producing endophytic fungus. Sci. Rep. 2020, 10, 21139. [Google Scholar] [CrossRef]
- Page, M.; Landry, N.; Boissinot, M.; Helie, M.C.; Harvey, M.; Gagne, M. Bacterial Mass Production of Taxanes and Paclitaxel. U.S. Patent No 6,030,818, 29 February 2000. Available online: https://patentimages.storage.googleapis.com/57/34/8c/542334a3e376bd/US6030818.pdf (accessed on 22 January 2021).
- Bacterial Mass Production of Taxanes with Erwinia. Available online: https://patentimages.storage.googleapis.com/a5/51/6d/3488bf95fd1bf5/US5561055.pdf (accessed on 22 January 2021).
- Ajikumar, P.K.; Xiao, W.H.; Tyo, K.E.J.; Wang, Y.; Simeon, F.; Leonard, E.; Mucha, O.; Phon, T.H.; Pfeifer, B.; Stephanopoulos, G. Isoprenoid pathway optimization for Taxol precursor over-production in Escherichia coli. Science 2010, 330, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Zhou, K.; Qiao, K.; Edgar, S.; Stephanopoulos, G. Distributing a metabolic pathway among a microbial consortium enhances production of natural products. Nat. Biotechnol. 2015, 33, 377–383. [Google Scholar] [CrossRef]
- Subramanian, M.; Marudhamuthu, M. Hitherto Unknown terpene synthase organization in taxol producing endophytic bacteria isolated from marine macroalgae. Curr. Microbiol. 2020, 77, 918–923. [Google Scholar] [CrossRef] [PubMed]
- Patil, R.A.; Kolewe, M.E.; Normanly, J.; Walker, E.L.; Roberts, S.C. Contribution of taxane biosynthetic pathway gene expression to observed variability in paclitaxel accumulation in Taxus suspension cultures. Biotechnol J. 2012, 7, 418–427. [Google Scholar] [CrossRef]
- Gallego, A.; Malik, S.; Yousefzadi, M.; Makhzoum, A.; Tremouillaux-Guiller, J.; Bonfill, M. Taxol from Corylus avellana: Paving the way for a new source of this anti-cancer drug. Plant Cell Tissue Organ Cult. 2017, 129, 1–16. [Google Scholar] [CrossRef]
- Qaderi, A.; Omidi, M.; Omidi, M.; Etminan, A.; Etminan, A.; Oladzad, A.; Ebrahimi, C.; Dehghani, M.; Mehrafarin, A. Hazel (Corylus avellana L.) as a new source of taxol and taxanes. J. Med. Plants 2012, 11, 66–67. [Google Scholar]
- Salehi, M.; Moieni, A.; Safaie, N.; Farhadi, S. Whole fungal elicitors boost paclitaxel biosynthesis induction in Corylus avellana cell culture. PLoS ONE 2020, 15, e0236191. [Google Scholar] [CrossRef]
- McElroy, C.; Jennewein, S. Taxol® Biosynthesis and production: From forests to fermenters. In Biotechnology of Natural Products; Schwab, W., Lange, B.M., Wüst, M., Eds.; Springer: Cham, Switzerland, 2018; pp. 145–185. ISBN 978-3-319-67903-7. [Google Scholar] [CrossRef]
- Edgar, S.; Li, F.S.; Qiao, K.; Weng, J.K.; Stephanopoulos, G. Engineering of taxadiene synthase for improved selectivity and yield of a key taxol biosynthetic intermediate. ACS Synth. Biol. 2017, 6, 201–205. [Google Scholar] [CrossRef]
- Danishefsky, S.J.; Masters, J.J.; Young, W.B.; Link, J.T.; Snyder, L.B.; Magee, T.V.; Jung, D.K.; Isaacs, R.C.A.; Bornmann, W.G.; Alaimo, C.A.; et al. Total synthesis of baccatin III and taxol. J. Am. Chem. Soc. 1996, 118, 2843–2859. [Google Scholar] [CrossRef]
- Doi, T.; Fuse, S.; Miyamoto, S.; Nakai, K.; Sasuga, D.; Takahashi, T. A formal total synthesis of taxol aided by an automated synthesizer. Chem. Asian J. 2006, 1, 370–383. [Google Scholar] [CrossRef] [PubMed]
- Fukaya, K.; Kodama, K.; Tanaka, Y.; Yamazaki, H.; Sugai, T.; Yamaguchi, Y.; Watanabe, A.; Oishi, T.; Sato, T.; Chida, N. Synthesis of paclitaxel. 2. Construction of the ABCD ring and formal synthesis. Org. Lett. 2015, 17, 2574–2577. [Google Scholar] [CrossRef] [PubMed]
- Fukaya, K.; Tanaka, Y.; Sato, A.C.; Kodama, K.; Yamazaki, H.; Ishimoto, T.; Nozaki, Y.; Iwaki, Y.M.; Yuki, Y.; Umei, K.; et al. Synthesis of paclitaxel. 1. Synthesis of the ABC ring of paclitaxel by SmI2-mediated cyclization. Org. Lett. 2015, 17, 2570–2573. [Google Scholar] [CrossRef]
- Hirai, S.; Utsugi, M.; Iwamoto, M.; Nakada, M. Formal total synthesis of (−)-taxol through Pd-catalyzed eight-membered carbocyclic ring formation. Chem. Eur. J. 2015, 21, 355–359. [Google Scholar] [CrossRef]
- Holton, R.A.; Somoza, C.; Kim, H.B.; Liang, F.; Biediger, R.J.; Boatman, P.D.; Shindo, M.; Smith, C.C.; Kim, S.; Nadizadeh, H.; et al. First total synthesis of taxol. 1. Functionalization of the B-ring. J. Am. Chem. Soc. 1994, 116, 1597–1598. [Google Scholar] [CrossRef]
- Masters, J.J.; Link, J.T.; Snyder, L.B.; Young, W.B.; Danishefsky, S.J. A total synthesis of taxol. Angew. Chem. Int. Ed. 1995, 34, 1723–1726. [Google Scholar] [CrossRef]
- Morihira, K.; Hara, R.; Kawahara, S.; Nishimori, T.; Nakamura, N.; Kusama, H.; Kuwajima, I. Enantioselective total synthesis of taxol. J. Am. Chem. Soc. 1998, 120, 12980–12981. [Google Scholar] [CrossRef]
- Mukaiyama, T.; Shiina, I.; Iwadare, H.; Saitoh, M.; Nishimura, T.; Ohkawa, N.; Sakoh, H.; Nishimura, K.; Tani, Y.I.; Hasegawa, M.; et al. Asymmetric total synthesis of taxol\R. Chem. Eur. J. 1999, 5, 121–161. [Google Scholar] [CrossRef]
- Nicolaou, K.C.; Yang, Z.; Liu, J.J.; Ueno, H.; Nantermet, P.G.; Guy, R.K.; Claiborne, C.F.; Renaud, J.; Couladouros, E.A.; Paulvannan, K.; et al. Total synthesis of taxol. Nature 1994, 367, 630–634. [Google Scholar] [CrossRef] [PubMed]
- Wender, P.A.; Badham, N.F.; Conway, S.P.; Floreancig, P.E.; Glass, T.E.; Gränicher, C.; Houze, J.B.; Jänichen, J.; Lee, D.; Marquess, D.G.; et al. The pinene path to taxanes. 5. Stereocontrolled synthesis of a versatile taxane precursor. J. Am. Chem. Soc. 1997, 119, 2755–2756. [Google Scholar] [CrossRef]
- Wender, P.A.; Badham, N.F.; Conway, S.P.; Floreancig, P.E.; Glass, T.E.; Houze, J.B.; Krauss, N.E.; Lee, D.; Marquess, D.G.; McGrane, P.L.; et al. The pinene path to taxanes. 6. A concise stereocontrolled synthesis of taxol. J. Am. Chem. Soc. 1997, 119, 2757–2758. [Google Scholar] [CrossRef]
- Kanda, Y.; Nakamura, H.; Umemiya, S.; Puthukanoori, R.K.; Appala, V.R.M.; Gaddamanugu, G.K.; Paraselli, B.R.; Baran, P.S. Two-phase synthesis of taxol. J. Am. Chem. Soc. 2020, 142, 10526–10533. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, F.Y.; Aleanizy, F.S.; El Tahir, E.; Alkahtani, H.M.; AlQuadeib, B.T. Chapter three—Paclitaxel. In Profiles of Drug Substances, Excipients and Related Methodology; Brittain, H.G., Ed.; Academic Press: Cambridge, MA, USA, 2019; Volume 44, pp. 205–238. ISBN 9780128171660. [Google Scholar] [CrossRef]
- Patel, R.N. Tour de paclitaxel: Biocatalysis for semisynthesis. Annu. Rev. Microbiol. 1998, 52, 361–395. [Google Scholar] [CrossRef]
- Witherup, K.M.; Look, S.A.; Stasko, M.W.; Ghiorzi, T.J.; Muschik, G.M.; Cragg, G.M. Taxus spp. needles contain amounts of taxol comparable to the bark of Taxus brevifolia: Analysis and isolation. J. Nat. Prod. 1990, 53, 1249–1255. [Google Scholar] [CrossRef]
- Schiff, P.B.; Fant, J.; Horwitz, S.B. Promotion of microtubule assembly in vitro by taxol. Nature 1979, 277, 665–667. [Google Scholar] [CrossRef]
- Parness, J.; Horwitz, S.B. Taxol binds to polymerized tubulin in vitro. J. Cell Biol. 1981, 91, 479–487. [Google Scholar] [CrossRef]
- Rao, S.; He, L.; Chakravarty, S.; Ojima, I.; Orr, G.A.; Horwitz, S.B. Characterization of the taxol binding site on the microtubule. Identification of Arg(282) in beta-tubulin as the site of photoincorporation of a 7-benzophenone analogue of Taxol. J. Biol. Chem. 1999, 274, 37990–37994. [Google Scholar] [CrossRef]
- Díaz, J.F.; Andreu, J.M. Assembly of purified GDP-tubulin into microtubules induced by taxol and taxotere: Reversibility, ligand stoichiometry, and competition. Biochemistry 1993, 32, 2747–2755. [Google Scholar] [CrossRef]
- Waters, J.C.; Chen, R.H.; Murray, A.W.; Salmon, E.D. Localization of Mad2 to kinetochores depends on microtubule attachment, not tension. J. Cell Biol. 1998, 141, 1181–1191. [Google Scholar] [CrossRef]
- Boudny, V.; Nakano, S. Src tyrosine kinase augments taxotere-induced apoptosis through enhanced expression and phosphorylation of Bcl-2. Br. J. Cancer 2002, 86, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Héliez, C.; Baricault, L.; Barboule, N.; Valette, A. Paclitaxel increases p21 synthesis and accumulation of its AKT-phosphorylated form in the cytoplasm of cancer cells. Oncogene 2003, 22, 3260–3268. [Google Scholar] [CrossRef] [PubMed]
- Tanimukai, H.; Kanayama, D.; Omi, T.; Takeda, M.; Kudo, T. Paclitaxel induces neurotoxicity through endoplasmic reticulum stress. Biochem. Biophys. Res. Commun. 2013, 437, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Risinger, A.L.; Riffle, S.M.; Lopus, M.; Jordan, M.A.; Wilson, L.; Mooberry, S.L. The taccalonolides and paclitaxel cause distinct effects on microtubule dynamics and aster formation. Mol. Cancer 2014, 13, 41. [Google Scholar] [CrossRef]
- Verde, F.; Berrez, J.M.; Antony, C.; Karsenti, E. Taxol-induced microtubule asters in mitotic extracts of Xenopus eggs: Requirement for phosphorylated factors and cytoplasmic dynein. J. Cell Biol. 1991, 112, 1177–1187. [Google Scholar] [CrossRef]
- Öztop, S.; Işik, A.; Güner, G.; Gürdal, H.; Karabulut, E.; Yilmaz, E.; Akyol, A. Class III beta-tubulin expression in colorectal neoplasms is a potential predictive biomarker for paclitaxel response. Anticancer Res. 2019, 39, 655–662. [Google Scholar] [CrossRef]
- Tame, M.A.; Manjón, A.G.; Belokhvostova, D.; Raaijmakers, J.A.; Medema, R.H. TUBB3 overexpression has a negligible effect on the sensitivity to taxol in cultured cell lines. Oncotarget 2017, 8, 71536–71547. [Google Scholar] [CrossRef] [PubMed]
- Gelderblom, H.; Verweij, J.; Nooter, K.; Sparreboom, A. Cremophor EL: The drawbacks and advantages of vehicle selection for drug formulation. Eur. J. Cancer 2001, 37, 1590–1598. [Google Scholar] [CrossRef]
- Mei, L.; Zhang, Y.; Zheng, Y.; Tian, G.; Song, C.; Yang, D.; Chen, H.; Sun, H.; Tian, Y.; Liu, K.; et al. A novel docetaxel-loaded poly (ε-caprolactone)/pluronic F68 nanoparticle overcoming multidrug resistance for breast cancer treatment. Nanoscale Res. Lett. 2009, 4, 1530–1539. [Google Scholar] [CrossRef] [PubMed]
- Yuan, H.; Guo, H.; Luan, X.; He, M.; Li, F.; Burnett, J.; Truchan, N.; Sun, D. Albumin nanoparticle of paclitaxel (abraxane) decreases while taxol increases breast cancer stem cells in treatment of triple negative breast cancer. Mol. Pharm. 2020, 17, 2275–2286. [Google Scholar] [CrossRef]
- Wang, X.; Song, L.; Li, N.; Qiu, Z.; Zhou, S.; Li, C.; Zhao, J.; Song, H.; Chen, X. Pharmacokinetics and biodistribution study of paclitaxel liposome in Sprague-Dawley rats and Beagle dogs by liquid chromatography-tandem mass spectrometry. Drug Res. 2013, 63, 603–606. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Huang, X.E.; Gao, L.L. A clinical study on the premedication of paclitaxel liposome in the treatment of solid tumors. Biomed. Pharmacother. 2009, 63, 603–607. [Google Scholar] [CrossRef]
- Orphan drug designation to LEP-ETU for ovarian cancer. Oncol. Times 2015, 37, 25. [CrossRef]
- Zhang, J.A.; Anyarambhatla, G.; Ma, L.; Ugwu, S.; Xuan, T.; Sardone, T.; Ahmad, I. Development and characterization of a novel Cremophor EL free liposome-based paclitaxel (LEP-ETU) formulation. Eur. J. Pharm. Biopharm. 2005, 59, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Fasol, U.; Frost, A.; Büchert, M.; Arends, J.; Fiedler, U.; Scharr, D.; Scheuenpflug, J.; Mross, K. Vascular and pharmacokinetic effects of EndoTAG-1 in patients with advanced cancer and liver metastasis. Ann. Oncol. 2012, 23, 1030–1036. [Google Scholar] [CrossRef] [PubMed]
- ClinicalTrials.gov. Available online: https://www.clinicaltrials.gov/ct2/results?cond=&term=lipusu&cntry=&state=&city=&dist=&Search=Search (accessed on 22 January 2021).
- ClinicalTrials.gov. Available online: https://www.clinicaltrials.gov/ct2/results?cond=&term=LEP-ETU&cntry=&state=&city=&dist=&Search=Search (accessed on 22 January 2021).
- ClinicalTrials.gov. Available online: https://www.clinicaltrials.gov/ct2/results?cond=&term=endotag&cntry=&state=&city=&dist=&Search=Search (accessed on 22 January 2021).
- ClinicalTrials.gov. Available online: https://www.clinicaltrials.gov/ct2/results?cond=&term=PTX-LDE&cntry=&state=&city=&dist=&Search=Search (accessed on 22 January 2021).
- ClinicalTrials.gov. Available online: https://www.clinicaltrials.gov/ct2/results?cond=&term=LE-DT&cntry=&state=&city=&dist=&Search=Search (accessed on 22 January 2021).
- ClinicalTrials.gov. Available online: https://www.clinicaltrials.gov/ct2/results?cond=&term=ATI-1123+&cntry=&state=&city=&dist=&Search=Search (accessed on 22 January 2021).
- ClinicalTrials.gov. Available online: https://www.clinicaltrials.gov/ct2/results?cond=&term=genexol-PM&cntry=&state=&city=&dist=&Search=Search (accessed on 22 January 2021).
- ClinicalTrials.gov. Available online: https://www.clinicaltrials.gov/ct2/results?cond=&term=NAnoxel&cntry=&state=&city=&dist=&Search=Search (accessed on 22 January 2021).
- ClinicalTrials.gov. Available online: https://www.clinicaltrials.gov/ct2/results?cond=&term=paclical&cntry=&state=&city=&dist=&Search=Search (accessed on 22 January 2021).
- Deeken, J.F.; Slack, R.; Weiss, G.J.; Ramanathan, R.K.; Pishvaian, M.J.; Hwang, J.; Lewandowski, K.; Subramaniam, D.; He, A.R.; Cotarla, I.; et al. A phase I study of liposomal-encapsulated docetaxel (LE-DT) in patients with advanced solid tumor malignancies. Cancer Chemother. Pharmacol. 2013, 71, 627–633. [Google Scholar] [CrossRef]
- Mahalingam, D.; Nemunaitis, J.J.; Malik, L.; Sarantopoulos, J.; Weitman, S.; Sankhala, K.; Hart, J.; Kousba, A.; Gallegos, N.S.; Anderson, G.; et al. Phase I study of intravenously administered ATI-1123, a liposomal docetaxel formulation in patients with advanced solid tumors. Cancer Chemother. Pharmacol. 2014, 74, 1241–1250. [Google Scholar] [CrossRef]
- Merrimack Discontinues Development of MM-310. Available online: https://investors.merrimack.com/news-releases/news-release-details/merrimack-discontinues-development-mm-310 (accessed on 22 January 2021).
- Trial to Study the Safety of Intravenous MNK-010 in Advanced Solid Tumors. Available online: https://clinicaltrials.gov/ct2/show/NCT02040558 (accessed on 22 January 2021).
- Zhang, M.; Li, M.; Du, L.; Zeng, J.; Yao, T.; Jin, Y. Paclitaxel-in-liposome-in-bacteria for inhalation treatment of primary lung cancer. Int. J. Pharm. 2020, 578, 119177. [Google Scholar] [CrossRef] [PubMed]
- Do, V.Q.; Park, K.H.; Park, J.M.; Lee, M.Y. Comparative in vitro toxicity study of docetaxel and nanoxel, a docetaxel-loaded micellar formulation using cultured and blood cells. Toxicol. Res. 2019, 35, 201–207. [Google Scholar] [CrossRef]
- Borga, O.; Lilienberg, E.; Bjermo, H.; Hansson, F.; Heldring, N.; Dediu, R. Pharmacokinetics of total and unbound paclitaxel after administration of paclitaxel micellar or nab-paclitaxel: An open, randomized, cross-over, explorative study in breast cancer patients. Adv. Ther. 2019, 36, 2825–2837. [Google Scholar] [CrossRef]
- Van Tomme, S.R.; Storm, G.; Hennink, W.E. In situ gelling hydrogels for pharmaceutical and biomedical applications. Int. J. Pharm. 2008, 355, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Ruel-Gariépy, E.; Shive, M.; Bichara, A.; Berrada, M.; Le Garrec, D.; Chenite, A.; Leroux, J.C. A thermosensitive chitosan-based hydrogel for the local delivery of paclitaxel. Eur. J. Pharm. Biopharm. 2004, 57, 53–63. [Google Scholar] [CrossRef]
- Li, C.; Ren, S.; Dai, Y.; Tian, F.; Wang, X.; Zhou, S.; Deng, S.; Liu, Q.; Zhao, J.; Chen, X. Efficacy, pharmacokinetics, and biodistribution of thermosensitive chitosan/β -glycerophosphate hydrogel loaded with docetaxel. AAPS PharmSciTech 2014, 15, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Bajaj, G.; Kim, M.R.; Mohammed, S.I.; Yeo, Y. Hyaluronic acid-based hydrogel for regional delivery of paclitaxel to intraperitoneal tumors. J. Control. Release 2012, 158, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Mao, Y.; Li, X.; Chen, G.; Wang, S. Thermosensitive hydrogel system with paclitaxel liposomes used in localized drug delivery system for in situ treatment of tumor: Better antitumor efficacy and lower toxicity. J. Pharm. Sci. 2016, 105, 194–204. [Google Scholar] [CrossRef]
- Ma, P.; Mumper, R.J. Paclitaxel nano-delivery systems: A comprehensive review. J. Nanomed. Nanotechnol. 2013, 4, 1000164. [Google Scholar] [CrossRef]
- Godara, S.; Lather, V.; Kirthanashri, S.V.; Awasthi, R.; Pandita, D. Lipid-PLGA hybrid nanoparticles of paclitaxel: Preparation, characterization, in vitro and in vivo evaluation. Mater. Sci. Eng. 2020, 109, 110576. [Google Scholar] [CrossRef]
- Houdaihed, L.; Evans, J.C.; Allen, C. Dual-targeted delivery of nanoparticles encapsulating paclitaxel and everolimus: A novel strategy to overcome breast cancer receptor heterogeneity. Pharm. Res. 2020, 37, 39. [Google Scholar] [CrossRef]
- Tang, H.; Chen, J.; Wang, L.; Li, Q.; Yang, Y.; Lv, Z.; Bao, H.; Li, Y.; Luan, X.; Li, Y.; et al. Co-delivery of epirubicin and paclitaxel using an estrone-targeted PEGylated liposomal nanoparticle for breast cancer. Int. J. Pharm. 2020, 573, 118806. [Google Scholar] [CrossRef] [PubMed]
- Duan, T.; Xu, Z.; Sun, F.; Wang, Y.; Zhang, J.; Luo, C.; Wang, M. HPA aptamer functionalized paclitaxel-loaded PLGA nanoparticles for enhanced anticancer therapy through targeted effects and microenvironment modulation. Biomed. Pharmacother. 2019, 117, 109121. [Google Scholar] [CrossRef] [PubMed]
- Cao, X.; Tan, T.; Zhu, D.; Yu, H.; Liu, Y.; Zhou, H.; Jin, Y.; Xia, Q. Paclitaxel-loaded macrophage membrane camouflaged albumin nanoparticles for targeted cancer therapy. Int. J. Nanomed. 2020, 15, 1915–1928. [Google Scholar] [CrossRef]
- Fang, W.S.; Liang, X.T. Recent progress in structure activity relationship and mechanistic studies of taxol analogues. Mini. Rev. Med. Chem. 2005, 5, 1–12. [Google Scholar] [CrossRef]
- Safavy, A.; Raisch, K.P.; Khazaeli, M.B.; Buchsbaum, D.J.; Bonner, J.A. Paclitaxel derivatives for targeted therapy of cancer: Toward the development of smart taxanes. J. Med. Chem. 1999, 42, 4919–4924. [Google Scholar] [CrossRef] [PubMed]
- Ndungu, J.M.; Lu, Y.J.; Zhu, S.; Yang, C.; Wang, X.; Chen, G.; Shin, D.M.; Snyder, J.P.; Shoji, M.; Sun, A. Targeted delivery of paclitaxel to tumor cells: Synthesis and in vitro evaluation. J. Med. Chem. 2010, 53, 3127–3132. [Google Scholar] [CrossRef] [PubMed]
- Ojima, I.; Zuniga, E.S.; Berger, W.T.; Seitz, J.D. Tumor-targeting drug delivery of new-generation taxoids. Future Med. Chem. 2012, 4, 33–50. [Google Scholar] [CrossRef] [PubMed]
- Ojima, I.; Wang, X.; Jing, Y.; Wang, C. Quest for efficacious next-generation taxoid anticancer agents and their tumor-targeted delivery. J. Nat. Prod. 2018, 81, 703–721. [Google Scholar] [CrossRef] [PubMed]
- Vineberg, J.G.; Wang, T.; Zuniga, E.S.; Ojima, I. Design, synthesis, and biological evaluation of theranostic vitamin-linker-taxoid conjugates. J. Med. Chem. 2015, 58, 2406–2416. [Google Scholar] [CrossRef] [PubMed]
- Ojima, I.; Geng, X.; Wu, X.; Qu, C.; Borella, C.P.; Xie, H.; Wilhelm, S.D.; Leece, B.A.; Bartle, L.M.; Goldmacher, V.S.; et al. Tumor-specific novel taxoid-monoclonal antibody conjugates. J. Med. Chem. 2002, 45, 5620–5623. [Google Scholar] [CrossRef] [PubMed]
- ClinicalTrials.gov. Available online: https://www.clinicaltrials.gov/ct2/results?cond=&term=oraxol&cntry=&state=&city=&dist= (accessed on 22 January 2021).
- Lee, K.W.; Lee, K.H.; Zang, D.Y.; Park, Y.I.; Shin, D.B.; Kim, J.W.; Im, S.A.; Koh, S.A.; Yu, K.S.; Cho, J.Y.; et al. Phase I/II study of weekly oraxol for the second-line treatment of patients with metastatic or recurrent gastric cancer. Oncologist 2015, 20, 896–897. [Google Scholar] [CrossRef]
- Ferlini, C.; Cicchillitti, L.; Raspaglio, G.; Bartollino, S.; Cimitan, S.; Bertucci, C.; Mozzetti, S.; Gallo, D.; Persico, M.; Fattorusso, C.; et al. Paclitaxel directly binds to Bcl-2 and functionally mimics activity of Nur77. Cancer Res. 2009, 69, 6906–6914. [Google Scholar] [CrossRef]
- Wang, X.; Liow, S.S.; Wu, Q.; Li, C.; Owh, C.; Li, Z.; Loh, X.J.; Wu, Y.L. Codelivery for paclitaxel and Bcl-2 conversion gene by PHB-PDMAEMA amphiphilic cationic copolymer for effective drug resistant cancer therapy. Macromol. Biosci. 2017, 17, 1700186. [Google Scholar] [CrossRef]
- Whitaker, R.H.; Placzek, W.J. Regulating the BCL2 family to improve sensitivity to microtubule targeting agents. Cells 2019, 8, 346. [Google Scholar] [CrossRef] [PubMed]
- Pires, M.M.; Emmert, D.; Hrycyna, C.A.; Chmielewski, J. Inhibition of P-glycoprotein-mediated paclitaxel resistance by reversibly linked quinine homodimers. Mol. Pharmacol. 2009, 75, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, P.S.; Beg, S.; Mehta, F.; Singh, B.; Trivedi, P. Novel dietary lipid-based self-nanoemulsifying drug delivery systems of paclitaxel with P-gp inhibitor: Implications on cytotoxicity and biopharmaceutical performance. Expert Opin. Drug Deliv. 2015, 12, 1809–1822. [Google Scholar] [CrossRef]
- Wang, F.; Zhang, D.; Zhang, Q.; Chen, Y.; Zheng, D.; Hao, L.; Duan, C.; Jia, L.; Liu, G.; Liu, Y. Synergistic effect of folate-mediated targeting and verapamil-mediated P-gp inhibition with paclitaxel -polymer micelles to overcome multi-drug resistance. Biomaterials 2011, 32, 9444–9456. [Google Scholar] [CrossRef]
- Zhong, J.; Guo, Z.; Fan, L.; Zhao, X.; Zhao, B.; Cao, Z.; Cheng, L.; Shi, Y.; Li, X.; Zhang, Y.; et al. ABCB1 polymorphism predicts the toxicity and clinical outcome of lung cancer patients with taxane-based chemotherapy. Thorac. Cancer 2019, 10, 2088–2095. [Google Scholar] [CrossRef] [PubMed]
- Muley, H.; Fadó, R.; Rodríguez-Rodríguez, R.; Casals, N. Drug uptake-based chemoresistance in breast cancer treatment. Biochem. Pharmacol. 2020, 177, 113959. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.L.; Xu, P.F.; Miao, C.; Fu, Z.Y.; Li, Q.P.; Tang, P.Y.; Wang, T. Hypoxia decreased chemosensitivity of breast cancer cell line MCF-7 to paclitaxel through cyclin B1. Biomed. Pharmacother. 2012, 66, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Ricker, J.L.; Chen, Z.; Yang, X.P.; Pribluda, V.S.; Swartz, G.M.; Van Waes, C. 2-Methoxyestradiol inhibits hypoxia-inducible factor 1α, tumor growth, and angiogenesis and augments paclitaxel efficacy in head and neck squamous cell carcinoma. Clin. Cancer Res. 2004, 10, 8665–8673. [Google Scholar] [CrossRef]
- Zeng, L.; Kizaka-Kondoh, S.; Itasaka, S.; Xie, X.; Inoue, M.; Tanimoto, K.; Shibuya, K.; Hiraoka, M. Hypoxia inducible factor-1 influences sensitivity to paclitaxel of human lung cancer cell lines under normoxic conditions. Cancer Sci. 2007, 98, 1394–1401. [Google Scholar] [CrossRef]
- Chen, D.; Bao, C.; Zhao, F.; Yu, H.; Zhong, G.; Xu, L.; Yan, S. Exploring specific miRNA-mRNA axes with relationship to taxanes-resistance in breast cancer. Front. Oncol. 2020, 10, 1397. [Google Scholar] [CrossRef] [PubMed]
- Bomane, A.; Gonçalves, A.; Ballester, P.J. Paclitaxel response can be predicted with interpretable multi-variate classifiers exploiting DNA-methylation and miRNA data. Front. Genet. 2019, 10, 1041. [Google Scholar] [CrossRef]
- Liskova, A.; Samec, M.; Koklesova, L.; Giordano, F.A.; Kubatka, P.; Golubnitschaja, O. Liquid biopsy is instrumental for 3PM dimensional solutions in cancer management. J. Clin. Med. 2020, 9, 2749. [Google Scholar] [CrossRef] [PubMed]
- Farrar, M.C.; Jacobs, T.F. Paclitaxel. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2020. [Google Scholar]
- ClinicalTrials.gov. Available online: https://www.clinicaltrials.gov/ct2/results?cond=Cancer+&term=carboplatin+paclitaxel&cntry=&state=&city=&dist=&Search=Search&recrs=a&recrs=b&recrs=d&recrs=f (accessed on 22 January 2021).
- Safra, T.; Waissengrin, B.; Levy, T.; Leidner, E.; Merose, R.; Matceyevsky, D.; Grisaru, D.; Laskov, I.; Mishaan, N.; Shayzaf, R.; et al. Weekly carboplatin and paclitaxel: A retrospective comparison with the three-weekly schedule in first-line treatment of ovarian cancer. Oncologist 2021, 26, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Cohen, M.H.; Gootenberg, J.; Keegan, P.; Pazdur, R. FDA drug approval summary: Bevacizumab (Avastin) plus carboplatin and paclitaxel as first-line treatment of advanced/metastatic recurrent nonsquamous non-small cell lung cancer. Oncologist 2007, 12, 713–718. [Google Scholar] [CrossRef] [PubMed]
- Secord, A.A.; Burdett, K.B.; Owzar, K.; Tritchler, D.; Sibley, A.B.; Liu, Y.; Starr, M.D.; Brady, J.C.; Lankes, H.A.; Hurwitz, H.I.; et al. Predictive blood-based biomarkers in patients with epithelial ovarian cancer treated with carboplatin and paclitaxel with or without bevacizumab: Results from GOG-0218. Clin. Cancer Res. 2020, 26, 1288–1296. [Google Scholar] [CrossRef]
- Battaglia, A.; Buzzonetti, A.; Fossati, M.; Scambia, G.; Fattorossi, A.; Madiyalakan, M.R.; Mahnke, Y.D.; Nicodemus, C. Translational immune correlates of indirect antibody immunization in a randomized phase II study using scheduled combination therapy with carboplatin/paclitaxel plus oregovomab in ovarian cancer patients. Cancer Immunol. Immunother. 2020, 69, 383–397. [Google Scholar] [CrossRef] [PubMed]
- Cejalvo, J.M.; Jacob, W.; Kanonnikoff, T.F.; Felip, E.; Mendivil, A.N.; Garcia, M.M.; Garcia, A.T.; Leighl, N.; Lassen, U.; Mau-Soerensen, M.; et al. A phase Ib/II study of HER3-targeting lumretuzumab in combination with carboplatin and paclitaxel as first-line treatment in patients with advanced or metastatic squamous non-small cell lung cancer. ESMO Open 2019, 4, e000532. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.J.; Atkinson, E.C.; Leichman, L.P.; Patel, H.; Iqbal, S.; Du, K.L.; Bizekis, C.; Goldberg, J.D.; Thomas, C.R.; Cohen, D.J.; et al. A phase I/II multisite study of nivolumab and carboplatin/paclitaxel with radiation therapy (RT) in patients with locally advanced esophageal squamous cell carcinoma (ESCC). J. Clin. Oncol. 2020, 38, 372. [Google Scholar] [CrossRef]
- Goldman, J.W.; Waterhouse, D.M.; George, B.; O’Dwyer, P.J.; Bhore, R.; Banerjee, S.; Lyons, L.; Louis, C.U.; Ong, T.J.; Kelly, K. Safety and efficacy results of a phase I, open-label study of concurrent and delayed nivolumab in combination with nab-paclitaxel and carboplatin in advanced non-small cell lung cancer. Front. Oncol. 2019, 9, 1256. [Google Scholar] [CrossRef]
- Jotte, R.; Cappuzzo, F.; Vynnychenko, I.; Stroyakovskiy, D.; Rodríguez-Abreu, D.; Hussein, M.; Soo, R.; Conter, H.J.; Kozuki, T.; Huang, K.C.; et al. Atezolizumab in combination with carboplatin and nab-paclitaxel in advanced squamous NSCLC: Results from a randomized phase III trial. J. Thorac. Oncol. 2020, 15, 1351–1360. [Google Scholar] [CrossRef]
- Lopresti, M.L.; Bian, J.J.; Sakr, B.J.; Strenger, R.S.; Legare, R.D.; Fenton, M.A.; Witherby, S.M.; Dizon, D.S.; Pandya, S.V.; Stuckey, A.R.; et al. Neoadjuvant weekly paclitaxel (wP) and carboplatin (Cb) with trastuzumab (T) and pertuzumab (P) in HER2-positive breast cancer (H+BC): A Brown University oncology group (BrUOG) study. Cancer Res. 2020, 80. [Google Scholar] [CrossRef]
- Shirasu, H.; Yokota, T.; Kawakami, T.; Hamauchi, S.; Onozawa, Y.; Ogawa, H.; Onoe, T.; Mori, K.; Onitsuka, T. Efficacy and feasibility of induction chemotherapy with paclitaxel, carboplatin and cetuximab for locally advanced unresectable head and neck cancer patients ineligible for combination treatment with docetaxel, cisplatin, and 5-fluorouracil. Int. J. Clin. Oncol. 2020, 25, 1914–1920. [Google Scholar] [CrossRef]
- Villaruz, L.C.; Cobo, M.; Syrigos, K.; Mavroudis, D.; Zhang, W.; Kim, J.S.; Socinski, M.A. A phase II study of nab-paclitaxel and carboplatin chemotherapy plus necitumumab in the first-line treatment of patients with stage IV squamous non-small cell lung cancer. Lung Cancer 2019, 136, 52–56. [Google Scholar] [CrossRef] [PubMed]
- ClinicalTrials.gov. Available online: https://www.clinicaltrials.gov/ct2/home (accessed on 22 January 2021).
- ClinicalTrials.gov. Available online: https://www.clinicaltrials.gov/ct2/results?cond=&term=monoclonal+antibody+AND+paclitaxel&cntry=&state=&city=&dist= (accessed on 22 January 2021).
- ClinicalTrials.gov. Available online: https://www.clinicaltrials.gov/ct2/results?cond=&term=monoclonal+antibody+AND+docetaxel&cntry=&state=&city=&dist=&Search=Search (accessed on 22 January 2021).
- Casak, S.J.; Fashoyin-Aje, I.; Lemery, S.J.; Zhang, L.; Jin, R.; Li, H.; Zhao, L.; Zhao, H.; Zhang, H.; Chen, H.; et al. FDA approval summary: Ramucirumab for gastric cancer. Clin. Cancer Res. 2015, 21, 3372–3376. [Google Scholar] [CrossRef] [PubMed]
- Wilke, H.; Muro, K.; Van Cutsem, E.; Oh, S.C.; Bodoky, G.; Shimada, Y.; Hironaka, S.; Sugimoto, N.; Lipatov, O.; Kim, T.Y.; et al. Ramucirumab plus paclitaxel versus placebo plus paclitaxel in patients with previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (RAINBOW): A double-blind, randomised phase 3 trial. Lancet Oncol. 2014, 15, 1224–1235. [Google Scholar] [CrossRef]
- Rakusic, Z.; Krpan, A.M.; Sjekavica, I. Fulminant Fournier’s gangrene in a patient with gastric cancer treated with ramucirumab and paclitaxel. Ther. Adv. Drug Saf. 2020, 11, 1–4. [Google Scholar] [CrossRef]
- ClinicalTrials.gov NCT04136782. Available online: https://www.clinicaltrials.gov/ct2/show/NCT04136782?term=NCT04136782&draw=2&rank=1 (accessed on 22 January 2021).
- ClinicalTrials.gov NCT04194203. Available online: https://www.clinicaltrials.gov/ct2/show/NCT04194203?term=NCT04194203&draw=2&rank=1 (accessed on 22 January 2021).
- Clinicaltrials.gov NCT04325698. Available online: https://www.clinicaltrials.gov/ct2/show/NCT04325698?term=NCT04325698&draw=2&rank=1 (accessed on 22 January 2021).
- ClinicalTrials.gov NCT04416035. Available online: https://www.clinicaltrials.gov/ct2/show/NCT04416035?term=NCT04416035&draw=2&rank=1 (accessed on 22 January 2021).
- ClinicalTrials.gov NCT03991403. Available online: https://www.clinicaltrials.gov/ct2/show/NCT03991403?term=NCT03991403&draw=2&rank=1 (accessed on 22 January 2021).
- ClinicalTrials.gov NCT04489888. Available online: https://www.clinicaltrials.gov/ct2/show/NCT04489888?term=NCT04489888&draw=2&rank=1 (accessed on 22 January 2021).
- ClinicalTrials.gov NCT03794778. Available online: https://www.clinicaltrials.gov/ct2/show/NCT03794778?term=NCT03794778&draw=2&rank=1 (accessed on 22 January 2021).
- ClinicalTrials.gov NCT04499924. Available online: https://www.clinicaltrials.gov/ct2/show/NCT04499924?term=NCT04499924&draw=2&rank=1 (accessed on 22 January 2021).
- ClinicalTrials.gov NCT04278092. Available online: https://www.clinicaltrials.gov/ct2/show/NCT04278092?term=NCT04278092&draw=2&rank=1 (accessed on 22 January 2021).
- ClinicalTrials.gov NCT03941093. Available online: https://www.clinicaltrials.gov/ct2/show/NCT03941093?term=NCT03941093&draw=2&rank=1 (accessed on 22 January 2021).
- ClinicalTrials.gov NCT03401827. Available online: https://www.clinicaltrials.gov/ct2/show/NCT03401827?term=NCT03401827&draw=2&rank=1 (accessed on 22 January 2021).
- Di Bartolomeo, M.; Niger, M.; Morano, F.; Corallo, S.; Antista, M.; Tamberi, S.; Lonardi, S.; Di Donato, S.; Berardi, R.; Scartozzi, M.; et al. Assessment of ramucirumab plus paclitaxel as switch maintenance versus continuation of first-line chemotherapy in patients with advanced HER-2 negative gastric or gastroesophageal junction cancers: The ARMANI phase III trial. BMC Cancer 2019, 19, 283. [Google Scholar] [CrossRef] [PubMed]
- Refolo, M.G.; Lotesoriere, C.; Lolli, I.R.; Messa, C.; D’Alessandro, R. Molecular mechanisms of synergistic action of ramucirumab and paclitaxel in gastric cancers cell lines. Sci. Rep. 2020, 10, 7162. [Google Scholar] [CrossRef] [PubMed]
- Sawatani, Y.; Komiyama, Y.; Nakashiro, K.I.; Uchida, D.; Fukumoto, C.; Shimura, M.; Hasegawa, T.; Kamimura, R.; Hitomi-Koide, M.; Hyodo, T.; et al. Paclitaxel potentiates the anticancer effect of cetuximab by enhancing antibody-dependent cellular cytotoxicity on oral squamous cell carcinoma cells in vitro. Int. J. Mol. Sci. 2020, 21, 6292. [Google Scholar] [CrossRef]
- Adkins, D.; Ley, J.; Trinkaus, K.; Thorstad, W.; Lewis, J.; Wildes, T.; Siegel, B.A.; Dehdashti, F.; Gay, H.; Mehan, P.; et al. A phase 2 trial of induction nab-paclitaxel and cetuximab given with cisplatin and 5-fluorouracil followed by concurrent cisplatin and radiation for locally advanced squamous cell carcinoma of the head and neck. Cancer 2013, 119, 766–773. [Google Scholar] [CrossRef]
- Borghaei, H.; Langer, C.J.; Millenson, M.; Tuttle, H.; Seldomridge, J.; Rovito, M.; Mintzer, D.; Treat, J. Phase II trial of cetuximab (C225) in combination with monthly carboplatin (Cb) and weekly paclitaxel (Pac) in patients with advanced NSCLC: Promising early results. J. Clin. Oncol. 2008, 26, 8104. [Google Scholar] [CrossRef]
- Enokida, T.; Ogawa, T.; Homma, A.; Okami, K.; Minami, S.; Nakanome, A.; Shimizu, Y.; Maki, D.; Ueda, Y.; Fujisawa, T.; et al. A multicenter phase II trial of paclitaxel, carboplatin, and cetuximab followed by chemoradiotherapy in patients with unresectable locally advanced squamous cell carcinoma of the head and neck. Cancer Med. 2020, 9, 1671–1682. [Google Scholar] [CrossRef] [PubMed]
- Hitt, R.; Irigoyen, A.; Nuñez, J.; Grau, J.; Saenz, J.G.; Pastor, M.; Jara, C.; Giron, C.G.; Hidalgo, M.; Hernandez, J.C. Phase II study of combination cetuximab and weekly paclitaxel in patients with metastatic/recurrent squamous cell carcinoma of head and neck (SCCHN): Spanish head and neck cancer group (TTCC). J. Clin. Oncol. 2007, 25, 6012. [Google Scholar] [CrossRef]
- Hussain, M.; Theodorescu, D. Re: Phase II trial of cetuximab with or without paclitaxel in patients with advanced urothelial tract carcinoma. Eur. Urol. 2014, 65, 501. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.S.; Moon, J.; Herbst, R.S.; Redman, M.W.; Dakhil, S.R.; Velasco, M.R.; Hirsch, F.R.; Mack, P.C.; Kelly, K.; Heymach, J.V.; et al. Phase II trial of carboplatin, paclitaxel, cetuximab, and bevacizumab followed by cetuximab and bevacizumab in advanced nonsquamous non-small-cell lung cancer SWOG S0536. J. Thorac. Oncol. 2013, 8, 1519–1528. [Google Scholar] [CrossRef] [PubMed]
- Langer, C.J.; Ruth, K.; Borghaei, H.; Treat, J.A.; Shafer, D.; Millenson, M.; Tuttle, H.; Rovito, M.; Mintzer, D. Phase II trial of cetuximab (C225) in combination with monthly carboplatin (Cb) and weekly paclitaxel (Pac) in patients with advanced NSCLC: Promising early results. J. Thorac. Oncol. 2007, 2, S465–S466. [Google Scholar] [CrossRef]
- Modi, S.; D’Andrea, G.; Norton, L.; Yao, T.J.; Caravelli, J.; Rosen, P.P.; Hudis, C.; Seidman, A.D. A phase I study of cetuximab/paclitaxel in patients with advanced-stage breast cancer. Clin. Breast Cancer 2006, 7, 270–277. [Google Scholar] [CrossRef]
- Pignata, S.; Scambia, G.; Lorusso, D.; De Giorgi, U.; Nicoletto, M.O.; Lauria, R.; Mosconi, A.M.; Sacco, C.; Omarini, C.; Tagliaferri, P.; et al. The MITO CERV-2 trial: A randomized phase II study of cetuximab plus carboplatin and paclitaxel, in advanced or recurrent cervical cancer. Gynecol. Oncol. 2019, 153, 535–540. [Google Scholar] [CrossRef]
- Socinski, M.A.; Saleh, M.N.; Trent, D.F.; Dobbs, T.W.; Zehngebot, L.M.; Levine, M.A.; Bordoni, R.; Stella, P.J. Randomized phase II trial of two dose schedules of carboplatin/paclitaxel/cetuximab in stage IIIB/IV non-small-cell lung cancer (NSCLC). Ann. Oncol. 2009, 20, 1068–1073. [Google Scholar] [CrossRef]
- Suntharalingam, M.; Winter, K.; Ilson, D.; Dicker, A.P.; Kachnic, L.; Konski, A.; Chakravarthy, A.B.; Anker, C.J.; Thakrar, H.; Horiba, N.; et al. Effect of the addition of cetuximab to paclitaxel, cisplatin, and radiation therapy for patients with esophageal cancer: The NRG Oncology RTOG 0436 phase 3 randomized clinical trial. JAMA Oncol. 2017, 3, 1520–1528. [Google Scholar] [CrossRef]
- Tahara, M.; Kiyota, N.; Yokota, T.; Hasegawa, Y.; Muro, K.; Takahashi, S.; Onoe, T.; Homma, A.; Taguchi, J.; Suzuki, M.; et al. Phase II trial of combination treatment with paclitaxel, carboplatin and cetuximab (PCE) as first-line treatment in patients with recurrent and/or metastatic squamous cell carcinoma of the head and neck (CSPOR-HN02). Ann. Oncol. 2018, 29, 1004–1009. [Google Scholar] [CrossRef]
- Bossi, P.; Miceli, R.; Locati, L.D.; Ferrari, D.; Vecchio, S.; Moretti, G.; Denaro, N.; Caponigro, F.; Airoldi, M.; Moro, C.; et al. A randomized, phase 2 study of cetuximab plus cisplatin with or without paclitaxel for the first-line treatment of patients with recurrent and/or metastatic squamous cell carcinoma of the head and neck. Ann. Oncol. 2017, 28, 2820–2826. [Google Scholar] [CrossRef] [PubMed]
- Wanebo, H.J.; Lee, J.; Burtness, B.A.; Ridge, J.A.; Ghebremichael, M.; Spencer, S.A.; Psyrri, D.; Pectasides, E.; Rimm, D.; Rosen, F.R.; et al. Induction cetuximab, paclitaxel, and carboplatin followed by chemoradiation with cetuximab, paclitaxel, and carboplatin for stage III/IV head and neck squamous cancer: A phase II ECOG-ACRIN trial (E2303). Ann. Oncol. 2014, 25, 2036–2041. [Google Scholar] [CrossRef]
- Wong, Y.N.; Litwin, S.; Vaughn, D.; Cohen, S.; Plimack, E.R.; Lee, J.; Song, W.; Dabrow, M.; Brody, M.; Tuttle, H.; et al. Phase II trial of cetuximab with or without paclitaxel in patients with advanced urothelial tract carcinoma. J. Clin. Oncol. 2012, 30, 3545–3551. [Google Scholar] [CrossRef] [PubMed]
- Picozzi, V.; Alseidi, A.; Winter, J.; Pishvaian, M.; Mody, K.; Glaspy, J.; Larson, T.; Matrana, M.; Carney, M.; Porter, S.; et al. Gemcitabine/nab-paclitaxel with pamrevlumab: A novel drug combination and trial design for the treatment of locally advanced pancreatic cancer. ESMO Open 2020, 5, e000668. [Google Scholar] [CrossRef] [PubMed]
- Staff, N.P.; Fehrenbacher, J.C.; Caillaud, M.; Damaj, M.I.; Segal, R.A.; Rieger, S. Pathogenesis of paclitaxel-induced peripheral neuropathy: A current review of in vitro and in vivo findings using rodent and human model systems. Exp. Neurol. 2020, 324, 113121. [Google Scholar] [CrossRef] [PubMed]
- Tonello, R.; Lee, S.H.; Berta, T. Monoclonal antibody targeting the matrix metalloproteinase 9 prevents and reverses paclitaxel-induced peripheral neuropathy in mice. J. Pain. 2019, 20, 515–527. [Google Scholar] [CrossRef] [PubMed]
- Huehnchen, P.; Muenzfeld, H.; Boehmerle, W.; Endres, M. Blockade of IL-6 signaling prevents paclitaxel-induced neuropathy in C57Bl/6 mice. Cell Death Dis. 2020, 11, 45. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.H.; Yeh, Y.M.; Chen, Y.F.; Hsu, Y.H.; Wang, H.H.; Lin, P.C.; Chang, L.Y.; Lin, C.C.K.; Chang, M.S.; Shen, M.R. Targeting interleukin-20 alleviates paclitaxel-induced peripheral neuropathy. Pain 2020, 161, 1237–1254. [Google Scholar] [CrossRef] [PubMed]
- Matsuoka, A.; Maeda, O.; Mizutani, T.; Nakano, Y.; Tsunoda, N.; Kikumori, T.; Goto, H.; Ando, Y. Bevacizumab exacerbates paclitaxel-induced neuropathy: A retrospective cohort study. PLoS ONE 2016, 11, e0168707. [Google Scholar] [CrossRef]
- Moreno-Aspitia, A.; Dueck, A.; Patel, T.; Hillman, D.; Tenner, K.; Dakhil, S.; Rowland, K.; McLaughlin, S.; Perez, E. Paclitaxel-related peripheral neuropathy associated with improved outcome of patients with early stage HER2+ breast cancer who did not receive trastuzumab in the N9831 clinical trial. Cancer Res. 2009, 69, 2100. [Google Scholar] [CrossRef]
- Sierecki, M.R.; Rugo, H.S.; McArthur, H.L.; Traina, T.A.; Paulson, M.; Rourke, M.; Norton, L.; Seidman, A.D.; Hudis, C.A.; Dickler, M.N. Incidence and severity of sensory neuropathy (SN) with bevacizumab (B) added to dose-dense (dd) doxorubicin/cyclophosphamide (AC) followed by nanoparticle albumin-bound (nab) paclitaxel (P) in patients (pts) with early stage breast cancer (BC). J. Clin. Oncol. 2008, 26. [Google Scholar] [CrossRef]
- Kazandjian, D.; Blumenthal, G.M.; Yuan, W.; He, K.; Keegan, P.; Pazdur, R. FDA approval of gefitinib for the treatment of patients with metastatic EGFR mutation–positive non–small cell lung cancer. Clin. Cancer Res. 2016, 22, 1307–1312. [Google Scholar] [CrossRef] [PubMed]
- Herbst, R.S.; Prager, D.; Hermann, R.; Fehrenbacher, L.; Johnson, B.E.; Sandler, A.; Kris, M.G.; Tran, H.T.; Klein, P.; Li, X.; et al. TRIBUTE investigator group. TRIBUTE: A phase III trial of erlotinib hydrochloride (OSI-774) combined with carboplatin and paclitaxel chemotherapy in advanced non-small-cell lung cancer. J. Clin. Oncol. 2005, 23, 5892–5899. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Zheng, B.; Xu, J.; Gao, S.; Lu, W. An albumin-bound drug conjugate of paclitaxel and indoleamine-2,3-dioxygenase inhibitor for enhanced cancer chemo-immunotherapy. Nanotechnology 2020, 31, 295101. [Google Scholar] [CrossRef]
- White, P.T.; Cohen, M.S. The discovery and development of sorafenib for the treatment of thyroid cancer. Expert Opin. Drug Discov. 2015, 10, 427–439. [Google Scholar] [CrossRef]
- Nawara, H.M.; Afify, S.M.; Hassan, G.; Zahra, M.H.; Atallah, M.N.; Mansour, H.; Abu Quora, H.A.; Alam, M.J.; Osman, A.; Kakuta, H.; et al. Paclitaxel and sorafenib: The effective combination of suppressing the self-renewal of cancer stem cells. Cancers 2020, 12, 1360. [Google Scholar] [CrossRef] [PubMed]
- De Jesus-Acosta, A.; Sugar, E.A.; O’Dwyer, P.J.; Ramanathan, R.K.; Von Hoff, D.D.; Rasheed, Z.; Zheng, L.; Begum, A.; Anders, R.; Maitra, A.; et al. Phase 2 study of vismodegib, a hedgehog inhibitor, combined with gemcitabine and nab-paclitaxel in patients with untreated metastatic pancreatic adenocarcinoma. Br. J. Cancer 2020, 122, 498–505. [Google Scholar] [CrossRef] [PubMed]
- Lorenzen, S.; Knorrenschild, J.R.; Pauligk, C.; Hegewisch-Becker, S.; Seraphin, J.; Thuss-Patience, P.; Kopp, H.G.; Dechow, T.; Vogel, A.; Luley, K.B.; et al. Phase III randomized, double-blind study of paclitaxel with and without everolimus in patients with advanced gastric or esophagogastric junction carcinoma who have progressed after therapy with a fluoropyrimidine/platinum-containing regimen (RADPAC). Int. J. Cancer 2020, 147, 2493–2502. [Google Scholar] [CrossRef]
- Alvarellos, M.L.; Lamba, J.; Sangkuhl, K.; Thorn, C.F.; Wang, L.; Klein, D.J.; Altman, R.B.; Klein, T.E. PharmGKB summary: Gemcitabine pathway. Pharmacogenet. Genomics 2014, 24, 564–574. [Google Scholar] [CrossRef]
- Von Hoff, D.D.; Ervin, T.; Arena, F.P.; Chiorean, E.G.; Infante, J.; Moore, M.; Seay, T.; Tjulandin, S.A.; Ma, W.W.; Saleh, M.N.; et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N. Engl. J. Med. 2013, 369, 1691–1703. [Google Scholar] [CrossRef]
- Wainberg, Z.A.; Hochster, H.S.; Kim, E.J.; George, B.; Kaylan, A.; Chiorean, E.G.; Waterhouse, D.M.; Guiterrez, M.; Parikh, A.; Jain, R.; et al. Open-label, phase I study of nivolumab combined with nab-paclitaxel plus gemcitabine in advanced pancreatic cancer. Clin. Cancer Res. 2020, 26, 4814–4822. [Google Scholar] [CrossRef] [PubMed]
- ClinicalTrials.gov. Available online: https://www.clinicaltrials.gov/ct2/results?term=paclitaxel+gemcitabine+nivolumab&Search=Apply&recrs=b&recrs=a&recrs=f&recrs=d&age_v=&gndr=&type=&rslt= (accessed on 22 January 2020).
- Yu, J.; Wang, Y.; Zhou, S.; Li, J.; Wang, J.; Chi, D.; Wang, X.; Lin, G.; He, Z.; Wang, Y. Remote loading paclitaxel–doxorubicin prodrug into liposomes for cancer combination therapy. Acta Pharm. Sin. B 2020, 10, 1730–1740. [Google Scholar] [CrossRef]
- Kaur, P.; Mishra, V.; Shunmugaperumal, T.; Goyal, A.K.; Ghosh, G.; Rath, G. Inhalable spray dried lipidnanoparticles for the co-delivery of paclitaxel and doxorubicin in lung cancer. J. Drug Deliv. Sci. Technol. 2020, 56, 101502. [Google Scholar] [CrossRef]
- Fraguas-Sanchez, A.I.; Fernández-Carballido, A.; Simancas-Herbada, R.; Martin-Sabroso, C.; Torres-Suárez, A.I. CBD loaded microparticles as a potential formulation to improve paclitaxel and doxorubicin-based chemotherapy in breast cancer. Int. J. Pharm. 2020, 574, 118916. [Google Scholar] [CrossRef] [PubMed]
- Zhu, C.; Jung, S.; Luo, S.; Meng, F.; Zhu, X.; Park, T.G.; Zhong, Z. Co-delivery of siRNA and paclitaxel into cancer cells by biodegradable cationic micelles based on PDMAEMA-PCL-PDMAEMA triblock copolymers. Biomaterials 2010, 31, 2408–2416. [Google Scholar] [CrossRef]
- Sun, T.M.; Du, J.Z.; Yao, Y.D.; Mao, C.Q.; Dou, S.; Huang, S.Y.; Zhang, P.Z.; Leong, K.W.; Song, E.W.; Wang, J. Simultaneous Delivery of siRNA and paclitaxel via a "two-in-one" micelleplex promotes synergistic tumor suppression. ACS Nano 2011, 5, 1483–1494. [Google Scholar] [CrossRef]
- Yin, T.; Wang, L.; Yin, L.; Zhou, J.; Huo, M. Co-delivery of hydrophobic paclitaxel and hydrophilic AURKA specific siRNA by redox-sensitive micelles for effective treatment of breast cancer. Biomaterials 2015, 61, 10–25. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.H.; Kim, E.; Park, D.E.; Shim, G.; Lee, S.; Kim, Y.B.; Kim, C.W.; Oh, Y.K. Cationic solid lipid nanoparticles for co-delivery of paclitaxel and siRNA. Eur. J. Pharm. Biopharm. 2012, 80, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Salzano, G.; Navarro, G.; Trivedi, M.S.; De Rosa, G.; Torchilin, V.P. Multifunctional polymeric micelles co-loaded with anti-survivin siRNA and paclitaxel overcome drug resistance in an animal model of ovarian cancer. Mol. Cancer Ther. 2015, 14, 1075–1084. [Google Scholar] [CrossRef]
- Škubník, J.; Rimpelová, S.; Jurášek, M.; Ruml, T. Mitotic poisons in research and medicine. Molecules 2020, 25, 4632. [Google Scholar] [CrossRef] [PubMed]
- Falchook, G.; Coleman, R.L.; Roszak, A.; Behbakht, K.; Matulonis, U.; Ray-Coquard, I.; Sawrycki, P.; Duska, L.R.; Tew, W.; Ghamande, S.; et al. Alisertib in combination with weekly paclitaxel in patients with advanced breast cancer or recurrent ovarian cancer: A randomized clinical trial. JAMA Oncol. 2019, 5, e183773. [Google Scholar] [CrossRef] [PubMed]
- Yasuhira, S.; Shibazaki, M.; Nishiya, M.; Maesawa, C. Paclitaxel-induced aberrant mitosis and mitotic slippage efficiently lead to proliferative death irrespective of canonical apoptosis and p53. Cell Cycle 2016, 15, 3268–3277. [Google Scholar] [CrossRef]
- Bombuwala, K.; Kinstle, T.; Popik, V.; Uppal, S.O.; Olesen, J.B.; Viña, J.; Heckman, C.A. Colchitaxel, a coupled compound made from microtubule inhibitors colchicine and paclitaxel. Beilstein J. Org. Chem. 2006, 2, 13. [Google Scholar] [CrossRef]
- Peterková, L.; Kmoníčková, E.; Ruml, T.; Rimpelová, S. Sarco/endoplasmic reticulum calcium ATPase inhibitors: Beyond anticancer perspective. J. Med. Chem. 2020, 63, 1937–1963. [Google Scholar] [CrossRef] [PubMed]
- Ashrafizadeh, M.; Zarrabi, A.; Hashemi, F.; Moghadam, E.R.; Hashemi, F.; Entezari, M.; Hushmandi, K.; Mohammadinejad, R.; Najafi, M. Curcumin in cancer therapy: A novel adjunct for combination chemotherapy with paclitaxel and alleviation of its adverse effects. Life Sci. 2020, 256, 117984. [Google Scholar] [CrossRef]
- Shen, L.; Liu, C.C.; An, C.Y.; Ji, H.F. How does curcumin work with poor bioavailability? Clues from experimental and theoretical studies. Sci. Rep. 2016, 6, 20872. [Google Scholar] [CrossRef] [PubMed]
- Nelson, K.M.; Dahlin, J.L.; Bisson, J.; Graham, J.; Pauli, G.F.; Walters, M.A. The essential medicinal chemistry of curcumin. J. Med. Chem. 2017, 60, 1620–1637. [Google Scholar] [CrossRef] [PubMed]
- Garofalo, M.; Saari, H.; Somersalo, P.; Crescenti, D.; Kuryk, L.; Aksela, L.; Capasso, C.; Madetoja, M.; Koskinen, K.; Oksanen, T.; et al. Antitumor effect of oncolytic virus and paclitaxel encapsulated in extracellular vesicles for lung cancer treatment. J. Control. Release 2018, 283, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Lal, G.; Rajala, M.S. Combination of oncolytic measles virus armed with BNiP3, a pro-apoptotic gene and paclitaxel induces breast cancer cell death. Front. Oncol. 2019, 8, 676. [Google Scholar] [CrossRef]
- ClinicalTrials.gov. Available online: https://www.clinicaltrials.gov/ct2/results?cond=&term=docetaxel+combination&cntry=&state=&city=&dist= (accessed on 1 November 2020).
- Bishop, R.T.; Marino, S.; Carrasco, G.; Li, B.; Allen, R.J.; Sparatore, A.; Ottewell, P.D.; Mollat, P.; Sims, A.H.; Capulli, M.; et al. Combined administration of a small-molecule inhibitor of TRAF6 and Docetaxel reduces breast cancer skeletal metastasis and osteolysis. Cancer Lett. 2020, 488, 27–39. [Google Scholar] [CrossRef]
- Hasegawa, H.; Kaneko, T.; Kanno, C.; Endo, M.; Yamazaki, M.; Kitabatake, T.; Monma, T.; Takeishi, E.; Sato, E.; Kano, M. Preoperative intra-arterial chemotherapy with docetaxel, cisplatin, and peplomycin combined with intravenous chemotherapy using 5-fluorouracil for oral squamous cell carcinoma. Int. J. Oral Maxillofac. Surg. 2020, 49, 984–992. [Google Scholar] [CrossRef] [PubMed]
- Rodallec, A.; Franco, C.; Robert, S.; Sicard, G.; Giacometti, S.; Lacarelle, B.; Bouquet, F.; Savina, A.; Lacroix, R.; Dignat-George, F.; et al. Prototyping trastuzumab docetaxel immunoliposomes with a new FCM-based method to quantify optimal antibody density on nanoparticles. Sci. Rep. 2020, 10, 4147. [Google Scholar] [CrossRef]
- Laber, D.A.; Eatrides, J.; Jaglal, M.V.; Haider, M.; Visweshwar, N.; Patel, A. A phase I/II study of docetaxel in combination with pegylated liposomal doxorubicin in metastatic castration-resistant prostate cancer. Med. Oncol. 2020, 37, 95. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Li, Y.; Liu, H.; Jain, A.; Patel, P.V.; Cheng, K. Co-delivery of IKBKE siRNA and cabazitaxel by hybrid nanocomplex inhibits invasiveness and growth of triple-negative breast cancer. Sci. Adv. 2020, 6, eabb0616. [Google Scholar] [CrossRef]
- Chen, Y.; Deng, Y.; Zhu, C.; Xiang, C. Anti prostate cancer therapy: Aptamer-functionalized, curcumin and cabazitaxel co-delivered, tumor targeted lipid-polymer hybrid nanoparticles. Biomed. Pharmacother. 2020, 127, 110181. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, N.C.; Jech, K.; Masters, S.; Brobst, S.W.; Alvarado, A.B.; Hoover, A.J.; Snader, K.M. Effects of genetic, epigenetic, and environmental factors on taxol content in Taxus brevifolia and related species. J. Nat. Prod. 1992, 55, 432–440. [Google Scholar] [CrossRef] [PubMed]




| Taxane Formulation | Number of Completed and Ongoing Clinical Trials | Ref. | |||
|---|---|---|---|---|---|
| Completed | Active | Recruiting | Not Yet Recruiting | ||
| Lipusu® | - 1 | 1 | - | - | [66] |
| LEP-ETU | 3 | - | - | - | [67] |
| EndoTAG-1 | - | 4 | 2 | - | [68] |
| PTX-LDE | - | - | - | - | [69] |
| LE-DT | 2 | - | - | - | [70] |
| ATI-1123 | 1 | - | - | - | [71] |
| Genexol-PM® | 8 | - | 1 | - | [72] |
| Nanoxel® | - | - | 1 | 1 | [73] |
| Paclical® | 1 | - | - | - | [74] |
| Monoclonal Antibody | Trade Name | Company | Molecular Target | Ref. |
|---|---|---|---|---|
| Oregovomab | OvaRex® | Quest PharmaTech | Human mucin 16/cancer antigen 125 | [121] |
| Lumretuzumab | n.t. | Roche | Human epidermal growth factor receptor 3 | [122] |
| Nivolumab | Opdivo® | Bristol Myers Squibb | Programmed cell death 1 protein | [123,124] |
| Atezolizumab | Tecentriq® | Roche | Programmed death-ligand 1 | [125] |
| Trastuzumab | Herceptin® | Roche | Human epidermal growth factor receptor 2 | [126] |
| Pertuzumab | Perjeta® | Roche | Human epidermal growth factor receptor 2 | [126] |
| Cetuximab | Erbitux® | Merck KGaA, Eli Lilly, Bristol-Myers Squibb | Epidermal growth factor receptor | [127] |
| Necitumumab | Portrazza® | Eli Lilly | Epidermal growth factor receptor | [128] |
| Compound Combination | Condition | Status | Phase | Clinical Trial Identifier | Ref. |
|---|---|---|---|---|---|
| Paclitaxel + carboplatin | Breast cancer | not yet recruiting | IV. | NCT04136782 | [135] |
| Paclitaxel + carboplatin + bevacizumab | Non-small cell lung cancer | recruiting | III. | NCT04194203 | [136] |
| recruiting | III. | NCT04325698 | [137] | ||
| recruiting | III. | NCT04416035 | [138] | ||
| Paclitaxel + carboplatin + bevacizumab + atezolizumab | Non-small cell lung cancer | recruiting | III. | NCT03991403 | [139] |
| Paclitaxel + carboplatin + pembrolizumab | Squamous head and neck carcinoma | recruiting | IV. | NCT04489888 | [140] |
| Paclitaxel + carboplatin + doxorubicin | Ovarian cancer | recruiting | IV. | NCT03794778 | [141] |
| Paclitaxel + ramucirumab | Gastroesophageal cancer | not yet recruiting | III. | NCT04499924 | [142] |
| Paclitaxel + cetuximab | Squamous head and neck carcinoma | recruiting | II. | NCT04278092 | [143] |
| Paclitaxel/gemcitabine + pamrevlumab | Pancreatic cancer | recruiting | III. | NCT03941093 | [144] |
| Paclitaxel + gemcitabine | Pancreatic cancer | unknown | IV. | NCT03401827 | [145] |
| Drug Combination | Search Term | Number of Clinical Trials (by October 2020) |
|---|---|---|
| Paclitaxel + carboplatin + bevacizumab | paclitaxel carboplatin bevacizumab | 164 |
| Paclitaxel + ramucirumab | paclitaxel ramucirumab | 34 |
| Paclitaxel + cetuximab | paclitaxel cetuximab | 70 |
| Paclitaxel + gefitinib | paclitaxel gefitinib | 20 |
| Paclitaxel + erlotinib | paclitaxel erlotinib | 51 |
| Paclitaxel + sorafenib | paclitaxel sorafenib | 28 |
| Paclitaxel + vismodegib | paclitaxel vismodegib | 5 |
| Paclitaxel + everolimus | paclitaxel everolimus | 57 |
| Paclitaxel + gemcitabine | paclitaxel gemcitabine | 499 |
| Paclitaxel + doxorubicin | paclitaxel rubicin | 284 |
| Paclitaxel + alisertib | paclitaxel alisertib | 8 |
| Paclitaxel + curcumin | paclitaxel curcumin | 2 |
| Paclitaxel + viral therapy | paclitaxel viral | 41 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Škubník, J.; Pavlíčková, V.; Ruml, T.; Rimpelová, S. Current Perspectives on Taxanes: Focus on Their Bioactivity, Delivery and Combination Therapy. Plants 2021, 10, 569. https://doi.org/10.3390/plants10030569
Škubník J, Pavlíčková V, Ruml T, Rimpelová S. Current Perspectives on Taxanes: Focus on Their Bioactivity, Delivery and Combination Therapy. Plants. 2021; 10(3):569. https://doi.org/10.3390/plants10030569
Chicago/Turabian StyleŠkubník, Jan, Vladimíra Pavlíčková, Tomáš Ruml, and Silvie Rimpelová. 2021. "Current Perspectives on Taxanes: Focus on Their Bioactivity, Delivery and Combination Therapy" Plants 10, no. 3: 569. https://doi.org/10.3390/plants10030569
APA StyleŠkubník, J., Pavlíčková, V., Ruml, T., & Rimpelová, S. (2021). Current Perspectives on Taxanes: Focus on Their Bioactivity, Delivery and Combination Therapy. Plants, 10(3), 569. https://doi.org/10.3390/plants10030569








