Bulgarian Medicinal Extracts as Natural Inhibitors with Antiviral and Antibacterial Activity
Abstract
:1. Introduction
2. Results
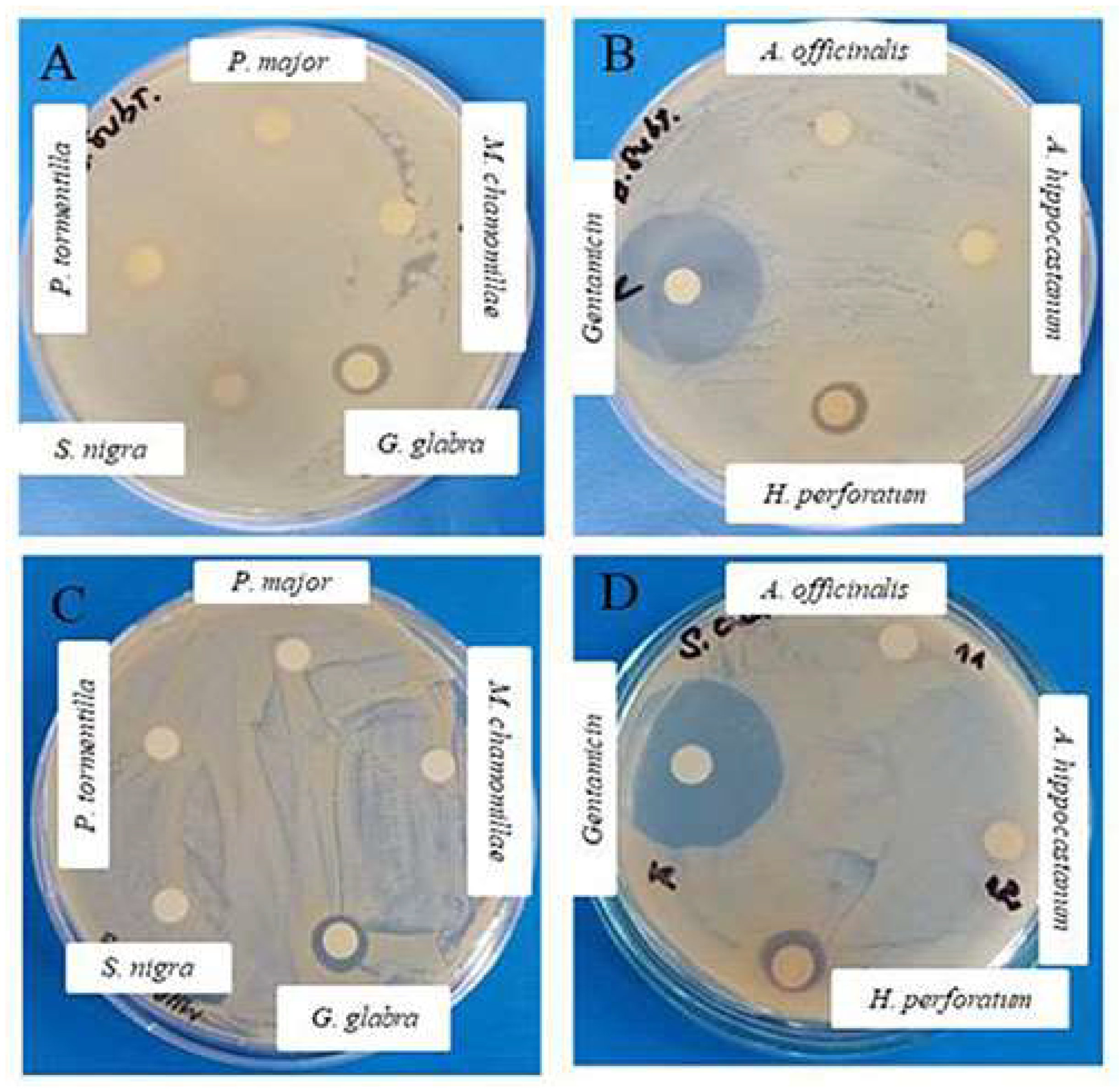
| Plant Extracts | Concentrations | Diameter of the Inhibition Zones (mm) | ||||
|---|---|---|---|---|---|---|
| B. subtilis | S. aureus | S. saprophyticus | E. coli 25,922 | E. coli 420 | ||
| Glycyrrhiza glabra L. | 10 mg/mL | - | - | - | - | - |
| 20 mg/mL | 9 ± 0.7 | - | - | - | - | |
| 40 mg/mL | 11 ± 0.6 | 12 ± 0.7 | - | - | - | |
| Hypericum perforatum | 10 mg/mL | - | - | - | - | - |
| 20 mg/mL | 9 ± 0.5 | - | - | - | ||
| 40 mg/mL | 10 ± 0 | 10 ± 0.5 | - | - | - | |
| Extract | Cytotoxicity (µg/mL) | |||||
|---|---|---|---|---|---|---|
| HEp-2 | MDBK | HCT-8 | ||||
| CC50 * Mean ± SD ** | MTC *** | CC50 * Mean ± SD ** | MTC *** | CC50 * Mean ± SD ** | MTC *** | |
| A. hippocastani | 965.0 ± 21.7 | 400.0 | 1450.0 ± 33.4 | 1000.0 | 1420.0 ± 46.2 | 800.0 |
| G. glabra | 1280.0 ± 34.3 | 550.0 | 1850.0 ± 45.2 | 1000.0 | 1820.0 ± 24.5 | 1000.0 |
| O. basilicum | 1055.0 ± 16.6 | 550.0 | 1530.0 ± 29.7 | 1000.0 | 1300.0 ± 37.2 | 1000.0 |
| A. sativum | 1320.0 ± 22.5 | 550.0 | 2200.0 ± 38.5 | 2000.0 | 1880.0 ± 55.7 | 1200.0 |
| P. reptans | 1540.0 ± 36.2 | 1000.0 | 1890.0 ± 36.7 | 200.0 | 1880.0 ± 37.1 | 200.0 |
| M. chamomilla | 920.0± 18.5 | 500.0 | 1300.0 ± 41.4 | 1000.0 | 1150.0 ± 44.6 | 1000.0 |
| T. vulgaris | 1500.0 ± 21.8 | 1000.0 | 1500.0 ± 18.2 | 500.0 | 1100.0 ± 16.8 | 400.0 |
| A. officinalis | 2030.0 ± 34.2 | 1000.0 | 2450.0 ± 38.9 | 2000.0 | 2300.0 ± 62.4 | 1500.0 |
| R. canina | 1800.0 ± 26.3 | 1200.0 | 1700.0 ± 39.5 | 300.0 | 1600.0 ± 37.6 | 280.0 |
| A. annua | 1990.0 ± 41.2 | 1000.0 | 1320.0 ± 22.2 | 350.0 | 1200.0 ± 20.1 | 320.0 |
| S. nigra | 1440.0 ± 19.5 | 1000.0 | 2100.0 ± 47.1 | 1000.0 | 1900.0 ± 48.3 | 1000.0 |
| H. perforatum | 1650.0 ± 28.3 | 1000.0 | 1320.0 ± 32.4 | 1000.0 | 1220.0 ± 28.5 | 1000.0 |
| P. lanceolata | 1620.0 ± 23.5 | 1000.0 | 1980.0 ± 56.2 | 1000.0 | 1700.0 ± 46.2 | 1000.0 |
| Extract | Antiviral Activity | |||
|---|---|---|---|---|
| HSV-1 (Victoria) | HCoV-OC43 | |||
| IC50 * Mean ± SD ** (µg/mL) | SI *** | IC50 * Mean ± SD ** (µg/mL) | SI *** | |
| A. hippocastani | 205.0 ± 7.4 | 7.1 | 380.0 ± 9.5 | 3.7 |
| G. glabra | 272.0 ± 3.6 | 6.8 | 400.0 ± 12.5 | 4.5 |
| O. basilicum | 340.0 ± 5.2 | 4.5 | - | - |
| A. sativum | 260.0 ± 4.7 | 8.5 | 900.0 ± 18.5 | 2.1 |
| P. reptans | - | - | 890.0 ± 17.3 | 2.1 |
| M. chamomilla | 365.0 ± 6.2 | 3.6 | - | - |
| T. vulgaris | 650.0 ± 8.3 | 2.3 | - | - |
| S. nigra | - | - | 950.0 ± 32.7 | 2.0 |
| Extract | Δlg | |||
|---|---|---|---|---|
| 15 min | 60 min | 90 min | 120 min | |
| A. hippocastani | 0 | 0.5 | 0.8 | 0.8 |
| G. glabra | 0 | 0.5 | 0.5 | 0.5 |
| O. basilicum | 0 | 0.5 | 0.8 | 0.8 |
| A. sativum | 0 | 0 | 0 | 0 |
| P. reptans | 0 | 1.0 | 1.0 | 1.0 |
| M. chamomilla | 0 | 0.5 | 0.5 | 0.5 |
| T. vulgaris | 0.5 | 1.0 | 1.2 | 1.2 |
| A. officinalis | 0 | 0 | 0 | 0 |
| R. canina | 0 | 1.0 | 1.0 | 1.0 |
| A. annua | 0 | 0 | 0 | 0 |
| S. nigra | 0.5 | 0.9 | 1.0 | 1.0 |
| H. perforatum | 0 | 0 | 0 | 0 |
| P. lanceolata | 0 | 0.5 | 0.8 | 0.8 |
| Extract | Δlg | |||
|---|---|---|---|---|
| 15 min | 60 min | 90 min | 120 min | |
| A. hippocastani | 0 | 0.3 | 0.3 | 0.3 |
| G. glabra | 0 | 0.5 | 0.5 | 0.5 |
| O. basilicum | 0 | 0 | 0 | 0 |
| A. sativum | 0 | 0 | 0.5 | 0.5 |
| P. reptans | 0 | 0.3 | 0.3 | 0.3 |
| M. chamomilla | 0 | 0.5 | 0.5 | 0.5 |
| T. vulgaris | 0.5 | 0.5 | 0.7 | 0.7 |
| A. officinalis | 0 | 0 | 0 | 0.5 |
| R. canina | 0 | 0 | 0.3 | 0.5 |
| A. annua | 0 | 0 | 0 | 0 |
| S. nigra | 0 | 0 | 0 | 0 |
| H. perforatum | 0 | 0.5 | 0.5 | 0.5 |
| P. lanceolata | 0 | 0.5 | 0.5 | 0.7 |
| Extract | Δlg | ||||
|---|---|---|---|---|---|
| 15 min | 30 min | 60 min | 90 min | 120 min | |
| A. hippocastani | 1.25 | 1.25 | 1.75 | 1.75 | 1.75 |
| G. glabra | 1.5 | 1.5 | 1.5 | 1.75 | 1.75 |
| O. basilicum | 1.0 | 1.0 | 1.0 | 2.0 | 2.0 |
| A. sativum | 0.5 | 1.5 | 1.5 | 1.5 | 1.5 |
| P. reptans | 1.75 | 1.75 | 1.75 | 1.75 | 1.75 |
| M. chamomilla | 1.0 | 1.0 | 1.75 | 1.75 | 1.75 |
| T. vulgaris | 0.5 | 1.0 | 2.0 | 2.0 | 2.0 |
| A. officinalis | 0.5 | 1.0 | 1.0 | 1.5 | 1.5 |
| R. canina | 1.25 | 1.5 | 1.5 | 1.5 | 1.5 |
| A. annua | 0.75 | 0.75 | 1.0 | 1.0 | 1.0 |
| S. nigra | 0.75 | 0.75 | 0.75 | 1.0 | 1.0 |
| H. perforatum | 1.0 | 1.0 | 2.0 | 2.0 | 2.0 |
| P. lanceolata | 0.5 | 1.0 | 2.0 | 2.0 | 2.0 |
3. Discussion
4. Materials and Methods
4.1. Cells
4.2. Viruses
4.3. Bacterial Strains and Growth Conditions
4.4. Researched Plant Material
Production of Dry Extract
| Plant Species | Area of the Collected Material | Biological Activities | References | |
|---|---|---|---|---|
| Plantago lanceolata (ribwort plantain) |  | Stem | Used to treat wounds and inflammation; in diseases of the skin, respiratory organs, digestive system, reproduction, blood circulation; analgesic, antitumor, antioxidant, immunomodulatory activity. | [57,58] |
| Matricaria chamomilla L. (chamomile) |  | Flower | Antibacterial, antifungal, antioxidant activity; mosquito repellent and larvicidal effects. | [59,60] |
| Glycyrrhiza glabra L. (licorice) |  | Root | Widely used for gastrointestinal problems (gastritis, peptic ulcers), cough, bronchitis, arthritis, respiratory infections, and tremors. Anti-inflammatory, antispasmodic, antioxidant, antimalarial, antifungal, antibacterial, antiviral, antidiabetic activity. | [61,62,63] |
| Sambucus nigra (elderberry) |  | Fruit | Anti-inflammatory, antiviral, immunomodulatory activity. | [49,50] |
| Potentilla reptans (creeping cinquefoil) |  | Stem | Antidiarrheal, anti-diabetic, antispasmodic, anti-inflammatory, antitumor, hepatoprotective, antioxidant, antifungal, antibacterial, antiviral activity. | [64] |
| Ocimum basilicum (basil) |  | Stem | Anti-inflammatory, antioxidant, anthelmintic, antibacterial, antiviral activity. | [65,66,67] |
| Thymus vulgaris (thyme) |  | Stem | Anti-inflammatory, cardioprotective, neuroprotective, anti-osteoporotic, antispasmodic, anthelmintic, gastroprotective, antitumor, antioxidant, antibacterial, antiviral, immunoprotective activity. | [68,69,70,71] |
| Artemisia annua (sweet wormwood) |  | Stem | Anti-fever, antimalarial, antimicrobial, antiviral action. | [72,73] |
| Rosa canina L. (rosehip) |  | Fruit | Anit-osteoarthritis, anti-anxiety, anti-depression, analgesic, anti-diabetic, antihyperlipidemic, neuroprotective, anti-inflammatory, antioxidant, antitumor, antimicrobial effect. | [74,75] |
| Allium sativum (garlic) |  | Bulb | In the prevention of infectious diseases, antiviral activity by inhibiting the entry of the virus, inhibition of viral RNA polymerase, reverse transcriptase, DNA synthesis; immunomodulatory activity. | [55] |
| Althaea officinalis (white rose) |  | Root | Cough suppressing, anti-inflammatory, antioxidant, antimicrobial, immunomodulatory action. | [76,77] |
| Aesculus hippocastani (horse chestnut) |  | Seed | Vascular supporting, anti-inflammatory, antioxidant, immunomodulatory, virucidal, antiviral (against HSV-1, VSV, RSV, Dengue virus) activity. | [51,78] |
| Hypericum perforatum (St. John’s wort) |  | Stem | Burn healing, anti-anxiety, mild to moderate anti-depression, neuroprotection, anti-inflammatory, antioxidant, antiviral, antimicrobial, antitumoral, wound-healing and pain relief effects. | [79,80] |
4.5. Disc Diffusion Assay
4.6. Cytotoxicity Assay
4.7. Antiviral Activity Assay
4.8. Virucidal Assay
4.9. Pre-Treatment of Healthy Cells
4.10. Effect on Viral Adsorption
4.11. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Piret, J.; Boivin, G. Resistance of herpes simplex viruses to nucleoside analogues: Mechanisms, prevalence, and management. Antimicrob. Agents Chemother. 2011, 55, 459–472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stoitsova, S.; Paunova-Krasteva, T.; Borisova, D. Modulation of Biofilm Growth by Sub-Inhibitory Amounts of Antibacterial Substances. In Microbial Biofilms—Importance and Applications; Dhanasekaran, D., Thajuddin, N., Eds.; IntechOpen: London, UK, 2016; pp. 441–462. [Google Scholar]
- Borges, A.; Abreu, A.C.; Dias, C.; Saavedra, M.J.; Borges, F.; Simões, M. New perspectives on the use of phytochemicals as an emergent strategy to control bacterial infections including biofilms. Molecules 2016, 21, 877. [Google Scholar] [CrossRef] [PubMed]
- Othman, L.; Sleiman, A.; Abdel-Massih, R.M. Antimicrobial activity of polyphenols and alkaloids in middle eastern plants. Front. Microbiol. 2019, 10, 911. [Google Scholar] [CrossRef] [PubMed]
- Poli, J.P.; Guinoiseau, E.; De Rocca Serra, D.; Sutour, S.; Paoli, M.; Tomi, F.; Quilichini, Y.; Berti, L.; Lorenzi, V. Anti-quorum sensing activity of 12 essential oils on chromobacterium violaceum and specific action of cis-cis-p-menthenolide from corsican Mentha suaveolens ssp. Insularis. Molecules 2018, 23, 2125. [Google Scholar] [CrossRef] [Green Version]
- Todorov, D.; Hinkov, A.; Shishkova, K.; Shishkov, S. Antiviral potential of Bulgarian medicinal plants. Phytochem. Rev. 2014, 13, 525–538. [Google Scholar] [CrossRef]
- Mukhtar, M.; Arshad, M.; Ahmad, M.; Pomerantz, R.J.; Wigdahl, B.; Parveen, Z. Antiviral potentials of medicinal plants. Virus Res. 2008, 131, 111–120. [Google Scholar] [CrossRef]
- Schippmann, U.; Leaman, D.; Cunningham, A. A Comparison of Cultivation and Wild Collection of Medicinal and Aromatic Plants Under Sustainability Aspects. Med. Aromat. Plants 2006, 17, 75–95. [Google Scholar] [CrossRef]
- Zahariev, D.; Radeva, V. Ethnobotanical research of the medicinal plants in Balchik Municipality (Bulgaria). Acta Sci. Nat. 2020, 7, 81–95. [Google Scholar] [CrossRef]
- Isaev, I.; Landjev, I.; Nechev, G. Herbs in Bulgaria and Their Use, 3rd ed.; Zemizdat: Sofia, Bulgaria, 1977; p. 115. [Google Scholar]
- Dimitrova, D.; Raycheva, T. Ethnobotany and Modern Agrarian Education in Bulgaria. Sci. Work. 2010, 2, 333–338. [Google Scholar]
- Ivancheva, S.; Stantcheva, B. Ethnobotanical inventory of medicinal plants in Bulgaria. J. Ethnopharmacol. 2000, 69, 165–172. [Google Scholar] [CrossRef]
- Nedelcheva, A. Medicinal plants from an old Bulgarian medical book. J. Med. Plants Res. 2012, 6, 2324–2339. [Google Scholar] [CrossRef] [Green Version]
- Ploetz, K.; Orr, B. Wild Herb Use in Bulgaria. Econ. Bot. 2004, 58, 231–241. [Google Scholar] [CrossRef]
- Leporatti, M.L.; Ivancheva, S. Preliminary comparative analysis of medicinal plants used in the traditional medicine of Bulgaria and Italy. J. Ethnopharmacol. 2003, 87, 123–142. [Google Scholar] [CrossRef]
- Ploetz, K.L. An Ethnobotanical Study of Wild Herb Use in Bulgaria. In A Thesis, Master of Science in Forestry; Michigan Technological University: Houghton, MI, USA, 2000. [Google Scholar]
- Kültür, Ş.; Sami, S.N. Medicinal plants used in Isperih (RazgradBulgaria) District. Turk. J. Pharm. Sci. 2009, 6, 107–124. [Google Scholar]
- de Boer, H. Local Awareness of Scarcity and Endangerment of Medicinal Plants in Roussenski Lom Natural Park in Northern Bulgaria. In Ethnobiology in the New Europe; Pardo-deSantayana, M., Pieroni, A., Puri, R.K., Eds.; Berghahn Books: New York, NY, USA, 2010; Volume 14, pp. 93–111. [Google Scholar]
- Bertsch, C.A. An Ethnobotanical Survey of the Economic and Cultural Significance of Non-Timber Forest Products in the Southwest Rhodope Mountain Region of Bulgaria. In A Thesis, Master of Science in Forestry; Michigan Technological University: Houghton, MI, USA, 2011. [Google Scholar]
- Vacheva, A.; Mustafa, B.; Staneva, J.; Marhova, M.; Kostadinova, S.; Todorova, M.; Ivanova, R.; Stoitsova, S. Effects of extracts from medicinal plants on biofilm formation by Escherichia coli urinary tract isolates. Biotechnol. Biotechnol. Equip. 2011, 25, 92–97. [Google Scholar] [CrossRef] [Green Version]
- Stoitsova, S.; Vacheva, A.; Paunova-Krasteva, T.; Ivanova, R.; Danova, S.; Manasiev, J. The multicellular behavior of Escherichia coli: A target for interferences. In New Trends in Microbiology; Najdenski, H., Ed.; The Stephan Angeloff Institute of Microbiology: Sofia, Bulgaria, 2012; pp. 147–158. ISBN 978-954-92882-1-6. [Google Scholar]
- Koleva, V.; Dragoeva, A.; Stoyanova, Z.; Koynova, T.; Dashev, G. An ethnobotanical study on current status of some medicinal plants used in Bulgaria. Int. J. Curr. Microbiol. App. Sci. 2015, 4, 297–305. [Google Scholar]
- Vilhelmova, N.; Simeonova, L.; Nikolova, N.; Pavlova, E.; Gospodinova, Z.; Antov, G.; Galabov, A.; Nikolova, I. Antiviral, Cytotoxic and Antioxidant Effects of Tanacetum Vulgare, L. Crude Extract In Vitro. Folia Med. 2020, 62, 172–179. [Google Scholar] [CrossRef]
- Zaharieva, M.M.; Dimitrova, L.L.; Philipov, S.; Nikolova, I.; Vilhelmova, N.; Grozdanov, P.; Nikolova, N.; Popova, M.; Bankova, V.; Konstantinov, S.M.; et al. In Vitro Antineoplastic and Antiviral Activity and In Vivo Toxicity of Geum urbanum L. Extracts. Molecules 2022, 27, 245. [Google Scholar] [CrossRef]
- Aliyu, A.B.; Koorbanally, N.A.; Moodley, B.; Singh, P.; Chenia, H.Y. Quorum sensing inhibitory potential and molecular docking studies of sesquiterpene lactones from Vernonia blumeoides. Phytochemistry 2016, 126, 23–33. [Google Scholar] [CrossRef]
- Kazemian, H.; Ghafourian, S.; Heidari, H.; Amiri, P.; Yamchi, J.K.; Shavalipour, A.; Houri, H.; Maleki, A.; Sadeghifard, N. Antibacterial, anti-swarming and anti-biofilm formation activities of Chamaemelum nobile against Pseudomonas aeruginosa. Rev. Soc. Bras. Med. Trop. 2015, 48, 432–436. [Google Scholar] [CrossRef] [Green Version]
- Bacha, K.; Tariku, Y.; Gebreyesus, F.; Zerihun, S.; Mohammed, A.; Weiland-Bräuer, N.; Schmitz, R.A.; Mulat, M. Antimicrobial and anti-Quorum Sensing activities of selected medicinal plants of Ethiopia: Implication for development of potent antimicrobial agents. BMC Microbiol. 2016, 16, 139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vilhelmova-Ilieva, N.; Jacquet, R.; Deffieux, D.; Pouységu, L.; Sylla, T.; Chassaing, S.; Nikolova, I.; Quideau, S.; Galabov, A.S. Anti-Herpes Simplex Virus Type 1 Activity of Specially Selected Groups of Tannins. Drug Res. 2019, 69, 374–381. [Google Scholar] [CrossRef] [PubMed]
- Trendafilova, A.; Ivanova, V.; Rangelov, M.; Todorova, M.; Ozek, G.; Yur, S.; Ozek, T.; Aneva, I.; Veleva, R.; Moskova-Doumanova, V.; et al. Caffeoylquinic Acids, Cytotoxic, Antioxidant, Acetylcholinesterase and Tyrosinase Enzyme Inhibitory Activities of Six Inula Species from Bulgaria. Chem. Biodivers. 2020, 17, e2000051. [Google Scholar] [CrossRef]
- Ma, L.; Yao, L. Antiviral effects of plant-derived essential oils and their components: An updated review. Molecules 2020, 25, 2627. [Google Scholar] [CrossRef]
- Reyes-Jurado, F.; Navarro-Cruz, A.R.; Ochoa-Velasco, C.E.; Palou, E.; López-Malo, A.; Ávila-Sosa, R. Essential oils in vapor phase as alternative antimicrobials: A review. Crit. Rev. Food Sci. Nutr. 2020, 60, 1641–1650. [Google Scholar] [CrossRef] [PubMed]
- Moloney, M.G. Natural Products as a Source for Novel Antibiotics. Trends Pharm. Sci. 2016, 37, 689–701. [Google Scholar] [CrossRef] [PubMed]
- Górniak, I.; Bartoszowski, R.; Króliczewski, J. Comprehensive review of antimicrobial activity of plant flavonoids. Phytochem. Rev. 2019, 18, 241–272. [Google Scholar] [CrossRef] [Green Version]
- Cowan, M.M. Plants products as antimicrobial agents. Clin. Microbiol. Rev. 1999, 12, 564–582. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jarić, S.; Kostić, O.; Mataruga, Z.; Pavlović, D.; Pavlović, M.; Mitrović, M.; Pavlović, P. Traditional wound-healing plants used in the Balkan region (Southeast Europe). J. Ethnopharmacol. 2018, 211, 311–328. [Google Scholar] [CrossRef]
- Chitemerere, T.A.; Mukanganyama, S. Evaluation of cell membrane integrity as a potential antimicrobial target for plant products. BMC Complement. Altern. Med. 2014, 14, 278. [Google Scholar] [CrossRef] [Green Version]
- Zdarta, A.; Smułek, W.; Pacholak, A.; Kaczorek, E. Environmental aspects of the use of hedera helix extract in bioremediation process. Microorganisms 2019, 7, 43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saddiqe, Z.; Naeem, I.; Maimoona, A. A review of the antibacterial activity of Hypericum perforatum L. J. Ethnopharmacol. 2010, 131, 511–521. [Google Scholar] [CrossRef] [PubMed]
- Tusevski, O.; Krstikj, M.; Petreska Stanoeva, J.; Stefova, M.; Gadzovska Simic, S. Phenolic Compounds Composition of Hypericum perforatum L. Wild-Growing Plants from the Republic of Macedonia. Agric. Conspec. Sci. 2019, 84, 67–75. [Google Scholar]
- Makarova, K.; Sajkowska-Kozielewicz, J.J.; Zawada, K.; Olchowik-Grabarek, E.; Ciach, M.A.; Gogolewski, K.; Dobros, N.; Ciechowicz, P.; Freichels, H.; Gambin, A. Harvest time affects antioxidant capacity, total polyphenol and flavonoid content of Polish St John’s wort’s (Hypericum perforatum L.) flowers. Sci. Rep. 2021, 11, 3989. [Google Scholar] [CrossRef]
- Gibbons, S.; Ohlendorf, B.; Johnsen, I. The genus Hypericum—A valuable resource of anti-Staphylococcal leads. Fitoterapia 2002, 73, 300–304. [Google Scholar] [CrossRef]
- Avato, P.; Raffo, F.; Guglielmi, G.; Vitali, C.; Rosato, A. Extracts from St John’s Wort and their antiMicrobial Activity. Phytother. Res. 2004, 18, 230–232. [Google Scholar] [CrossRef]
- Nazlı, O.; Baygar, T.; Demirci Dönmez, Ç.E.; Dere, Ö.; Uysal, A.İ.; Aksözek, A.; Işık, C.; Aktürk, S. Antimicrobial and antibiofilm activity of polyurethane/Hypericum perforatum extract (PHPE) composite. Bioorg. Chem. 2019, 82, 224–228. [Google Scholar] [CrossRef]
- Irani, M.; Sarmadi, M.; Bernard, F.; Ebrahimi Pour, G.H.; Bazarnov, H.S. Leaves antimicrobial activity of Glycyrrhiza glabra L. Iran. J. Pharm. Res. 2010, 9, 425–428. [Google Scholar]
- Long, D.R.; Mead, J.; Hendricks, J.M.; Hardy, M.E.; Voyich, J.M. 18β-Glycyrrhetinic acid inhibits methicillin-resistant Staphylococcus aureus survival and attenuates virulence gene expression. Antimicrob. Agents Chemother. 2013, 57, 241–247. [Google Scholar] [CrossRef] [Green Version]
- Sultana, S.; Haque, A.; Hamid, K.; Urmi, K.F.; Roy, S. Antimicrobial, Cytotoxic and Antioxidant Activity of methanolic extract of Glycyrrhiza glabra. Agric. Biol. J. N. Am. 2010, 1, 957–960. [Google Scholar] [CrossRef]
- Rodino, S.; Butu, A.; Butu, M.; Cornea, P.C. Comparative studies on antibacterial activity of licorice, elderberry and dandelion. Dig. J. Nanomater. Biostruct. 2015, 10, 947–955. [Google Scholar]
- Gupta, V.K.; Fatima, A.; Faridi, U.; Negi, A.S.; Shanker, K.; Kumar, J.K.; Rahuja, N.; Luqman, S.; Sisodia, B.S.; Saikia, D.; et al. Antimicrobial potential of Glycyrrhiza glabra roots. J. Ethnopharmacol. 2008, 116, 377–380. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Zuckerman, D.M.; Brantley, S.; Sharpe, M.; Childress, K.; Hoiczyk, E.; Pendleton, A.R. Sambucus nigra extracts inhibit infectious bronchitis virus at an early point during replication. BMC Vet. Res. 2014, 10, 24. [Google Scholar] [CrossRef] [Green Version]
- Torabian, G.; Valtchev, P.; Adil, Q.; Dehghani, F. Anti-influenza activity of elderberry (Sambucus nigra). J. Funct. Foods 2019, 54, 353–360. [Google Scholar] [CrossRef]
- Salinas, F.; Vázquez, L.; Gentilini, M.; O’Donohoe, A.; Regueira, E.; Nabaes Jodar, M.S.; Viegas, M.; Michelini, F.; Hermida, G.; Alché, L.; et al. Aesculus hippocastanum L. seed extract shows virucidal and antiviral activities against respiratory syncytial virus (RSV) and reduces lung inflammation in vivo. Antivir. Res. 2019, 164, 1–11. [Google Scholar] [CrossRef]
- Weber, N.D.; Andersen, D.O.; North, J.A.; Murray, B.K.; Lawson, L.D.; Hughes, B.G. In vitro virucidal effects of Allium sativum (Garlic) extract and compounds. Planta Med. 1992, 58, 417–423. [Google Scholar] [CrossRef]
- Alam, K.; Hoq, O.; Uddin, O. Medicinal plant Allium sativum-A Review. J Med. Plants Stud. 2016, 4, 72–79. [Google Scholar]
- Seo, D.J.; Lee, M.; Jeon, S.B.; Park, H.; Jeong, S.; Lee, B.-H.; Choi, C. Antiviral activity of herbal extracts against the hepatitis A virus. Food Control 2017, 72, 9–13. [Google Scholar] [CrossRef]
- Rouf, R.; Uddin, S.; Kumer Sarker, D.; Islam, M.; Ali, E.; Shilpi, J.; Nahar, D.L.; Tiralongo, E.; Sarker, S. Anti-viral potential of garlic (Allium sativum) and it′s organosulfur compounds: A systematic update of pre-clinical and clinical data. Trends Food Sci. Technol. 2020, 104, 219–234. [Google Scholar] [CrossRef]
- De Soyza, A.; Hall, A.J.; Mahenthiralingam, E.; Drevinek, P.; Kaca, W.; Drulis-Kawa, Z.; Stoitsova, S.R.; Toth, V.; Coenye, T.; Zlosnik, J.E.A.; et al. Developing an international Pseudomonas aeruginosa reference panel. MicrobiologyOpen 2013, 2, 1010–1023. [Google Scholar] [CrossRef]
- Samuelsen, A.B. The traditional uses, chemical constituents and biological activities of Plantago major L. A review. J. Ethnopharmacol. 2000, 71, 1–21. [Google Scholar] [CrossRef]
- Zubair, M.; Widén, C.; Renvert, S.; Rumpunen, K. Water and ethanol extracts of Plantago major leaves show anti-inflammatory activity on oral epithelial cells. J. Tradit. Complement. Med. 2019, 9, 169–171. [Google Scholar] [CrossRef] [PubMed]
- Al-Dabbagh, B.; Elhaty, I.; Elhaw, M.; Murali, C.; Almansoori, A.; Awad, B.; Amin, A. Antioxidant and anticancer activities of chamomile (Matricaria recutita L.). BMC Res. Notes 2019, 12, 3. [Google Scholar] [CrossRef] [PubMed]
- Höferl, M.; Wanner, J.; Tabanca, N.; Ali, A.; Gochev, V.; Schmidt, E.; Kaul, V.; Singh, V.; Jirovetz, L. Biological Activity of Matricaria chamomilla Essential Oils of Various Chemotypes. Planta Med. Int. Open 2020, 7, e114–e121. [Google Scholar] [CrossRef]
- Kaur, R.; Kaur, H.; Dhindsa, A.S. Glycyrrhiza glabra: A phytopharmacological review. Int. J. Pharm. Sci. Res. 2013, 4, 2470–2477. [Google Scholar] [CrossRef]
- Wang, L.; Yang, R.; Yuan, B.; Liu, Y.; Liu, C. The antiviral and antimicrobial activities of licorice, a widely-used Chinese herb. Acta Pharm. Sin. B 2015, 5, 310–315. [Google Scholar] [CrossRef] [Green Version]
- Hamad, G.; Elaziz, A.; Hassan, S.; Shalaby, M.; Mohdaly, A. Chemical Composition, Antioxidant, Antimicrobial and Anticancer Activities of Licorice (Glycyrrhiza glabra L.) Root and Its Application in Functional Yoghurt. J. Food Nutr. Res. 2020, 8, 707–715. [Google Scholar] [CrossRef]
- Tomczyk, M.; Latté, K.P. Potentilla-A review of its phytochemical and pharmacological profile. J. Ethnopharmacol. 2009, 122, 184–204. [Google Scholar] [CrossRef]
- Chiang, L.C.; Ng, L.T.; Cheng, P.W.; Chiang, W.; Lin, C.C. Antiviral activities of extracts and selected pure constituents of Ocimum basilicum. Clin. Exp. Pharmacol. Physiol. 2005, 32, 811–816. [Google Scholar] [CrossRef]
- Khalil, A.T.; Khan, I.; Ahmad, K.; Khan, Y.A.; Khan, M.; Khan, M.J. Synergistic antibacterial effect of honey and Herba Ocimi Basilici against some bacterial pathogens. J. Tradit. Chin. Med. 2013, 33, 810–814. [Google Scholar] [CrossRef]
- Osei Akoto, C.; Acheampong, A.; Boakye, Y.; Naazo, A.A.; Adomah, D. Anti-Inflammatory, Antioxidant, and Anthelmintic Activities of Ocimum basilicum (Sweet Basil) Fruits. J. Chem. 2020, 2020, 2153534. [Google Scholar] [CrossRef]
- Oliveira, J.R.D.; de Jesus Viegas, D.; Martins, A.P.R.; Carvalho, C.A.T.; Soares, C.P.; Camargo, S.E.A.; Jorge, A.O.C.; de Oliveira, L.D. Thymus vulgaris L. extract has antimicrobial and anti-inflammatory effects in the absence of cytotoxicity and genotoxicity. Arch. Oral Biol. 2017, 82, 271–279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Catella, C.; Camero, M.; Lucente, M.S.; Fracchiolla, G.; Sblano, S.; Tempesta, M.; Martella, V.; Buonavoglia, C.; Lanave, G. Virucidal and antiviral effects of Thymus vulgaris essential oil on feline coronavirus. Res. Vet. Sci. 2021, 137, 44–47. [Google Scholar] [CrossRef] [PubMed]
- Niksic, H.; Becic, F.; Koric, E.; Gusic, I.; Omeragic, E.; Muratovic, S.; Miladinovic, B.; Duric, K. Cytotoxicity screening of Thymus vulgaris L. essential oil in brine shrimp nauplii and cancer cell lines. Sci. Rep. 2021, 11, 13178. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.M.; Ramu, R.; Shirahatti, P.S.; Shivamallu, C.; Amachawadi, R.G. A systematic review on ethnopharmacology, phytochemistry and pharmacological aspects of Thymus vulgaris Linn. Heliyon 2021, 7, e07054. [Google Scholar] [CrossRef]
- Jakovljević, M.R.; Grujičić, D.; Vukajlović, J.T.; Marković, A.; Milutinović, M.; Stanković, M.; Vuković, N.; Vukić, M.; Milošević-Djordjević, O. In vitro study of genotoxic and cytotoxic activities of methanol extracts of Artemisia vulgaris L. and Artemisia alba Turra. S. Afr. J. Bot. 2020, 132, 117–126. [Google Scholar] [CrossRef]
- Nair, M.S.; Huang, Y.; Fidock, D.A.; Polyak, S.J.; Wagoner, J.; Towler, M.J.; Weathers, P.J. Artemisia annua L. extracts inhibit the in vitro replication of SARS-CoV-2 and two of its variants. J. Ethnopharmacol. 2021, 274, 114016. [Google Scholar] [CrossRef]
- Oyedemi, S.O.; Oyedemi, B.O.; Prieto, J.M.; Coopoosamy, R.M.; Stapleton, P.; Gibbons, S. In vitro assessment of antibiotic-resistance reversal of a methanol extract from Rosa canina L. S. Afr. J. Bot. 2016, 105, 337–342. [Google Scholar] [CrossRef]
- Khazael, M.; Khazael, M.R.; Pazhouhi, M. An overview of therapeutic potentials of Rosa canina: A traditionally valuable herb. WCRJ 2020, 7, e1580. [Google Scholar] [CrossRef]
- Bonaterra, G.; Bronischewski, K.; Hunold, P.; Schwarzbach, H.; Heinrich, E.-U.; Fink, C.; Abdel-Aziz, H.; Müller, J.; Kinscherf, R. Anti-inflammatory and Anti-oxidative Effects of Phytohustil® and Root Extract of Althaea officinalis L. on Macrophages in vitro. Front. Pharmacol. 2020, 11, 290. [Google Scholar] [CrossRef]
- Tahmouzi, S.; Salek Nejat, M.R. New infertility therapy effects of polysaccharides from Althaea officinalis leaf with emphasis on characterization, antioxidant and anti-pathogenic activity. Int. J. Biol. Macromol. 2020, 145, 777–787. [Google Scholar] [CrossRef] [PubMed]
- Owczarek, A.; Kolodziejczyk-czepas, J.; Woźniak-serwata, J.; Magiera, A.; Kobiela, N.; Wąsowicz, K.; Olszewska, M.A. Potential activity mechanisms of aesculus hippocastanum bark: Antioxidant effects in chemical and biological in vitro models. Antioxidants 2021, 10, 995. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, A.I.; Pinho, C.; Sarmento, B.; Dias, A.C.P. Neuroprotective activity of hypericum perforatum and its major components. Front. Plant Sci. 2016, 7, 1004. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aygül, A.; Şerbetçi, T. The antibacterial and antivirulent potential of Hypericum lydium against Staphylococcus aureus: Inhibition of growth, biofilm formation, and hemolytic activity. Eur. J. Integr. Med. 2020, 35, 101139. [Google Scholar] [CrossRef]
- Balouiri, M.; Sadiki, M.; Ibnsouda, S. Methods for in vitro evaluating antimicrobial activity: A review. J. Pharm. Anal. 2016, 6, 71–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reed, L.J.; Muench, H. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 1938, 27, 493–497. [Google Scholar]
| Extract | Δlg | ||||
|---|---|---|---|---|---|
| 15 min | 30 min | 60 min | 90 min | 120 min | |
| A. hippocastani | 1.75 | 2.0 | 2.75 | 3.25 | 3.25 |
| G. glabra | 0.25 | 0.5 | 1.25 | 1.5 | 1.5 |
| O. basilicum | 2.5 | 2.5 | 3.0 | 3.25 | 3.25 |
| A. sativum | 2.5 | 2.5 | 3.0 | 3.25 | 3.5 |
| P. reptans | 2.5 | 2.5 | 3.0 | 3.25 | 3.5 |
| M. chamomilla | 0.5 | 1.5 | 1.25 | 2.0 | 2.75 |
| T. vulgaris | 0.5 | 1.75 | 2.25 | 3.0 | 3.5 |
| A. officinalis | 1.75 | 2.0 | 2.5 | 3.25 | 3.25 |
| R. canina | 1.75 | 2.0 | 2.5 | 3.0 | 3.0 |
| A. annua | 0.5 | 0.5 | 0.5 | 2.0 | 3.0 |
| S. nigra | 0.5 | 1.0 | 1.5 | 1.5 | 1.5 |
| H. perforatum | 1.75 | 2.0 | 2.5 | 3.25 | 3.25 |
| P. lanceolata | 0.5 | 0.5 | 0.5 | 1.5 | 1.5 |
| Extract | Δlg | |||
|---|---|---|---|---|
| 15 min | 30 min | 45 min | 60 min | |
| A. hippocastani | 5.0 | 5.5 | 5.5 | 6.0 |
| G. glabra | 1.0 | 1.75 | 1.75 | 1.75 |
| O. basilicum | 2.5 | 2.5 | 3.0 | 3.5 |
| A. sativum | 1.25 | 1.25 | 2.0 | 2.25 |
| P. reptans | 2.0 | 2.75 | 2.75 | 2.75 |
| M. chamomilla | 2.0 | 2.0 | 2.0 | 2.0 |
| T. vulgaris | 1.5 | 1.75 | 1.75 | 1.75 |
| A. officinalis | 1.0 | 1.0 | 2.0 | 2.0 |
| R. canina | 1.0 | 1.0 | 1.5 | 2.0 |
| A. annua | 1.0 | 1.0 | 1.75 | 1.75 |
| S. nigra | 2.0 | 2.25 | 2.75 | 2.75 |
| H. perforatum | 3.0 | 3.5 | 3.5 | 3.5 |
| P. lanceolata | 1.0 | 1.0 | 1.75 | 1.75 |
| Extract | Δlg | ||||
|---|---|---|---|---|---|
| 15 min | 30 min | 60 min | 90 min | 120 min | |
| A. hippocastani | 3.0 | 3.75 | 4.25 | 5.0 | 5.5 |
| G. glabra | 1.5 | 1.75 | 2.0 | 2.0 | 2.0 |
| O. basilicum | 0.5 | 1.0 | 1.0 | 1.33 | 1.33 |
| A. sativum | 2.0 | 2.25 | 2.25 | 2.5 | 3.0 |
| P. reptans | 1.5 | 1.75 | 1.75 | 2.0 | 2.5 |
| M. chamomilla | 1.5 | 2.0 | 2.0 | 3.0 | 3.0 |
| T. vulgaris | 1.0 | 1.0 | 1.5 | 1.5 | 1.5 |
| A. officinalis | 0 | 0 | 0.5 | 0.5 | 0.5 |
| R. canina | 1.5 | 1.5 | 1.75 | 1.75 | 1.75 |
| A. annua | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| S. nigra | 1.0 | 1.0 | 1.5 | 2.0 | 2.0 |
| H. perforatum | 1.0 | 1.0 | 1.5 | 1.75 | 1.75 |
| P. lanceolata | 1.5 | 1.5 | 2.0 | 2.0 | 2.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nikolova, I.; Paunova-Krasteva, T.; Petrova, Z.; Grozdanov, P.; Nikolova, N.; Tsonev, G.; Triantafyllidis, A.; Andreev, S.; Trepechova, M.; Milkova, V.; et al. Bulgarian Medicinal Extracts as Natural Inhibitors with Antiviral and Antibacterial Activity. Plants 2022, 11, 1666. https://doi.org/10.3390/plants11131666
Nikolova I, Paunova-Krasteva T, Petrova Z, Grozdanov P, Nikolova N, Tsonev G, Triantafyllidis A, Andreev S, Trepechova M, Milkova V, et al. Bulgarian Medicinal Extracts as Natural Inhibitors with Antiviral and Antibacterial Activity. Plants. 2022; 11(13):1666. https://doi.org/10.3390/plants11131666
Chicago/Turabian StyleNikolova, Ivanka, Tsvetelina Paunova-Krasteva, Zdravka Petrova, Petar Grozdanov, Nadya Nikolova, Georgi Tsonev, Alexandros Triantafyllidis, Stoyan Andreev, Madlena Trepechova, Viktoria Milkova, and et al. 2022. "Bulgarian Medicinal Extracts as Natural Inhibitors with Antiviral and Antibacterial Activity" Plants 11, no. 13: 1666. https://doi.org/10.3390/plants11131666
APA StyleNikolova, I., Paunova-Krasteva, T., Petrova, Z., Grozdanov, P., Nikolova, N., Tsonev, G., Triantafyllidis, A., Andreev, S., Trepechova, M., Milkova, V., & Vilhelmova-Ilieva, N. (2022). Bulgarian Medicinal Extracts as Natural Inhibitors with Antiviral and Antibacterial Activity. Plants, 11(13), 1666. https://doi.org/10.3390/plants11131666







