An Insight into Salvia haematodes L. (Lamiaceae) Bioactive Extracts Obtained by Traditional and Green Extraction Procedures
Abstract
:1. Introduction
2. Results and Discussion
2.1. Biological Activity of S. haematodes Extracts
2.2. Medium Pressure Liquid Chromatography (MPLC) Fractionation
3. Materials and Methods
3.1. Chemicals and Reagents
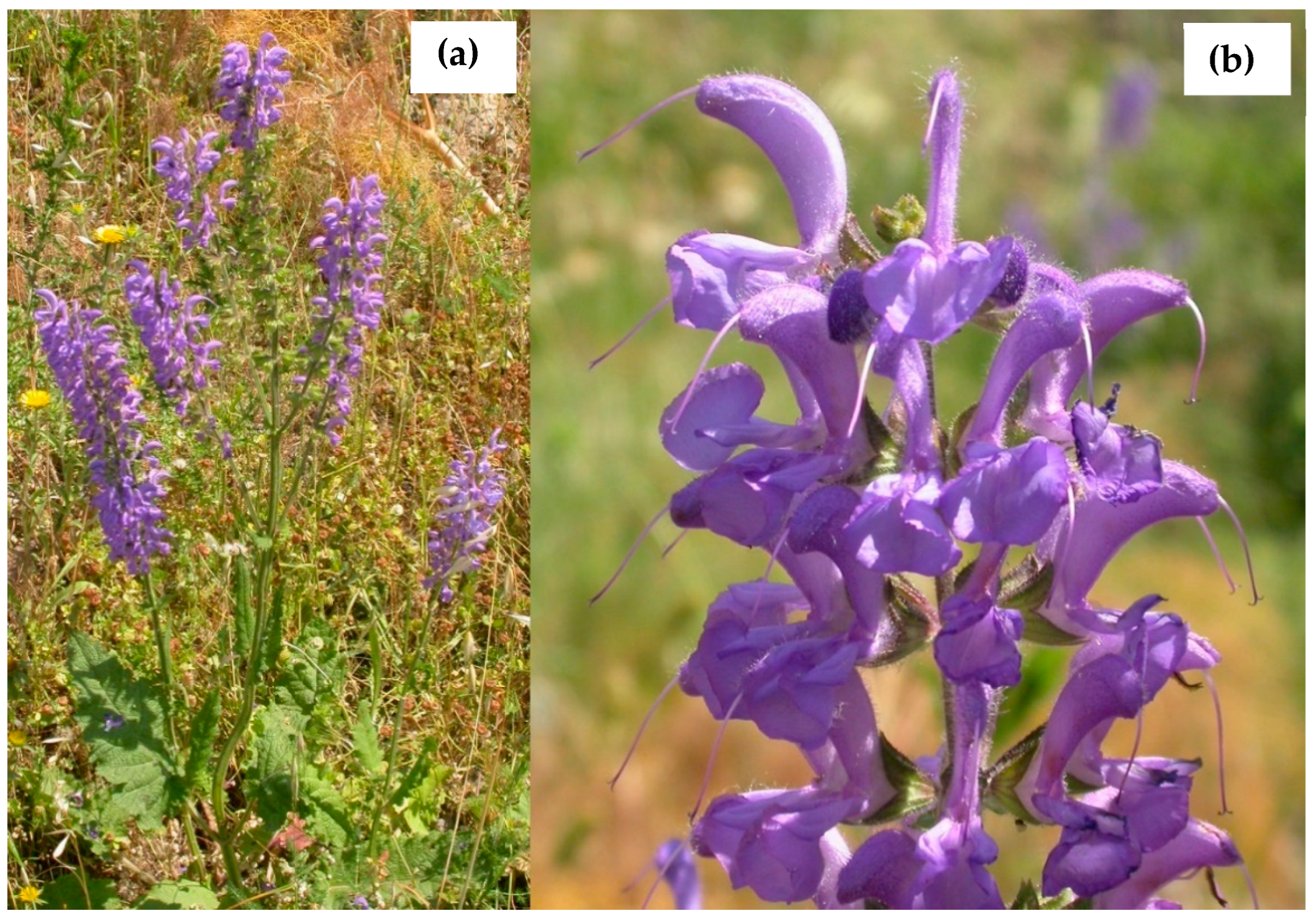
3.2. Plant Materials
3.3. Extraction and Fractionation by Medium Pressure Liquid Chromatography (MPLC)
- (a)
- Soxhlet apparatus (SHS) (conventional glass with an extraction chamber with a diameter of 8 cm and a height of 30 cm, accompanied by a flask of capacity of 1 L; 600 mL, 8 extractive cycles);
- (b)
- extractor Naviglio® (SHN) (Nuova Estrazione S.a.s., Naples, Italy, 2 L capacity model; 30 extractive cycles each of which being 4 min). The combined extractive solutions were evaporated to dryness in vacuo using a rotary evaporator at 35–40 °C.
3.4. Chemical Analysis
3.5. Analysis of Achetylcholinesterase (AChE) and Butyrylcholinesterase (BChE) Inhibitory Activity
3.6. In Vitro Antioxidant Tests
3.7. Statistical Analysis
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bentham, G. Labiatae. In Genera Plantarum; Bentham, G., Hooker, J.D., Eds.; Reeve and Co.: London, UK, 1876; Volume 2, pp. 1160–1196. [Google Scholar]
- Walker, J.B.; Sytsma, K.J.; Treutlein, J.; Wink, M. Salvia (Lamiaceae) is not monophyletic: Implications for the systematics, radiation, and ecological specializations of Salvia and tribe Mentheae. Am. J. Bot. 2004, 91, 1115–1125. [Google Scholar] [CrossRef] [PubMed]
- Pignatti, S.; Guarino, R.; La Rosa, M. Flora d’Italia; Edagricole: Milan, Italy, 2017; Volume 2. [Google Scholar]
- Senatore, F.; De Feo, V. Essential oils from Salvia spp. (Lamiaceae). II. Chemical composition of the essential oil from Salvia pratensis L. su bsp. haematodes (L.) Briq. inflorescences. J. Essent. Oil Res. 1998, 10, 135–137. [Google Scholar] [CrossRef]
- Akbar, S. Pharmacological investigations on the ethanolic extract of Salvia haematodes. Fitoterapia 1989, 60, 270–272. [Google Scholar]
- Akbar, S.; Tariq, M.; Nisa, M. A study on CNS depressant activity of Salvia haematodes Wall. Int. J. Crude Drug Res. 1985, 22, 41–44. [Google Scholar] [CrossRef]
- Loizzo, M.R.; Abouali, M.; Salehi, P.; Sonboli, A.; Kanani, M.; Menichini, F.; Tundis, R. In vitro antioxidant and antiproliferative activities of nine Salvia species. Nat. Prod. Res. 2014, 28, 2278–2285. [Google Scholar] [CrossRef]
- Tundis, R.; Loizzo, M.R.; Menichini, F.; Bonesi, M.; Colica, C.; Menichini, F. In vitro cytotoxic activity of Salvia leriifolia Benth. extract and isolated constituents against a panel of human cancer cell lines. Chem. Biodiv. 2011, 8, 1152–1162. [Google Scholar] [CrossRef] [PubMed]
- Loizzo, M.R.; Tundis, R.; Conforti, F.; Menichini, F.; Bonesi, M.; Nadjafi, F.; Frega, N.G.; Menichini, F. Salvia leriifolia Benth. (Lamiaceae) extract demonstrates in vitro antioxidant properties and cholinesterase inhibitory activity. Nutr. Res. 2010, 30, 823–830. [Google Scholar] [CrossRef] [PubMed]
- Loizzo, M.R.; Menichini, F.; Tundis, R.; Bonesi, M.; Conforti, F.; Nadjafi, F.; Statti, G.A.; Frega, N.G.; Menichini, F. In vitro biological activity of Salvia leriifolia Benth essential oil relevant to the treatment of Alzheimer’s disease. J. Oleo Sci. 2009, 58, 443–446. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tundis, R.; Leporini, M.; Bonesi, M.; Rovito, S.; Passalacqua, N.G. Salvia officinalis L. from Italy: A comparative chemical and biological study of its essential oil in the Mediterranean context. Molecules 2020, 25, 5826. [Google Scholar] [CrossRef] [PubMed]
- Orhan, I.E.; Senol, F.S.; Ercetin, T.; Kahraman, A.; Celep, F.; Akaydin, G.; Sener, B.; Dogan, M. Assessment of anticholinesterase and antioxidant properties of selected sage (Salvia) species with their total phenol and flavonoid contents. Ind. Crops Prod. 2013, 41, 21–30. [Google Scholar] [CrossRef]
- Perry, N.S.L.; Houghton, P.J.; Jenner, P.; Keith, A.; Perry, E.K. Salvia lavandulaefolia essential oil inhibits cholinesterase in vivo. Phytomedicine 2002, 9, 48–51. [Google Scholar] [CrossRef]
- Ibach, B.; Haen, E. Acetylcholinesterase inhibition in Alzheimer’s Disease. Curr. Pharm. Des. 2004, 10, 231–251. [Google Scholar] [CrossRef] [PubMed]
- Marucci, G.; Buccioni, M.; Dal Ben, D.; Lambertucci, C.; Volpini, R.; Amenta, F. Efficacy of acetylcholinesterase inhibitors in Alzheimer’s disease. Neuropharmacology 2021, 190, 108352. [Google Scholar] [CrossRef] [PubMed]
- Perry, E.; McKeith, I.; Ballard, C. Butyrylcholinesterase and progression of cognitive deficits in dementia with Lewy bodies. Neurology 2003, 60, 1852–1853. [Google Scholar] [CrossRef] [PubMed]
- Giacobini, E. Cholinesterase inhibitors for Alzheimer’s disease: From tacrine to future applications. Neurochem. Int. 1998, 32, 413–419. [Google Scholar] [CrossRef]
- Houghton, P.J.; Rena, Y.; Howes, M.-J. Acetylcholinesterase inhibitors from plants and fungi. Nat. Prod. Rep. 2006, 23, 181–199. [Google Scholar] [CrossRef] [PubMed]
- Mamache, W.; Amira, S.; Ben Souici, C.; Laouer, H.; Benchikh, F. In vitro antioxidant, anticholinesterases, anti-α-amylase, and anti-α-glucosidase effects of Algerian Salvia aegyptiaca and Salvia verbenaca. J. Food Biochem. 2020, 44, e13472. [Google Scholar] [CrossRef] [PubMed]
- Topcu, G.; Kolak, U.; Ozturk, M.; Boga, M.; Hatipoglu, S.D.; Bahadori, F.; Culhaoglu, B.; Dirmenci, T. Investigation of Anticholinesterase activity of a series of Salvia extracts and the constituents of Salvia staminea. Nat. Prod. J. 2013, 3, 3–9. [Google Scholar] [CrossRef]
- Perry, G.; Cash, A.D.; Smith, M.A. Alzheimer disease and oxidative stress. J. Biomed. Biotechnol. 2002, 2, 120–123. [Google Scholar] [CrossRef]
- Chen, Z.; Zhong, C. Oxidative stress in Alzheimer’s disease. Neurosci. Bull. 2014, 30, 271–281. [Google Scholar] [CrossRef]
- Miyazawa, M.; Yamafuji, C. Inhibition of acetylcholinesterase activity by tea tree oil and constituent terpenoids. Flavour Fragr. J. 2006, 21, 198–201. [Google Scholar] [CrossRef]
- Bonesi, M.; Menichini, F.; Tundis, R.; Loizzo, M.R.; Conforti, F.; Passalacqua, N.G.; Statti, G.A.; Menichini, F. Acetylcholinesterase and butyrylcholinesterase inhibitory activity of Pinus species essential oils and their constituents. J. Enz. Inhib. Med. Chem. 2010, 25, 622–628. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elufioye, T.O.; Obuotor, E.M.; Agbedahunsi, J.M.; Adesanya, S.A. Anticholinesterase constituents from the leaves of Spondias mombin L. (Anacardiaceae). Biol. Targets Ther. 2017, 11, 107–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karakaya, S.; Yilmaz, S.V.; Özdemir, Ö.; Koca, M.; Pınar, N.M.; Demirci, B.; Yıldırım, K.; Sytar, O.; Hasan Turkez, H.; Baser, K.H.C. A caryophyllene oxide and other potential anticholinesterase and anticancer agent in Salvia verticillata subsp. amasiaca (Freyn & Bornm.) Bornm. (Lamiaceae). J. Essent. Oil Res. 2020, 32, 512–525. [Google Scholar]
- Dalai, M.K.; Bhadra, S.; Chaudhary, S.K.; Bandyopadhyay, A.; Mukherjee, P.K. Anti-cholinesterase activity of the standardized extract of Syzygium aromaticum L. Phcog. Mag. 2014, 10, S276–S282. [Google Scholar] [PubMed] [Green Version]
- Farag, M.A.; Ezzat, S.M.; Salama, M.M.; Tadros, M.G.; Serya, R.A.T. Anti-acetylcholinesterase activity of essential oils and their major constituents from four Ocimum species. Z. Naturforsch. 2016, 71, 393–402. [Google Scholar] [CrossRef] [PubMed]
- Kawamoto, H.; Takeshita, F.; Murata, K. Inhibitory effects of essential oil extracts from Panax plants against β-secretase, cholinesterase, and amyloid aggregation. Nat. Prod. Commun. 2019, 14, 1–7. [Google Scholar] [CrossRef]
- Sharma, N.; Tan, M.A.; An, S.S.A. Phytosterols: Potential metabolic modulators in neurodegenerative diseases. Int. J. Mol. Sci. 2021, 22, 12255. [Google Scholar] [CrossRef]
- Ayaz, M.; Junaid, M.; Ullah, F.; Subhan, F.; Sadiq, A.; Ali, G.; Ovais, M.; Shahid, M.; Ahmad, A.; Wadood, A.; et al. Anti-Alzheimer’s studies on β-sitosterol isolated from Polygonum hydropiper L. Front. Pharmacol. 2017, 8, 697. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baskar, A.A.; Al Numair, K.S.; Gabriel Paulraj, M.; Alsaif, M.A.; Muamar, M.A.; Ignacimuthu, S. β-Sitosterol prevents lipid peroxidation and improves antioxidant status and histoarchitecture in rats with 1,2-dimethylhydrazine-induced colon cancer. J. Med. Food 2012, 15, 335–343. [Google Scholar] [CrossRef]
- Shi, C.; Wu, F.; Zhu, X.; Xu, J. Incorporation of β-sitosterol into the membrane increases resistance to oxidative stress and lipid peroxidation via estrogen receptor-mediated PI3K/GSK3b signaling. Biochim. Biophys. Acta 2013, 1830, 2538–2544. [Google Scholar] [CrossRef] [PubMed]
- Vivancos, M.; Moreno, J.J. β-Sitosterol modulates antioxidant enzyme response in RAW 264.7 macrophages. Free Radic. Biol. Med. 2005, 39, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.; Muhammad Zahoor, M.; Zeb, A.; Sahibzada, M.U.K.; Ul Bari, W.; Naz, S. Isolation, characterization, pharmacological evaluation and in silico modeling of bioactive secondary metabolites from Ziziphus oxyphylla a member of Rhamnaceae family. Trop. J. Pharm. Res. 2020, 19, 351–359. [Google Scholar] [CrossRef]
- Tenuta, M.C.; Deguin, B.; Loizzo, M.R.; Dugay, A.; Acquaviva, R.; Malfa, G.A.; Bonesi, M.; Bouzidi, C.; Tundis, R. Contribution of flavonoids and iridoids to the hypoglycaemic, antioxidant, and nitric oxide (NO) inhibitory activities of Arbutus unedo L. Antioxidants 2020, 9, 184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leporini, M.; Bonesi, M.; Loizzo, M.R.; Passalacqua, N.G.; Tundis, R. The essential oil of Salvia rosmarinus Spenn. from Italy as a source of health-promoting compounds: Chemical profile and antioxidant and cholinesterase inhibitory activity. Plants 2020, 9, 798. [Google Scholar] [CrossRef] [PubMed]
- Lopresti, A.L. Salvia (sage): A review of its potential cognitive-enhancing and protective effects. Drugs R D 2017, 17, 53–64. [Google Scholar] [CrossRef] [Green Version]
| S. haematodes | Extract/Fraction | AChE | BChE | SI # |
|---|---|---|---|---|
| SHN | Total | 396.4 ± 3.4 a | 559.9 ± 5.2 a | 1.4 |
| Methanol | 4.5% # | 33.1% # | - | |
| n-Hexane | 22.9 ± 1.0 a | 408.4 ± 3.8 a | 17.8 | |
| SHS | Total | 249.8 ± 2.7 a | 35.8 ± 0.9 a | 0.1 |
| Methanol | 458.2 ± 4.2 a | 312.1 ± 3.4 a | 0.7 | |
| n-Hexane | 214.2 ± 3.2 a | 30.9 ± 1.1 a | 0.1 | |
| Physostigmine | 0.2 ± 0.02 | 2.4 ± 0.04 | 12 |
| Compound | Class | RI a | SHN | SHS | I.M. b |
|---|---|---|---|---|---|
| Sabinene | MH | 973 | 1.3 ± 0.04 | tr | 1, 2, 3 |
| Eugenol | PH | 1354 | 0.7 ± 0.02 | - | 1, 2 |
| trans-Caryophyllene | SH | 1415 | 7.7 ± 2.3 | 4.6 ± 0.7 | 1, 2, 3 |
| α-Humulene | SH | 1455 | 1.5 ± 0.2 | tr | 1, 2 |
| γ-Muurolene | SH | 1478 | 0.3 ± 0.01 | - | 1, 2 |
| γ-Cadinene | SH | 1515 | 0.4 ± 0.05 | 0.3 ± 0.04 | 1, 2 |
| δ-Cadinene | SH | 1526 | 1.4 ± 0.01 | 0.5 ± 0.06 | 1, 2 |
| Caryophyllene oxide | OS | 1580 | tr | 3.5 ± 1.0 | 1, 2 |
| Neophytadiene | DI | 1837 | 24.9 ± 2.3 | 17.8 ± 1.5 | 1, 2 |
| Phytol | DI | 2111 | 2.5 ± 1.2 | 1.4 ± 0.7 | 1, 2 |
| Methyl myristate | FA | 1726 | 0.9 ± 0.02 | - | 1, 2 |
| Methyl palmitate | FA | 1928 | 1.7 ± 0.3 | 6.7 ± 0.7 | 1, 2 |
| Methyl linoleate | FA | 1996 | 3.1 ± 0.4 | 2.4 ± 0.03 | 1, 2 |
| Methyl heptadecanoate | FA | 2030 | 1.2 ± 0.2 | 1.8 ± 0.1 | 1, 2 |
| Methyl stearate | FA | 2128 | 1.8 ± 0.1 | 3.7 ± 0.1 | 1, 2 |
| Tetradecane | AL | 1400 | 0.7 ± 0.02 | 2.9 ± 0.1 | 1, 2, 3 |
| Heptadecane | AL | 1700 | 0.5 ± 0.03 | tr | 1, 2, 3 |
| Octadecane | AL | 1800 | 0.7 ± 0.01 | 0.4 ± 0.05 | 1, 2, 3 |
| Nonadecane | AL | 1900 | 0.3 ± 0.01 | 3.5 ± 0.5 | 1, 2, 3 |
| Docosane | AL | 2200 | 1.1 ± 0.02 | 1.0 ± 0.06 | 1, 2, 3 |
| Tetracosane | AL | 2400 | 1.2 ± 0.01 | tr | 1, 2, 3 |
| Pentacosane | AL | 2500 | 1.4 ± 0.2 | 8.6 ± 0.7 | 1, 2, 3 |
| Heptacosane | AL | 2700 | 1.8 ± 0.04 | 1.0 ± 0.1 | 1, 2, 3 |
| Octacosane | AL | 2800 | 0.9 ± 0.01 | 1.3 ± 0.01 | 1, 2, 3 |
| Stigmasterol | ST | 17.2 ± 1.5 | 5.4 ± 0.9 | 1, 2 | |
| β-Sitosterol | ST | 20.1 ± 2.1 | 2.3 ± 0.1 | 1, 2 |
| S. haematodes | DPPH Test (IC50 μg/mL) | ABTS Test (IC50 μg/mL) | FRAP Test * (μM Fe(II)/g) | β-Carotene Bleaching Test (IC50 μg/mL) | ||
|---|---|---|---|---|---|---|
| Extract/Fraction | 30 min | 60 min | ||||
| SHN | Total | 0.4 ± 0.07 a | 28.1 ± 1.1 a | 49.6 ± 1.7 a | 5.3 ± 0.05 a | 7.9 ± 0.08 a |
| n-Hexane | 17.9 ± 0.8 a | 81.1 ± 2.8 a | 10.3 ± 0.9 a | 7.7 ± 0.02 | 14.0 ± 0.02 | |
| Methanol | 0.3 ± 0.03 a | 15.6 ± 1.3 a | 70.3 ± 2.8 a | 1.7 ± 0.09 a | 1.6 ± 1.5 a | |
| SHS | Total | 1.2 ± 0.02 b | 42.1 ± 1.9 a | 48.7 ± 1.7 a | 2.9 ± 0.05 a | 2.6 ± 0.05 |
| n-Hexane | 41.9 ± 1.6 a | 220.5 ± 2.5 a | 1.2 ± 0.05 a | 2.8 ± 0.03 a | 2.9 ± 0.07 c | |
| Methanol | 0.9 ± 0.04 b | 18.0 ± 0.9 a | 58.7 ± 1.2 b | 2.7 ± 0.02 a | 2.5 ± 0.04 | |
| Ascorbic acid | 5.2 ± 0.8 | 1.2 ± 0.03 | - | |||
| BHT | - | - | 63.4 ± 4.5 | |||
| Propyl gallate | 1.3 ± 0.04 | 1.2 ± 0.03 | ||||
| S. haematodes Methanol Fraction | TPC a | TFC b | TFC/TPC |
|---|---|---|---|
| SHN | 55.2 ± 1.3 | 36.5 ± 1.0 | 0.7 |
| SHS | 29.0 ± 1.1 | 7.2 ± 0.5 | 0.2 |
| S. haematodes | Fraction | AChE | BChE | SI |
|---|---|---|---|---|
| SHN | N1 | 40.2 ± 1.5 a | 61.5 ± 1.6 a | 1.5 |
| N2 | 180.7 ± 4.2 a | 166.3 ± 2.4 a | 0.9 | |
| N3 | 62.1 ± 2.6 a | 73.9 ± 2.2 a | 1.2 | |
| N4 | 564.9 ± 3.4 a | 129.8 ± 2.5 a | 0.2 | |
| N5 | 115.2 ± 1.8 a | 52.7 ± 1.3 a | 0.5 | |
| N6 | 408.6 ± 3.5 a | 53.9 ± 1.6 a | 0.1 | |
| N7 | 141.9 ± 2.8 a | 55.9 ± 1.5 a | 0.3 | |
| N8 | 110.0 ± 2.0 a | 31.5 ± 1.0 a | 0.3 | |
| N9 | 39.5 ± 1.2 a | 43.4 ± 1.1 a | 1.1 | |
| SHS | S1 | 40.4 ± 1.1 a | 112.6 ± 2.4 a | 2.8 |
| S2 | 114.4 ± 3.1 a | 51.4 ± 1.1 a | 0.4 | |
| S3 | 90.9 ± 2.2 a | 82.2 ± 1.4 a | 0.9 | |
| S4 | 418.7 ± 3.6 a | 207.7 ± 4.4 a | 0.5 | |
| S5 | 444.8 ± 3.9 a | 167.0 ± 3.5 a | 0.4 | |
| S6 | 458.7 ± 3.7 a | 110.1 ± 1.2 a | 0.2 | |
| S7 | 307.8 ± 2.8 a | 173.8 ± 4.0 a | 0.6 | |
| Physostigmine | 0.2 ± 0.02 | 2.4 ± 0.04 | 12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tundis, R.; Passalacqua, N.G.; Bonesi, M.; Loizzo, M.R. An Insight into Salvia haematodes L. (Lamiaceae) Bioactive Extracts Obtained by Traditional and Green Extraction Procedures. Plants 2022, 11, 781. https://doi.org/10.3390/plants11060781
Tundis R, Passalacqua NG, Bonesi M, Loizzo MR. An Insight into Salvia haematodes L. (Lamiaceae) Bioactive Extracts Obtained by Traditional and Green Extraction Procedures. Plants. 2022; 11(6):781. https://doi.org/10.3390/plants11060781
Chicago/Turabian StyleTundis, Rosa, Nicodemo Giuseppe Passalacqua, Marco Bonesi, and Monica Rosa Loizzo. 2022. "An Insight into Salvia haematodes L. (Lamiaceae) Bioactive Extracts Obtained by Traditional and Green Extraction Procedures" Plants 11, no. 6: 781. https://doi.org/10.3390/plants11060781
APA StyleTundis, R., Passalacqua, N. G., Bonesi, M., & Loizzo, M. R. (2022). An Insight into Salvia haematodes L. (Lamiaceae) Bioactive Extracts Obtained by Traditional and Green Extraction Procedures. Plants, 11(6), 781. https://doi.org/10.3390/plants11060781









