The Lack of Standardization and Pharmacological Effect Limits the Potential Clinical Usefulness of Phytosterols in Benign Prostatic Hyperplasia
Abstract
1. Introduction
2. Phytosterols—Characteristics
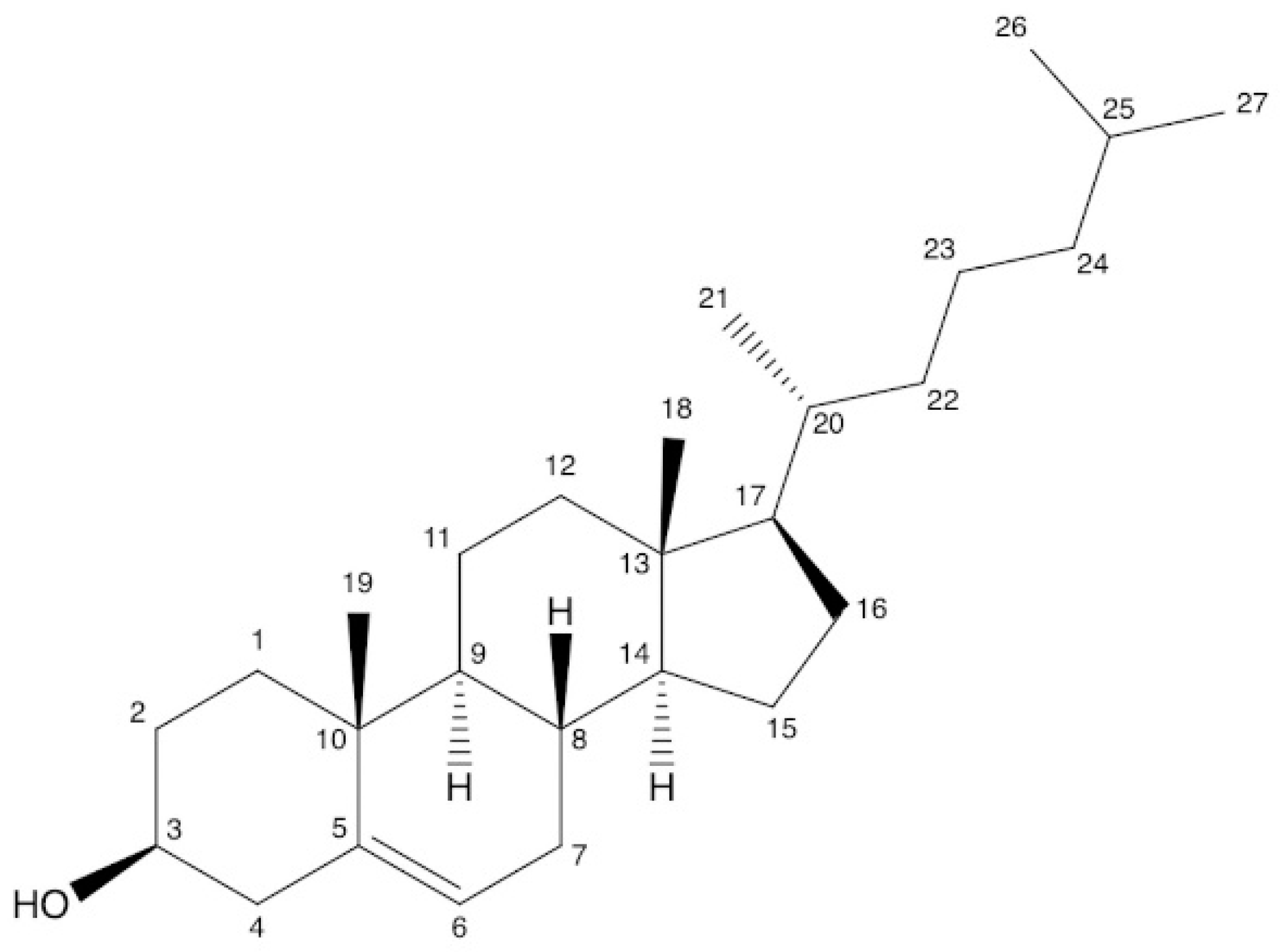
2.1. Chemical Properties of Plant Sterols
2.2. Sources of Plant Sterols
3. Phytosterols—Beneficial Effects in BPH
3.1. Pathophysiology of Benign Prostatic Hyperplasia
3.2. Molecular Mechanism of PSs in BPH Development
- Anti-androgenic effect of phytosterols in BPH
- Phytosterols as anti-inflammatory and antioxidant dietary components in BPH
- Apoptotic effect of phytosterols in BPH
3.3. Phytosterols in BPH—Clinical Evidence
| Type of Study and Subjects | Treatment | Outcomes | Ref. |
|---|---|---|---|
| RCT patients with HBP (n = 200). Duration: 6 months | SIT (20 mg, which contains a mixture of PS), three times/day or placebo | Significant improvement in symptoms score and urinary flow parameters | [102] |
| RCT patients with HBP (n = 117) Duration: 18 months | SIT (20 mg, which contains a mixture of PS), three times/day or placebo | The effects on QOL of SIT are maintained over at least 18 months in men with symptomatic BPH | [103] |
| RCT patients with HBP (n = 177) Duration: 6 months | SIT (130 mg) and placebo | SIT is an effective option in the treatment of BPH. | [104] |
| Single-site study Randomization: noted but method not described (n = 62) Duration: 6 months | SIT (0,15 mg) and placebo | No improvements | [107] |
| Single-site study Randomization: unclear (n = 80) Duration: 1 month | SIT (65 mg) and placebo | SIT is an effective option in the treatment of BPH | [108] |
| RCT mild-to-moderate BPH symptoms (n = 99) Duration: 3 months | Saw palmetto oil (3% SIT), Saw palmetto oil (0.2% SIT) and placebo | Efficacy of SIT enriched saw palmetto oil is superior to conventional oil | [109] |
4. Regulatory Framework and Agreement with Label Declaration
5. Analysis of Phytosterols in Dietary Supplements
5.1. Sample Preparation
5.2. Determination Methods
- Gas Chromatography
- High-performance Liquid Chromatography
| Method | Detector | Sample Preparation/Extraction | Analytical Methods | Target Compounds | Ref. |
|---|---|---|---|---|---|
| GC | FID |
| Column: (25m × 0.25mm, 0,33 μm, Dimethylpolysiloxane stationary phase) Temperatures (°C): Detector: 325; Injector: 325 Gas (mL/min): Helium (0.5) Injection type: Split ratio, 1:40 Injection volume (μL): 1 | campesterol stigmasterol SIT total sterols | [118] |
| GC | FID/MS |
| Column: (30 m × 0.32 mm, 0.25 μm, (poly (94%methyl/5% phenyl) silicone)) Temperatures (°C): column 250, injector 290, detector 290 Gas (mL/min): H2 (1) Injection type Split ratio, 1:25 Injection volume (μL): 1 | campesterol stigmasterol SIT | [22] |
| GC | FID |
| Column: (30 m × 0.32 mm, 0.25 μm) (5%-phenyl)-methylpolysiloxane stationary phase)/(30 m × 0.32 mm, 0.25 μm, (5%-phenyl) (1%-vinyl)-methylpolysiloxane stationary phase) Temperatures (°C): column 250, Injector 290, detector 290 Gas (mL/min): H2 (1) Injection type Split ratio, 1:25 Injection volume (μL): 1 | 17 phytosterols | [138] |
| GC | FID/MS |
| Column: (15 m × 0.32-mm,0.25 μm/5% diphenyl-95%-Dimethylpolysiloxane) Temperatures (°C): column 270, injector 280, detector 300. Gas (ml/min): helium (0.58) Injector type: split ratio, 17:1 Injection volume (μL): 0.5 | SIT β-sitosteryl glucoside (BSSG) | [139] |
| GC | FID |
| Column: (25 m × 0.32 mm, 17 μm/5% phenyl-methylsilicone or methyl silicone gum stationary phase) Temperatures (°C): Column 190→255, injector: 250, detector: 300 Gas (mL/min): helium 2/15/3; makeup helium 20/hydrogen 35/air 380 Injection volume (μL): 1 | Campesterol Stigmasterol SIT | [119] |
| GC | FID/MS |
| Column: (60 m × 0.25 mm, 0.25 um/5% phenyl methyl siloxane stationary phase) Temperatures (°C): column 80→325, detector 230. Gas (mL/min): helium (1) Injection volume (μL): 1 | campesterol stigmasterol SIT total sterols | [120] |
| LC | APCI–MS |
| 1. Column: phenyl (150 mm × 3.9 mm, 3,5 μm) Mobile phase: 58% acetonitrile, 42% water Flow rate (mL/min): 1.1 (isocratic) 2. Column: ACE C18 (150 mm × 3.0 mm, 3 μm) Mobile phase: 90% methanol, 10% water Flow rate (mL/min): 0.80 (isocratic) Injection volume (μL): 5 for qualitative, 10 for quantitative measurement | campesterol, cycloartenol, lupenone, lupeol, SIT, and stigmasterol (Standard Reference Materials containing saw palmetto) | [39] |
| HPLC | ESI-MS |
| Column: C18 (250 × 3.0 mm, 5 μm) Mobile phase: 95% methanol: 5% water Flow rate (mL/min): 0.5 (isocratic) | campesterol stigmasterol β-sitosterol | [141] |
| HPLC | UV |
| Column: RP-18 (125-4 mm, 5 μm) Mobile phase: hexane, propan-1-ol (99.5:0.5; v/v) Flow rate (mL/min): 0.8−1 (isocratic) Injection volume (μL): 50 UV detection: 212 nm | β-sitosterol | [142] |
| UHPLC | UV/CAD |
| Column: (100 × 2.1 mm, 1,7 μm) Phenyl-hexyl Mobile phase: acetonitrile: water Flow rate (mL/min): 0.9 (gradient) Temperature: 60 °C Inj. vol. (μL): 2 Run time (min): 8.5 | ergosterol, brassicasterol, campesterol, campestanol, fucosterol, stigmasterol, stigmastanol, SIT esterified form | [122] |
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wei, J.T.; Calhoun, E.; Jacobsen, S.J. Urologic diseases in America project: Benign prostatic hyperplasia. J. Urol. 2005, 173, 1256–1261. [Google Scholar] [CrossRef] [PubMed]
- Parsons, J.K.; Bergstrom, J.; Silberstein, J.; Barrett-Connor, E. Prevalence and characteristics of lower urinary tract symptoms in men aged > or =80 years. Urology 2008, 72, 318–321. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.H.; Lim, H.J.; Kim, M.S.; Lee, M.S. Dietary supplements for benign prostatic hyperplasia: An overview of systematic reviews. Maturitas 2012, 73, 180–185. [Google Scholar] [CrossRef]
- Eleazu, C.; Eleazu, K.; Kalu, W. Management of Benign Prostatic Hyperplasia: Could Dietary Polyphenols Be an Alternative to Existing Therapies? Front. Pharmacol. 2017, 8, 234. [Google Scholar] [CrossRef]
- Fogaing, C.; Alsulihem, A.; Campeau, L.; Corcos, J. Is Early Surgical Treatment for Benign Prostatic Hyperplasia Preferable to Prolonged Medical Therapy: Pros and Cons. Medicina 2021, 57, 368. [Google Scholar] [CrossRef] [PubMed]
- Peng, Z.F.; Zhou, J.; Song, P.; Yang, L.C.; Yang, B.; Ren, Z.J.; Wang, L.C.; Wei, Q.; Dong, Q. Retrospective analysis of the changes in the surgical treatment of benign prostatic hyperplasia during an 11-year period: A single-center experience. Asian J. Androl. 2021, 23, 294–299. [Google Scholar] [CrossRef]
- Tarter, T.H.; Vaughan, E.D., Jr. Inhibitors of 5alpha-reductase in the treatment of benign prostatic hyperplasia. Curr. Pharm. Des. 2006, 12, 775–783. [Google Scholar] [CrossRef]
- Kim, E.H.; Brockman, J.A.; Andriole, G.L. The use of 5-alpha reductase inhibitors in the treatment of benign prostatic hyperplasia. Asian J. Urol. 2018, 5, 28–32. [Google Scholar] [CrossRef]
- Azzouni, F.; Godoy, A.; Li, Y.; Mohler, J. The 5 alpha-reductase isozyme family: A review of basic biology and their role in human diseases. Adv. Urol. 2012, 2012, 530121. [Google Scholar] [CrossRef]
- Kim, J.H.; Baek, M.J.; Sun, H.Y.; Lee, B.; Li, S.; Khandwala, Y.; Del Giudice, F.; Chung, B.I. Efficacy and safety of 5 alpha-reductase inhibitor monotherapy in patients with benign prostatic hyperplasia: A meta-analysis. PLoS ONE 2018, 13, e0203479. [Google Scholar] [CrossRef]
- Gormley, G.J.; Stoner, E.; Bruskewitz, R.C.; Imperato-McGinley, J.; Walsh, P.C.; McConnell, J.D.; Andriole, G.L.; Geller, J.; Bracken, B.R.; Tenover, J.S. The effect of finasteride in men with benign prostatic hyperplasia. The Finasteride Study Group. N. Engl. J. Med. 1992, 327, 1185–1191. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.H.; Larson, J.A.; Andriole, G.L. Management of Benign Prostatic Hyperplasia. Annu. Rev. Med. 2016, 67, 137–151. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, S.A.; Lee, J.Y.; Meehan, A.G.; Kusek, J.W. Time Course of Incident Adverse Experiences Associated with Doxazosin, Finasteride and Combination Therapy in Men with Benign Prostatic Hyperplasia: The MTOPS Trial. J. Urol. 2016, 195, 1825–1829. [Google Scholar] [CrossRef]
- Roehrborn, C.G.; Boyle, P.; Nickel, J.C.; Hoefner, K.; Andriole, G. Efficacy and safety of a dual inhibitor of 5-alpha-reductase types 1 and 2 (dutasteride) in men with benign prostatic hyperplasia. Urology 2002, 60, 434–441. [Google Scholar] [CrossRef]
- Mysore, V. Finasteride and sexual side effects. Indian Dermatol. Online J. 2012, 3, 62–65. [Google Scholar] [CrossRef]
- The National Institutes of Health (NIH). Dietary Supplement Label Database. Available online: https://dsld.od.nih.gov/search/prostate/bWFya2V0X3N0YXR1cz1hbGwvZW50cnlfZGF0ZT0yMDExLDwMjIv c29ydD1tYXR jaC9wYWdlX3NpemU9MjAvcGFnZV9pbmRleD0xLw (accessed on 7 February 2022).
- Leisegang, K.; Jimenez, M.; Durairajanayagam, D.; Finelli, R.; Majzoub, A.; Henkel, R.; Agarwal, A. A Systematic Review of Herbal Medicine in the Clinical Treatment of Benign Prostatic Hyperplasia. Phytomedicine 2022, 2, 100153. [Google Scholar] [CrossRef]
- Wilt, T.J.; Ishani, A.; Rutks, I.; MacDonald, R. Phytotherapy for benign prostatic hyperplasia. Public Health Nutr. 2000, 3, 459–472. [Google Scholar] [CrossRef]
- Csikós, E.; Horváth, A.; Ács, K.; Papp, N.; Balázs, V.L.; Dolenc, M.S.; Kenda, M.; Kočevar Glavač, N.; Nagy, M.; Protti, M.; et al. Treatment of Benign Prostatic Hyperplasia by Natural Drugs. Molecules 2021, 26, 7141. [Google Scholar] [CrossRef]
- Hosbas Coskun, S.; Wise, S.A.; Kuszak, A.J. The Importance of Reference Materials and Method Validation for Advancing Research on the Health Effects of Dietary Supplements and Other Natural Products. Front. Nutr. 2021, 8, 786261. [Google Scholar] [CrossRef]
- Bot, A. Phytosterols. In Encyclopedia of Food Chemistry; Melton, L., Shahidi, F., Varelis, P., Eds.; Academic Press: Oxford, UK, 2019; pp. 225–228. [Google Scholar] [CrossRef]
- Srigley, C.T.; Haile, E.A. Quantification of Plant Sterols/Stanols in Foods and Dietary Supplements Containing Added Phytosterols. J. Food Compost. Anal. 2015, 40, 163–176. [Google Scholar] [CrossRef]
- Lagarda, M.J.; García-Llatas, G.; Farré, R. Analysis of phytosterols in foods. J. Pharm. Biomed. Anal. 2006, 41, 1486–1496. [Google Scholar] [CrossRef] [PubMed]
- García-Llatas, G.; Rodríguez-Estrada, M.T. Current and New Insights on Phytosterol Oxides in Plant Sterol-Enriched. Food. Chem. Phys. Lipids 2011, 164, 607–624. [Google Scholar] [CrossRef] [PubMed]
- Moreau, R.A.; Whitaker, B.D.; Hicks, K.B. Phytosterols, phytostanols, and their conjugates in foods: Structural diversity, quantitative analysis, and health-promoting uses. Prog. Lipid. Res. 2022, 41, 457–500. [Google Scholar] [CrossRef] [PubMed]
- Moreau, R.A.; Nyström, L.; Whitaker, B.D.; Winkler-Moser, J.K.; Baer, D.J.; Gebauer, S.K.; Hicks, K.B. Phytosterols and Their Derivatives: Structural Diversity, Distribution, Metabolism, Analysis, and Health-Promoting Uses. Prog. Lipid Res. 2018, 70, 35–61. [Google Scholar] [CrossRef] [PubMed]
- Daels, E.; Foubert, I.; Goderis, B. The effect of adding a commercial phytosterol ester mixture on the phase behavior of palm oil. Food Res. Int. 2017, 100 Pt 1, 841–849. [Google Scholar] [CrossRef]
- Davidson, M.H.; Maki, K.C.; Umporowicz, D.M.; Ingram, K.A.; Dicklin, M.R.; Schaefer, E.; Lane, R.W.; McNamara, J.R.; Ribaya-Mercado, J.D.; Perrone, G.; et al. Safety and tolerability of esterified phytosterols administered in reduced-fat spread and salad dressing to healthy adult men and women. Am. Coll. Nutr. 2001, 20, 307–319. [Google Scholar] [CrossRef]
- Mussner, M.J.; Parhofer, K.G.; Von Bergmann, K.; Schwandt, P.; Broedl, U.; Otto, C. Effects of phytosterol ester-enriched margarine on plasma lipoproteins in mild to moderate hypercholesterolemia are related to basal cholesterol and fat intake. Metabolism 2002, 51, 189–194. [Google Scholar] [CrossRef]
- Kwak, H.S.; Ahn, H.J.; Ahn, J. Development of Phytosterol Ester-Added Cheddar Cheese for Lowering Blood Cholesterol. Asian-Australas J. Anim. Sci. 2005, 18, 267–276. [Google Scholar] [CrossRef]
- Piironen, V.; Lindsay, D.G.; Miettinen, T.A.; Toivo, J.; Lampi, A.-M. Plant sterols: Biosynthesis, biological function and their importance to human nutrition. J. Sci. Food Agric. 2000, 80, 939–966. [Google Scholar] [CrossRef]
- Normén, L.; Bryngelsson, S.; Johnsson, M.; Evheden, P.; Ellegård, L.; Brants, H.; Andersson, H.; Dutta, P. The Phytosterol Content of Some Cereal Foods Commonly Consumed in Sweden and in the Netherlands. J. Food Compos. Anal. 2002, 15, 693–704. [Google Scholar] [CrossRef]
- Othman, R.A.; Myrie, S.B.; Jones, P.J. Non-cholesterol sterols and cholesterol metabolism in sitosterolemia. Atherosclerosis 2013, 231, 291–299. [Google Scholar] [CrossRef]
- Piironen, V.; Lampi, A.M. Phytosterols as Functional Food Components and Nutraceuticals; Dutta, P.C., Ed.; Marcel Dekker, Inc.: New York, NY, USA, 2004; pp. 1–32. [Google Scholar]
- Martins, C.M.; Fonseca, F.A.; Ballus, C.A.; Figueiredo-Neto, A.M.; Meinhart, A.D.; de Godoy, H.T.; Izar, M.C. Common sources and composition of phytosterols and their estimated intake by the population in the city of São Paulo, Brazil. Nutrition 2013, 29, 865–871. [Google Scholar] [CrossRef]
- Yang, R.; Xue, L.; Zhang, L.; Wang, X.; Qi, X.; Jiang, J.; Yu, L.; Wang, X.; Zhang, W.; Zhang, Q.; et al. Phytosterol Contents of Edible Oils and Their Contributions to Estimated Phytosterol Intake in the Chinese Diet. Foods 2019, 8, 334. [Google Scholar] [CrossRef] [PubMed]
- Nair, P.P.; Turjman, N.; Kessie, G.; Calkins, B.; Goodman, G.T.; Davidovitz, H.; Nimmagadda, G. Diet, nutrition intake, and metabolism in populations at high and low risk for colon cancer. Dietary cholesterol, beta-sitosterol, and stigmasterol. Am. J. Clin. Nutr. 1984, 40 (Suppl. S4), 927–930. [Google Scholar] [CrossRef]
- Geavlete, P.; Multescu, R.; Geavlete, B. Serenoa repens extract in the treatment of benign prostatic hyperplasia. Ther. Adv. Urol. 2011, 3, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Bedner, M.; Schantz, M.M.; Sander, L.C.; Sharpless, K.E. Development of liquid chromatographic methods for the determination of phytosterols in Standard Reference Materials containing saw palmetto. J. Chromatogr. A 2008, 1192, 74–80. [Google Scholar] [CrossRef]
- Schauer, I.G.; Rowley, D.R. The functional role of reactive stroma in benign prostatic hyperplasia. Differentiation 2011, 82, 200–210. [Google Scholar] [CrossRef] [PubMed]
- Vickman, R.E.; Franco, O.E.; Moline, D.C.; Vander Griend, D.J.; Thumbikat, P.; Hayward, S.W. The role of the androgen receptor in prostate development and benign prostatic hyperplasia: A review. Asian J. Urol. 2020, 7, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Pizzorno, J.E.; Murray, M.T.; Joiner-Bey, H. 12—Benign Prostatic Hyperplasia. In The Clinician’s Handbook of Natural Medicine, 3rd ed.; Pizzorno, J.E., Murray, M.T., Joiner-Bey, H., Eds.; Churchill Livingstone: Edinburgh, UK, 2016; pp. 137–146. [Google Scholar] [CrossRef]
- Gao, W.; Bohl, C.E.; Dalton, J.T. Chemistry and structural biology of androgen receptor. Chem. Rev. 2005, 105, 3352–3370. [Google Scholar] [CrossRef]
- Kalu, W.O.; Okafor, P.N.; Ijeh, I.I.; Eleazu, C. Effect of kolaviron, a biflavanoid complex from Garcinia kola on some biochemical parameters in experimentally induced benign prostatic hyperplasic rats. Biomed. Pharmacother. 2016, 83, 1436–1443. [Google Scholar] [CrossRef]
- Ajayi, A.; Abraham, K. Understanding the Role of Estrogen in the Development of Benign Prostatic Hyperplasia. Afr. J. Urol. 2018, 24, 93–97. [Google Scholar] [CrossRef]
- Miwa, Y.; Kaneda, T.; Yokoyama, O. Association Between Lower Urinary Tract Symptoms and Serum Levels of Sex Hormones in Men. Urology 2008, 72, 552–555. [Google Scholar] [CrossRef]
- Ellem, S.J.; Risbridger, G.P. The dual, opposing roles of estrogen in the prostate. Ann. N. Y. Acad. Sci. 2009, 1155, 174–186. [Google Scholar] [CrossRef] [PubMed]
- McPherson, S.J.; Hussain, S.; Balanathan, P.; Hedwards, S.L.; Niranjan, B.; Grant, M.; Chandrasiri, U.P.; Toivanen, R.; Wang, Y.; Taylor, R.A.; et al. Estrogen receptor-beta activated apoptosis in benign hyperplasia and cancer of the prostate is androgen independent and TNFalpha mediated. Proc. Natl. Acad. Sci. USA 2010, 107, 3123–3128. [Google Scholar] [CrossRef]
- Robert, G.; Descazeaud, A.; Nicolaïew, N.; Terry, S.; Sirab, N.; Vacherot, F.; Maillé, P.; Allory, Y.; de la Taille, A. Inflammation in benign prostatic hyperplasia: A 282 patients’ immunohistochemical analysis. Prostate 2009, 69, 1774–1780. [Google Scholar] [CrossRef]
- Chughtai, B.; Lee, R.; Te, A.; Kaplan, S. Role of inflammation in benign prostatic hyperplasia. Rev. Urol. 2011, 13, 147–150. [Google Scholar]
- Latil, A.; Pétrissans, M.T.; Rouquet, J.; Robert, G.; de la Taille, A. Effects of hexanic extract of Serenoa repens (Permixon® 160 mg) on inflammation biomarkers in the treatment of lower urinary tract symptoms related to benign prostatic hyperplasia. Prostate 2015, 75, 1857–1867. [Google Scholar] [CrossRef]
- Nickel, J.C.; Roehrborn, C.G.; O’Leary, M.P.; Bostwick, D.G.; Somerville, M.C.; Rittmaster, R.S. The relationship between prostate inflammation and lower urinary tract symptoms: Examination of baseline data from the REDUCE trial. Eur. Urol. 2008, 54, 1379–1384. [Google Scholar] [CrossRef]
- Kirschenbaum, A.; Klausner, A.P.; Lee, R.; Unger, P.; Yao, S.; Liu, X.-H.; Levine, A.C. Expression of Cyclooxygenase-1 and Cyclooxygenase-2 in the Human Prostate. Urology 2000, 56, 671–676. [Google Scholar] [CrossRef] [PubMed]
- Hudson, C.N.; He, K.; Pascal, L.E.; Liu, T.; Myklebust, L.K.; Dhir, R.; Srivastava, P.; Yoshimura, N.; Wang, Z.; Ricke, W.A.; et al. Increased COX-1 expression in benign prostate epithelial cells is triggered by mitochondrial dysfunction. Am. J. Clin. Exp. Urol. 2022, 10, 234–245. [Google Scholar] [PubMed]
- Bonkhoff, H. Estrogen receptor signaling in prostate cancer: Implications for carcinogenesis and tumor progression. Prostate 2018, 78, 2–10. [Google Scholar] [CrossRef]
- Di Silverio, F.; Gentile, V.; De Matteis, A.; Mariotti, G.; Giuseppe, V.; Antonio Luigi, P.; Sciarra, A. Distribution of Inflammation, Pre-Malignant Lesions, Incidental Carcinoma in Histologically Confirmed Benign Prostatic Hyperplasia: A Retrospective Analysis. Eur. Urol. 2003, 43, 164–175. [Google Scholar] [CrossRef] [PubMed]
- Minciullo, P.L.; Inferrera, A.; Navarra, M.; Calapai, G.; Magno, C.; Gangemi, S. Oxidative stress in benign prostatic hyperplasia: A systematic review. Urol. Int. 2015, 94, 249–254. [Google Scholar] [CrossRef]
- Winner, K.; Polycarp, O.; Ifeoma, I.; Chinedum, E. Effect of Fractions of Kolaviron on Some Indices of Benign Prostatic Hyperplasia in Rats: Identification of the Constituents of the Bioactive Fraction Using GC-MS. RSC Adv. 2016, 6, 94352–94360. [Google Scholar] [CrossRef]
- Cabeza, M.; Bratoeff, E.; Heuze, I.; Ramírez, E.; Sánchez, M.; Flores, E. Effect of beta-sitosterol as inhibitor of 5 alpha-reductase in hamster prostate. Proc. West. Pharmacol. Soc. 2003, 46, 153–155. [Google Scholar]
- Kamei, H.; Noguchi, K.; Matsuda, H.; Murata, K. Screening of Euphorbiaceae Plant Extracts for Anti-5α-reductase. Biol. Pharm. Bull. 2018, 41, 1307–1310. [Google Scholar] [CrossRef]
- Lesuisse, D.; Berjonneau, J.; Ciot, C.; Devaux, P.; Doucet, B.; Gourvest, J.F.; Khemis, B.; Lang, C.; Legrand, R.; Lowinski, M.; et al. Determination of oenothein B as the active 5-alpha-reductase-inhibiting principle of the folk medicine Epilobium parviflorum. J. Nat. Prod. 1996, 59, 490–492. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, R.W.; Mark, M.; Soldati, F. Inhibition of 5 α-reductase and aromatase by PHL-00801 (Prostatonin®), a combination of PY102 (Pygeum africanum) and UR102 (Urtica dioica) extracts. Phytomedicine 1996, 3, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Heim, S.; Seibt, S.; Stier, H.; Moré, M.I. Uromedic® Pumpkin Seed Derived Δ7-Sterols, Extract and Oil Inhibit 5α-Reductases and Bind to Androgen Receptor in Vitro. Pharm. Pharmacol. 2018, 9, 193–207. [Google Scholar] [CrossRef]
- Iehlé, C.; Délos, S.; Guirou, O.; Tate, R.; Raynaud, J.P.; Martin, P.M. Human prostatic steroid 5 alpha-reductase isoforms--a comparative study of selective inhibitors. J. Steroid Biochem. Mol. Biol. 1995, 54, 273–279. [Google Scholar] [CrossRef]
- Anderson, L. European Union Herbal Monograph on Serenoa repens (W. Bartram) Small, Fructus; Committee on Herbal Medicinal Products: London, UK, 2015. [Google Scholar]
- Nahata, A.; Dixit, V.K. Evaluation of 5α-reductase inhibitory activity of certain herbs useful as antiandrogens. Andrologia 2014, 46, 592–601. [Google Scholar] [CrossRef]
- Kang, X.C.; Chen, T.; Zhou, J.L.; Shen, P.Y.; Dai, S.H.; Gao, C.Q.; Zhang, J.Y.; Xiong, X.Y.; Liu, D.B. Phytosterols in hull-less pumpkin seed oil, rich in ∆7-phytosterols, ameliorate benign prostatic hyperplasia by lowing 5α-reductase and regulating balance between cell proliferation and apoptosis in rats. Food Nutr. Res. 2021, 65. [Google Scholar] [CrossRef] [PubMed]
- Nattagh-Eshtivani, E.; Barghchi, H.; Pahlavani, N.; Barati, M.; Amiri, Y.; Fadel, A.; Khosravi, M.; Talebi, S.; Arzhang, P.; Ziaei, R.; et al. Biological and pharmacological effects and nutritional impact of phytosterols: A comprehensive review. Phytother. Res. 2022, 36, 299–322. [Google Scholar] [CrossRef]
- Umetani, M.; Shaul, P. 27-Hydroxycholesterol: The first identified endogenous SERM. Trends Endocrinol. Metab. 2011, 22, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, L.B.; Shefer, S.; Salen, G.; Tint, S.G.; Batta, A.K. Competitive inhibition of hepatic sterol 27-hydroxylase by sitosterol: Decreased activity in sitosterolemia. Proc. Assoc. Am. Physicians 1998, 110, 32–39. [Google Scholar]
- Song, L.; Qu, D.; Zhang, Q.; Jiang, J.; Zhou, H.; Jiang, R.; Li, Y.; Zhang, Y.; Yan, H. Phytosterol esters attenuate hepatic steatosis in rats with non-alcoholic fatty liver disease rats fed a high-fat diet. Sci. Rep. 2017, 7, 41604. [Google Scholar] [CrossRef]
- Kim, K.A.; Lee, I.A.; Gu, W.; Hyam, S.R.; Kim, D.H. β-Sitosterol attenuates high-fat diet-induced intestinal inflammation in mice by inhibiting the binding of lipopolysaccharide to toll-like receptor 4 in the NF-κB pathway. Mol. Nutr. Food Res. 2014, 58, 963–972. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Zhang, L.; Joo, D.; Sun, S.C. NF-κB signaling in inflammation. Signal Transduct. Target Ther. 2017, 2, 17023. [Google Scholar] [CrossRef]
- Liao, P.C.; Lai, M.H.; Hsu, K.P.; Kuo, Y.H.; Chen, J.; Tsai, M.C.; Li, C.X.; Yin, X.J.; Jeyashoke, N.; Chao, L.K. Identification of β-Sitosterol as In Vitro Anti-Inflammatory Constituent in Moringa oleifera. J. Agric. Food Chem. 2018, 66, 10748–10759. [Google Scholar] [CrossRef]
- Kasirzadeh, S.; Ghahremani, M.H.; Setayesh, N.; Jeivad, F.; Shadboorestan, A.; Taheri, A.; Beh-Pajooh, A.; Azadkhah Shalmani, A.; Ebadollahi-Natanzi, A.; Khan, A.; et al. β-Sitosterol Alters the Inflammatory Response in CLP Rat Model of Sepsis by Modulation of NF-κB Signaling. Biomed. Res. Int. 2021, 2021, 5535562. [Google Scholar] [CrossRef]
- Yang, G.; An, H.J. β-sitosteryl-3-O-β-glucopyranoside isolated from the bark of Sorbus commixta ameliorates pro-inflammatory mediators in RAW 264.7 macrophages. Immunopharmacol. Immunotoxicol. 2014, 36, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Yuan, L.; Zhang, F.; Shen, M.; Jia, S.; Xie, J. Phytosterols Suppress Phagocytosis and Inhibit Inflammatory Mediators via ERK Pathway on LPS-Triggered Inflammatory Responses in RAW264.7 Macrophages and the Correlation with Their Structure. Foods 2019, 8, 582. [Google Scholar] [CrossRef] [PubMed]
- Sudeep, H.V.; Venkatakrishna, K.; Amrutharaj, B.; Anitha; Shyamprasad, K. A phytosterol-enriched saw palmetto supercritical CO2 extract ameliorates testosterone-induced benign prostatic hyperplasia by regulating the inflammatory and apoptotic proteins in a rat model. BMC Complement. Altern. Med. 2019, 19, 270. [Google Scholar] [CrossRef]
- Hamid, A.R.; Umbas, R.; Mochtar, C.A. Recent role of inflammation in prostate diseases: Chemoprevention development opportunity. Acta. Med. Indones. 2011, 43, 59–65. [Google Scholar]
- Hussain, T.; Tan, B.; Yin, Y.; Blachier, F.; Tossou, M.C.; Rahu, N. Oxidative Stress and Inflammation: What Polyphenols Can Do for Us? Oxid. Med. Cell. Longev. 2016, 2016, 7432797. [Google Scholar] [CrossRef]
- Ștefănescu, R.; Farczadi, L.; Huțanu, A.; Ősz, B.E.; Mărușteri, M.; Negroiu, A.; Vari, C.E. Tribulus terrestris Efficacy and Safety Concerns in Diabetes and Erectile Dysfunction, Assessed in an Experimental Model. Plants 2021, 10, 744. [Google Scholar] [CrossRef] [PubMed]
- Salehi, B.; Quispe, C.; Sharifi-Rad, J.; Cruz-Martins, N.; Nigam, M.; Mishra, A.P.; Konovalov, D.A.; Orobinskaya, V.; Abu-Reidah, I.M.; Zam1, W.; et al. Phytosterols: From Preclinical Evidence to Potential Clinical Applications. Front. Pharmacol. 2021, 11, 599959. [Google Scholar] [CrossRef] [PubMed]
- Van Rensburg, S.J.; Daniels, W.M.; van Zyl, J.M.; Taljaard, J.J. A comparative study of the effects of cholesterol, beta-sitosterol, beta-sitosterol glucoside, dehydroepiandrosterone sulphate and melatonin on in vitro lipid peroxidation. Metab. Brain. Dis. 2000, 15, 257–265. [Google Scholar] [CrossRef]
- Chen, Z.; Wu, A.; Jin, H.; Liu, F. β-Sitosterol attenuates liver injury in a rat model of chronic alcohol intake. Arch. Pharm. Res. 2020, 43, 1197–1206. [Google Scholar] [CrossRef]
- International, B.R. Retracted: Apoptosis and Molecular Targeting Therapy in Cancer. Biomed. Res. Int. 2020, 2020, 2451249. [Google Scholar] [CrossRef]
- Megyesi, J.; Tarcsafalvi, A.; Seng, N.; Hodeify, R.; Price, P.M. Cdk2 phosphorylation of Bcl-xL after stress converts it to a pro-apoptotic protein mimicking Bax/Bak. Cell Death Discov. 2016, 2, 15066. [Google Scholar] [CrossRef]
- Minutoli, L.; Rinaldi, M.; Marini, H.; Irrera, N.; Crea, G.; Lorenzini, C.; Puzzolo, D.; Valenti, A.; Pisani, A.; Adamo, E.B.; et al. Apoptotic Pathways Linked to Endocrine System as Potential Therapeutic Targets for Benign Prostatic Hyperplasia. Int. J. Mol. Sci. 2016, 17, 1311. [Google Scholar] [CrossRef]
- Kyprianou, N.; Tu, H.; Jacobs, S.C. Apoptotic versus proliferative activities in human benign prostatic hyperplasia. Hum. Pathol. 1996, 27, 668–675. [Google Scholar] [CrossRef]
- Rodríguez-Berriguete, G.; Fraile, B.; de Bethencourt, F.R.; Prieto-Folgado, A.; Bartolome, N.; Nuñez, C.; Prati, B.; Martínez-Onsurbe, P.; Olmedilla, G.; Paniagua, R.; et al. Role of IAPs in prostate cancer progression: Immunohistochemical study in normal and pathological (benign hyperplastic, prostatic intraepithelial neoplasia and cancer) human prostate. BMC Cancer 2010, 10, 18. [Google Scholar] [CrossRef]
- Minutoli, L.; Altavilla, D.; Marini, H.; Rinaldi, M.; Irrera, N.; Pizzino, G.; Bitto, A.; Arena, S.; Cimino, S.; Squadrito, F.; et al. Inhibitors of apoptosis proteins in experimental benign prostatic hyperplasia: Effects of serenoa repens, selenium and lycopene. J. Biomed. Sci. 2014, 21, 19. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Liu, H.T. MAPK signal pathways in the regulation of cell proliferation in mammalian cells. Cell Res. 2002, 12, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Ohtsuka, T.; Buchsbaum, D.; Oliver, P.; Makhija, S.; Kimberly, R.; Zhou, T. Synergistic induction of tumor cell apoptosis by death receptor antibody and chemotherapy agent through JNK/p38 and mitochondrial death pathway. Oncogene 2003, 22, 2034–2044. [Google Scholar] [CrossRef] [PubMed]
- Davis, R.J. Signal transduction by the JNK group of MAP kinases. Cell 2000, 103, 239–252. [Google Scholar] [CrossRef]
- Yue, J.; López, J.M. Understanding MAPK Signaling Pathways in Apoptosis. Int. J. Mol. Sci. 2020, 21, 2346. [Google Scholar] [CrossRef]
- Papatsoris, A.G.; Papavassiliou, A.G. Molecular ‘palpation’ of BPH: A tale of MAPK signalling? Trends Mol. Med. 2001, 7, 288–292. [Google Scholar] [CrossRef]
- Ropiquet, F.; Giri, D.; Lamb, D.J.; Ittmann, M. FGF7 and FGF2 are increased in benign prostatic hyperplasia and are associated with increased proliferation. J. Urol. 1999, 162, 595–599. [Google Scholar] [CrossRef]
- Carson, C.; Rittmaster, R. The role of dihydrotestosterone in benign prostatic hyperplasia. Urology 2003, 61 (Suppl. S1), 2–7. [Google Scholar] [CrossRef]
- Wells, A.; Gupta, K.; Chang, P.; Swindle, S.; Glading, A.; Shiraha, H. Epidermal growth factor receptor-mediated motility in fibroblasts. Microsc. Res. Tech. 1998, 43, 395–411. [Google Scholar] [CrossRef]
- Ahel, J.; Hudorović, N.; Vičić-Hudorović, V.; Nikles, H. Tgf-beta in the natural history of prostate cancer. Acta Clin Croat. 2019, 58, 128–138. [Google Scholar] [CrossRef] [PubMed]
- Pugazhenthi, S.; Nesterova, A.; Sable, C.; Heidenreich, K.A.; Boxer, L.M.; Heasley, L.E.; Reusch, J.E. Akt/protein kinase B up-regulates Bcl-2 expression through cAMP-response element-binding protein. J. Biol. Chem. 2000, 275, 10761–10766. [Google Scholar] [CrossRef] [PubMed]
- Von Holtz, R.L.; Fink, C.S.; Awad, A.B. beta-Sitosterol activates the sphingomyelin cycle and induces apoptosis in LNCaP human prostate cancer cells. Nutr. Cancer. 1998, 32, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Berges, R.R.; Windeler, J.; Trampisch, H.J.; Senge, T. Randomised, placebo-controlled, double-blind clinical trial of beta-sitosterol in patients with benign prostatic hyperplasia. Beta-sitosterol Study Group. Lancet 1995, 345, 1529–1532. [Google Scholar] [CrossRef] [PubMed]
- Berges, R.R.; Kassen, A.; Senge, T. Treatment of symptomatic benign prostatic hyperplasia with beta-sitosterol: An 18-month follow-up. BJU Int. 2000, 85, 842–846. [Google Scholar] [CrossRef]
- Klippel, K.F.; Hiltl, D.M.; Schipp, B. A multicentric, placebo-controlled, double-blind clinical trial of beta-sitosterol (phytosterol) for the treatment of benign prostatic hyperplasia. German BPH-Phyto Study group. Br. J. Urol. 1997, 80, 427–432. [Google Scholar] [CrossRef]
- Wilt, T.; Ishani, A.; MacDonald, R.; Stark, G.; Mulrow, C.; Lau, J. Beta-sitosterols for benign prostatic hyperplasia. Cochrane Database Syst. Rev. 2000, 1999, CD001043. [Google Scholar] [CrossRef]
- Coleman, C.I.; Hebert, J.H.; Reddy, P. The effect of phytosterols on quality of life in the treatment of benign prostatic hyperplasia. Pharmacotherapy 2002, 22, 1426–1432. [Google Scholar] [CrossRef]
- Kadow, C.; Abrams, P.H. A double-blind trial of the effect of beta-sitosteryl glucoside (WA184) in the treatment of benign prostatic hyperplasia. Eur. Urol. 1986, 12, 187–189. [Google Scholar] [CrossRef]
- Fischer, A.; Jurincic-Winkler, C.D.; Klippel, K.F. Conservative treatment of benign prostatic hyperplasia with high-dosage b-sitosterol (65 mg): Results of a placebo-controlled double-blind study. Uroscopy 1993, 1, 12–20. [Google Scholar]
- Sudeep, H.V.; Thomas, J.V.; Shyamprasad, K. A double blind, placebo-controlled randomized comparative study on the efficacy of phytosterol-enriched and conventional saw palmetto oil in mitigating benign prostate hyperplasia and androgen deficiency. BMC Urol. 2020, 20, 86. [Google Scholar] [CrossRef] [PubMed]
- Commission Regulation (EC) No 608/2004 of 31 March 2004. Concerning the Labelling of Foods and Food Ingredients with Added Phytosterols, Phytosterol Esters, Phytostanols and/or Phytostanol Esters (Text with EEA Relevance). 2004, 97. Available online: http://data.europa.eu/eli/reg/2004/608/oj/eng (accessed on 16 February 2023).
- Ling, W.H.; Jones, P.J. Dietary phytosterols: A review of metabolism, benefits and side effects. Life Sci. 1995, 57, 195–206. [Google Scholar] [CrossRef]
- Hendriks, H.F.; Brink, E.J.; Meijer, G.W.; Princen, H.M.; Ntanios, F.Y. Safety of long-term consumption of plant sterol esters-enriched spread. Eur. J. Clin. Nutr. 2003, 57, 681–692. [Google Scholar] [CrossRef] [PubMed]
- Perini, M.; Paolini, M.; Camin, F.; Appendino, G.; Vitulo, F.; De Combarieu, E.; Sardone, N.; Martinelli, E.M.; Pace, R. Combined use of isotopic fingerprint and metabolomics analysis for the authentication of saw palmetto (Serenoa repens) extracts. Fitoterapia 2018, 127, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Saw Palmetto Extract|USP-NF. Available online: https://www.uspnf.com/official-text/revision-bulletins/saw-palmetto-extract (accessed on 16 February 2023).
- European Pharmacopoeia 10.0|PDF|Chemistry|Pharmaceutical. Available online: https://ro.scribd.com/document/508063535/European-Pharmacopoeia-10-0 (accessed on 16 February 2023).
- Dreikorn, K. The role of phytotherapy in treating lower urinary tract symptoms and benign prostatic hyperplasia. World J. Urol. 2002, 19, 426–435. [Google Scholar] [CrossRef]
- Giammarioli, S.; Boniglia, C.; Di Stasio, L.; Gargiulo, R.; Mosca, M.; Carratù, B. Phytosterols in supplements containing Serenoa repens: An example of variability of active principles in commercial plant-based products. Nat. Prod. Res. 2019, 33, 2257–2261. [Google Scholar] [CrossRef]
- Kim, K.C.; Choi, M.-J.; Kim, K.-M.; Hill, W.S.; Dohnalek, M.; Davis, S.; Jung, J.-C. Analysis of Serenoa repens Extracts on Korean Market and Their Comparison to USP Saw Palmetto Extract Standards. Food Suppl. Biomater. Health 2021, 1, e26. [Google Scholar] [CrossRef]
- Sorenson, W.R.; Sullivan, D. Determination of campesterol, stigmasterol, and beta-sitosterol in saw palmetto raw materials and dietary supplements by gas chromatography: Collaborative study. J AOAC Int. 2007, 90, 670–678. [Google Scholar] [CrossRef] [PubMed]
- Penugonda, K.; Lindshield, B.L. Fatty Acid and Phytosterol Content of Commercial Saw Palmetto Supplements. Nutrients 2013, 5, 3617–3633. [Google Scholar] [CrossRef]
- Sorenson, W.R.; Sullivan, D. Determination of campesterol, stigmasterol, and beta-sitosterol in saw palmetto raw materials and dietary supplements by gas chromatography: Single-laboratory validation. J AOAC Int. 2006, 89, 22–34. [Google Scholar] [CrossRef] [PubMed]
- Fibigr, J.; Šatínský, D.; Solich, P. A UHPLC method for the rapid separation and quantification of phytosterols using tandem UV/Charged aerosol detection—A comparison of both detection techniques. J. Pharm. Biomed. Anal. 2017, 140, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Duong, S.; Strobel, N.; Buddhadasa, S.; Stockham, K.; Auldist, M.; Wales, B.; Orbell, J.; Cran, M. Rapid measurement of phytosterols in fortified food using gas chromatography with flame ionization detection. Food Chem. 2016, 211, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Du, M.; Ahn, D.U. Simultaneous Analysis of Tocopherols, Cholesterol, and Phytosterols Using Gas Chromatography. J. Food Sci. 2002, 67, 1696–1700. [Google Scholar] [CrossRef]
- Vu, D.C.; Lei, Z.; Sumner, L.W.; Coggeshall, M.V.; Lin, C.-H. Identification and Quantification of Phytosterols in Black Walnut Kernels. J. Food. Compost. Anal. 2019, 75, 61–69. [Google Scholar] [CrossRef]
- Zhang, T.; Wang, T.; Liu, R.; Chang, M.; Jin, Q.; Wang, X. Chemical Characterization of Fourteen Kinds of Novel Edible Oils: A Comparative Study Using Chemometrics. LWT 2020, 118, 108725. [Google Scholar] [CrossRef]
- Alvarez-Sala, A.; Garcia-Llatas, G.; Cilla, A.; Barberá, R.; Sánchez-Siles, L.M.; Lagarda, M.J. Impact of Lipid Components and Emulsifiers on Plant Sterols Bioaccessibility from Milk-Based Fruit Beverages. J. Agric. Food Chem. 2016, 64, 5686–5691. [Google Scholar] [CrossRef]
- Hamdan, I.J.A.; Claumarchirant, L.; Garcia-Llatas, G.; Alegría, A.; Lagarda, M.J. Sterols in infant formulas: Validation of a gas chromatographic method. Int. J. Food Sci. Nutr. 2017, 68, 695–703. [Google Scholar] [CrossRef]
- Wang, M.; Zhang, L.; Wu, X.; Zhao, Y.; Wu, L.; Lu, B. Quantitative Determination of Free and Esterified Phytosterol Profile in Nuts and Seeds Commonly Consumed in China by SPE/GC–MS. LWT 2019, 100, 355–361. [Google Scholar] [CrossRef]
- Claassen, F.W.; van de Haar, C.; van Beek, T.A.; Dorado, J.; Martinez-Inigo, M.J.; Sierra-Alvarez, R. Rapid Analysis of Apolar Low Molecular Weight Constituents in Wood Using High Pressure Liquid Chromatography with Evaporative Light Scattering Detection. Phytochem. Anal. 2000, 11, 251–256. [Google Scholar] [CrossRef]
- Abidi, S.L. Chromatographic analysis of plant sterols in foods and vegetable oils. J. Chromatogr. A 2001, 935, 173–201. [Google Scholar] [CrossRef]
- De Monte, C.; Carradori, S.; Granese, A.; Di Pierro, G.B.; Leonardo, C.; De Nunzio, C. Modern extraction techniques and their impact on the pharmacological profile of Serenoa repens extracts for the treatsment of lower urinary tract symptoms. BMC Urol. 2014, 14, 63. [Google Scholar] [CrossRef]
- Islam, M.A.; Jeong, B.-G.; Kerr, W.L.; Chun, J. Validation of Phytosterol Analysis by Alkaline Hydrolysis and Trimethylsilyl Derivatization Coupled with Gas Chromatography for Rice Products. J. Cereal Sci. 2021, 101, 103305. [Google Scholar] [CrossRef]
- Feng, S.; Wang, L.; Belwal, T.; Li, L.; Luo, Z. Phytosterols Extraction from Hickory (Carya Cathayensis Sarg.) Husk with a Green Direct Citric Acid Hydrolysis Extraction Method. Food Chem. 2020, 315, 126217. [Google Scholar] [CrossRef] [PubMed]
- Feng, S.; Liu, S.; Luo, Z.; Tang, K. Direct saponification preparation and analysis of free and conjugated phytosterols in sugarcane (Saccharum officinarum L.) by reversed-phase high-performance liquid chromatography. Food Chem. 2015, 181, 9–14. [Google Scholar] [CrossRef]
- Standard Methods for the Analysis of Oils, Fats and Derivatives—6th Edition. Available online: https://www.elsevier.com/books/standard-methods-for-the-analysis-of-oils-fats-and-derivatives/paquot/978-0-08-022379-7 (accessed on 17 February 2023).
- Srigley, C.T.; Hansen, S.L.; Smith, S.A.; Abraham, A.; Bailey, E.; Chen, X.; Chooi, S.H.; Clement, L.M.; Dao, M.; Fardin Kia, A.R.; et al. Sterols and Stanols in Foods and Dietary Supplements Containing Added Phytosterols: A Collaborative Study. J. Am. Oil Chem. Soc. 2018, 95, 247–257. [Google Scholar] [CrossRef]
- Phillips, K.M.; Ruggio, D.M.; Ashraf-Khorassani, M. Analysis of Steryl Glucosides in Foods and Dietary Supplements by Solid-Phase Extraction and Gas Chromatography. J. Food Lipids 2005, 12, 124–140. [Google Scholar] [CrossRef]
- Sherma, J.; Rabel, F. Review of Advances in Planar Chromatography-Mass Spectrometry Published in the Period 2015–2019. J. Liq. Chromatogr. Relat. 2020, 43, 394–412. [Google Scholar] [CrossRef]
- Lu, B.; Zhang, Y.; Wu, X.; Shi, J. Separation and determination of diversiform phytosterols in food materials using supercritical carbon dioxide extraction and ultraperformance liquid chromatography-atmospheric pressure chemical ionization-mass spectrometry. Anal. Chim. Acta 2007, 588, 50–63. [Google Scholar] [CrossRef] [PubMed]
- Nzekoue, F.K.; Caprioli, G.; Ricciutelli, M.; Cortese, M.; Alesi, A.; Vittori, S.; Sagratini, G. Development of an Innovative Phytosterol Derivatization Method to Improve the HPLC-DAD Analysis and the ESI-MS Detection of Plant Sterols/Stanols. Int. Food Res. J. 2020, 131, 108998. [Google Scholar] [CrossRef]
- Hryniewicka, M.; Starczewska, B.; Tkaczuk, N. Simple Approach Based on Ultrasound-Assisted Emulsification Microextraction for Determination of β-Sitosterol in Dietary Supplements and Selected Food Products. Microchem. J. 2020, 155, 104775. [Google Scholar] [CrossRef]
- Shah, U.M.; Patel, S.M.; Patel, P.H.; Hingorani, L.; Jadhav, R.B. Development and Validation of a Simple Isocratic HPLC Method for Simultaneous Estimation of Phytosterols in Cissus quadrangularis. Indian J. Pharm. Sci. 2010, 72, 753–758. [Google Scholar] [CrossRef]
- Özdemir, İ.S.; Dağ, Ç.; Özinanç, G.; Suçsoran, Ö.; Ertaş, E.; Bekiroğlu, S. Quantification of Sterols and Fatty Acids of Extra Virgin Olive Oils by FT-NIR Spectroscopy and Multivariate Statistical Analyses. LWT 2018, 91, 125–132. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, Y.; Xia, Z.; Wang, Y.; Wu, Y.; Gong, Z. Rapid Determination of Phytosterols by NIRS and Chemometric Methods. Spectrochim. Acta Part A Spectrochim. Acta. A Mol. Biomol. Spectrosc. 2019, 211, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Llatas, G.; Alegría, A.; Barberá, R.; Cilla, A. Current Methodologies for Phytosterol Analysis in Foods. Microchem. J. 2021, 168, 106377. [Google Scholar] [CrossRef]
- Gomes Silva, M.; Santos, V.S.; Fernandes, G.D.; Calligaris, G.A.; Santana, M.H.A.; Cardoso, L.P.; Ribeiro, A.P.B. Physical approach for a quantitative analysis of the phytosterols in free phytosterol-oil blends by X-ray Rietveld method. Int. Food Res. J. 2019, 124, 2–15. [Google Scholar] [CrossRef] [PubMed]
- Nisca, A.; Ștefănescu, R.; Stegăruș, D.I.; Mare, A.D.; Farczadi, L.; Tanase, C. Phytochemical Profile and Biological Effects of Spruce (Picea abies) Bark Subjected to Ultrasound Assisted and Microwave-Assisted Extractions. Plants 2021, 10, 870. [Google Scholar] [CrossRef]
- Lee, J.H.; Lee, K.; Jun, S.H.; Song, S.H.; Shin, C.H.; Song, J. A Multiplex Phytosterol Assay Utilizing Gas Chromatography-Mass Spectrometry for Diagnosis of Inherited Lipid Storage Disorders. Ann. Lab. Med. 2019, 39, 411–413. [Google Scholar] [CrossRef]
- Almeling, S.; Ilko, D.; Holzgrabe, U. Charged Aerosol Detection in Pharmaceutical Analysis. J. Pharm. Biomed. Anal. 2012, 69, 50–63. [Google Scholar] [CrossRef]
- Viinamäki, J.; Ojanperä, I. Photodiode Array to Charged Aerosol Detector Response Ratio Enables Comprehensive Quantitative Monitoring of Basic Drugs in Blood by Ultra-High Performance Liquid Chromatography. Anal. Chim. Acta 2015, 865, 1–7. [Google Scholar] [CrossRef]
- Laakso, P. Analysis of Sterols from Various Food Matrices. Eur. J. Lipid Sci. Technol. 2005, 107, 402–410. [Google Scholar] [CrossRef]
- Clement, L.M.; Hansen, S.L.; Costin, C.D.; Perri, G.L. Quantitation of Sterols and Steryl Esters in Fortified Foods and Beverages by GC/FID. J. Am. Oil Chem. Soc. 2010, 87, 973–980. [Google Scholar] [CrossRef]
- Careri, M.; Elviri, L.; Mangia, A. Liquid Chromatography–UV Determination and Liquid Chromatography–Atmospheric Pressure Chemical Ionization Mass Spectrometric Characterization of Sitosterol and Stigmasterol in Soybean Oil. J. Chromatogr. A 2001, 935, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Maguire, L.S.; O’Sullivan, S.M.; Galvin, K.; O’Connor, T.P.; O’Brien, N.M. Fatty acid profile, tocopherol, squalene and phytosterol content of walnuts, almonds, peanuts, hazelnuts and the macadamia nut. Int. J. Food Sci. Nutr. 2004, 55, 171–178. [Google Scholar] [CrossRef]
- Yuan, C.; Ju, Y.; Jin, R.; Ren, L.; Liu, X. Simultaneous HPLC–DAD Analysis of Tocopherols, Phytosterols, and Squalene in Vegetable Oil Deodorizer Distillates. Chromatographia 2015, 78, 273–278. [Google Scholar] [CrossRef]
- Sedbare, R.; Raudone, L.; Zvikas, V.; Viskelis, J.; Liaudanskas, M.; Janulis, V. Development and Validation of the UPLC-DAD Methodology for the Detection of Triterpenoids and Phytosterols in Fruit Samples of Vaccinium macrocarpon Aiton and Vaccinium oxycoccos L. Molecules 2022, 27, 4403. [Google Scholar] [CrossRef]
- Acworth, I.N.; Bailey, B.; Plante, M.; Gamache, P. Simple and Direct Analysis of Phytosterols in Red Palm Oil by Reverse Phase HPLC and Charged Aerosol Detection. Planta Med. 2011, 77, PA2. [Google Scholar] [CrossRef]
- Nair, V.D.; Kanfer, I.; Hoogmartens, J. Determination of stigmasterol, beta-sitosterol and stigmastanol in oral dosage forms using high performance liquid chromatography with evaporative light scattering detection. J. Pharm. Biomed. Anal. 2006, 41, 731–737. [Google Scholar] [CrossRef]
- Slavin, M.; Yu, L. A Single Extraction and HPLC Procedure for Simultaneous Analysis of Phytosterols, Tocopherols and Lutein in Soybeans. Food Chem. 2012, 135, 2789–2795. [Google Scholar] [CrossRef]
- Ito, M.; Ishimaru, M.; Shibata, T.; Hatate, H.; Tanaka, R. High-Performance Liquid Chromatography with Fluorescence Detection for Simultaneous Analysis of Phytosterols (Stigmasterol, β-Sitosterol, Campesterol, Ergosterol, and Fucosterol) and Cholesterol in Plant Foods. Food Anal. Methods 2017, 10, 2692–2699. [Google Scholar] [CrossRef]
- Horník, S.; Sajfrtová, M.; Karban, J.; Sýkora, J.; Březinová, A.; Wimmer, Z. LC-NMR Technique in the Analysis of Phytosterols in Natural Extracts. J. Anal. Methods Chem. 2013, 2013, 526818. [Google Scholar] [CrossRef] [PubMed]
- Gachumi, G.; El-Aneed, A. Mass Spectrometric Approaches for the Analysis of Phytosterols in Biological Samples. J. Agric. Food Chem. 2017, 65, 10141–10156. [Google Scholar] [CrossRef]
- Cañabate-Díaz, B.; Segura Carretero, A.; Fernández-Gutiérrez, A.; Belmonte Vega, A.; Garrido Frenich, A.; Martínez Vidal, J.L.; Duran Martos, J. Separation and Determination of Sterols in Olive Oil by HPLC-MS. Food Chem. 2007, 102, 593–598. [Google Scholar] [CrossRef]
- Baila-Rueda, L.; Cenarro, A.; Cofán, M.; Orera, I.; Barcelo-Batllori, S.; Pocoví, M.; Ros, E.; Civeira, F.; Nerín, C.; Domeño, C. Simultaneous Determination of Oxysterols, Phytosterols and Cholesterol Precursors by High Performance Liquid Chromatography Tandem Mass Spectrometry in Human Serum. Anal. Methods 2013, 5, 2249–2257. [Google Scholar] [CrossRef]
- Sánchez-Machado, D.I.; López-Hernández, J.; Paseiro-Losada, P.; López-Cervantes, J. An HPLC method for the quantification of sterols in edible seaweeds. Biomed. Chromatogr. 2004, 18, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Peters, F.T.; Remane, D. Aspects of Matrix Effects in Applications of Liquid Chromatography–Mass Spectrometry to Forensic and Clinical Toxicology—A Review. Anal. Bioanal. Chem. 2012, 403, 2155–2172. [Google Scholar] [CrossRef]



| Molecules | Sample | IC50 μg/mL | Ref. |
|---|---|---|---|
| Sitosterol Finasteride | standardized extract standard | 1.1 0.003 | [59] |
| Stigmasterol | Phyllanthus urinaria, extract from the whole plant | 11.2 | [60] |
| Plant extract with PSs content | |||
| Serenoa repens | whole plant | 25–2200 | [65] |
| Epilobium parviflorum | stem and leaves | 160 | [61] |
| Pygeum africanum | standardized extract | 780 | [62] |
| Curcubita pepo | pupmkin seed oil and soft extract | 5880 | [63] |
| Urtica dioica | standardized extract | 14,700 | [62] |
| Phytosterols Percentage of Sterol in Total Extract % (w/w) | ||||
|---|---|---|---|---|
| β-Sitosterol | Stigmasterol | Campesterol | Total Sterols | References |
| 0.030–0.200 | 0.004–0.044 | 0.009–0.062 | 0.055–0.308 | [117] |
| 0.249–0.271 | 0.081–0.166 | 0.057–0.144 | 0.420–0.585 | [118] |
| 0.141–0.388 | 0.011–0.136 | 0.038–0.155 | NR | [119] |
| 0.010–3.255 | 0.001–1.975 | 0.003–2.228 | 0.015–7.511 | [120] |
| 0.001–0.276 | 0.008–0.104 | 0.022–0.117 | NR | [121] |
| 0.1 | NR | NR | 0.2 | EU/USP monograph [114,115] |
| 0.041 | 0.004 | 0.010 | NR | SRM 3250 [39] |
| 0.164 | 0.022 | 0.050 | NR | SRM 3251 [39] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buț, M.-G.; Jîtcă, G.; Imre, S.; Vari, C.E.; Ősz, B.E.; Jîtcă, C.-M.; Tero-Vescan, A. The Lack of Standardization and Pharmacological Effect Limits the Potential Clinical Usefulness of Phytosterols in Benign Prostatic Hyperplasia. Plants 2023, 12, 1722. https://doi.org/10.3390/plants12081722
Buț M-G, Jîtcă G, Imre S, Vari CE, Ősz BE, Jîtcă C-M, Tero-Vescan A. The Lack of Standardization and Pharmacological Effect Limits the Potential Clinical Usefulness of Phytosterols in Benign Prostatic Hyperplasia. Plants. 2023; 12(8):1722. https://doi.org/10.3390/plants12081722
Chicago/Turabian StyleBuț, Mădălina-Georgiana, George Jîtcă, Silvia Imre, Camil Eugen Vari, Bianca Eugenia Ősz, Carmen-Maria Jîtcă, and Amelia Tero-Vescan. 2023. "The Lack of Standardization and Pharmacological Effect Limits the Potential Clinical Usefulness of Phytosterols in Benign Prostatic Hyperplasia" Plants 12, no. 8: 1722. https://doi.org/10.3390/plants12081722
APA StyleBuț, M.-G., Jîtcă, G., Imre, S., Vari, C. E., Ősz, B. E., Jîtcă, C.-M., & Tero-Vescan, A. (2023). The Lack of Standardization and Pharmacological Effect Limits the Potential Clinical Usefulness of Phytosterols in Benign Prostatic Hyperplasia. Plants, 12(8), 1722. https://doi.org/10.3390/plants12081722








