Abstract
Penetrating injuries of the heart, named penetrating cardiac injury (PCI), may cause hemorrhagic shock as well as cardiac tamponade, leading to death if not treated immediately. This systematic review aims to highlight the main aspects of penetrating cardiac injuries after firearm wounds. The cases of 39 subjects (age 37.05 + 15.4) were selected (6 fatal cases). Specifically, 4/39 cases involved subjects under 18 y.o.; analyzing the entrance wound, in 30/39 cases it was located in the anterior chest, 4/39 in the posterior chest, 3/39 in the shoulder/axilla area, 1/39 in the neck, and 1/39 in the pelvis (gluteus). The exit wound was found in only 3/39 cases. Several factors may influence the prognosis: firstly, prompt intervention represents a crucial point, then considering the complications related to PCI, the most important are myocardial infarction, and projectile migration with embolization. The mortality rate is related to: (1) area and severity of the heart injury; (2) duration of transport and intervention; (3) contemporary lesion to other organ/s; (4) the quantity of blood lost; (5) and presence/absence of cardiac tamponade. Based on these findings, a correct approach in the management of PCI may be considered important from a forensic point of view, both as regards to medical liability and from the trial perspective.
1. Introduction
Penetrating cardiac trauma usually generates lethal injuries. Penetrating injuries of the heart, named penetrating cardiac injury (PCI), may cause hemorrhagic shock as well as cardiac tamponade, leading to death if not treated immediately [1,2]. PCIs are traditionally related to stab wounds such as knife injury or firearm wounds. Moreover, penetrating cardiac trauma may be caused by non-firearm-related blast injuries [3].
In the case of firearm wounds, the relative cardiac injuries are particularly severe: about 90% of victims die before arriving at a hospital [4]. On the contrary, the survival rate of the hospitalized cases is estimated between 20–75% [3]. Clinical outcome is related to the condition at first observation at the hospital, ranging from complete hemodynamic stability to cardiac arrest. It is important to note that in the last few years, survival rates have increased in consideration of improvements in prehospital care, diagnostic procedures, and surgical procedures [5].
Victim survival rate is related to different variables such as age, type of injury (it is related to the different ammunitions and relative weapons), physiopathological state, and the association with other organ damage [6].
In this study, we performed a systematic review concerning PCI following firearm wounds, analyzing original articles and case reports with the aim of defining the main aspects, such as the importance of crime scene investigation (CSI), radiological and clinical data, and the role of autopsy in fatal cases.
2. Materials and Methods
A systematic review of the literature was performed according to the PRISMA guidelines [7]. The literature review was performed using PubMed and Scopus databases. On these websites, we searched for articles from 1st January 1990 to 1st September 2022 using the following key terms: “Penetrating cardiac injuries” AND “Firearm”, AND “Gunshot”, AND “Weapon”, AND “Gunshot wounds”, AND “Firearm wounds”.
2.1. Inclusion and Exclusion Criteria
The case reports and original articles published in peer-reviewed journals were screened if the keywords matched with the “Article title”, “Abstract”, and “Keywords”. To identify further studies that met the inclusion criteria, the references of the selected papers were also reviewed.
The exclusion criteria were: (1) wrong publication type (articles not relevant to the study), (2) review, (3) letters or editorials, (4) articles not in English, (5) meta-analysis, (6) retrospective studies. The inclusion criteria were: (1) original article, (2) case report, (3) articles in English.
2.2. Quality Assessment and Data Extraction
M.E. and F.S. analyzed all the articles, evaluating the whole text. In cases of discrepancy of opinions between inclusion or exclusion of articles, they were submitted to M.S.
2.3. Characteristics of Eligible Studies
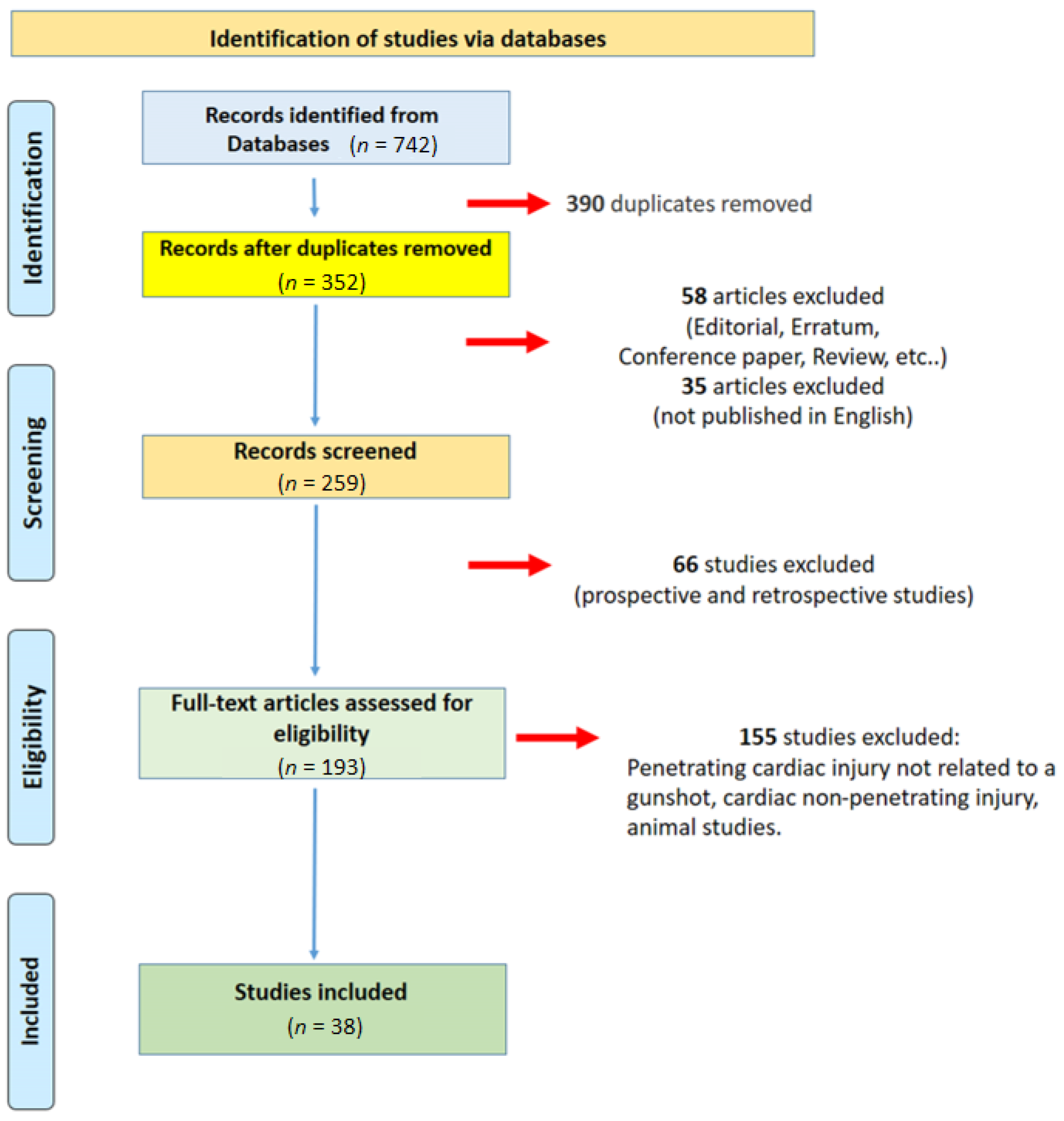
A total of 742 articles were collected. Of these, 390 duplicates were removed. A total of 193 articles were eligible. After an accurate evaluation, 38 articles were included in the present systematic review (Figure 1).
Figure 1.
Data source flow chart showing the literature review process and case inclusion. A total of 38 articles were analyzed.
3. Results
PCIs are uncommon: it is estimated that less than 10 cases per year were counted in most hospitals [8].
After the literature review, 38 articles (39 cases) were selected, and the main characteristics are summarized in Table 1. The majority of the articles were published in the USA (15), while the other cases belong to the following countries: Brazil (4), Turkey and Germany (3), Italy, France, and Pakistan (2), Nepal, Czech Republic, Spain, Japan, Taiwan, Serbia, Canada, and India (1).

Table 1.
The main findings of each analyzed case are listed ranking them from the more recent to the oldest.
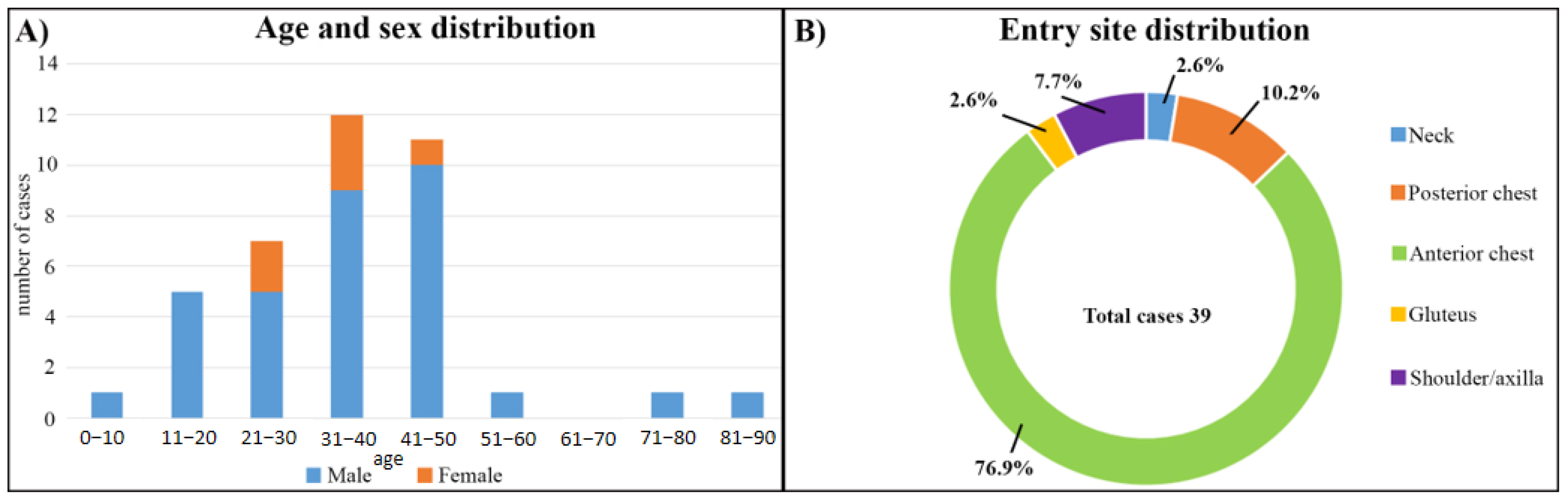
The analyzed cases involved 39 subjects (age 37.05 + 15.4): 33 males (age 37.3 + 16.3) and 6 females (age 35.6 + 9.8).
As summarized in Figure 2A, 4/39 cases involved subjects under 18 y.o.; despite the risk of death in young children in cases of PCI being higher compared to adults considering the close proximity with other vital organs, in all cases, the victims survived the accident. In particular, Rasool et al. (2014) [27] reported the case of a 10-year-old boy with a PCI and lesion of different organs such as the stomach and liver. Despite these severe clinical conditions, the boy survived surgical intervention. Lovasik et al. (2021) [11] described the case of a young male with a single gunshot wound to the right chest who was discharged 14 days after admission. Knowlin et al. (2018) [13] described the case of a healthy 11-year-old male after sustaining a gunshot wound with an entrance in the left posterior axillary line and exit wound in the anterior chest; despite the severity of the lesions, cardiac function was grossly normal. A prompt recovery was reported by Abou-Leila and Voronov (2017) [17]; in their case, the young victim was discharged 4 days post-intervention.
Figure 2.
Patients’ demographics and entry site characteristics. (A) The age and sex distribution of the affected patients is shown, with most patients being male in the second through fourth decade of life. (B) Entry site distribution analysis shows injury to the chest (anterior and posterior), shoulder/axilla region, gluteus, and neck.
As summarized in Figure 2B, analyzing the entrance wound, in 30/39 cases, it is located in the anterior chest, 4/39 in the posterior chest, 3/39 in the shoulder/axilla area, 1/39 in the neck, and 1/39 in the pelvis (gluteus). Nevertheless, as reported by Ovali et al. (2021) [9], the PCI may not be related to a thoracic wound, but the injury zone may originate from a gunshot in the neck, as in their case. In the same way, Romero-Velez et al. (2020) [12] presented the case of a victim with multiple gunshot wounds; however, the heart injuries originated from the right gluteal fold, whichmay be considered as an atypical area for PCI.
Analyzing all cases (39/39), the exit wound was found in only 3/39 cases [13,26,36]; a particular case is described by De Giorgio and Raino (2007) [36]: they described multiple gunshots with PCIs, which may be considered fatal for the victim. The peculiarity of this case is represented by the penetration of the two bullets into the heart with a single, common exit wound, demonstrating the importance of the post-mortem examination in similar cases in order to define the exact dynamics. The shot distance does not influence the possibility that the projectile may be retained; Konecny et al. (2016) [23] described an attempted suicide, and despite the short distance, the projectile was retained.
There were six fatal cases (five males and one female), with an average age of 53.6 +19.8, much higher compared to data of all selected cases. Analyzing the scenario of the fatal cases, four were suicides, one was homicide, and another one was not classified by the authors. In three cases (two suicides and one homicide), the subject died at the crime scene; in all these cases, an autopsy was performed, confirming severe cardiac injuries in two cases [14,36], while in another one, the subject shot another bullet to his head after a shot to his thorax [29]. In one case, the woman died immediately after she had arrived at the emergency department [31], while in the other two cases, one patient died for multiorgan failure (the delay in the arrival at the hospital was decisive for the patient’s death) [30], and another from a cerebrovascular event [42]. In the fatal case reported by Cvetkovic et al. (2018) [14], there were two gunshot wounds, hitting the heart at different points. The forensic interest of the discussed case was related to the fact that this was a suicide with multiple gunshots. Usually, in similar cases, there is the suspicion of homicide: following a careful evaluation, the authors justified the two gunshots, confirming the importance of an autopsy.
It is important to note that several factors may influence the prognosis of victims with a PCI: firstly, prompt intervention is a crucial point. Faschingbauer et al. (2006) [38] described a case of a single gunshot with penetrating cardiac injury: the patient survived thanks to prompt surgery. Siddiqui et al. (2015) [25] discussed two cases proposing a different surgical approach in relation to the heart wound. Particularly, in their cases, no exit wound was detected. Both patients survived after prompt medical and surgical interventions. As reported by Tran et al. (2021) [10] and Karigyo et al. (2011) [32], to reduce the risks of cardiac tamponade, prompt surgery is important, particularly in the case of a retained bullet. The case reported by Incorvaia et al. (2007) [37] is singular, with the victim hit in the chest by a bullet that fell from the sky. Despite the bullet falling at terminal velocity compared to their initial muzzle velocity, it was sufficient to cause significant injuries. In the described case, the bullet was able to injure four organs, including the heart, diaphragm, stomach, and spleen. Prompt surgery may be decisive in cases of severe injuries, such as the presence of a hole in both ventricles, such as in the case reported by Kwan et al. (1995) [44]: with prompt surgery the victim survived the accident.
The most important complications related to PCI are myocardial infarction [40] and projectile migration with embolization [20]. Particularly, myocardial infarction could be related to the abuse of different substances; however, in the analyzed cases, the toxicological investigations were reported in only two cases [33,36], while this tool may be considered fundamental in order to ascertain the exact cause of death [47,48,49,50,51].
Considering the complications that may be related to the PCI, Obrador et al. (2015) [24], in their case report, discussed the risk of infection developing, such as pneumonia in victims with PCI. In particular, the authors strongly encouraged post-operative follow up in order to reduce these risks. Ustin et al. (2011) [33] reported the case of a pregnant woman who attempted suicide. Despite the woman surviving the attempted suicide, and the baby being delivered at term, the subsequent clinical investigation demonstrated pituitary infarction after hemorrhagic shock, emphasizing the importance of considering endocrine dysfunction in all cases of persistent hypotension. In the evaluation of the severity of the injury, as reported by Rupprecht and Gaab (2018) [15], the rib may result decisive in reducing the severity of heart lesions.
Based on the selected cases, it is possible to have adverse effects or complications after several hours or days post-accident. Sapkota and Koirala (2016) [21] presented a case of a singular wound to the heart, with the patient admitted to the emergency room after 9 h; nevertheless, the victim survived the operation, returning to his normal life. Volpe et al. (2018) [16] discussed a singular case of a victim with two retained projectiles, with a penetrating cardiac injury. In this case, the symptoms started 16 days after the accident; the location near the apex of the right ventricle could be considered decisive in the containment of the bleeding. Nevertheless, the subject was operated on and discharged. Similarly, Meira et al. (2005) [39] discussed the case of a subject with a penetrating injury and a stable hemodynamic condition: surgery to remove the bullet from the heart was performed 11 days after the accident.
Another important consideration is related to the opportunity to perform a radiological investigation, particularly when the projectile is retained. The chest-X ray represents the basic approach: it should be considered mandatory, and it is usually supported by CT, ECHO, and FAST. As highlighted by different authors [11,17,18,22,26,28,41,42,43,45,46], the support of radiographic investigation, as well as the CT scan, may be considered fundamental in order to identify the retained projectile, guiding surgical operations. This concept is reported by Fu et al. (2017) [19], particularly when multiple lesions on the heart were detected. In only 1/39 cases [12], did the authors report that the victim was operated on without radiological investigation because of the severity of the lesions. The role of radiological support is important in the evaluation of projectile trajectory in order to evaluate the possibility of other organ damage. As previously described, the possibility to involve other abdominal organs is possible in young subjects as well as in adults, as reported by Harter et al. (2010) [34] and Ellertson and Johnson (2008) [35].
4. Discussion
According to the literature, there are several important considerations concerning PCI after a gunshot. PCIs were first described by Hollerius in 1868 [52]. Moreover, in 1989, Noughton et al. suggested that timely transport, resuscitation, and immediate surgery represent the main essential aspects in the management of penetrating cardiac trauma [53]. A first confirmation was given by Campbell et al. in 1997. They analyzed 1198 PCI cases in South Africa, finding that about 6% reached the hospital alive, while 94% were transferred directly to the mortuary [54]. Mittal et al. analyzed the outcome of patients with PCI in a level II Trauma Center in northern Detroit for 14 years: 45% of victims reported gunshot wounds and 55% had stab wounds; survival rate was 47% in gunshot injuries and 80% in stab injuries. In this study, the authors confirmed that the mortality rate may be significantly reduced with early diagnosis, rapid transportation to the hospital, and correct treatment [55].
In 1998, Asensio et al. analyzed the survival rate after PCIs, resulting in an overall survival rate of 36.6% [56]. Moreover, the same research group published another report estimating the survival rate at about 33%. In this study, they reported that the severity of hemorrhages and blood pressure were the most relevant factors influencing survival rate [57,58].
Tyburski et al. conducted a retrospective study reporting a survival rate of 23% after a PCIs related to gunshots. Several factors influence the prognosis, such as physiological status at admission, presence of cardiac tamponade, mechanism of injury, and type and number of cardiac chambers involved (survival rate of 51% in single-chamber injuries versus a 13% survival rate in multiple-chamber and great vessel injuries) [59]. In other studies, it has highlighted that the survival rate may be related both to the kind of lesion and to the number of heart chambers involved [60]. With reference to the anatomic site affected, Karaca et al. in 2015 found 17% mortality in cases of exclusive chest involvement, while the worst outcome was observed in cases of multi-chambers or concomitant involvement of other organs [4]. Other authors highlighted the significance of response time and surgical intervention as essential to hemodynamic stability and survival rate [61,62].
Swaroop et al. emphasized the importance of the interval time between accident and rescue operation, demonstrating that longer interval times are strictly related to higher mortality rates, particularly for interval times of 46–60 min. [63]. In 2016, Meizoso et al. confirmed the positive impact in the survival rate of surgical timing: patients having surgery after 10 min had higher mortality compared with those operated on before [64]. In agreement with these findings, Campbell reported that victims who had surgery within 30 min had a better survival rate compared with those in whom surgery was delayed [54]. It is important to note that short interval times are not frequent in real cases.
Other studies have compared the survival rate of stab wound cardiac injuries to the survival rate of gunshot PCIs, concluding that the gunshot injuries resulted in worse outcomes (survival rates were 5%-11.5% for gunshot and 33–50.3% for stab wounds) [65,66,67].
A study performed in a Scandinavian trauma center reported that victims admitted with a gunshot PCI had a survival rate of 50% [68], while a retrospective study conducted in a Brazilian trauma center highlighted that PCI after a firearm incident had a mortality rate of 52.2% [69]. Other studies reported a mortality rate ranging from 39 to 94 % for PCI due to a gunshot/stab wound [70,71,72,73,74,75,76,77].
Tavares Pereira et al. estimated the incidence of penetrating injuries during a 20-year period, comparing the periods 1990–1999 (group 1) and 2000–2009 (group 2); 48.4% of patients sustained stab wounds, and 51.6% were victims of gunshot wounds. The total mortality rate was 16.1%, but the authors observed a trend in mortality reduction when comparing group 1 with group 2 (20.3% versus 10.3%), demonstrating a decrease in mortality over the years [78].
From a forensic point of view, firearm wounds represent a central issue in forensic pathology, particularly in the definition of dynamics and the responsibility on the crime scene, as well as the possible medical doctor responsibility in patient management. In particular, atypical wound site or unexpected trajectories of pellets or bullets may complicate the interpretation of wounds, injuries, and mechanisms, and the post-mortem investigation combined to a multidisciplinary approach became an indispensable tool [79,80]. For example, the use of histological, immunohistochemical, and molecular techniques could be very useful to assess wound vitality and to improve the methods to define the time since death [81,82]. At the external examination of the corpse, forensic pathologists may find either the same number of entrance and exit wounds, or alternatively, a great number of entrance wounds (in the case of retained bullets), or rarely, a great number of exit wounds (in the case of fragmentation or explosion of bullets inside the body). As reported in this review, this last possibility rarely occurred. Moreover, as documented in this literature review, the site of injuries may not be considered fundamental for the survival rate of the victim because PCI may be generated from an atypical injury site (for example from the neck or gluteo). Compared to the site, it is more important the establish the exact trajectory of the projectile.
The most important finding in fatal cases is cardiac tamponade: it is life-threatening, slow, or rapid compression of the heart due to the pericardial accumulation of fluid, pus, blood, clots, or gas, because of effusion, trauma, or heart rupture.
Another crucial point is bullet embolization into the systemic circulation after gunshot injury, particularly when a PCI occurs: it may be fatal for the victim.
In a forensic context, crime scene investigations (CSI) following firearm accidents are also essential for both medical and forensic pathologists in cases of critical and fatal injuries [80]. Important elements such as bullet trajectory can be deduced through CSI and can aid in investigations and autopsies. In this regard, Bonsignore et al. [29] were able to define which shot hit the victim in the heart among different lesions combining the evidence collected during CSI with the autoptic findings. Moreover, understanding the dynamics of the accident is vital for predicting possible organ damage. It is also essential to check the compatibility of the weapon allegedly used with the injury in cases of homicide.
As summarized in our data, the exit wound was reported in only three cases. In our opinion, these findings are strictly related to the fact that a great number of the published papers are related to the surgical techniques to repair heart damage or to remove the retained bullet.
In light of the findings of this review, the mortality rate after a PCI is related to:
- √
- Area and severity of the heart injury;
- √
- Duration of transport and intervention;
- √
- Contemporary lesion to other organ/s;
- √
- The quantity of blood lost;
- √
- Presence/absence of cardiac tamponade.
Usually, the first hour after the accident may be considered crucial. A timely diagnosis and subsequently prompt treatment may be decisive to improve the survival rate for the victim, reaching more than 70% [9]. Moreover, after a PCI with subsequent treatment and discharge, the survival rate is about 88% at nine years, although it is important to start a long-term follow-up [10]. Contrariwise, in the absence of treatment in the first hour, the mortality rate is about 75% [9]. Other factors that could positively or negatively influence the patient’s outcome are related to different situations. Indeed, considering that PCI management is a complex challenge, limited experience in the field of routine cardiac surgery, the misrecognition or failure to ascertain concomitant injuries to the chest or abdominal cavity due to the high kinetic energy of the projectile, or secondary injuries due to bone fragments, may be considered negative factors. On the contrary, the arrival of the victim at a top-level trauma center experienced in thoracic cardiac surgery as well as recourse to the multidisciplinary management of complications may be considered positive factors [83,84,85].
Radiological investigations are a very useful tool to identify the retained bullet. Indeed, when there is no exit wound, the retained projectile may generate additional complications, such as infection, ischemia, and thrombosis: each of these conditions could be fatal for the victim. For these reasons, prompt removal should be evaluated in each case. As emerged from the literature review, in these cases, the final location of the projectile is influenced by different factors, such as the entry site, the size and weight of the projectile, the firing dynamic, and the victim’s position after firing, the hemodynamic situation, respiratory motion, and finally the severity of the injury. Based on the discussed data, when the victim is hemodynamically stable, it is strongly recommended to immediately carry out a whole-body radiographic examination, even if the wounds are not located in the chest or abdominal region. The chest X-ray is the fastest screening method, but it should be supported by other radiologic techniques in order to investigate organ injury and the possible bullet embolization pathway. In this way, angiography could be very useful to confirm arterial injury and embolization, while a CT scan may help in the identification of other injuries in vascular structures and organs; ECHO represents a valuable tool to ascertain cardiac damage, particularly in the presence of valvular regurgitation and hemopericardium. It is important to note that the use of radiological techniques is fundamental in the post-mortem examination to establish the trajectory of the bullet, as well as the presence of organ injuries to define the exact cause of death. Moreover, radiological technologies are considered a very useful tool to clarify several important forensic aspects of PCI, as well as to perform a differential diagnosis between entry and exit wounds and estimate the firing distance [84,85,86,87].
This literature review contains several strengths: the use of different keywords, with inclusion and exclusion criteria; the wide temporal period analyzed (from 1 January 1990 to 1 September 2022). At the same time, several limitations are present: the inclusion of articles published only on Pubmed or Scopus; the impossibility of applying a complete statistical analysis due to the small sample size; the absence of different information, such as the presence of pre-existence pathologies, the dynamic of the event, and multisystem lesion involvement. Finally, the toxicological findings were reported in only two articles, while this tool could be considered fundamental in the definition of the exact cause of death.
5. Conclusions
In conclusion, the management and prognosis of victims affected by PCIs after a firearm wound relies on several crucial factors. The most crucial factor is the hemodynamic situation after the accident; this is related to the type of firearm lesion. An injury to the heart chambers or vessel lesions can lead to cardiac tamponade, therefore requiring immediate hospitalization, stabilization, and surgery. When the victim is hemodynamically stable in the emergency room, about 60–70% will not need surgery.
When analyzing forensic cases, it is essential to consider the above outcomes: a correct approach in the management of PCI may be considered important from a forensic point of view, both as regards to medical liability and from the trial perspective.
Based on these considerations, the post-mortem examination with a multidisciplinary approach remains the gold standard method in cases of firearm murder, and it should always be performed, even if the dynamics seem clear.
Author Contributions
Conceptualization, F.S. and M.S.; methodology, F.S., G.C., M.E., E.S., P.M., and M.S.; formal analysis, F.S., G.C., M.E., P.Z., E.S., P.M., and M.S.; data curation, F.S., G.C., M.E., P.Z., E.S., P.M., and M.S.; writing—original draft preparation, F.S. and M.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article.
Acknowledgments
The authors thank the Scientific Bureau of the University of Catania for language support.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Šimek, M.; Konečný, J.; Hájek, R.; Čižmář, I.; Kutěj, V.; Lonský, V. Penetrating Injuries of the Heart and Great Vessels-Fifteen Years of Experience of the Cardiac Surgery Service as a Part of the Major Trauma Centre. Acta Chir. Orthop. Traumatol. Cechoslov. 2018, 85, 144–148. [Google Scholar]
- Ingraham, A.; Sperry, J. Operative Management of Cardiac Injuries: Diagnosis, Technique, and Postoperative Complications. Curr. Trauma Rep. 2015, 1, 225–231. [Google Scholar] [CrossRef]
- Dokoupil, M.; Marecová, K.; Uvíra, M.; Joukal, M.; Mrázková, E.; Chmelová, J.; Handlos, P. Fatal delayed hemopericardium and hemothorax following blunt chest trauma. Forensic Sci. Med. Pathol. 2019, 15, 272–275. [Google Scholar] [CrossRef] [PubMed]
- Karaca, M.A. Evaluation of Gunshot Wounds in the Emergency Department. Turk. J. Trauma Emerg. Surg. 2015, 21, 248–255. [Google Scholar] [CrossRef]
- Mina, M.J.; Jhunjhunwala, R.; Gelbard, R.B.; Dougherty, S.D.; Carr, J.S.; Dente, C.J.; Nicholas, J.M.; Wyrzykowski, A.D.; Salomone, J.P.; Vercruysse, G.A.; et al. Factors affecting mortality after penetrating cardiac injuries: 10-year experience at urban level I trauma center. Am. J. Surg. 2017, 213, 1109–1115. [Google Scholar] [CrossRef]
- Topal, A.E.; Celik, Y.; Eren, M.N. Predictors of Outcome in Penetrating Cardiac Injuries. J. Trauma 2010, 69, 574–578. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Kang, N.; Hsee, L.; Rizoli, S.; Alison, P. Penetrating cardiac injury: Overcoming the limits set by Nature. Injury 2009, 40, 919–927. [Google Scholar] [CrossRef]
- Ovali, C.; Kocaoglu, A.S.; Demirdizen, G.; Aydar, Y. Penetrating Heart Injury Repaired with Peripheral Cannulation: Case Report. Prehosp. Disaster. Med. 2021, 36, 793–796. [Google Scholar] [CrossRef]
- Tran, D.; Jones, D.; Moore, R.; Guarneri, R. Abdominal Aorta Bullet Embolism: Presentation and Management. Ann. Vasc. Surg. 2021, 74, 524.e17–524.e21. [Google Scholar] [CrossRef]
- Lovasik, B.P.; Nauser, C.L.; Klingensmith, N.J.; Nguyen, J.H. Bullet Embolism into the Common Iliac Artery from a Gunshot Wound to the Heart. Am. Surg. 2021, 88, 1014–1015. [Google Scholar] [CrossRef] [PubMed]
- Romero-Velez, G.; Kaban, J.M.; Chao, E.; Lewis, E.R.; Stone, M.E.J.; Teperman, S.; Reddy, S.H. Use of the EVARREST Patch for Penetrating Cardiac Injury. Trauma Case Rep. 2020, 28, 100324. [Google Scholar] [CrossRef] [PubMed]
- Knowlin, L.T.; McAteer, J.P.; Kane, T.D. Cardiac Injury Following Penetrating Chest Trauma: Delayed Diagnosis and Successful Repair. J. Pediatr. Surg. Case Rep. 2018, 39, 45–47. [Google Scholar] [CrossRef]
- Cvetković, D.; Živković, V.; Juković, F.; Nikolić, S. Double suicidal gunshot wounds to the heart. Forensic Sci. Med. Pathol. 2017, 14, 248–250. [Google Scholar] [CrossRef] [PubMed]
- Rupprecht, H.; Gaab, K. Delayed Cardiac Rupture Induced by Traumatic Myocardial Infarction: Consequence of a 45-Magnum Blast Injury; A Comprehensive Case Review. Bull. Emerg. Trauma 2018, 6, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Volpe, M.A.; Paredes, J.E.M.; Redigolo, L.C.; Sanchez, I.S.M.; Lanichek, F.; Silveira, L.Z.D. Heart Injury with Projectile Lodged Inside the Heart. Rev. Bras. de Cir. Cardiovasc. 2018, 33, 303–305. [Google Scholar] [CrossRef] [PubMed]
- Abou-Leila, A.; Voronov, G. The journey of harmless bullet: The perioperative care of penetrating cardiac injury. Anesthesia Essays Res. 2017, 11, 790–793. [Google Scholar] [CrossRef] [PubMed]
- Santos, E.C.L.; Tchaick, R.M.; Ferraz, D.L.D.M.; Oliveira, J.P.S.D.P.; Figueira, F.A.M.D.S.; Lima, G.A.D.F.C.A. Embolization by Bullet Dislodged from the Heart. Rev. Bras. Cir. Cardiovasc. 2017, 32, 539–541. [Google Scholar] [CrossRef]
- Fu, H.-Y.; Ting, M.; Wang, Y.-C.; Yu, H.-Y. Intracardiac foreign body resulting from a transmediastinal gunshot mimics an extracardiac foreign body: An image presentation. J. Formos. Med. Assoc. 2017, 116, 815–818. [Google Scholar] [CrossRef]
- Imbert, P.-Y.; Goin, G.; Goudard, Y.; De La Villéon, B.; Bonnet, P.-M.; Sockeel, P.; Pauleau, G. Pulmonary Artery Bullet Embolism Following Cardiac Gunshot Wound. Ann. Vasc. Surg. 2016, 36, e11–e290. [Google Scholar] [CrossRef]
- Sapkota, R.; Koirala, B. Traumatic Pseudoaneurysm of the Heart. Gen. Thorac. Cardiovasc. Surg. 2016, 64, 101–104. [Google Scholar] [CrossRef] [PubMed]
- Kaya, A.; Caliskan, E.; Tatlisu, M.A.; Hayiroglu, M.I.; Tekessin, A.I.; Cakilli, Y.; Avsar, S.; Oz, A.; Uzman, O. A Retained Bullet in Pericardial Sac: Penetrating Gunshot Injury of the Heart. Case Rep. Cardiol. 2016, 2016, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Konecny, J.; Klvacek, A.; Simek, M.; Lonsky, V.; Santavy, P. Complex gunshot injury to the heart as a consequence of suicide attempt in a schizophrenic patient. Int. J. Surg. Case Rep. 2016, 24, 80–82. [Google Scholar] [CrossRef] [PubMed]
- Obrador, L.Z.; Al-Lal, Y.M.; Palacios, J.D.T.; Prats, I.A.; Fuentes, F.T. Transmediastinal and Transcardiac Gunshot Wound with Hemodynamic Stability. Case Rep. Surg. 2014, 2014, 1–3. [Google Scholar] [CrossRef]
- Siddiqui, F.A.; Kabeer, J.; Shahabuddin, S. Surviving shot through the heart: Management in two cases. J. Pak. Med Assoc. 2015, 65, 93–94. [Google Scholar]
- Suzuki, T.; Wada, T.; Funaki, S.; Abe, H.; Seki, I.; Imaki, S.; Nakazawa, A. Traumatic left ventricular free-wall laceration by a gunshot: Report of a case. Surg. Today 2012, 44, 1152–1155. [Google Scholar] [CrossRef]
- Rasool, S.H.; Arif, M.; Arain, G.M. Right Ventricle Injury by Stray Bullet. Pak. J. Med. Health Sci. 2014, 8, 1133–1134. [Google Scholar]
- Mills, E.E.; Birnbaum, P.L.; Davis, J.W. Asymptomatic Gunshot Wound to the Heart with Retained Intracardiac Pellet. Ann. Thorac. Surg. 2014, 97, e15–e16. [Google Scholar] [CrossRef]
- Bonsignore, A.; Bernucci, L.V.; Canepa, M.; Ventura, F. Suicide Due to Four Speargun Shots. Am. J. Forensic Med. Pathol. 2013, 34, 201–204. [Google Scholar] [CrossRef]
- Porcu, P.; Moreau-Gaudry, A.; Chavanon, O.; Blin, D. Haemostasis of a right ventricle-gunshot wound using a novel haemostatic vacuum device. Interact. Cardiovasc. Thorac. Surg. 2012, 15, 294–296. [Google Scholar] [CrossRef]
- Branch, C.F.; Adams, J. Left Ventricular Rupture with Resulting Cardiac Tamponade Due to Blast Force Trauma from Gunshot Wound. J. Emerg. Med. 2012, 43, 263–265. [Google Scholar] [CrossRef] [PubMed]
- Karigyo, C.J.T.; Fan, O.G.; Rodrigues, R.J.; Tarasiewich, M.J. Ferimento cardíaco transfixante por projétil de arma de fogo: Relato de caso. Rev. Bras. de Cir. Cardiovasc. 2011, 26, 298–300. [Google Scholar] [CrossRef] [PubMed]
- Ustin, J.S.; Sinha, P.S.; Kelly, K.B. Sheehan-like syndrome in a pregnant patient with a cardiac gunshot wound. Inj. Extra 2011, 42, 61–63. [Google Scholar] [CrossRef]
- Hartert, M.; Dahm, M.; Neufang, A.; Vahl, C.-F. Minimum Cause--Maximum Effect: The Travelogue of a Bullet. Interact. Cardiovasc. Thorac. Surg. 2010, 11, 698–700. [Google Scholar] [CrossRef]
- Ellertson, D.G.; Johnson, S.B. Total Inflow Occlusion to Repair a Penetrating Cardiac Injury: Case Report. J. Trauma: Inj. Infect. Crit. Care 2008, 64, 1628–1629. [Google Scholar] [CrossRef]
- de Giorgio, F.; Rainio, J. Two Entrances, One Exit—An Atypical Shotgun Injury: A Case Report. Med. Sci. Law 2007, 47, 353–356. [Google Scholar] [CrossRef]
- Incorvaia, A.N.; Poulos, D.M.; Jones, R.N.; Tschirhart, J.M. Can a Falling Bullet Be Lethal at Terminal Velocity? Cardiac Injury Caused by a Celebratory Bullet. Ann. Thorac. Surg. 2007, 83, 283–284. [Google Scholar] [CrossRef]
- Faschingbauer, M.; Schulz, A.P.; Jürgens, C. Cardial Gunshot Injury: Treatment in a Trauma Hospital without a Cardiac Unit. Eur. J. Emerg. Med. 2006, 13, 238–241. [Google Scholar] [CrossRef]
- Meira, E.B.D.S.; Guidugli, R.B.; Meira, D.B.D.S.; Rocha, R.M.; Ghefter, M.C.; Richter, I. Abordagem terapêutica dos projéteis retidos no coração. Rev. Bras. de Cir. Cardiovasc. 2005, 20, 91–93. [Google Scholar] [CrossRef]
- Bali, H.K.; Vijayvergiya, R.; Banarjee, S.; Kumar, N. Gunshot injury of the heart: An unusual cause of acute myocardial infarction. Tex. Hear. Inst. J. 2003, 30, 158–160. [Google Scholar]
- Habdank, K.; Nolan, R.L. Gunshot Wound to the Thorax with Bullet Embolization to the External Carotid Artery. J. Thorac. Imaging 2003, 18, 42–44. [Google Scholar] [CrossRef]
- Kurt, N.; Küçük, H.F.; Celik, G.; Demirhan, R.; Celik, G.; Gül, O.; Ektirici, S.; Gülmen, M. Bullet Embolism of the Right External Iliac Artery Following Cardiac Gunshot Wound (a Case Report). Ulus. Travma Derg. 2001, 7, 131–133. [Google Scholar]
- Doty, J.R.; Cameron, D.E.; Elmaci, T.; Salomon, N.W. Penetrating Trauma to the Tricuspid Valve and Ventricular Septum: Delayed Repair. Ann. Thorac. Surg. 1999, 67, 252–253. [Google Scholar] [CrossRef]
- Kwan, T.; Salciccioli, L.; Elsakr, A.; Burack, J.; Feit, A. Coronary artery fistula coexisting with a ventricular septal defect due to a penetrating gunshot wound. Catheter. Cardiovasc. Diagn. 1995, 34, 235–239. [Google Scholar] [CrossRef] [PubMed]
- Wait, M.A.; Mueller, M.; Barth, M.J.; Brickner, E.; Salman, T.; Jessen, M.E. Traumatic coronary sinocameral fistula from a penetrating cardiac injury. J. Trauma 1994, 36, 894–897. [Google Scholar] [CrossRef] [PubMed]
- Skipper, R.; Dębski, R. Intramyocardial Shotgun Pellets Diagnosed on Initial Emergency Room Chest X-ray. J. Trauma 1990, 30, 1609–1610. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Liberto, A.; Zuccarello, P.; Ministeri, F.; Licciardello, G.; Barbera, N.; Sessa, F.; Salerno, M. Heart rupture as an acute complication of cocaine abuse: A case report. Leg. Med. 2022, 58, 102084. [Google Scholar] [CrossRef]
- Montisci, M.; Thiene, G.; Ferrara, S.D.; Basso, C. Cannabis and Cocaine: A Lethal Cocktail Triggering Coronary Sudden Death. Cardiovasc. Pathol. 2008, 17, 344–346. [Google Scholar] [CrossRef]
- Sessa, F.; Esposito, M.; Messina, G.; Di Mizio, G.; Di Nunno, N.; Salerno, M. Sudden Death in Adults: A Practical Flow Chart for Pathologist Guidance. Healthcare 2021, 9, 870. [Google Scholar] [CrossRef]
- Turillazzi, E.; Bello, S.; Neri, M.; Pomara, C.; Riezzo, I.; Fineschi, V. Cardiovascular effects of cocaine: Cellular, ionic and molecular mechanisms. Curr. Med. Chem. 2012, 19, 5664–5676. [Google Scholar] [CrossRef]
- Cerretani, D.; Bello, S.; Cantatore, S.; Fiaschi, A.; Montefrancesco, G.; Neri, M.; Pomara, C.; Riezzo, I.; Fiore, C.; Bonsignore, A.; et al. Acute administration of 3,4-methylenedioxymethamphetamine (MDMA) induces oxidative stress, lipoperoxidation and TNFα-mediated apoptosis in rat liver. Pharmacol. Res. 2011, 64, 517–527. [Google Scholar] [CrossRef] [PubMed]
- Asensio, J.A.; Petrone, P.; Pereira, B.; Peña, D.; Prichayudh, S.; Tsunoyama, T.; Ruiz, F.; Marttos, A.; Capin, A.; De Marchena, E. Penetrating Cardiac Injuries: A Historic Perspective and Fascinating Trip Through Time. J. Am. Coll. Surg. 2009, 208, 462–472. [Google Scholar] [CrossRef] [PubMed]
- Naughton, M.J.; Brissie, R.M.; Bessey, P.Q.; Mceachern, M.M.; Donald, J.M.; Laws, H.L. Demography of Penetrating Cardiac Trauma. Ann. Surg. 1989, 209, 676–683. [Google Scholar] [CrossRef] [PubMed]
- Campbell, N.C.; Thomson, S.R.; Muckart, D.J.J.; Meumann, C.M.; Van Middelkoop, I.; Botha, J.B.C. Review of 1198 cases of penetrating cardiac trauma. Br. J. Surg. 1997, 84, 1737–1740. [Google Scholar] [CrossRef] [PubMed]
- Mittal, V.; McAleese, P.; Young, S.; Cohen, M. Penetrating Cardiac Injuries. Am. Surg. 1999, 65, 444–448. [Google Scholar] [CrossRef] [PubMed]
- Asensio, J. Penetrating Cardiac Injuries: A Prospective Study of Variables Predicting Outcomes. J. Am. Coll. Surg. 1998, 186, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Asensio, J.A.; Berne, J.D.; Demetriades, D.; Chan, L.; Murray, J.; Falabella, A.; Gomez, H.; Chahwan, S.; Velmahos, G.; Cornwell, E.E.; et al. One Hundred Five Penetrating Cardiac Injuries: A 2-Year Prospective Evaluation. J. Trauma Acute Care Surg. 1998, 44, 1073–1082. [Google Scholar] [CrossRef]
- Asensio, J.A.; Soto, S.N.; Forno, W.; Roldan, G.; Petrone, P.; Salim, A.; Rowe, V.; Demetriades, D. Penetrating cardiac injuries: A complex challenge. Injury 2001, 32, 533–543. [Google Scholar] [CrossRef]
- Tyburski, J.G.; Astra, L.; Wilson, R.F.; Dente, C.; Steffes, C. Factors Affecting Prognosis with Penetrating Wounds of the Heart. J. Trauma Inj. Infect. Crit. Care 2000, 48, 587–591. [Google Scholar] [CrossRef]
- Mitchell, M.E.; Muakkassa, F.F.; Poole, G.V.; Rhodes, R.S.; Griswold, J.A. Surgical approach of choice for penetrating cardiac wounds. J. Trauma Inj. Infect. Crit. Care 1993, 34, 17–20. [Google Scholar] [CrossRef]
- Crandall, M.; Sharp, D.; Unger, E.; Straus, D.; Brasel, K.; Hsia, R.; Esposito, T. Trauma Deserts: Distance from a Trauma Center, Transport Times, and Mortality from Gunshot Wounds in Chicago. Am. J. Public Health 2013, 103, 1103–1109. [Google Scholar] [CrossRef] [PubMed]
- Tanmoy, G.; Kumar, S.K.; Chaitali, S.; Chiranjib, B.; Manasij, M. Thoracic Gunshot Wound: A Report of 3 Cases and Review of Management [Heridas de Bala Torácicas: Informe de 3 Casos y Revisión de La Conducta a Seguir]. Prensa Med. Argent. 2016, 102, 471–476. [Google Scholar]
- Swaroop, M.; Straus, D.C.; Agubuzu, O.; Esposito, T.J.; Schermer, C.R.; Crandall, M.L. Pre-hospital transport times and survival for Hypotensive patients with penetrating thoracic trauma. J. Emergencies Trauma Shock. 2013, 6, 16–20. [Google Scholar] [CrossRef]
- Meizoso, J.P.; Ray, J.J.; Karcutskie, C.A.; Allen, C.J.; Zakrison, T.L.; Pust, G.D.; Koru-Sengul, T.; Ginzburg, E.; Pizano, L.R.; Schulman, C.I.; et al. Effect of Time to Operation on Mortality for Hypotensive Patients with Gunshot Wounds to the Torso: The Golden 10 Minutes. J. Trauma Acute Care Surg. 2016, 81, 685–691. [Google Scholar] [CrossRef]
- Gunay, C.; Cingoz, F.; Kuralay, E.; Demirkilic, U.; Tatar, H. Surgical Challenges for Urgent Approach in Penetrating Heart Injuries. Hear. Surg. Forum 2007, 10, E473–E477. [Google Scholar] [CrossRef] [PubMed]
- Molina, E.J.; Gaughan, J.P.; Kulp, H.; McClurken, J.B.; Goldberg, A.J.; Seamon, M.J. Outcomes after emergency department thoracotomy for penetrating cardiac injuries: A new perspective. Interact. Cardiovasc. Thorac. Surg. 2008, 7, 845–848. [Google Scholar] [CrossRef] [PubMed]
- Tang, A.L.; Inaba, K.; Branco, B.C.; Oliver, M.; Bukur, M.; Salim, A.; Rhee, P.; Herrold, J.; Demetriades, D. Postdischarge Complications After Penetrating Cardiac Injury. Arch. Surg. 2011, 146, 1061–1066. [Google Scholar] [CrossRef]
- Kaljusto, M.-L.; Skaga, N.O.; Pillgram-Larsen, J.; Tønnessen, T. Survival predictor for penetrating cardiac injury; a 10-year consecutive cohort from a scandinavian trauma center. Scand. J. Trauma Resusc. Emerg. Med. 2015, 23, 1–7. [Google Scholar] [CrossRef]
- Rodrigues, A.J.; Furlanetti, L.; Faidiga, G.B.; Scarpelini, S.; Evora, P.R.B.; Vicente, W. Penetrating cardiac injuries: A 13-year retrospective evaluation from a Brazilian trauma center. Interact. Cardiovasc. Thorac. Surg. 2005, 4, 212–215. [Google Scholar] [CrossRef]
- Thourani, V.H.; Feliciano, D.V.; Cooper, W.A.; Brady, K.M.; Adams, A.B.; Rozycki, G.S.; Symbas, P.N. Penetrating Cardiac Trauma at an Urban Trauma Center: A 22-Year Perspective. Am. Surg. 1999, 65, 811–818. [Google Scholar] [CrossRef]
- Shanmuganathan, K.; Matsumoto, J. Imaging of Penetrating Chest Trauma. Radiol. Clin. N. Am. 2006, 44, 225–238. [Google Scholar] [CrossRef] [PubMed]
- Clarke, D.; Quazi, M.A.; Reddy, K.; Thomson, S.R. Emergency operation for penetrating thoracic trauma in a metropolitan surgical service in South Africa. J. Thorac. Cardiovasc. Surg. 2011, 142, 563–568. [Google Scholar] [CrossRef] [PubMed]
- Morse, B.C.; Mina, M.J.; Carr, J.S.; Jhunjhunwala, R.; Dente, C.J.; Zink, J.U.; Nicholas, J.M.; Wyrzykowski, A.D.; Salomone, J.P.; Vercruysse, G.A.; et al. Penetrating Cardiac Injuries: A 36-Year Perspective at an Urban, Level i Trauma Center. J. Trauma Acute Care Surg. 2016, 81, 623–631. [Google Scholar] [CrossRef] [PubMed]
- Isaza-Restrepo, A.; Bolívar-Sáenz, D.J.; Tarazona-Lara, M.; Tovar, J.R. Penetrating cardiac trauma: Analysis of 240 cases from a hospital in Bogota, Colombia. World J. Emerg. Surg. 2017, 12, 1–7. [Google Scholar] [CrossRef]
- Sessa, F.; Salerno, M.; Bertozzi, G.; Messina, G.; Ricci, P.; Ledda, C.; Rapisarda, V.; Cantatore, S.; Turillazzi, E.; Pomara, C. Touch DNA: Impact of handling time on touch deposit and evaluation of different recovery techniques: An experimental study. Sci. Rep. 2019, 9, 1–9. [Google Scholar] [CrossRef]
- Tozzo, P.; Giuliodori, A.; Rodriguez, D.; Caenazzo, L. Effect of Dactyloscopic Powders on DNA Profiling from Enhanced Fingerprints: Results from an Experimental Study. Am. J. Forensic Med. Pathol. 2014, 35, 68–72. [Google Scholar] [CrossRef]
- Tozzo, P.; Mazzobel, E.; Marcante, B.; Delicati, A.; Caenazzo, L. Touch DNA Sampling Methods: Efficacy Evaluation and Systematic Review. Int. J. Mol. Sci. 2022, 23, 15541. [Google Scholar] [CrossRef]
- Pereira, B.M.T.; Nogueira, V.B.; Calderan, T.R.A.; Villaça, M.P.; Petrucci, O.; Fraga, G.P. Penetrating cardiac trauma: 20-y experience from a university teaching hospital. J. Surg. Res. 2013, 183, 792–797. [Google Scholar] [CrossRef]
- Pomara, C.; Gianpaolo, D.P.; Monica, S.; Maglietta, F.; Sessa, F.; Guglielmi, G.; Turillazzi, E. “Lupara Bianca” a Way to Hide Cadavers after Mafia Homicides. A Cemetery of Italian Mafia. A Case Study. Leg. Med. 2015, 17, 192–197. [Google Scholar] [CrossRef]
- Sessa, F.; Maglietta, F.; Asmundo, A.; Pomara, C. Forensic Genetics and Genomic. In Forensic and Clinical Forensic Autopsy; Pomara, C., Fineschi, V., Eds.; CRC Press: Boca Raton, FL, USA, 2021; pp. 177–192. [Google Scholar]
- Salerno, M.; Cocimano, G.; Roccuzzo, S.; Russo, I.; Piombino-Mascali, D.; Márquez-Grant, N.; Zammit, C.; Esposito, M.; Sessa, F. New Trends in Immunohistochemical Methods to Estimate the Time since Death: A Review. Diagnostics 2022, 12. [Google Scholar] [CrossRef]
- Pennisi, G.; Torrisi, M.; Cocimano, G.; Esposito, M.; Salerno, M.; Sessa, F. Vitality markers in forensic investigations: A literature review. Forensic Sci. Med. Pathol. 2022; online ahead of print. [Google Scholar] [CrossRef]
- González-Hadad, A.; Ordoñez, C.A.; Parra, M.W.; Caicedo, Y.; Padilla, N.; Millán, M.; García, A.; Vidal-Carpio, J.M.; Pino, L.F.; Herrera, M.A.; et al. Damage Control in Penetrating Cardiac Trauma | El Control de Daños En El Trauma Cardíaco Penetrante. Colomb Med 2021, 52, e4034519. [Google Scholar] [CrossRef] [PubMed]
- Fais, P.; Giraudo, C.; Viero, A.; Amagliani, A.; Viel, G.; Montisci, M.; Miotto, D.; Cecchetto, G. Identification of Bullet Entrance in Different Type of Intermediate Firearm Wounds through Micro-Computed Tomography Analysis. J. Forensic Radiol. Imaging 2015, 3, 147–152. [Google Scholar] [CrossRef]
- Cecchetto, G.; Giraudo, C.; Amagliani, A.; Viel, G.; Fais, P.; Cavarzeran, F.; Feltrin, G.; Davide Ferrara, S.; Montisci, M. Estimation of the Firing Distance through Micro-CT Analysis of Gunshot Wounds. Int. J. Leg. Med. 2011, 125, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Giorgetti, A.; Giraudo, C.; Viero, A.; Bisceglia, M.; Lupi, A.; Fais, P.; Quaia, E.; Montisci, M.; Cecchetto, G.; Viel, G. Radiological Investigation of Gunshot Wounds: A Systematic Review of Published Evidence. Int. J. Leg. Med. 2019, 133, 1149–1158. [Google Scholar] [CrossRef] [PubMed]
- Agius, A.; Calleja, N.; Camenzuli, C.; Sultana, R.; Pullicino, R.; Zammit, C.; Calleja Agius, J.; Pomara, C. Perceptions of First-Year Medical Students towards Learning Anatomy Using Cadaveric Specimens through Peer Teaching. Anat. Sci. Educ. 2018, 11, 346–357. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).