Abstract
This study used real-world data (RWD) to explore the long-term effects of East Asian traditional medicine (EATM) on heart failure (HF). A comprehensive search was conducted across five databases to identify relevant studies, which were then reviewed using the Arksey and O’Malley scoping review framework. The analysis focused on a descriptive examination of the long-term outcomes associated with EATM intervention. Methodologically, the study explored various aspects, including study subjects, interventions, applied clinical outcomes, and statistical methods. Out of 258 studies, 12 were selected. Eight studies involved patients with HF, while the others used HF as an outcome. Datasets from the National Health Insurance Research Database were used in Taiwan, while electronic medical record data were used in China and Japan. EATM interventions have been found to be associated with lower mortality and readmission rates. One study indicated that an increased dose of Fuzi, a botanical drug, or prompt use of Fuzi after diagnosis led to a decreased mortality hazard ratio. In two studies examining readmission rates, a significant increase was observed in the non-exposed group, with odds ratios of 1.28 and 1.18. Additionally, in patients with breast cancer, the subdistribution hazard ratio for the occurrence of doxorubicin-induced HF was reduced to 0.69. Although cohort studies with survival analysis were common, methodological flaws, such as issues with statistical methods and HF diagnosis, were identified. Despite these challenges, the study observed an association between EATM and improved clinical outcomes in patients with HF, emphasizing the potential of RWD studies to complement randomized controlled trials, especially for longer-term follow-ups. These results provide foundational data for future RWD research.
1. Introduction
Heart failure (HF) is a complex clinical syndrome resulting from structural or functional abnormalities of the heart that damage the ability of the ventricles to fill and drain blood [1]. It involves various mechanisms, including myocardial stretching, matrix remodeling, neurohormonal activation, and inflammation [2,3,4]. The prevalence of HF in developed countries is approximately 1–2%, and is increasing owing to population growth and aging [5,6]. In particular, the mortality rate after 5 years of hospitalization for HF, a high-severity disease, is 42.3% [7]. HF arises from factors, such as high blood pressure, dilated cardiomyopathy, coronary artery heart disease, diabetes, and obesity, impairing heart function and leading to complications [1,8,9,10,11]. This multifactorial condition emphasizes the need for diverse approaches based on country-specific variations owing to significant geographical differences in etiology [12]. Although the standard treatment for HF includes drugs, such as angiotensin receptor blockers, beta-blockers, and diuretics, drug therapy has known side effects, including bradycardia and hypotension [1]. In cases of unsuccessful standard treatment, implanted cardioverter defibrillators (ICD), cardiac resynchronization therapy, and heart transplantation are required [1]. However, these interventions are accompanied by potential side effects, such as infection, arteriosclerosis, and thrombosis. Moreover, owing to the scarcity of donors, heart transplantation remains challenging, highlighting the need for complementary treatment strategies to prevent HF progression and manage complications [3,13].
In East Asia, interventions using East Asian traditional medicine (EATM), such as acupuncture, botanical drugs (herbal medicine), pharmacopuncture, and qigong, have been used to treat heart disease [14,15]. Research on heart function in HF has explored the use of acupuncture and moxibustion, with a combination of these interventions and conventional medication showing improvements in left ventricular ejection fraction (LVEF), cardiac output, 6-min walking test scores, and brain natriuretic peptide levels [16]. Botanical drugs have been used in patients with ischemic heart disease and angina pectoris, and Rhodiola is known to be effective in improving electrophysiology and symptoms in patients with ischemic heart disease [17]. Herbal drug injections have been demonstrated to be effective and safe for chronic heart failure (CHF) treatment when used in combination with traditional approaches [18]. However, the clinical characteristics of HF necessitate long-term follow-up, posing challenges for conducting extended clinical trials of EATM [19]. Although many surrogate outcomes have been evaluated in short-term clinical trials, assessing patient mortality, HF-related hospitalization, cardiovascular disease prevalence, and the use of ICD or cardiac resynchronization therapy requires long-term follow-up [19]. Therefore, a different approach is needed to identify the long-term clinical endpoints.
Despite the demonstrated efficacy of EATM interventions in HF, verifying long-term clinical outcomes has been hindered by the lack of resources for extensive clinical trials. Real-world data (RWD), including health insurance claims, hospital electronic medical records (EMRs), and registry data, offer an alternative to exploring the effects of specific interventions on long-term clinical outcomes without conducting clinical trials. In Taiwan, Korea, Japan, and China, RWD studies on the treatment effects of EATM intervention for HF are underway, using various epidemiological research methodologies, such as retrospective cohort or case-control studies based on diverse data sources. Nevertheless, an overview, scoping, and summary of RWD studies on HF have not been conducted. Therefore, we conducted a scoping review to explore RWD studies using EATM interventions to treat HF. This study aimed to explore the long-term effects of EATM intervention. Additionally, we analyzed the characteristics, advantages, and limitations of the RWD study design for HF and suggested future directions for follow-up studies.
2. Methods
This study followed the scoping review methodology developed by Arksey and O’Malley [20], chosen for its relevance in the exploration of a new topic involving RWD [21]. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extensions for Scoping Reviews guidelines were followed to develop this scoping review protocol [22]. The protocol for the review was recorded by the Open Science Framework and registered on 24 August 2022 (https://osf.io/wrc9d/ (accessed on 24 August 2022)).
2.1. Step 1: Checking Study Questions
The research team, comprising clinical research experts, Korean medicine specialists in circulatory diseases, and Korean medicine clinical researchers, conducted a literature search and specified the scope of the subject. The search addressed key inquiries about HF based on RWD. It provided valuable insights by examining the study design, identifying frequently used clinical outcomes, and evaluating the long-term effectiveness and safety of EATM interventions in HF. Additionally, the study scrutinized botanical drug regimens for HF treatment. It aimed to identify specific botanicals, distinguished by their scientific names, used to treat individuals with HF. Overall, these findings enhance our understanding of HF treatment in real-world clinical scenarios.
2.2. Step 2: Checking Relevant Studies
This review focused on peer-reviewed studies using RWD-based EATM interventions in patients with HF. The initial literature search was conducted in May 2022, and the final search, using the same strategy, was conducted in September 2023. The following databases were searched: MEDLINE via PubMed, EMBASE via Elsevier, Cochrane Central Register of Controlled Trials, Cumulative Index to Nursing and Allied Health Literature, and Allied and Complementary Medicine. The search strategies were discussed by clinical research experts and Korean medicine doctors, employing a combination of terms, including HF, RWD (“cohort” or “case-control” or “cross-sectional”), and EATM (“Chinese medicine” or “Kampo medicine” or “Korean medicine”). The search strategy incorporated various medical subject heading terms and synonyms, and detailed search formulas are provided in Supplementary Table S1.
2.3. Step 3: Study Selection
Three authors (JP, SB, and DS) independently performed the study selection. EndNote 20 was used to remove duplicates from the searched publications that included titles and abstracts. For studies identified as potentially relevant, the full text was checked to determine inclusion. All articles were extracted in Excel and categorized as either included or excluded based on predefined criteria, with reviewers providing reasons for the exclusion. Discrepancies were resolved through discussions with other researchers. The inclusion criteria were as follows: (1) longitudinal studies using RWD, such as prospective cohort, retrospective cohort, and case-control studies; (2) studies using EATM intervention; and (3) studies focused on patients with HF or the occurrence of HF. The exclusion criteria were as follows: (1) studies not following a longitudinal design but instead using a snapshot (cross-sectional) research approach, such as assessing medical usage status in a specific year; (2) survey research and biomarker development studies; (3) interventions conducted by non-physicians; and (4) non-RWD research, including randomized controlled trials (RCTs).
2.4. Step 4: Charting Data
The pilot data extraction sheet was completed through discussions with the research team. Following several pilot tests, the extracted items included general information about the study, data source and type of RWD study, HF diagnostic criteria, statistical methods for analyzing clinical outcomes, risk factors associated with HF prognosis, co-medications, HF-related clinical presentations, and detailed information about botanical drugs. Data extraction was independently performed by three reviewers (JP, SB, and DS), who cross-checked the data from all studies. Any discrepancies among the reviewers were resolved through discussions with other researchers (JL).
2.5. Step 5: Comparing, Summarizing, and Reporting Results
The extracted data were used to establish a comparison, synthesis, and summarization framework. Table 1 presents the characteristics of the included studies and Table 2 presents the research methodologies and statistical analysis techniques. The classification of clinical outcomes is detailed in Table 3, and the effectiveness and safety of the EATM are provided in Table 4. Table 5 and Table 6 present information on the botanical drug used and its components, while specifics regarding usage frequency and regimen analysis are available in the Supplementary Materials.

Table 1.
Characteristics of the included studies with key questions and real-world data sources.

Table 2.
Diagnosis and patient selection criteria, and statistical analysis methods with considered covariates.

Table 3.
Types of clinical outcomes used in included studies.

Table 4.
Effectiveness of East Asian traditional medicine intervention in included studies.

Table 5.
Components of prescribed botanical drugs (herbal medicines) in the included studies.

Table 6.
Botanical drugs (herbal medicines) used in the included studies.
3. Results
3.1. Characteristics of the Included Studies
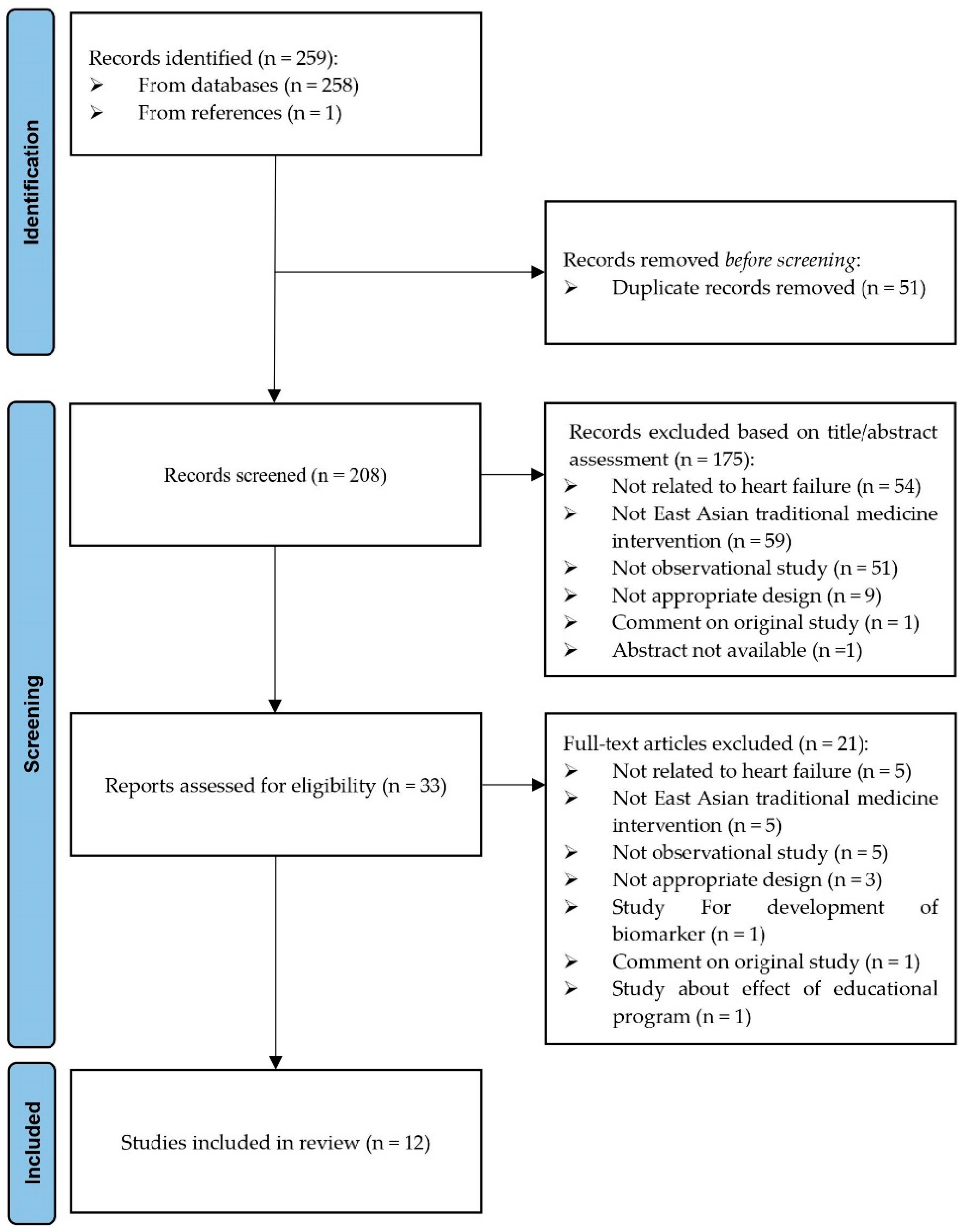
Of the 258 studies identified, 12 were selected (Figure 1), of which 8 were conducted in patients with HF [23,24,25,26,27,28,29,30]. Of the remaining four studies, HF occurrence was the primary outcome in two [31,32] and secondary outcome in the other two studies [33,34]. Among the eight studies involving patients with HF, four included patients with CHF [23,24,26,28], one included patients with acute HF [25], and one included patients with acute decompensated HF [27]. Two studies included unspecified patients with HF [29,30]. Geographically, the studies were distributed as follows: six in China [24,26,27,28,33,34], five in Taiwan [23,29,30,31,32], and one in Japan [25]. The National Health Insurance Research Database was used in Taiwan, whereas in the other two countries, EMR data from hospitals was used (Table 1).
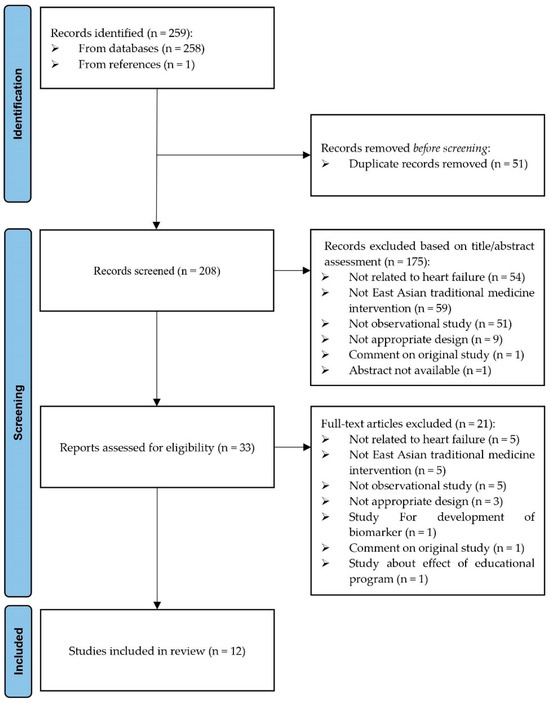
Figure 1.
PRISMA flow chart: Selection of studies for scoping review.
3.2. Diagnosis and Patient Selection Criteria, and Statistical Analysis Methods
Regarding methodological and statistical analyses, five studies conducted survival analysis using propensity score matching [23,24,29,31,32]; some included a dose–response analysis to explore causality [23]. Independent t-tests or chi-square tests (which did not consider the time-to-event analysis) were used to compare the mean or ratio of clinical indicators [27,28,29,33,34]. Logistic regression analysis was used to identify the factors influencing the occurrence of cardiac events [24,25,33,34]. Regression analysis was also conducted to predict the factors influencing the use of traditional Chinese medicine [27,30,32,33,34]. One study performed multivariate logistic regression analyses and presented nomograms, receiver operating characteristic curves, and clinical decision curve analyses to construct a model for predicting survival [26]. Table 2 presents the covariates used in each study.
3.3. Clinical Outcomes
The clinical outcomes used were classified into mortality, cardiovascular events (including HF occurrence), hospitalization, cardiac function, medical cost, safety, and dose–response relation (Table 3).
Although its effect on mortality remains debatable, EATM intervention in patients with HF appears to reduce mortality. In the study by Tai et al., the hazard ratio was 0.99 (95% confidence interval, 0.76–1.27), indicating no significant reduction in mortality [23]. However, other studies reported a lower 5-year mortality rate in the TCM group than in the control group, with a hazard ratio of 0.24 [29] or odds ratio of 0.19 [26]. In patients with myocardial infarction (MI), the odds ratio of cardiogenic death in the control group ranged from 1.34 to 2.64 [33,34]. Regarding hospital visits, the overall TCM use was associated with a reduction in readmission rates. Guan et al. showed that the readmission rate due to HF was significantly lower in a TCM user group [24]. Another study comparing TCM users of Fuzi (a medicinal botanical drug) versus TCM users without Fuzi found no significant differences in admission rates to intensive care units and hospitalization rates due to HF, MI, and stroke [23]. However, the study noted a trend indicating a lower mortality rate associated with the prompt use of Fuzi after the diagnosis of HF and an increase in Fuzi dosage [23]. Among individuals undergoing doxorubicin chemotherapy for breast cancer, TCM use was associated with a lower incidence of CHF [31]. Another study found a lower incidence of HF when botanical drugs were used for over 180 days in patients with hypertension [32]. Among patients with MI, the TCM group had a lower incidence of acute HF [33,34]. Regarding cardiac function, the TCM group showed a greater improvement in NYHA classification and LVEF [24]. In another study, TCM use had no significant effect on LVDD and cardiac index but was associated with improvement in LVEF, CO, every cardiac output, and 6-min walking test scores [28]. Regarding medical costs, expenses for outpatient treatment or hospitalization within one year after HF diagnosis were significantly lower in a TCM user group [29]. No significant adverse events were reported in the available literature (Table 4) [23,27,28].
3.4. Botanical Drug (Herbal Medicine) Regimens
Of the 12 studies, 10 reported the use of botanical drugs prescribed in various forms such as decoctions, pills, capsules, and injections for treatment [23,24,27,28,29,30,31,32,33,34]. One study assessed the prevalence of the use of medications that can cause or exacerbate HF [25]. The botanical drugs used in each study are listed in Table 5 and Table 6. Of the 10 studies, Panax ginseng C. A. Meyer (Renshen) was used in 8, followed by Astragalus membranaceus Bunge (Huangqi) and Salvia miltiorrhiza Bunge (Danshen). Additionally, Glycyrrhiza uralensis Fisch. (Gancao) was employed in six studies (Table 5 and Supplementary Table S2). Detailed information on the prescribed botanical drugs is provided in Supplementary Table S3.
4. Discussion
In this study, a scoping review method was used to investigate the RWD research status of EATM interventions for HF. Among the 12 selected studies, 8 were conducted in patients with HF [23,24,25,26,27,28,29,30], 2 used HF as the primary outcome [31,32], and 2 used HF as the secondary outcome [33,34]. All interventions were based on traditional botanical drugs, including TCM and Kampo. Mortality was the most frequently used outcome variable [23,24,25,26,27,29,31,33,34]. Overall, the use of EATM was associated with lower mortality and readmission rates. Furthermore, TCM use in patients with other conditions (such as breast cancer, hypertension, and MI) was associated with a lower incidence of HF. Among the 12 studies, 10 confirmed the use of botanical drugs for treatment, with Panax ginseng C. A. Meyer being the most used. The incidence of adverse events was not higher in the TCM group.
Regarding cost-effectiveness, one year after the occurrence of HF, the TCM group exhibited lower medical costs and shorter hospital stays. However, five years after the onset of HF, the TCM group experienced higher costs, accompanied by an increased frequency of outpatient visits. Additionally, traditional medicine is commonly used concurrently with standard treatments, making it costlier than groups receiving only standard treatments. Therefore, economic evaluations should consider not only direct medical costs but also direct non-medical costs, quality-adjusted life years, and other relevant factors [35,36]. The criteria for economic evaluation may vary by country, emphasizing the need for additional country-specific research.
Regarding the herbs prescribed for treatment, Panax ginseng C. A. Meyer (Renshen), Astragalus membranaceus Bunge (Huangqi), and Salvia miltiorrhiza Bunge (Danshen) were predominantly used. Panax ginseng C. A. Meyer (Renshen), known for its ability to tonify qi and yang, has diverse pharmacological effects, regulates blood glucose and cholesterol levels, and lowers blood pressure, thereby influencing the risk factors associated with cardiovascular diseases [37,38]. Similar to Panax ginseng C. A. Meyer, Astragalus membranaceus Bunge (Huangqi), which tonifies qi, is reported to have anti-inflammatory, antioxidant, vascular protective, and diuretic effects [39,40,41]. In China, the combination of Panax ginseng C. A. Meyer (Renshen) and Astragalus membranaceus Bunge (Huangqi) is commonly used for CHF because of the synergistic effects of the combination of the two herbs [40]. Salvia miltiorrhiza Bunge (Danshen), known for its blood-activating and stasis-resolving characteristics, is reported to exert cardiac protective effects attributed to its antioxidative, anti-inflammatory, and antiapoptotic properties [42]. Guo et al. conducted data mining to report the prescription rules for herbs commonly used for preserving ejection fraction in HF [43]. All three of these herbs were included, highlighting the primary functions of herbal medicine as qi-replenishing, yang-warming, blood-activating, and diuresis-inducing. This suggests that the appropriateness of considering these three herbs for HF aligns with previous findings and our research findings. Despite the positive therapeutic effects of botanical drugs on cardiovascular health, six studies in the analysis included interventions with concurrent standard treatments. Hence, it is crucial to consider the potential interaction between botanical drugs and standard treatments, rather than attributing effects solely to botanical drugs.
In a previous RCT, the traditional botanical drug Qili Qiangxin capsule reduced N-terminal-pro-brain natriuretic peptide levels, although all-cause mortality was not explored owing to the relatively short duration of the RCT [44]. In contrast, our study employed a retrospective cohort design with a long-term follow-up, allowing for the analysis of all-cause mortality [23,25,26,29,31]. We observed differences in the treatment effects between RWDs and RCTs. Regarding readmission, an RCT by Li et al. on the effect of Qili Qiangxin capsules on HF reported a readmission rate of 3.28% in the treatment group (8 of 244 patients) versus 6.48% in the control group (16 of 247 patients) [44]. However, in an RWD study by Guan et al. who investigated the effect of Shenmai injection on CHF, the readmission rate was 32.37% in the treatment group (146 out of 451 patients) versus 38.93% in the control group (232 of 596 patients) [24]. Although participant baseline characteristics, study settings, and interventions differed slightly, the effect size of TCM treatment varied considerably between RWD and RCT design studies, despite measuring the same outcome variable. Similar differences between RWD and RCT results have been observed in other studies [45,46,47]. RWD studies analyze larger sample sizes over longer periods, catering to a more diverse population, and can yield different effect estimates even when the outcome variable is the same as in existing RCTs. Generalizing and predicting which research design will provide a more significant effect on the intervention between RCT and RWD is challenging. However, unlike RCTs, observational studies cannot establish causality and can only demonstrate an association. Therefore, both research designs should be used complementarily.
Some problems have not been described in detail regarding study subjects, and previous RCTs have been criticized for not providing detailed information on HF diagnoses [48]. A review related to the existing RCTs treating HF has highlighted the ambiguity in distinguishing between HF with reduced (LVEF ≤ 40%) and preserved (LVEF ≥ 50%) ejection fractions [19], which have different treatment strategies and prognoses [49]. Furthermore, the evaluation of cardiac function using the NYHA class or ejection fraction has not been widely used. These indices can significantly influence prognosis and treatment response [49]. Consequently, follow-up studies should explicitly present patient characteristics by providing a detailed diagnosis of individuals with HF and an assessment of cardiac function.
The selection of the exposed and non-exposed groups lacked the appropriate utilization of physical, radiological, and biochemical indices, leading to limitations in assessing comparability between the groups. This limitation might be inherent in claims data, and there could be systematic differences between users and non-users of EATM. Although statistical adjustments were implemented in the analysis stage, such as regression, efforts to minimize bias in subject group selection are crucial. Another issue pertains to the statistical analysis methods. To analyze time-to-event data, survival analysis, such as Cox proportional hazard regression, should be applied. However, several studies used mean comparison (t-test) or frequency comparison (chi-square test) instead, representing a methodological error [28,29,33,34]. Statistical analysis methods suitable for the long-term follow-up of RWD research should be considered. Additionally, study design considerations, such as setting the first diagnosis time as the index date rather than the date of the first administration of the treatment group, should be adopted to avoid immortal bias [50,51]. In addition, as in the study by Tai et al. included in this review, dose–response analysis should be actively applied to explore causality [23].
To overcome the limitations observed in existing observational studies on HF, the following recommendations are proposed. First, regarding health insurance data, the inadequacy of baseline characteristic information that can be used as covariates is noted, while EMR data from hospitals lacks long-term clinical outcome data. Therefore, there is a need to integrate these two data sources in future studies. Additionally, synchronizing pattern identification should be considered as it influences the treatment strategy in RWD studies [52]. Second, conducting dose–response analyses is essential to strengthen the evidence of association. Tai et al.’s study employed the restricted cubic spline method in evaluating dose or treatment initiation time [23]. Whereas previous research categorized participants into quartiles, adopting an analysis method that maximizes the advantages of continuous variable data is crucial. Third, it is emphasized that existing HF clinical trials predominantly used surrogate outcomes such as echocardiography, symptoms, and blood tests. However, outcomes such as cardiogenic death or HF readmission, which could provide insights into long-term prognosis, should be actively incorporated. Lastly, quantitative synthesis faces challenges due to the different outcomes reported in each study. A study on the core outcome set for a clinical trial of TCM for HF is currently underway [53]. However, extending this set is crucial when using RWD. Accumulating evidence with common outcomes offers the potential for future quantitative synthesis in observational studies using RWD.
To our knowledge, this study has the advantage of being the first literature review on RWD-based EATM interventions for HF. This study not only explored the effectiveness, but also presented the applied design, regimen, study subjects, and statistical methods. In addition, the outcomes and covariates used are described in detail to provide fundamental data to those who would conduct RWD studies using EATM for HF in the future. However, because of the inherent limitations of the observational study, this research also has fundamental constraints. First, the study’s findings only suggest an association and do not confirm the efficacy of EATM. Whether the effect is from the botanical drug alone or synergistic with standard treatment is unclear; thus, it requires supplementation through experimental studies. Additionally, the included studies lacked precise dosages or administration details, highlighting the need for more accurate descriptions in further research. Second, analyzing safety or compliance was challenging owing to data limitations. To overcome these limitations, future studies should incorporate health insurance data and hospital EMRs to establish diverse measures for evaluating safety and compliance, including laboratory tests and confirmation of medication adherence. Third, the study’s limitations include its applicability beyond East Asia, as it focuses on traditional medicine for HF in East Asian populations. A comprehensive review is needed to determine if the findings apply universally or have geographic specificity. Fourth, the search strategy, encompassing “Chinese medicine”, “Kampo medicine”, and “Korean medicine”, aimed to investigate overall traditional medicine status. However, the extracted studies only broadly assessed the exposure to traditional medicine or included interventions based on herbs such as injections and decoctions, omitting diverse EATM interventions such as acupuncture and moxibustion. This is considered a limitation of RWD studies because, in retrospective studies based on health insurance data or hospital EMRs, the exact treatment procedure cannot be accurately determined. That the treatment was not mentioned in the paper does not imply non-administration [54,55]. Thus, a more comprehensive evaluation of various East Asian traditional medicine interventions is needed through registries, prospective cohorts, and other forward-looking research.
5. Conclusions
This study investigated mortality, readmission rates, cardiac function, and medical expenses as the clinical endpoints of EATM treatment for HF. The review results showed that EATM treatment for HF was associated with reduced mortality and readmission rates. Observational studies using RWD can supplement the limitations of existing RCTs by examining clinical endpoints that require long-term follow-ups. However, RWD studies need to measure objective covariates, such as the detailed classification of HF and cardiac function evaluation, to enhance the reliability of findings. Efforts should be made to reduce bias in the selection of study subjects, and time-to-event analytical statistical methods need supplementation. The data from our study can serve as fundamental information for future research endeavors.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare12010061/s1, Supplementary Table S1: Literature searching strategy; Supplementary Table S2: Frequency of used botanical drugs (herbal medicines) in the studies; Supplementary Table S3: Analysis of botanical drug (herbal medicine) regimens.
Author Contributions
H.C. and J.L. conceptualized the manuscript and contributed to data curation; J.P., H.J., S.K. and S.B. contributed to the methodology and original drafting of the manuscript; D.S., H.J., I.Y. and J.L. reviewed the writing and contributed to manuscript drafting. All authors have read and agreed to the published version of the manuscript.
Funding
This work received support from the National Research Foundation of Korea, grant funded by the Korean government (No.: 2022R1C1C2008738). Additionally, the research was backed by a grant from the Korea Health Technology Project through the Korea Health Industry Development Institute, funded by the Ministry of Health and Welfare, Republic of Korea (Grant No. HF23C0063). The Basic Science Research Program, funded by the Ministry of Education through the National Research Foundation of Korea (NRF) (No. RS-2023-00270676), also provided support. Furthermore, this work received assistance from a grant from the National Medical Center, Republic of Korea (Grant Number: NMC2023-MS-02).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data that support the findings of this study are available from the corresponding authors upon reasonable request.
Conflicts of Interest
There are no conflicts of interest.
References
- Writing Committee Members; ACC/AHA Joint Committee Members. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure. J. Card. Fail. 2022, 28, e1–e167. [Google Scholar] [CrossRef] [PubMed]
- Halade, G.V.; Lee, D.H. Inflammation and Resolution Signaling in Cardiac Repair and Heart Failure. eBioMedicine 2022, 79, 103992. [Google Scholar] [CrossRef] [PubMed]
- The Korean Society of Heart Failure. 2022 KSHF Guideline for the Management of HEART FAILURE; Korean Society of Heart Failure: Seoul, Republic of Korea, 2022; Available online: https://www.kshf.or.kr/ (accessed on 6 September 2022).
- Li, L.; Zhao, Q.; Kong, W. Extracellular Matrix Remodeling and Cardiac Fibrosis. Matrix Biol. 2018, 68–69, 490–506. [Google Scholar] [CrossRef] [PubMed]
- Groenewegen, A.; Rutten, F.H.; Mosterd, A.; Hoes, A.W. Epidemiology of Heart Failure. Eur. J. Heart Fail. 2020, 22, 1342–1356. [Google Scholar] [CrossRef] [PubMed]
- Roth, G.A.; Forouzanfar, M.H.; Moran, A.E.; Barber, R.; Nguyen, G.; Feigin, V.L.; Naghavi, M.; Mensah, G.A.; Murray, C.J.L. Demographic and Epidemiologic Drivers of Global Cardiovascular Mortality. N. Engl. J. Med. 2015, 372, 1333–1341. [Google Scholar] [CrossRef] [PubMed]
- Loehr, L.R.; Rosamond, W.D.; Chang, P.P.; Folsom, A.R.; Chambless, L.E. Heart Failure Incidence and Survival (from the Atherosclerosis Risk in Communities Study). Am. J. Cardiol. 2008, 101, 1016–1022. [Google Scholar] [CrossRef] [PubMed]
- Roger, V.L. Epidemiology of Heart Failure: A Contemporary Perspective. Circ. Res. 2021, 128, 1421–1434. [Google Scholar] [CrossRef]
- Carbone, S.; Lavie, C.J.; Elagizi, A.; Arena, R.; Ventura, H.O. The Impact of Obesity in Heart Failure. Cardiol. Clin. 2022, 40, 209–218. [Google Scholar] [CrossRef]
- Seol, H.; Kim, J.S. Prevalence, Mechanisms, and Management of Ischemic Stroke in Heart Failure Patients. Semin. Neurol. 2021, 41, 340–347. [Google Scholar] [CrossRef]
- Slivnick, J.; Lampert, B.C. Hypertension and Heart Failure. Heart Fail. Clin. 2019, 15, 531–541. [Google Scholar] [CrossRef]
- Savarese, G.; Becher, P.M.; Lund, L.H.; Seferovic, P.; Rosano, G.M.C.; Coats, A.J.S. Global Burden of Heart Failure: A Comprehensive and Updated Review of Epidemiology. Cardiovasc. Res. 2023, 118, 3272–3287. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.; Duan, C.; Yang, Y.; Yuan, G.; Zhou, Y.; Zhu, X.; Wei, N.; Hu, Y. Heart Transplantation: A Bibliometric Review from 1990–2021. Curr. Probl. Cardiol. 2022, 47, 101176. [Google Scholar] [CrossRef] [PubMed]
- Hao, P.; Jiang, F.; Cheng, J.; Ma, L.; Zhang, Y.; Zhao, Y. Traditional Chinese Medicine for Cardiovascular Disease: Evidence and Potential Mechanisms. J. Am. Coll. Cardiol. 2017, 69, 2952–2966. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Kim, T.-H.; Leem, J. Acupuncture for Heart Failure: A Systematic Review of Clinical Studies. Int. J. Cardiol. 2016, 222, 321–331. [Google Scholar] [CrossRef] [PubMed]
- Liang, B.; Yan, C.; Zhang, L.; Yang, Z.; Wang, L.; Xian, S.; Lu, L. The Effect of Acupuncture and Moxibustion on Heart Function in Heart Failure Patients: A Systematic Review and Meta-Analysis. Evid. Based Complement. Alternat. Med. 2019, 2019, 6074967. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Hou, J.; Yan, S.; Zhu, L.; Wang, Y.; Du, H.; Zhang, W.; Zhao, H. Chinese Herbal Medicine Therapy for Coronary Heart Disease Complicated with Anxiety: A Systematic Review of Randomized Controlled Trials. J. Tradit. Chin. Med. 2020, 40, 1–16. [Google Scholar]
- Shi, L.; Xie, Y.; Liao, X.; Chai, Y.; Luo, Y. Shenmai Injection as an Adjuvant Treatment for Chronic Cor Pulmonale Heart Failure: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. BMC Complement. Altern. Med. 2015, 15, 418. [Google Scholar] [CrossRef]
- Hu, J.; Qiu, R.; Li, C.; Li, M.; Dai, Q.; Chen, S.; Zhao, C.; Shang, H. Problems with the Outcome Measures in Randomized Controlled Trials of Traditional Chinese Medicine in Treating Chronic Heart Failure Caused by Coronary Heart Disease: A Systematic Review. BMC Complement. Med. Ther. 2021, 21, 217. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping Studies: Towards a Methodological Framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic Review or Scoping Review? Guidance for Authors When Choosing between a Systematic or Scoping Review Approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Tai, C.-J.; El-Shazly, M.; Yang, Y.-H.; Tsai, Y.-H.; Csupor, D.; Hohmann, J.; Wu, Y.-C.; Tseng, T.-G.; Chang, F.-R.; Wang, H.-C. The Effectiveness of Fuzi in Combination with Routine Heart Failure Treatment on Chronic Heart Failure Patients. J. Ethnopharmacol. 2022, 289, 115040. [Google Scholar] [CrossRef] [PubMed]
- Guan, H.; Dai, G.; Gao, W.; Zhang, T.; Sun, C.; Ren, L.; Hou, X.; Liu, Z. Effect of Shenmai Injection on Long-Term Prognosis of Patients with Chronic Heart Failure: A Multicenter, Large Sample Capacity, Long-Term Follow-Up Retrospective Cohort Study. Chin. J. Integr. Med. 2022, 28, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Komagamine, J.; Kaminaga, M.; Omori, T.; Tatsumi, S. The Use of Kampo Medications That May Cause Heart Failure in Hospitalized Acute Heart Failure Patients in a Japanese Hospital. J. Gen. Fam. Med. 2021, 22, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Guan, H.; Dai, G.-H.; Gao, W.-L.; Zhao, X.; Cai, Z.-H.; Zhang, J.-Z.; Yao, J.-X. A 5-Year Survival Prediction Model for Chronic Heart Failure Patients Induced by Coronary Heart Disease with Traditional Chinese Medicine Intervention. Evid. Based Complement. Alternat. Med. 2021, 2021, 4381256. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Spatz, E.S.; Tan, Q.; Liu, S.; Lu, Y.; Masoudi, F.A.; Schulz, W.L.; Krumholz, H.M.; Li, J.; Group, C.P.C. Traditional Chinese Medicine Use in the Treatment of Acute Heart Failure in Western Medicine Hospitals in China: Analysis from the China PEACE Retrospective Heart Failure Study. J. Am. Heart Assoc. 2019, 8, e012776. [Google Scholar] [CrossRef]
- Sui, Y.; Liu, L.; Tian, Q.; Deng, X.; Zhang, Y.; Li, Z. A Retrospective Study of Traditional Chinese Medicine as an Adjunctive Therapy for Patients with Chronic Heart Failure. Medicine 2018, 97, e11696. [Google Scholar] [CrossRef]
- Tsai, M.-Y.; Hu, W.-L.; Chiang, J.-H.; Huang, Y.-C.; Chen, S.-Y.; Hung, Y.-C.; Chen, Y.-H. Improved Medical Expenditure and Survival with Integration of Traditional Chinese Medicine Treatment in Patients with Heart Failure: A Nationwide Population-Based Cohort Study. Oncotarget 2017, 8, 90465. [Google Scholar] [CrossRef]
- Tsai, M.-Y.; Hu, W.-L.; Lin, C.-C.; Lee, Y.-C.; Chen, S.-Y.; Hung, Y.-C.; Chen, Y.-H. Prescription Pattern of Chinese Herbal Products for Heart Failure in Taiwan: A Population-Based Study. Int. J. Cardiol. 2017, 228, 90–96. [Google Scholar] [CrossRef]
- Huang, C.-H.; Chang, H.-P.; Su, S.-Y.; Chen, W.-K.; Chang, Y.-J.; Lee, Y.-C.; Kuo, Y.-J. Traditional Chinese Medicine Is Associated with a Decreased Risk of Heart Failure in Breast Cancer Patients Receiving Doxorubicin Treatment. J. Ethnopharmacol. 2019, 229, 15–21. [Google Scholar] [CrossRef]
- Liu, C.-T.; Hung, I.-L.; Hsu, C.Y.; Hu, K.-C.; Chen, Y.-H.; Tsai, M.-Y. Chinese Herbal Medicine Reduces the Risk of Heart Failure in Hypertensive Patients: A Nationwide, Retrospective, Cohort Study. Front. Cardiovasc. Med. 2022, 9, 922728. [Google Scholar] [CrossRef] [PubMed]
- Guohua, D.; Wulin, G.; Dongxue, B.; Chunhua, L.; Yuhan, L.; Ning, W.; Chen, Z. Efficacy of Traditional Chinese Medicine in Patients with Acute Myocardial Infarction Suffering from Diabetes Mellitus. J. Tradit. Chin. Med. 2018, 38, 412–418. [Google Scholar] [CrossRef]
- Wulin, G.; Guohua, D.; Tong, Z.; Dongxue, B.; Chunhua, L.; Xiaojing, S.; Fang, Z.; Chen, Z. Tonifying Qi and Activating Blood Circulation in Terms of Traditional Chinese Medicine: Their Effects in Patients with Myocardial Infarction. J. Tradit. Chin. Med. 2018, 38, 726–732. [Google Scholar] [CrossRef]
- Chen, Y. Health Technology Assessment and Economic Evaluation: Is It Applicable for the Traditional Medicine? Integr. Med. Res. 2022, 11, 100756. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Wu, E.Q.; Ahn, J.; Kamae, I.; Xie, J.; Yang, H. The Development of Health Technology Assessment in Asia: Current Status and Future Trends. Value Health Reg. Issues 2020, 21, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Aminifard, T.; Razavi, B.M.; Hosseinzadeh, H. The Effects of Ginseng on the Metabolic Syndrome: An Updated Review. Food Sci. Nutr. 2021, 9, 5293–5311. [Google Scholar] [CrossRef] [PubMed]
- Tang, M.-M.; Zhao, S.-T.; Li, R.-Q.; Hou, W. Therapeutic Mechanisms of Ginseng in Coronary Heart Disease. Front. Pharmacol. 2023, 14, 1271029. [Google Scholar] [CrossRef]
- Wang, P.; Wang, Z.; Zhang, Z.; Cao, H.; Kong, L.; Ma, W.; Ren, W. A Review of the Botany, Phytochemistry, Traditional Uses, Pharmacology, Toxicology, and Quality Control of the Astragalus Memeranaceus. Front. Pharmacol. 2023, 14, 1242318. [Google Scholar] [CrossRef]
- Xu, J.; Zhang, Z.; Zhou, K.; Li, Y.; Wan, J.; Mao, T.; Ji, X.; Liu, J.; Lin, Q. Integration of Network Pharmacology and Molecular Docking Technology Reveals the Mechanism of the Herbal Pairing of Codonopsis Pilosula (Franch.) Nannf and Astragalus Membranaceus (Fisch.) Bge on Chronic Heart Failure. Ann. Palliat. Med. 2021, 10, 7942–7959. [Google Scholar] [CrossRef]
- Fu, J.; Wang, Z.; Huang, L.; Zheng, S.; Wang, D.; Chen, S.; Zhang, H.; Yang, S. Review of the Botanical Characteristics, Phytochemistry, and Pharmacology of Astragalus Membranes (Huangqi). Phytother. Res. 2014, 28, 1275–1283. [Google Scholar] [CrossRef]
- Wang, Q.; Li, J.; Chu, X.; Jiang, X.; Zhang, C.; Liu, F.; Zhang, X.; Li, Y.; Shen, Q.; Pang, B. Potential Chemoprotective Effects of Active Ingredients in Salvia Miltiorrhiza on Doxorubicin-Induced Cardiotoxicity: A Systematic Review of in Vitro and in Vivo Studies. Front. Cardiovasc. Med. 2023, 10, 1267525. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.; Wang, J.; Peng, G.; Li, P.; Zhu, M. A Data Mining-Based Study on Medication Rules of Chinese Herbs to Treat Heart Failure with Preserved Ejection Fraction. Chin. J. Integr. Med. 2022, 28, 847–854. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhang, J.; Huang, J.; Ma, A.; Yang, J.; Li, W.; Wu, Z.; Yao, C.; Zhang, Y.; Yao, W.; et al. A Multicenter, Randomized, Double-Blind, Parallel-Group, Placebo-Controlled Study of the Effects of Qili Qiangxin Capsules in Patients with Chronic Heart Failure. J. Am. Coll. Cardiol. 2013, 62, 1065–1072. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Ye, L.; Bian, J.; Ma, L.; Zheng, C.; Guo, H. Effect of Jiawei Shenfu Decoction on Tumor Necrosis Factor-Alpha and Nuclear Factor-Kappa B in Patients Who Have Chronic Heart Failure with Syndromes of Deficiency of Heart Yang. J. Tradit. Chin. Med. 2019, 39, 418–424. [Google Scholar] [PubMed]
- Xian, S.; Yang, Z.; Lee, J.; Jiang, Z.; Ye, X.; Luo, L.; Jin, L.; Yang, T.; Ye, S.; Lu, D. A Randomized, Double-Blind, Multicenter, Placebo-Controlled Clinical Study on the Efficacy and Safety of Shenmai Injection in Patients with Chronic Heart Failure. J. Ethnopharmacol. 2016, 186, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Xian, S.; Yang, Z.; Ren, P.; Ye, X.; Ye, S.; Wang, Q.; Wang, Z.; Shen, S.; Huang, X. Effect of Yangxinkang Tablets on Chronic Heart Failure: A Multi-Center Randomized Double-Blind Placebo-Controlled Trial. Chin. J. Integr. Med. 2015, 21, 733–742. [Google Scholar] [CrossRef] [PubMed]
- Leem, J.; Lee, S.M.K.; Park, J.H.; Lee, S.; Chung, H.; Lee, J.M.; Kim, W.; Lee, S.; Woo, J.S. Efficacy and Safety of Electroacupuncture in Acute Decompensated Heart Failure: A Study Protocol for a Randomized, Patient- and Assessor-Blinded, Sham Controlled Trial. BMC Complement. Altern. Med. 2017, 17, 361. [Google Scholar] [CrossRef] [PubMed]
- 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Available online: https://www.ahajournals.org/doi/epub/10.1161/CIR.0000000000001063 (accessed on 6 September 2022).
- Yadav, K.; Lewis, R.J. Immortal Time Bias in Observational Studies. JAMA 2021, 325, 686–687. [Google Scholar] [CrossRef]
- Tyrer, F.; Bhaskaran, K.; Rutherford, M.J. Immortal Time Bias for Life-Long Conditions in Retrospective Observational Studies Using Electronic Health Records. BMC Med. Res. Methodol. 2022, 22, 86. [Google Scholar] [CrossRef]
- Kim, S.-H.; Jeong, J.-H.; Lim, J.-H.; Kim, B.-K. Acupuncture Using Pattern-Identification for the Treatment of Insomnia Disorder: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Integr. Med. Res. 2019, 8, 216–226. [Google Scholar] [CrossRef]
- Zhang, M.; Chua, H.Z.; Zhang, J.; Niu, B.; Zheng, W.; Li, K.; Zhang, B. Developing a Core Outcome Set on Traditional Chinese Medicine (COS-TCM) for Chronic Heart Failure (CHF): A Study Protocol. BMJ Open 2021, 11, e047148. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-J.; Lim, Y.-C.; Lee, Y.-S.; Kwon, S.; Lee, Y.J.; Ha, I.-H. Analysis of Medical Service Utilization for Post-Stroke Sequelae in Korea between 2016 and 2018: A Cross-Sectional Study. Sci. Rep. 2022, 12, 20501. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.; Yeo, S.; Lim, S. Effects of Acupuncture on Cardiovascular Risks in Patients with Hypertension: A Korean Cohort Study. Acupunct. Med. 2021, 39, 116–125. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).