Iron Deficiency as a Factor of Worse Prognosis in Patients with Acute Myocardial Infarction
Abstract
:1. Introduction
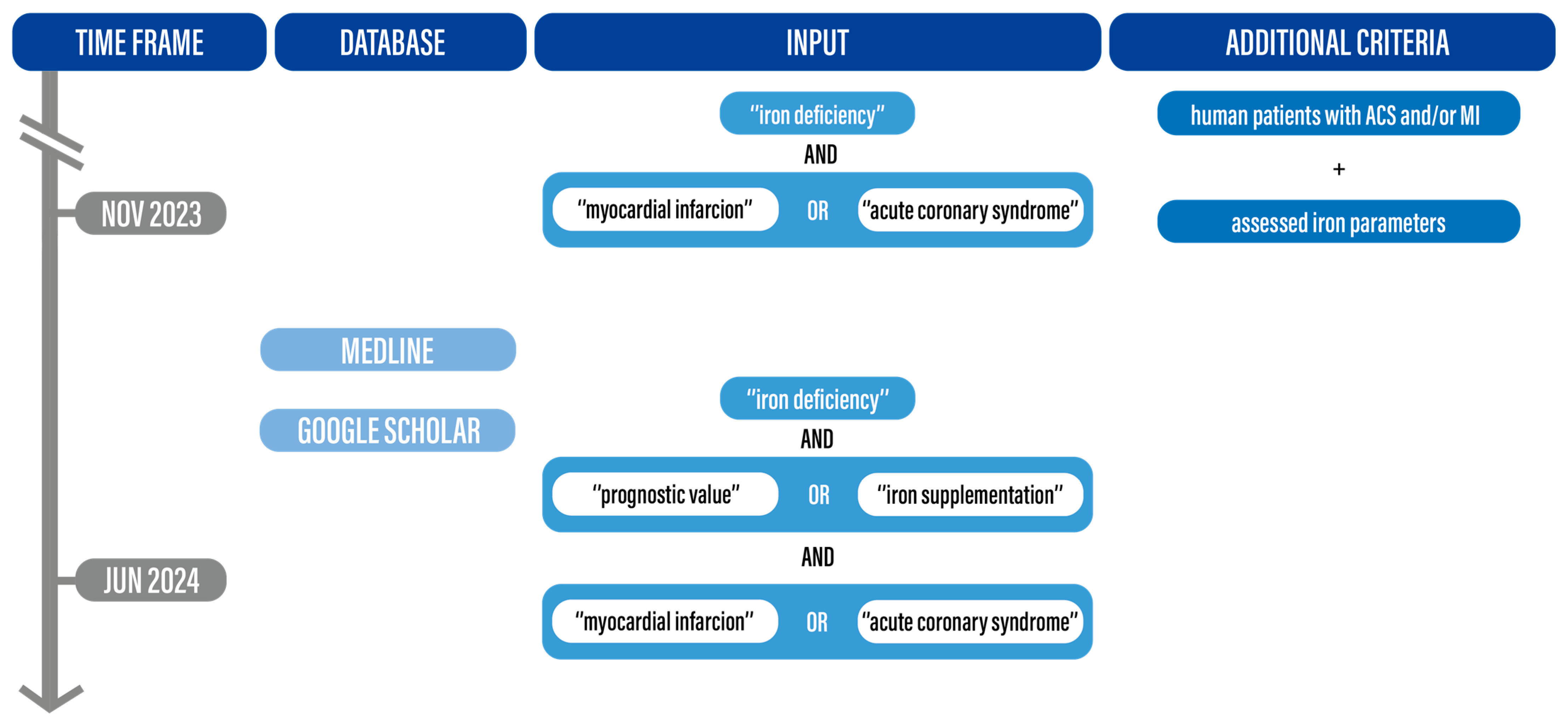
2. Materials and Methods
3. Pathophysiology of Iron Deficiency in Patients with Coronary Artery Disease
3.1. Physiology of Iron Metabolism
3.2. Etiology and Pathogenesis of Iron Deficiency in Cardiovascular Disease
3.3. Iron Deficiency and Ischemia-Related Cardiomyocyte Damage
4. Diagnosis
5. Iron Deficiency and Prognosis in Acute Coronary Syndromes
6. Iron Supplementation and ACS
7. Discussion
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| ACS | acute coronary syndrome |
| AMI | acute myocardial infarction |
| CABG | coronary artery bypass grafting |
| CAD | coronary artery disease |
| CI | confidence interval |
| CMR | cardiac magnetic resonance imaging |
| CRP | C-reactive protein |
| CVD | cardiovascular diseases |
| DMT1 | divalent metal transporter 1 |
| eNOS | endothelial nitric oxide synthase |
| EF | ejection fraction |
| Fer | ferritin |
| FPN | transcription ferroportin |
| FPN1 | transcription ferroportin 1 |
| HF | heart failure |
| HR | hazard ratio |
| ID | iron deficiency |
| IQR | interquartile range |
| LV | left ventricle |
| LVEF | left ventricular ejection fraction |
| MI | myocardial infarction |
| MMP | metalloproteinase |
| NCX | Na+/Ca2+ exchanger |
| n/s | not specified |
| NSTEMI | non-ST-elevated myocardial infraction |
| NT-proBNP | N-terminal pro B-type natriuretic peptide |
| NYHA | New York Heart Association |
| OR | odds ratio |
| PCI | percutaneous intervention |
| PKG | protein kinase-G |
| QOL | quality of life |
| ROS | reactive oxygen species |
| RR | risk ratio |
| RyR2 | ryanodine receptor 2 |
| SER | sarcoplasmic reticulum |
| SERCA 2 | sarcoplasmic reticulum Ca2+-adenosine triphosphatase |
| sGC | soluble guanylate cyclase |
| STEMI | ST-elevated myocardial infarction |
| sTFR | soluble transferrin receptor |
| Tf | transferrin |
| TfR1 | transferrin receptor 1 |
| TIBC | total iron binding capacity |
| TIMP | tissue inhibitor of metalloproteinase |
| TSAT | transferrin saturation |
| UA | unstable angina |
References
- WHO Factsheet on Cardiovascular Diseases. Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 1 July 2024).
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on Cardiovascular Disease Prevention in Clinical Practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- Pasricha, S.R.; Tye-Din, J.; Muckenthaler, M.U.; Swinkels, D.W. Iron Deficiency. Lancet 2021, 397, 233–248. [Google Scholar] [PubMed]
- Pasricha, S.S.; Flecknoe-Brown, S.C.; Allen, K.J.; Gibson, P.R.; McMahon, L.P.; Olynyk, J.K.; Roger, S.D.; Savoia, H.F.; Tampi, R.; Thomson, A.R.; et al. Diagnosis and Management of Iron Deficiency Anaemia: A Clinical Update. Med. J. Aust. 2010, 193, 525–532. [Google Scholar] [CrossRef]
- Zeller, T.; Waldeyer, C.; Ojeda, F.; Schnabel, R.B.; Schäfer, S.; Altay, A.; Lackner, K.J.; Anker, S.D.; Westermann, D.; Blankenberg, S.; et al. Adverse Outcome Prediction of Iron Deficiency in Patients with Acute Coronary Syndrome. Biomolecules 2018, 8, 60. [Google Scholar] [CrossRef]
- Ponikowski, P.; Kirwan, B.-A.; Anker, S.D.; McDonagh, T.; Dorobantu, M.; Drozdz, J.; Fabien, V.; Filippatos, G.; Göhring, U.M.; Keren, A.; et al. Ferric Carboxymaltose for Iron Deficiency at Discharge after Acute Heart Failure: A Multicentre, Double-Blind, Randomised, Controlled Trial. Lancet 2020, 396, 1895–1904. [Google Scholar] [CrossRef]
- Anker, S.D.; Comin Colet, J.; Filippatos, G.; Willenheimer, R.; Dickstein, K.; Drexler, H.; Lüscher, T.F.; Bart, B.; Banasiak, W.; Niegowska, J.; et al. Ferric Carboxymaltose in Patients with Heart Failure and Iron Deficiency. N. Engl. J. Med. 2009, 361, 2436–2448. [Google Scholar] [CrossRef]
- Kalra, P.R.; Cleland, J.G.F.; Petrie, M.C.; Thomson, E.A.; Kalra, P.A.; Squire, I.B.; Ahmed, F.Z.; Al-Mohammad, A.; Cowburn, P.J.; Foley, P.W.X.; et al. Intravenous Ferric Derisomaltose in Patients with Heart Failure and Iron Deficiency in the UK (IRONMAN): An Investigator-Initiated, Prospective, Randomised, Open-Label, Blinded-Endpoint Trial. Lancet 2022, 400, 2199–2209. [Google Scholar] [CrossRef]
- von Haehling, S.; Jankowska, E.A.; van Veldhuisen, D.J.; Ponikowski, P.; Anker, S.D. Iron Deficiency and Cardiovascular Disease. Nat. Rev. Cardiol. 2015, 12, 659–669. [Google Scholar] [CrossRef]
- Toyokuni, S.; Yanatori, I.; Kong, Y.; Zheng, H.; Motooka, Y.; Jiang, L. Ferroptosis at the Crossroads of Infection, Aging and Cancer. Cancer Sci. 2020, 111, 2665–2671. [Google Scholar] [CrossRef]
- Savarese, G.; von Haehling, S.; Butler, J.; Cleland, J.G.F.; Ponikowski, P.; Anker, S.D. Iron Deficiency and Cardiovascular Disease. Eur. Heart J. 2023, 44, 14–27. [Google Scholar] [CrossRef]
- Corradi, F.; Masini, G.; Bucciarelli, T.; De Caterina, R. Iron Deficiency in Myocardial Ischaemia: Molecular Mechanisms and Therapeutic Perspectives. Cardiovasc. Res. 2023, 119, 2405–2420. [Google Scholar] [CrossRef] [PubMed]
- Rymer, J.A.; Rao, S.V. Anemia and Coronary Artery Disease. Coron. Artery Dis. 2018, 29, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Jankowska, E.A.; Von Haehling, S.; Anker, S.D.; MacDougall, I.C.; Ponikowski, P. Iron Deficiency and Heart Failure: Diagnostic Dilemmas and Therapeutic Perspectives. Eur. Heart J. 2013, 34, 816–829. [Google Scholar] [PubMed]
- Andrews, N.C. Disorders of Iron Metabolism. N. Engl. J. Med. 1999, 341, 1986–1995. [Google Scholar] [CrossRef]
- Florian, A.; Ludwig, A.; Rösch, S.; Yildiz, H.; Klumpp, S.; Sechtem, U.; Yilmaz, A. Positive Effect of Intravenous Iron-Oxide Administration on Left Ventricular Remodelling in Patients with Acute ST-Elevation Myocardial Infarction—A Cardiovascular Magnetic Resonance (CMR) Study. Int. J. Cardiol. 2014, 173, 184–189. [Google Scholar] [CrossRef]
- Huang, C.H.; Chang, C.C.; Kuo, C.L.; Huang, C.S.; Chiu, T.W.; Lin, C.S.; Liu, C.S. Serum Iron Concentration, but Not Hemoglobin, Correlates with TIMI Risk Score and 6-Month Left Ventricular Performance after Primary Angioplasty for Acute Myocardial Infarction. PLoS ONE 2014, 9, e104495. [Google Scholar] [CrossRef]
- Lakhal-Littleton, S. Mechanisms of Cardiac Iron Homeostasis and Their Importance to Heart Function. Free Radic. Biol. Med. 2019, 133, 234–237. [Google Scholar] [CrossRef]
- Bice, J.S.; Burley, D.S.; Baxter, G.F. Novel Approaches and Opportunities for Cardioprotective Signaling Through 3′,5′-Cyclic Guanosine Monophosphate Manipulation. J. Cardiovasc. Pharmacol. Ther. 2014, 19, 269–282. [Google Scholar] [CrossRef]
- Inserte, J.; Garcia-Dorado, D. The cGMP/PKG Pathway as a Common Mediator of Cardioprotection: Translatability and Mechanism. Br. J. Pharmacol. 2015, 172, 1996–2009. [Google Scholar] [CrossRef]
- van der Pol, A.; van Gilst, W.H.; Voors, A.A.; van der Meer, P. Treating Oxidative Stress in Heart Failure: Past, Present and Future. Eur. J. Heart Fail. 2019, 21, 425–435. [Google Scholar] [CrossRef]
- Badura, K.; Buławska, D.; Dąbek, B.; Witkowska, A.; Lisińska, W.; Radzioch, E.; Skwira, S.; Młynarska, E.; Rysz, J.; Franczyk, B. Primary Electrical Heart Disease—Principles of Pathophysiology and Genetics. Int. J. Mol. Sci. 2024, 25, 1826. [Google Scholar] [CrossRef] [PubMed]
- Jung, C.; Rezar, R.; Wischmann, P.; Masyuk, M.; Datz, C.; Bruno, R.R.; Kelm, M.; Wernly, B. The Role of Anemia on Admission in Acute Coronary Syndrome—An Umbrella Review of Systematic Reviews and Meta-Analyses. Int. J. Cardiol. 2022, 367, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Killip, S.; Bennett, J.M.; Chambers, M.D. Iron Deficiency Anemia. Am. Fam. Physician 2007, 75, 671–678. [Google Scholar] [PubMed]
- Badura, K.; Janc, J.; Wąsik, J.; Gnitecki, S.; Skwira, S.; Młynarska, E.; Rysz, J.; Franczyk, B. Anemia of Chronic Kidney Disease—A Narrative Review of Its Pathophysiology, Diagnosis, and Management. Biomedicines 2024, 12, 1191. [Google Scholar] [CrossRef]
- Cosentino, N.; Campodonico, J.; Pontone, G.; Guglielmo, M.; Trinei, M.; Sandri, M.T.; Riggio, D.; Baggiano, A.; Milazzo, V.; Moltrasio, M.; et al. Iron Deficiency in Patients with ST-Segment Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention. Int. J. Cardiol. 2020, 300, 14–19. [Google Scholar] [CrossRef]
- Obradovic, D.; Loncar, G.; Zeymer, U.; Pöss, J.; Feistritzer, H.J.; Freund, A.; Jobs, A.; Fuernau, G.; Desch, S.; Ceglarek, U.; et al. Impact of Anaemia and Iron Deficiency on Outcomes in Cardiogenic Shock Complicating Acute Myocardial Infarction. Eur. J. Heart Fail. 2024, 26, 448–457. [Google Scholar] [CrossRef]
- Fujinaga, H.; Okumura, T.; Harada, K. Iron Deficiency Predicts Poor Outcomes after Primary Intervention in Nonanemic Patients with Stemi. J. Am. Coll. Cardiol. 2013, 61, E206. [Google Scholar] [CrossRef]
- Meroño, O.; Cladellas, M.; Ribas-Barquet, N.; Poveda, P.; Recasens, L.; Bazán, V.; García-García, C.; Ivern, C.; Enjuanes, C.; Orient, S.; et al. Iron Deficiency Is a Determinant of Functional Capacity and Health-Related Quality of Life 30 Days After an Acute Coronary Syndrome. Rev. Española De Cardiol. Engl. Ed. 2017, 70, 363–370. [Google Scholar] [CrossRef]
- Silva, C.; Martins, J.; Campos, I.; Arantes, C.; Braga, C.G.; Salomé, N.; Gaspar, A.; Azevedo, P.; Álvares Pereira, M.; Marques, J.; et al. Prognostic Impact of Iron Deficiency in Acute Coronary Syndromes. Rev. Port. De Cardiol. Engl. Ed. 2021, 40, 525–536. [Google Scholar] [CrossRef]
- González-D’Gregorio, J.; Miñana, G.; Núñez, J.; Núñez, E.; Ruiz, V.; García-Blas, S.; Bonanad, C.; Mollar, A.; Valero, E.; Amiguet, M.; et al. Iron Deficiency and Long-Term Mortality in Elderly Patients with Acute Coronary Syndrome. Biomark. Med. 2018, 12, 987–999. [Google Scholar] [CrossRef]
- Jenča, D.; Melenovský, V.; Mrázková, J.; Šramko, M.; Kotrč, M.; Želízko, M.; Adámková, V.; Piťha, J.; Kautzner, J.; Wohlfahrt, P. Iron Deficiency and All-Cause Mortality after Myocardial Infarction. Eur. J. Intern. Med. 2024, 126, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Reinhold, J.; Papadopoulou, C.; Baral, R.; Vassiliou, V.S. Iron Deficiency for Prognosis in Acute Coronary Syndrome—A Systematic Review and Meta-Analysis. Int. J. Cardiol. 2021, 328, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Mohanty, N.K.; Dash, B.K.; Satpathy, C.; Banerjee, M.; Routray, S. Prognostic Impact of Iron Metabolism Changes in Patients with Acute Coronary Syndrome and Its Correlation with TIMI Risk Score and 6-Month Left Ventricular Performance. Indian J. Cardiovasc. Dis. Women 2024, 9, 195–200. [Google Scholar] [CrossRef]
- Inserte, J.; Barrabés, J.A.; Aluja, D.; Otaegui, I.; Bañeras, J.; Castellote, L.; Sánchez, A.; Rodríguez-Palomares, J.F.; Pineda, V.; Miró-Casas, E.; et al. Implications of Iron Deficiency in STEMI Patients and in a Murine Model of Myocardial Infarction. JACC Basic. Transl. Sci. 2021, 6, 567–580. [Google Scholar] [CrossRef] [PubMed]
- Van Der Schouw, Y.T.; Van Der Veeken, P.M.W.C.; Kok, F.J.; Koster, J.F.; Schouten, E.G.; Hofman, A. Original Contribution Iron Status in the Acute Phase and Six weeks after Myocardial Infarction. Free. Radic. Biol. Med. 1990, 8, 47–53. [Google Scholar] [CrossRef]
- Makrecka-Kuka, M.; Krumschnabel, G.; Gnaiger, E. High-Resolution Respirometry for Simultaneous Measurement of Oxygen and Hydrogen Peroxide Fluxes in Permeabilized Cells, Tissue Homogenate and Isolated Mitochondria. Biomolecules 2015, 5, 1319–1338. [Google Scholar] [CrossRef]
- Alayash, A. Hemoglobin-Based Blood Substitutes and the Treatment of Sickle Cell Disease: More Harm than Help? Biomolecules 2017, 7, 2. [Google Scholar] [CrossRef]
- Madaudo, C.; Coppola, G.; Parlati, A.L.M.; Corrado, E. Discovering Inflammation in Atherosclerosis: Insights from Pathogenic Pathways to Clinical Practice. Int. J. Mol. Sci. 2024, 25, 6016. [Google Scholar] [CrossRef]
- Dziegala, M.; Kasztura, M.; Kobak, K.; Bania, J.; Banasiak, W.; Ponikowski, P.; Jankowska, E.A. Influence of the Availability of Iron during Hypoxia on the Genes Associated with Apoptotic Activity and Local Iron Metabolism in Rat H9C2 Cardiomyocytes and L6G8C5 Skeletal Myocytes. Mol. Med. Rep. 2016, 14, 3969–3977. [Google Scholar] [CrossRef]
- Schrage, B.; Rübsamen, N.; Schulz, A.; Münzel, T.; Pfeiffer, N.; Wild, P.S.; Beutel, M.; Schmidtmann, I.; Lott, R.; Blankenberg, S.; et al. Iron Deficiency Is a Common Disorder in General Population and Independently Predicts All-Cause Mortality: Results from the Gutenberg Health Study. Clin. Res. Cardiol. 2020, 109, 1352–1357. [Google Scholar] [CrossRef]
- Erriquez, A.; Campo, G.; Guiducci, V.; Escaned, J.; Moreno, R.; Casella, G.; Menozzi, M.; Cerrato, E.; Sacchetta, G.; Menozzi, A.; et al. Complete vs Culprit-Only Revascularization in Older Patients with Myocardial Infarction and High Bleeding Risk. JAMA Cardiol. 2024, 9, 565. [Google Scholar] [CrossRef] [PubMed]



| Author | Cosentino N [26] | Obradovic D [27] | Fujinaga H. (Abstract Only) [28] | Merono O [29] | Silva C [30] | González-D’Gregorio J [31] | Zeller T [5] | Jenča D [32] |
|---|---|---|---|---|---|---|---|---|
| Year | 2019 | 2024 | 2013 | 2016 | 2021 | 2018 | 2018 | 2024 |
| Study type | prospective observational | randomized trial | prospective observational | prospective observational | retrospective | prospective observational cohort | prospective observational cohort | prospective observational cohort |
| Population | 420 | 427 | 352 | 244–>226 | 817 | 252 | 836 | 1156 |
| ID (%) | 237 (56%) | 72 (~17%) [patients with ID without anemia] | 169 (48%) | 139–>102 (57%–>46%) | 298 (36%) | n/s | 243 (29.1%) | 357 (31%) |
| Observation time | ACS-related hospitalization | 30 days | ACS-related hospitalization | 30 days | 2 years | IQR: 2–5.4 years | 4 years | 1224 days |
| Conclusions | ID in ACS is associated with better in-hospital prognosis [OR 0.50 (CI 0.27–0.93)]. | ID in AMI complicated by cardiogenic shock is associated with lower probability of death from any cause or renal replacement therapy [OR 0.63 (CI 0.31–1.08)]. | ID on admission is associated with elevated CRP and higher Killip–Kimball class, and predicts poor outcomes after primary PCI in nonanemic STEMI patients. | ID is associated with worse exercise tolerance [OR 2.9 (CI 1.4–5.5)] and lower quality of life [OR: 1.9 (CI: 1.1–3.3)] but has no effect on mortality during short-term follow-up. | ID is an independent predictor of death / development of heart failure in ACS patients [HR 1.66 (CI 1.11–2.50)]. | Lower TSAT levels are independently associated with an increased risk of long-term mortality [HR 1.54 (CI 1.03–2.30)]. | Iron deficiency is associated with unfavorable medium-term outcomes (independent of systolic heart function), the extent of myocardial necrosis and anemia [HR 1.52 (CI 1.03–2.26)]. | Iron deficiency is a common burden in patients with first ACS without past CAD history and, depending on measured parameters, is associated with all-cause mortality. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Misiewicz, A.; Badura, K.; Matuszewska-Brycht, O.; Krekora, J.; Drożdż, J. Iron Deficiency as a Factor of Worse Prognosis in Patients with Acute Myocardial Infarction. Biomedicines 2025, 13, 769. https://doi.org/10.3390/biomedicines13040769
Misiewicz A, Badura K, Matuszewska-Brycht O, Krekora J, Drożdż J. Iron Deficiency as a Factor of Worse Prognosis in Patients with Acute Myocardial Infarction. Biomedicines. 2025; 13(4):769. https://doi.org/10.3390/biomedicines13040769
Chicago/Turabian StyleMisiewicz, Aleksander, Krzysztof Badura, Oliwia Matuszewska-Brycht, Jan Krekora, and Jarosław Drożdż. 2025. "Iron Deficiency as a Factor of Worse Prognosis in Patients with Acute Myocardial Infarction" Biomedicines 13, no. 4: 769. https://doi.org/10.3390/biomedicines13040769
APA StyleMisiewicz, A., Badura, K., Matuszewska-Brycht, O., Krekora, J., & Drożdż, J. (2025). Iron Deficiency as a Factor of Worse Prognosis in Patients with Acute Myocardial Infarction. Biomedicines, 13(4), 769. https://doi.org/10.3390/biomedicines13040769






