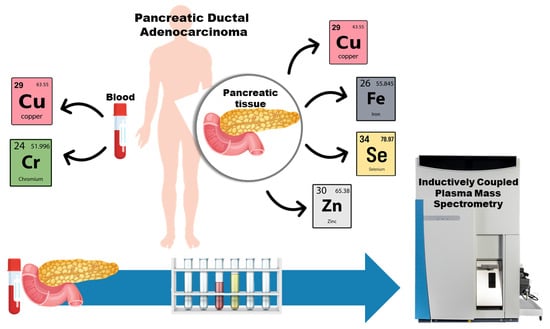
Toxic Metal and Essential Element Concentrations in the Blood and Tissues of Pancreatic Ductal Adenocarcinoma Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Characteristics of the Subjects
- Stage 0 (carcinoma in situ): cancer cells are only present in the top layers of pancreatic duct cells and have not invaded deeper tissues;
- Stage Ia: cancer (max. 2 cm) is confined to the pancreas and has not spread beyond;
- Stage Ib: cancer (larger than 2 cm) is confined to the pancreas and has not spread beyond;
- Stage IIb: cancer has extended beyond the pancreas (from 1 to 3 regional lymph nodes) but has not invaded major blood vessels;
- Stage III: cancer has spread to nearby major blood vessels but has not spread to distant organs;
- Stage IV: cancer has spread to distant organs, such as the liver, lungs or other organs.
2.2. Sample Preparation
2.3. Quantification of Metals
2.4. Statistics
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- AIRC, Associazione Italiana per la Ricerca sul Cancro. Available online: https://www.airc.it/cancro/informazioni-tumori/guida-ai-tumori/tumore-del-pancreas (accessed on 4 September 2023).
- WHO, World Health Organization. Available online: https://platform.who.int/mortality/themes/theme-details/topics/indicator-groups/indicator-group-details/MDB/pancreas-cancer (accessed on 4 September 2023).
- Djordjevic, V.R.; Wallace, D.R.; Schweitzer, A.; Boricic, N.; Knezevic, D.; Matic, S.; Grubor, N.; Kerkez, M.; Radenkovic, D.; Bulat, Z.; et al. Environmental cadmium exposure and pancreatic cancer: Evidence from case control, animal and in vitro studies. Environ. Int. 2019, 128, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, G.G.; Reis, I.M. Is cadmium a cause of human pancreatic cancer? Cancer Epidemiol. Biomark. Prev. 2000, 9, 139–145. [Google Scholar]
- Zhao, L.; Islam, R.; Wang, Y.; Zhang, X.; Liu, L.-Z. Epigenetic regulation in chromium-, nickel- and cadmium-induced carcinogenesis. Cancers 2022, 14, 5768. [Google Scholar] [CrossRef] [PubMed]
- Hartwig, A.; Schwerdtle, T. Interactions by carcinogenic metal compounds with DNA repair processes: Toxicological implications. Toxicol. Lett. 2002, 127, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Mortoglou, M.; Manić, L.; Buha Djordjevic, A.; Bulat, Z.; Djordjevic, V.; Manis, K.; Valle, E.; York, L.; Wallace, D.; Uysal-Onganer, P. Nickel’s role in pancreatic ductal adenocarcinoma: Potential involvement of microRNAs. Toxics 2022, 10, 148. [Google Scholar] [CrossRef] [PubMed]
- Camargo, J.; Pumarega, J.A.; Alguacil, J.; Sanz-Gallén, P.; Gasull, M.; Delclos, G.L.; Amaral, A.F.S.; Porta, P. Toenail concentrations of trace elements and occupational history in pancreatic cancer. Environ. Int. 2019, 127, 216–225. [Google Scholar] [CrossRef] [PubMed]
- Park, J.M.; Mau, C.-Z.; Chen, Y.-C.; Su, Y.-H.; Chen, H.-A.; Huang, S.-Y.; Chang, J.-S.; Chiu, C.-F. A case–control study in Taiwanese cohort and meta-analysis of serum ferritin in pancreatic cancer. Sci. Rep. 2021, 11, 21242. [Google Scholar] [CrossRef]
- Bocca, B.; Madeddu, R.; Asara, Y.; Tolu, P.; Marchal, J.A.; Forte, G. Assessment of reference ranges for blood Cu, Mn, Se and Zn in a selected Italian population. J. Trace Elem. Med. Biol. 2011, 25, 19–26. [Google Scholar] [CrossRef]
- Lelièvre, P.; Sancey, L.; Coll, J.-L.; Deniaud, A.; Busser, B. The multifaceted roles of copper in cancer: A trace metal element with dysregulated metabolism, but also a target or a bullet for therapy. Cancers 2020, 12, 3594. [Google Scholar] [CrossRef]
- Wang, L.; Wang, J.; Liu, X.; Liu, Q.; Zhang, G.; Liang, L. Association between selenium intake and the risk of pancreatic cancer: A meta-analysis of observational studies. Biosci. Rep. 2016, 36, e00395. [Google Scholar] [CrossRef]
- Bhutia, Y.D.; Ogura, J.; Grippo, P.J.; Torres, C.; Sato, T.; Wachtel, M.; Ramachandran, S.; Babu, E.; Sivaprakasam, S.; Rajasekaran, D.; et al. Chronic exposure to excess iron promotes EMT and cancer via p53 loss in pancreatic cancer. Asian J. Pharm. Sci. 2020, 15, 237–251. [Google Scholar] [CrossRef]
- Karapinar, H.S.; Türkdoğan, M.K.; Kiliçel, F. Serum trace element levels of liver cirrhosis and pancreatic cancer patients. Arch. Community Med. Public Health 2022, 8, 055–061. [Google Scholar]
- Kelleher, S.L.; McCormick, N.H.; Velasquez, V.; Lopez, V. Zinc in specialized secretory tissues: Roles in the pancreas, prostate, and mammary gland. Adv. Nutr. 2011, 2, 101–111. [Google Scholar] [CrossRef]
- Li, M.; Zhang, Y.; Liu, Z.; Bharadwaj, U.; Wang, H.; Wang, X.; Zhang, S.; Liuzzi, J.P.; Chang, S.M.; Cousins, R.J.; et al. Aberrant expression of zinc transporter ZIP4 (SLC39A4) significantly contributes to human pancreatic cancer pathogenesis and progression. Proc. Natl. Acad. Sci. USA 2007, 104, 18636–18641. [Google Scholar] [CrossRef]
- Richter, P.; Faroon, O.; Pappas, R.S. Cadmium and cadmium/zinc ratios and tobacco-related morbidities. Int. J. Environ. Res. Public Health 2017, 14, 1154. [Google Scholar] [CrossRef]
- AJCC. Cancer Staging Manual, 8th ed.; Amin, M.B., Edge, S.B., Eds.; Springer International Publishing AG: New York, NY, USA, 2018; p. 1032. [Google Scholar]
- Miller, K.D.; Siegel, R.L.; Lin, C.C.; Mariotto, A.B.; Kramer, J.L.; Rowland, J.H.; Stein, K.D.; Alteri, R.; Jemal, A. Cancer treatment and survivorship statistics, 2016. CA Cancer J. Clin. 2016, 66, 271–289. [Google Scholar] [CrossRef]
- Carrigan, P.E.; Hentz, J.G.; Gordon, G.; Morgan, J.L.; Raimondo, M.; Anbar, A.D.; Miller, L.J. Distinctive heavy metal composition of pancreatic juice in patients with pancreatic carcinoma. Cancer Epidemiol. Biomark. Prev. 2007, 16, 2656–2663. [Google Scholar] [CrossRef]
- Bocca, B.; Forte, G.; Oggiano, R.; Clemente, S.; Asara, Y.; Peruzzu, P.; Farace, C.; Pala, S.; Fois, A.G.; Pirina, P.; et al. Level of neurotoxic metals in amyotrophic lateral sclerosis: A population-based case–control study. J. Neurol. Sci. 2015, 359, 11–17. [Google Scholar] [CrossRef]
- IARC, International Agency for Research on Cancer. Chromium, Nickel and Welding; IARC: Lyon, France, 1990; Volume 49. [Google Scholar]
- Yao, H.; Guo, L.; Jiang, B.-H.; Luo, J.; Shi, X. Oxidative stress and chromium (VI) carcinogenesis. J. Environ. Pathol. Toxicol. Oncol. 2008, 27, 77–88. [Google Scholar] [CrossRef]
- Henkler, F.; Brinkmann, J.; Luch, A. The role of oxidative stress in carcinogenesis induced by metals and xenobiotics. Cancers 2010, 2, 376–396. [Google Scholar] [CrossRef]
- Al-Fartusie, F.; Farhan, M.; Al-Bairmani, H.; Nabil, N.; Aldhaheri, M.; Al-Temimi, R. Estimation of some vital trace elements in patients with acute pancreatitis: A case-control study. Braz. J. Pharm. Sci. 2022, 58, e20639. [Google Scholar] [CrossRef]
- Antwi, S.O.; Eckert, E.C.; Sabaque, C.V.; Leof, E.R.; Hawthorne, K.M.; Bamlet, W.R.; Chaffee, K.G.; Oberg, A.L.; Petersen, G.M. Exposure to environmental chemicals and heavy metals, and risk of pancreatic cancer. Cancer Causes Control 2015, 26, 1583–1591. [Google Scholar] [CrossRef]
- Amaral, A.F.S.; Porta, M.; Silverman, D.T.; Milne, R.L.; Kogevinas, M.; Rothman, N.; Cantor, K.P.; Jackson, B.P.; Pumarega, J.A.; López, T.; et al. Pancreatic cancer risk and levels of trace elements. Gut 2012, 61, 1583–1588. [Google Scholar] [CrossRef]
- Gómez-Tomás, A.; Pumarega, J.; Alguacil, J.; Amaral, A.F.S.; Malats, N.; Pallarès, N.; Gasull, M.; Porta, M. for the PANKRAS II Study Group. Concentrations of trace elements and KRAS mutations in pancreatic ductal adenocarcinoma. Environ. Mol. Mutagen. 2019, 60, 693–703. [Google Scholar] [CrossRef]
- Schilling, K.; Larner, F.; Saad, A.; Roberts, R.; Kocher, H.M.; Blyuss, O.; Halliday, A.N.; Crnogorac-Jurcevicg, T. Urine metallomics signature as an indicator of pancreatic cancer. Metallomics 2020, 12, 752–757. [Google Scholar] [CrossRef]
- Lener, M.R.; Scott, R.J.; Wiechowska-Kozłowska, A.; Serrano-Fernández, P.; Baszuk, P.; Jaworska-Bieniek, K.; Sukiennicki, G.; Marciniak, W.; Muszyńska, M.; Kładny, J.; et al. Serum concentrations of selenium and copper in patients diagnosed with pancreatic cancer. Cancer Res. Treat. 2016, 48, 1056–1064. [Google Scholar] [CrossRef]
- Guo, Q.; Li, L.; Hou, S.; Yuan, Z.; Li, C.; Zhang, W.; Zheng, L.; Li, X. The role of iron in cancer progression. Front. Oncol. 2021, 11, 778492. [Google Scholar] [CrossRef]
- Al-Ostoot, F.H.; Salah, S.; Khamees, H.A.; Khanum, S.A. Tumor angiogenesis: Current challenges and therapeutic opportunities. Cancer. Treat. Res. Commun. 2021, 28, 100422. [Google Scholar] [CrossRef]
- Lugano, R.; Ramachandran, M.; Dimberg, A. Tumor angiogenesis: Causes, consequences, challenges and opportunities. Cell. Mol. Life Sci. 2020, 77, 1745–1770. [Google Scholar] [CrossRef]
- Backe, M.B.; Moen, I.W.; Ellervik, C.; Hansen, J.B.; Mandrup-Poulsen, T. Iron regulation of pancreatic beta-cell functions and oxidative stress. Annu. Rev. Nutr. 2016, 36, 241–273. [Google Scholar] [CrossRef]
- Friedman, G.D.; van den Eeden, S.K. Risk factors for pancreatic cancer: An exploratory study. Int. J. Epidemiol. 1993, 22, 30–37. [Google Scholar] [CrossRef]
- Gaur, A.; Collins, H.; Wulaningsih, W.; Holmberg, L.; Garmo, H.; Hammar, N.; Walldius, G.; Jungner, I.; Van Hemelrijck, M. Iron metabolism and risk of cancer in the Swedish AMORIS study. Cancer Causes Control 2013, 24, 1393–1402. [Google Scholar] [CrossRef]
- Zhao, Z.; Li, C.; Hu, M.; Li, J.; Liu, R. Plasma ferritin levels, HFE polymorphismsm, and risk of pancreatic cancer among Chinese Han population. Tumour Biol. 2014, 35, 7629–7633. [Google Scholar] [CrossRef]
- Zanini, S.; Renzi, S.; Limongi, A.R.; Bellavite, P.; Giovinazzo, F.; Bermano, G. A review of lifestyle and environment risk factors for pancreatic cancer. Eur. J. Cancer 2021, 145, 53–70. [Google Scholar] [CrossRef]
- IARC, International Agency for Research on Cancer. Inorganic and Organic Lead Compounds; IARC: Lyon, France, 2006; Volume 87. [Google Scholar]
- Sani, A.H.; Amanabo, M. Lead: A concise review of its toxicity, mechanism and health effect. GSC Biol. Pharm. Sci. 2021, 15, 055–062. [Google Scholar] [CrossRef]
- Forte, G.; Madeddu, R.; Tolu, P.; Asara, Y.; Marchal, J.A.; Bocca, B. Reference intervals for blood Cd and Pb in the general population of Sardinia (Italy). Int. J. Hyg. Environ. Health 2011, 214, 102–109. [Google Scholar] [CrossRef]
- Barbosa, F., Jr.; Tanus-Santos, J.E.; Gerlach, R.F.; Parsons, P.J. A critical review of biomarkers used for monitoring human exposure to lead: Advantages, limitations, and future needs. Environ. Health Perspect. 2005, 113, 1669–1674. [Google Scholar] [CrossRef] [PubMed]
- Farzin, L.; Moassesi, M.E.; Sajadi, F.; Ahmadi Faghih, M.A. Evaluation of trace elements in pancreatic cancer patients in Iran. Middle East J. Cancer 2013, 4, 79–86. [Google Scholar]
- Chatterjee, S.; Combs, G.F., Jr.; Chattopadhyay, A.; Stolzenberg-Solomon, R. Serum selenium and pancreatic cancer: A prospective study in the prostate, lung, ovarian, and colorectal cancer cohort. Cancer Causes Control 2019, 30, 457–464. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Zhang, Y.; Bharadwaj, U.; Zhai, Q.J.; Ahern, C.H.; Fisher, W.E.; Brunicardi, F.C.; Logsdon, C.D.; Chen, C.; Yao, Q. Down-regulation of ZIP4 by RNA interference inhibits pancreatic cancer growth and increases the survival of nude mice with pancreatic cancer xenografts. Clin. Cancer Res. 2009, 15, 5993–6001. [Google Scholar] [CrossRef]
- Yu, Z.; Yu, Z.; Chen, Z.B.; Yang, L.; Ma, M.J.; Lu, S.N.; Wang, C.S.; Teng, C.B.; Nie, Y.Z. Zinc chelator TPEN induces pancreatic cancer cell death through causing oxidative stress and inhibiting cell autophagy. Cell Physiol. 2019, 234, 20648–20661. [Google Scholar] [CrossRef] [PubMed]
- Pungpapong, S.; Scolapio, J.S.; Woodward, T.A.; Wallace, M.B.; Raimondo, M. Is zinc concentration in pancreatic fluid a marker for pancreatic diseases? JOP 2005, 6, 425–430. [Google Scholar] [PubMed]
- Callejón-Leblic, B.; Gómez-Ariza, J.L.; Pereira-Vega, A.; García-Barrera, T. Metal dyshomeostasis based biomarkers of lung cancer using human biofluids. Metallomics 2018, 10, 1444–1451. [Google Scholar] [CrossRef]
- Hohberger, B.; Chaudhri, M.A.; Michalke, B.; Lucio, M.; Nowomiejska, K.; Schlötzer-Schrehardt, U.; Grieb, P.; Rejdak, R.; Jünemann, A.G.M. Levels of aqueous humor trace elements in patients with open-angle glaucoma. J. Trace Elem. Med. Biol. 2018, 45, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Forte, G.; Bocca, B.; Pisano, A.; Collu, C.; Farace, C.; Sabalic, A.; Senofonte, M.; Fois, A.G.; Mazzarello, V.L.; Pirina, P.; et al. The levels of trace elements in sputum as biomarkers for idiopathic pulmonary fibrosis. Chemosphere 2021, 271, 129514. [Google Scholar] [CrossRef]
| PDAC | Controls | |
|---|---|---|
| Subject (no.) | 20 | |
| Total population | 46 | |
| Operated PDAC patients (OPPs) | 32 | |
| Non-operated PDAC patients (NOPPs) | 14 | |
| Mean age (years) | 67.2 ± 9.4 | 60.5 ± 8.5 |
| Sex (no.) | ||
| Females | 25 | 11 |
| Males | 21 | 9 |
| Cancer stages (no.) | ||
| Stage 0 | 5 | |
| Stage Ia | 6 | |
| Stage Ib | 5 | |
| Stage IIb | 10 | |
| Stage III | 6 | |
| Stage IV | 14 | |
| Metastasis (no.) | ||
| Yes | 14 | |
| No | 32 |
| PDAC Patients (No. 46) | OPPs (No. 32) | NOPPs (No. 14) | HCs (No. 20) | Statistical Test (Patients vs. HCs) | |
|---|---|---|---|---|---|
| Cd (ng/mL) | 0.21–0.58–1.52 | 0.27–0.58–1.51 | 0.20–0.54–1.47 | 0.11–0.50–1.57 | ns |
| Cr (ng/mL) | 0.26–0.70–1.63 a | 0.30–0.74–1.60 b | 0.26–0.64–1.59 b | 0.17–0.38–1.33 | a p < 0.01; b p < 0.05 |
| Cu (ng/mL) | 853–1251–1682 a | 914–1274–1775 a | 851–1148–1670 b | 779–982–1312 | a p < 0.01; b p < 0.05 |
| Fe (µg/mL) | 234–400–608 | 236–398–588 | 240–407–610 | 324–426–689 | ns |
| Mn (ng/mL) | 3.79–7.24–15.8 | 3.78–7.24–14.6 | 4.13–7.43–15.8 | 5.63–9.81–16.4 | ns |
| Ni (ng/mL) | 0.44–0.83–2.36 | 0.44–0.79–2.54 | 0.47–0.84–1.77 | 0.41–0.77–2.02 | ns |
| Pb (ng/mL) | 8.48–29.6–94.3 | 8.38–23.4–53.4 | 9.43–32.2–112 | 6.76–16.8–63.5 | ns |
| Se (ng/mL) | 90.6–129–203 | 101–149–233 | 90.4–119–176 | 108–151–187 | ns |
| Zn (µg/mL) | 4.04–6.86–10.0 | 4.71–7.99–10.6 | 3.93–6.41–9.42 | 5.31–7.02–10.2 | ns |
| Cancer Tissue (No. 32) | Non-Cancer Tissue (No. 32) | Statistical Test (Cancer vs. Non-Cancer) | |
|---|---|---|---|
| Cd (ng/g) | 84.2–1593–5080 | 43.8–346–6883 | ns |
| Cr (ng/g) | 7.90–31.3–590 | 12.2–32.6–309 | ns |
| Cu (ng/g) | 2232–4664–6307 | 485–1330–5557 | p < 0.01 |
| Fe (µg/g) | 60.4–172–552 | 47.9–94.8–319 | p < 0.05 |
| Mn (ng/g) | 214–1098–3532 | 25.3–296–3891 | ns |
| Ni (ng/g) | 18.0–89.7–1919 | 14.3–56.5–1806 | ns |
| Pb (ng/g) | 6.33–23.4–130 | 4.44–12.1–73.4 | ns |
| Se (ng/g) | 327–598–1350 | 40.2–223–738 | p < 0.01 |
| Zn (µg/g) | 27.3–49.7–107 | 3.78–24.1–116 | p < 0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Forte, G.; Pisano, A.; Bocca, B.; Fenu, G.; Farace, C.; Etzi, F.; Perra, T.; Sabalic, A.; Porcu, A.; Madeddu, R. Toxic Metal and Essential Element Concentrations in the Blood and Tissues of Pancreatic Ductal Adenocarcinoma Patients. Toxics 2024, 12, 32. https://doi.org/10.3390/toxics12010032
Forte G, Pisano A, Bocca B, Fenu G, Farace C, Etzi F, Perra T, Sabalic A, Porcu A, Madeddu R. Toxic Metal and Essential Element Concentrations in the Blood and Tissues of Pancreatic Ductal Adenocarcinoma Patients. Toxics. 2024; 12(1):32. https://doi.org/10.3390/toxics12010032
Chicago/Turabian StyleForte, Giovanni, Andrea Pisano, Beatrice Bocca, Grazia Fenu, Cristiano Farace, Federica Etzi, Teresa Perra, Angela Sabalic, Alberto Porcu, and Roberto Madeddu. 2024. "Toxic Metal and Essential Element Concentrations in the Blood and Tissues of Pancreatic Ductal Adenocarcinoma Patients" Toxics 12, no. 1: 32. https://doi.org/10.3390/toxics12010032
APA StyleForte, G., Pisano, A., Bocca, B., Fenu, G., Farace, C., Etzi, F., Perra, T., Sabalic, A., Porcu, A., & Madeddu, R. (2024). Toxic Metal and Essential Element Concentrations in the Blood and Tissues of Pancreatic Ductal Adenocarcinoma Patients. Toxics, 12(1), 32. https://doi.org/10.3390/toxics12010032