A Case Report of Successful Treatment of Minoxidil Toxicosis Using Hemodialysis in a Cat
Abstract
Simple Summary
Abstract
1. Introduction
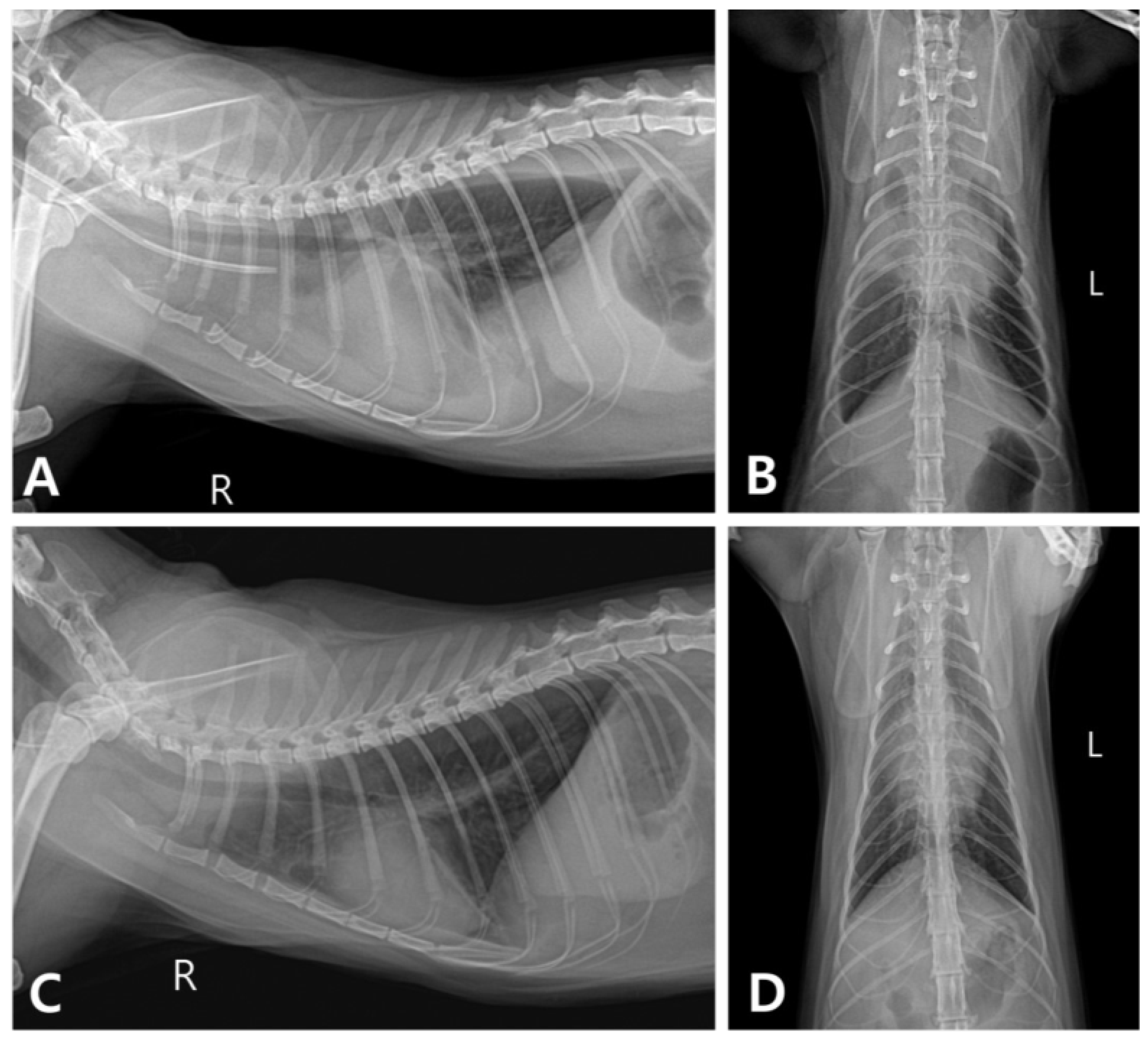
2. Case Description
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bennett, W.M.; Golper, T.A.; Muther, R.S.; McCarron, D.A. Efficacy of minoxidil in the treatment of severe hypertension in systemic disorders. J. Cardiovasc. Pharmacol. 1980, 2 (Suppl. S2), S142–S148. [Google Scholar] [CrossRef] [PubMed]
- Ranchoff, R.E.; Bergfeld, W.F. Topical minoxidil reduces blood pressure. J. Am. Acad. Dermatol. 1985, 12, 586–587. [Google Scholar] [CrossRef] [PubMed]
- Rose, S.R.; Tomaszewski, C. Evaluation of oral and topical minoxidil exposures reported to us poison centres from 1985–1991. Drug. Invest. 1994, 8, 81–94. [Google Scholar] [CrossRef]
- Satoh, H.; Morikaw, S.; Fujiwara, C.; Terada, H.; Uehara, A.; Ohno, R. A case of acute myocardial infarction associated with topical use of minoxidil (RiUP) for treatment of baldness. Jpn. Heart J. 2000, 41, 519–523. [Google Scholar] [CrossRef]
- De Clementi, C.; Bailey, K.L.; Goldstein, S.C.; Orser, M.S. Suspected toxicosis after topical administration of minoxidil in 2 cats. J. Vet. Emerg. Crit. Care 2004, 14, 287–292. [Google Scholar] [CrossRef]
- Jordan, T.J.M.; Yaxley, P.E.; Culler, C.A.; Balakrishnan, A. Successful management of minoxidil toxicosis in a dog. J. Am. Vet. Med. Assoc. 2018, 252, 222–226. [Google Scholar] [CrossRef]
- Tater, K.C.; Gwaltney-Brant, S.; Wismer, T. Topical minoxidil exposures and toxicoses in dogs and cats: 211 cases (2001–2019). J. Am. Anim. Hosp. Assoc. 2021, 57, 225–231. [Google Scholar] [CrossRef]
- Cowgill, L.D.; Guillaumin, J. Extracorporeal renal replacement therapy and blood purification in critical care. J. Vet. Emerg. Crit. Care 2013, 23, 194–204. [Google Scholar] [CrossRef]
- Hoffman, L.; Londoño, L.A.; Martinez, J. Management of severe baclofen toxicosis using hemodialysis in conjunction with mechanical ventilation in a cat with chronic kidney disease. J. Feline Med. Surg. Open Rep. 2021, 7, 20551169211033770. [Google Scholar] [CrossRef]
- Klainbart, S.; Kuzi, S.; Segev, G. Treatment of phenobarbital overdose by hemodialysis in a cat with suspected porto-systemic shunt. Isr. J. Vet. Med. 2017, 72, 42–45. [Google Scholar]
- Mauro, K.D.; Culler, C.A.; Vigani, A. Emergency treatment with intermittent hemodialysis for amikacin overdose in a cat. J. Vet. Emerg. Crit. Care 2021, 31, 813–817. [Google Scholar] [CrossRef] [PubMed]
- Sica, D.A. Minoxidil: An underused vasodilator for resistant or severe hypertension. J. Clin. Hypertens. 2004, 6, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Lowenthal, D.T.; Onesti, G.; Mutterperl, R.; Affrime, M.; Martinez, E.W.; Kim, K.E.; Busby, P.; Shirk, J.; Swartz, C. Long-term clinical effects, bioavailability, and kinetics of minoxidil in relation to renal function. J. Clin. Pharmacol. 1978, 18, 500–508. [Google Scholar] [CrossRef] [PubMed]
- Leenen, F.H.; Smith, D.L.; Unger, W.P. Topical minoxidil: Cardiac effects in bald man. Br. J. Clin. Pharmacol. 1988, 26, 481–485. [Google Scholar] [CrossRef]
- Johnson, T.E.; Fick, M.E.; Haraschak, J.L.; Vernier, M.E.; Kadotani, S. Successful management of minoxidil 5% toxicosis in 2 cats from the same household. J. Vet. Emerg. Crit. Care 2023, 33, 454–459. [Google Scholar] [CrossRef]
- Song, J.; Kim, S.; Moon, J.; Jung, D. Successful management of suspected minoxidil toxicosis in a cat following accidental dermal exposure. Vet. Med.-Czech 2022, 67, 323–329. [Google Scholar] [CrossRef]
- Reina-Doreste, Y.; Stern, J.A.; Keene, B.W.; Tou, S.P.; Atkins, C.E.; DeFrancesco, T.C.; Ames, M.K.; Hodge, T.E.; Meurs, K.M. Case-control study of the effects of pimobendan on survival time in cats with hypertrophic cardiomyopathy and congestive heart failure. J. Am. Vet. Med. Assoc. 2014, 245, 534–539. [Google Scholar] [CrossRef]
- Ward, J.L.; Kussin, E.Z.; Tropf, M.A.; Tou, S.P.; DeFrancesco, T.C.; Keene, B.W. Retrospective evaluation of the safety and tolerability of pimobendan in cats with obstructive vs nonobstructive cardiomyopathy. J. Vet. Intern. Med. 2020, 34, 2211–2222. [Google Scholar] [CrossRef]
- Schober, K.E.; Rush, J.E.; Luis Fuentes, V.; Glaus, T.; Summerfield, N.J.; Wright, K.; Lehmkuhl, L.; Wess, G.; Sayer, M.P.; Loureiro, J.; et al. Effects of pimobendan in cats with hypertrophic cardiomyopathy and recent congestive heart failure: Results of a prospective, double-blind, randomized, nonpivotal, exploratory field study. J. Vet. Intern. Med. 2021, 35, 789–800. [Google Scholar] [CrossRef]
- McEvoy, G.K. AHFS Drug Information 2000; American Society of Health-System Pharmacists, Inc.: Bethesda, MD, USA, 2000; 3546p. [Google Scholar]
- National Center for Biotechnology Information. PubChem Compound Summary for, Minoxidil. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Minoxidil (accessed on 7 May 2024).
- Mirrakhimov, A.E.; Barbaryan, A.; Gray, A.; Ayach, T. The role of renal replacement therapy in the management of pharmacologic poisonings. Int. J. Nephrol. 2016, 2016, 3047329. [Google Scholar] [CrossRef]
- Patterson, S.C.; Ramstad, T.; Mills, K.A. Development and validation of a procedure for the determination of minoxidil in hair-regrowth formulations using two variants of capillary zone electrophoresis. Farmaco 2005, 60, 547–554. [Google Scholar] [CrossRef]
- Segev, G.; Foster, J.D.; Francey, T.; Langston, C.; Schweighauser, A.; Cowgill, L.D. International renal interest society best practice consensus guidelines for intermittent hemodialysis in dogs and cats. Vet. J. 2024, 305, 106092. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahn, W.; Lee, T.; Jung, S.; Nam, A. A Case Report of Successful Treatment of Minoxidil Toxicosis Using Hemodialysis in a Cat. Vet. Sci. 2024, 11, 487. https://doi.org/10.3390/vetsci11100487
Ahn W, Lee T, Jung S, Nam A. A Case Report of Successful Treatment of Minoxidil Toxicosis Using Hemodialysis in a Cat. Veterinary Sciences. 2024; 11(10):487. https://doi.org/10.3390/vetsci11100487
Chicago/Turabian StyleAhn, Woonchan, Taeho Lee, Soyoung Jung, and Aryung Nam. 2024. "A Case Report of Successful Treatment of Minoxidil Toxicosis Using Hemodialysis in a Cat" Veterinary Sciences 11, no. 10: 487. https://doi.org/10.3390/vetsci11100487
APA StyleAhn, W., Lee, T., Jung, S., & Nam, A. (2024). A Case Report of Successful Treatment of Minoxidil Toxicosis Using Hemodialysis in a Cat. Veterinary Sciences, 11(10), 487. https://doi.org/10.3390/vetsci11100487




