Abstract
Bioceramic endodontic cements, known for their antibacterial properties, calcium ion release, and alkaline pH, may come into contact with various irrigants after furcal perforation repair. This study aimed to evaluate the effect of different irrigating solutions and setting times on the shear bond strength (SBS) of Biodentine® (Septodont, Saint-Maur-des-Fosses Cedex, France) to a self-adhering flowable composite. Sixty Biodentine® (Septodont, Saint-Maur-des-Fosses Cedex, France) blocks were prepared and divided into two groups based on the setting time: 72 h and 7 days. These were further subdivided into five subgroups based on the irrigation solution applied: distilled water, sodium hypochlorite, ethylenediaminetetraacetic acid, chlorhexidine, and phosphoric acid. They were then restored with Dyad FlowTM (KerrTM, Orange, CA, USA). SBS and failure modes were assessed at 24 h and 6 months. A two-way analysis of variance (ANOVA) test was performed to analyze the effect of the different irrigating solutions and setting times on the SBS of Biodentine® (Septodont, Saint-Maur-des-Fosses Cedex, France) and Dyad FlowTM (KerrTM, Orange, CA, USA). The level of significance was set at a ≤0.05. At 24 h, SBS was significantly influenced by both the irrigant solution (p = 0.029) and setting time (p = 0.018); at 6 months, SBS was influenced only by the irrigating solutions (p < 0.001). The predominant mode of bond failure was adhesive across all groups. In conclusion, while the setting time did not affect the bond strength, certain irrigating solutions reduced it. Thus, careful consideration of surface treatments applied to Biodentine® is crucial for successful endodontic and restorative outcomes.
1. Introduction
Biodentine® (Septodont, Saint-Maur-des-Fosses Cedex, France) is a bioceramic material that is frequently used in endodontics with different clinical applications for its good sealing ability, high compressive strength, short setting time [1,2,3], biocompatibility, bioactivity, and biomineralization properties [1,4,5,6]. Therefore, it is recommended as a dentine substitute under resin composite restorations and endodontic repair material [2,4,7]. Moreover, this material, as a putty formulation, could be used in several endodontic treatments, such as apexification [8], root end-filling material (apicoectomy) [9], pulpotomy [10], resorption [11], and perforation [12].
A clinical advantage of this bioceramic, according to the manufacturer, is its short setting time of approximately 12 min [2,3,4,6]. This characteristic is attributed to the addition of calcium chloride to the liquid; this compound acts as the setting accelerator and as a water-reducing agent [4,6,13,14,15]. However, after repairing the furcal perforation, the bioceramic interacts with various irrigants, such as sodium hypochlorite (NaClO), chlorhexidine (CHX), and ethylenediaminetetraacetic acid (EDTA); these are used in the endodontic treatment to disinfect the root canal system [16,17,18]. In addition, Biodentine® may be in contact with phosphoric acid (H3PO4) before the placement of a composite in the regenerative endodontic treatment [19,20,21]. Hence, the setting time of the bioceramic and its contact with irrigants are important clinical factors that could compromise its mechanical properties and its ability to bond to a restoration material.
In this sense, the bond strength between restorative and bioceramic materials is essential to seal and guarantee the success of the treatment [20,22]. The relationship between the two lies in their use together in a layered approach, where Biodentine® provides a strong, biologically compatible foundation, and the self-adhering flowable composite is applied on the top to create a durable and aesthetic restoration. The effectiveness of this combination depends on the bond strength between the Biodentine® and the composite, which can be influenced by factors like surface treatments, setting times, and the types of irrigating solutions used. Inadequate bonding can lead to bacterial infiltration into the periradicular tissues, potentially compromising the repair or regenerative procedure [1]. Despite the significance of this bond, there is limited research addressing the impact of different irrigating solutions and setting times on the bond strength between bioceramic materials and restorative composites. This gap in the literature highlights the need for a deeper understanding of how these variables influence bond strength. The evaluated irrigation solutions differ in their effectiveness and impact on bond strength: 5.25% NaClO and 17% EDTA can aggressively alter the dentin surface, potentially reducing SBS, while 2% CHX provides antimicrobial benefits with a less adverse effect on bonding.
To address this limitation, the purpose of this study was to evaluate the effect of various irrigating solutions (5.25% NaClO, 2% CHX, and 17% EDTA) and setting times (72 h or 7 days) in the shear bond strength (SBS) of Biodentine® and a self-adhering flowable composite (Dyad FlowTM; KerrTM, Orange, CA, USA). The tested null hypothesis was that there were no statistically significant differences in the SBS of Biodentine® and a self-adhering flowable composite when the setting time variated and diverse irrigating solutions were applied.
2. Materials and Methods
In this study, the bond strength between Biodentine® and a self-adhering flowable material was evaluated according to the following factors: (1) setting time of Biodentine® in two levels (72 h and 7 days) and (2) irrigation solutions in three levels (5.25% NaClO, 2% CHX, 17% EDTA). Control groups using H3PO4 and distilled water were evaluated too. The primary response variable was the SBS (n = 6). The sample size was estimated according to the data from a previous study [22] considering a comparative study design with 10 independent groups, a minimum detectable difference with an average of 3.87, a standard deviation of 2, a statistical power of 0.8, and an a = 0.05. The main composition and characteristics of the materials used are described in Table 1.

Table 1.
Characteristics of materials used in the study, according to manufacturer specifications.
Sixty cylindrical acrylic blocks (5 mm height × 10 mm diameter) were prepared by packing cold-cure acrylic into PVC molds. Then, a central hole (5 mm diameter and 1 mm depth) was made in the surface of the acrylic block using a rotary instrument. Biodentine® was mixed following the manufacturer’s instructions and inserted in the holes of the acrylic blocks. According to the different setting times, half of the specimens (n = 30) were stored for 72 h or 7 days, at 37 °C, with 100% of humidity, in an incubator (Vacuum Oven DZF6050, Shanghai Hasuc Instrument Manufacture Co., Ltd, Shanghai, China). Then, the specimens were randomly divided into five experimental groups (n = 6) based on the surface treatment: negative control group (distilled water; Adesco, Mexico); NaClO group (5.25% NaClO; Clorox™, the Clorox Company, Oakland, CA, USA); EDTA group (17% EDTA; MD-Cleanser™ Smear Layer Remove, Metabiomed, Cheongju, Republic of Korea); CHX group (2% chlorhexidine; Consepsis™, Ultradent, South Jordan, UT, USA); and H3PO4 positive control group (37% H3PO4; Total Etch, Ivoclar Vivadent, Schaan, Liechtenstein). The corresponding irrigating solution was applied over the bioceramic material for 1 min. Subsequently, the Biodentine® surface was rinsed with distilled water and dried with pressurized air.
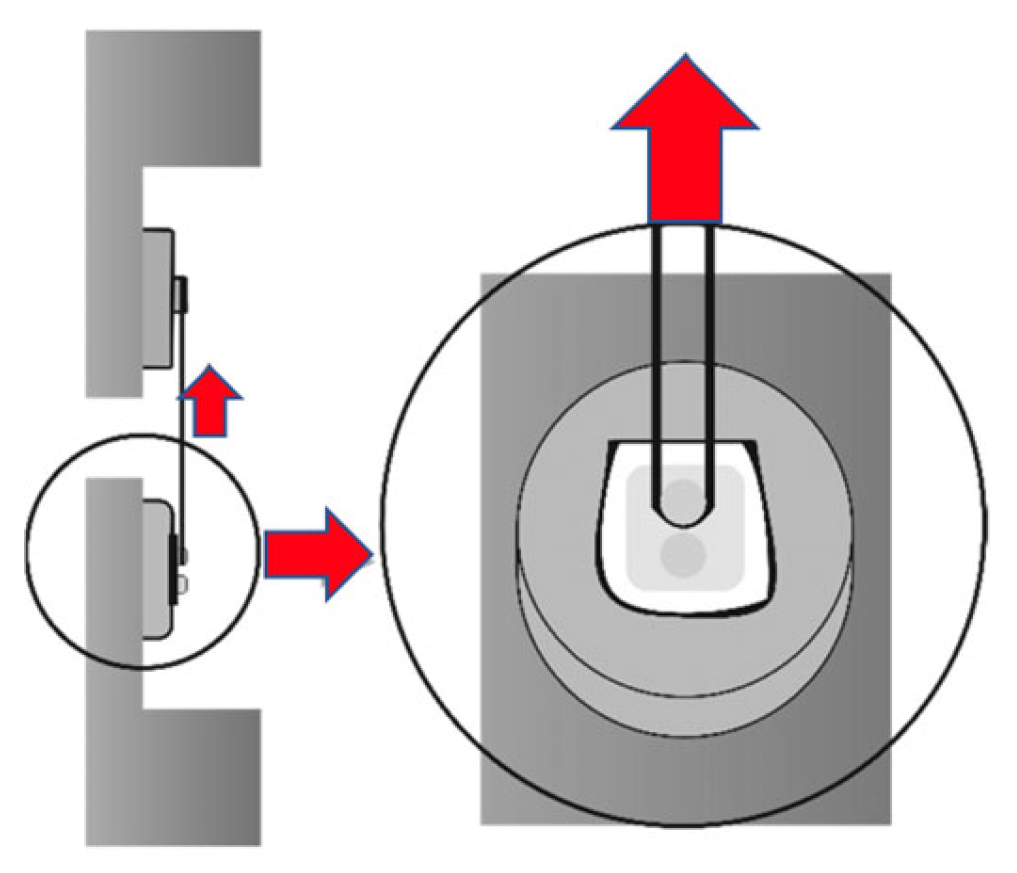
After the surface treatments, an elastomer mold (1.5 mm in diameter and 1.0 mm in thickness) with two cylindrical orifices was placed on the Biodentine®’s surface. The plastic molds containing the specimens were fixed to a microshear test device (Odeme Dental Research, Luzerna-SC, Brazil) (Figure 1).
Figure 1.
Diagram of the shear bond strength test. Red arrows indicate the direction of the force.
Each orifice was filled with Dyad FlowTM self-adhesive flowable composite (Kerr, Orange, CA, USA). The mold was then covered with a polyester strip and a glass slide, and the resin composite was photo-activated for 20 s with a Light-Emitting Diode light-curing unit (Bluephase16i, Ivoclar Vivadent, Schaan, Liechtenstein) with an irradiance of 1100 mW/cm2. After that, the elastomer mold was carefully removed. All specimens were stored in distilled water at 37 °C with 100% relative humidity to simulate the oral-environment clinical conditions.
2.1. Evaluation of Shear Bond Strength
SBS was measured in different aging periods. These aging times were chosen following the directions of the ISO/TS 11405 International Standard [23]. Since each cylinder had two Dyad FlowTM samples attached to its surface, one was tested after 24 h of aging, and the other one after 6 months. To ensure consistency, a single investigator prepared and tested all the samples.
To measure the SBS, a stainless-steel wire (0.2 mm diameter) was looped around the Dyad FlowTM resin block and aligned to the bonded interface. The SBS test was conducted using a mechanical testing machine (Instron 4465, MA, USA) at a speed of 1 mm/min until failure and a load cell of 500 N. SBS was calculated by dividing the maximum force achieved by the area of the bonded specimens.
2.2. Evaluation of Mechanical Failure
Failures were observed under a stereomicroscope (Renfert, Hilzingen, Germany) at 15× and classified into 3 types: adhesive, cohesive, or mixed [24].
- (a)
- Adhesive: fracture occurring between the composite resin and the bioceramic cement, with no composite resin remnants on the bioceramic surface.
- (b)
- Cohesive: fracture within the composite resin, with resin remnants covering most of the bioceramic surface.
- (c)
- Mixed: a combination of adhesive and cohesive failure, with some areas of the bioceramic showing composite resin remnants and others without.
2.3. Statistical Analysis
The statistical tests were performed using Sigma Plot 14.0 software. The data were analyzed to verify the normal distribution and variance homogeneity of the samples. A two-way analysis of variance (ANOVA) test was performed to analyze the effect of the different irrigating solutions and setting times on the SBS of Biodentine® and Dyad FlowTM. The level of significance was set to a ≤ 0.05.
3. Results
3.1. Evaluation of Shear Bond Strength
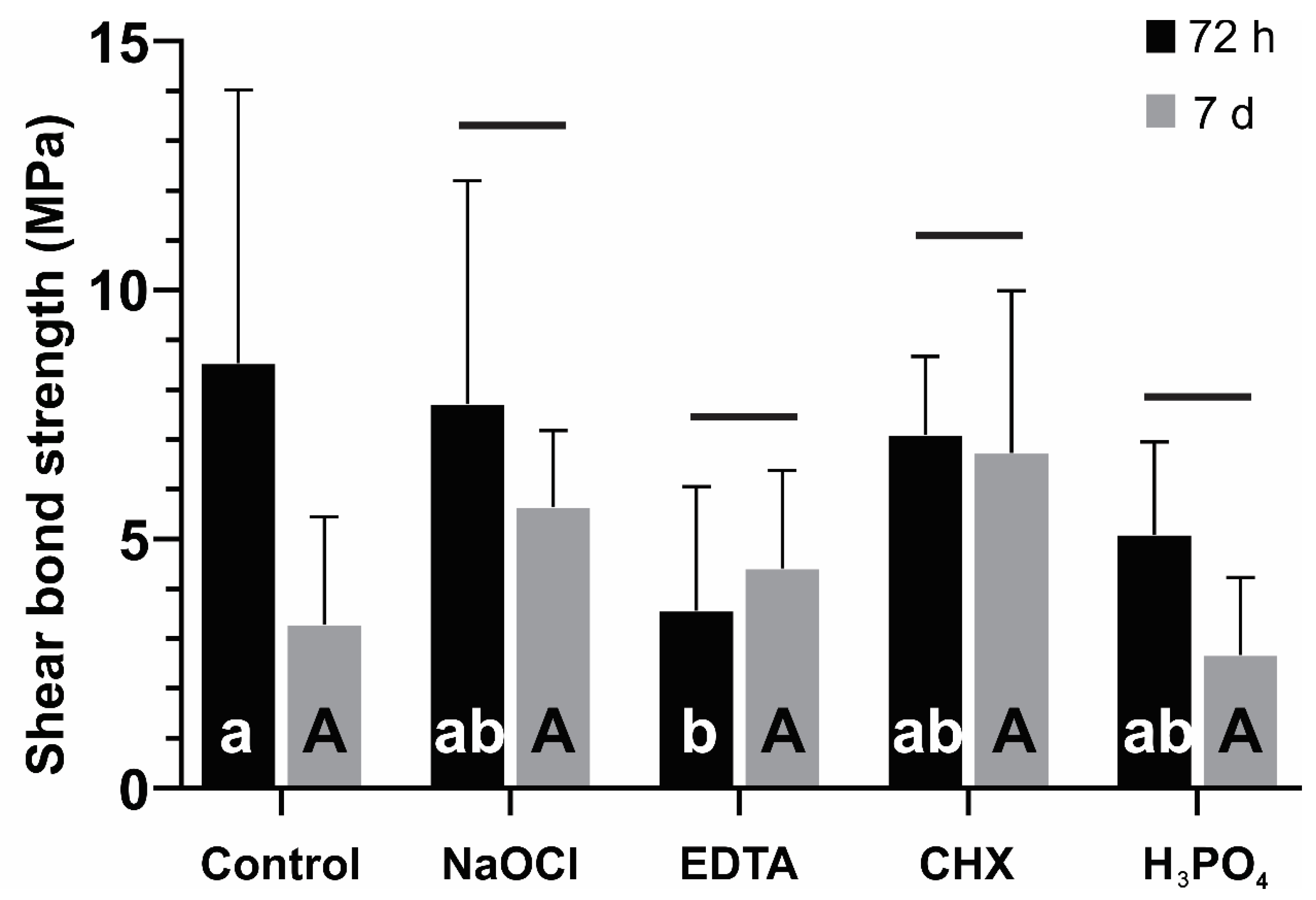
The means and standard deviations of the SBS values for each storing condition are summarized in Figure 2 and Figure 3. The two-way ANOVA test revealed that SBS values at 24 h were significantly influenced by both factors: the surface treatment (p = 0.029) and the setting time (p = 0.018). However, the interaction between these factors was not significant (p = 0.131). After 72 h of setting, when compared to the control, only EDTA achieved statistically significant lower values (p < 0.05). After 7 days of setting, no statistically significant values were observed among the groups (p > 0.05). When comparing the 72 h and 7-day setting time, only the control group had statistically significant differences, being that the SBS values at 7 days were lower than those observed at 72 h (Figure 2).
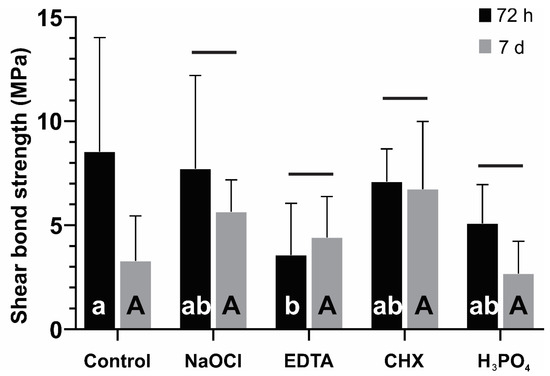
Figure 2.
Shear bond strength (MPa) measured after 24 h of the Dyad FlowTM application over a Biodentine® cylinder as a function of the setting time of the material (72 h and 7 days) and the irrigant solution used. The bars under the same horizontal line indicate that no statistically significant differences between the 72 h and the 7-day setting time of the bioceramic material were observed. Lowercase letters indicate differences between the irrigating solutions when they were applied to the bioceramic material and set for 72 h. Capital letters indicate differences between the irrigating solutions when they were applied to the bioceramic material and set for 7 days.
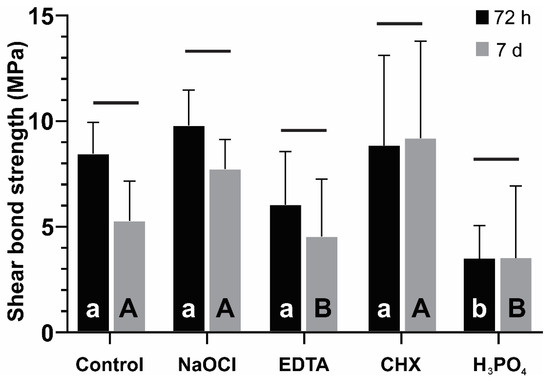
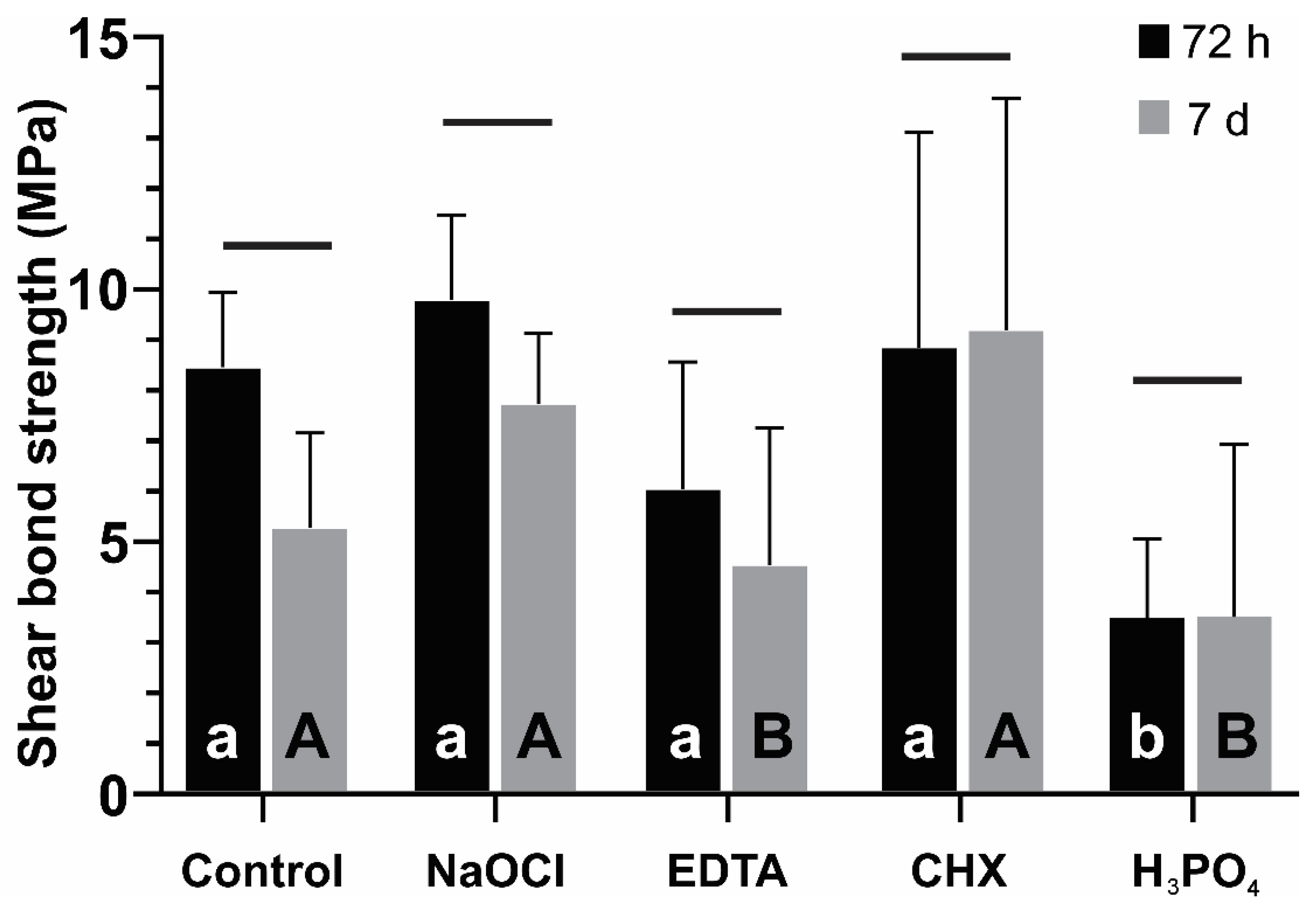
Figure 3.
Shear bond strength (MPa) measured after 6 months of the Dyad FlowTM application over a Biodentine® cylinder as a function of the setting time of the material (72 h and 7 days) and the irrigant solution used. The bars under the same horizontal line indicate that no statistically significant differences between the 72 h and the 7-day setting time of the bioceramic material were observed. Lowercase letters indicate differences between the irrigating solutions when they were applied to the bioceramic material and set for 72 h. Capital letters indicate differences between the irrigating solutions when they were applied to the bioceramic material and set for 7 days.
On the other hand, the SBS values at 6 months were influenced by the irrigating solutions (p < 0.001) but not by the setting time (p = 0.083) or the interaction between these factors (p = 0.514). At 72 h setting, when compared to the control, only H3PO4 achieved statistically significant lower values (p < 0.05). At 7 days of setting, statistically significant values were observed in EDTA and H3PO4 groups. When comparing the 72 h and 7-day setting time, no group had statistically significant differences (Figure 3).
3.2. Evaluation of Mode of Failure
The modes of failure of the specimens after the SBS test at 24 h and 6 months are presented in Table 2 and Table 3. Adhesive failure predominated in all groups. This is associated with low bond strengths between Biodentine® and Dyad FlowTM.

Table 2.
Mode of failure after 24 h of aging.

Table 3.
Mode of failure after 6 months of aging.
4. Discussion
The success of endodontic treatments, when a bioceramic is used, does not depend only on the sealing of the material to the tooth. Many factors, such as the disinfection of the root canal system and the proper bonding of the restoration to the bioceramic, are key parameters as well [1,3]. The SBS is the method used for evaluating the interfacial adhesion between the substrate and the bonded material [22], so the purpose of this study was to evaluate the effect of various irrigating solutions and setting times in the SBS between Biodentine® and Dyad FlowTM. In this study, the null hypothesis tested was partially rejected. In first place, the results showed that the SBS was not influenced by the interaction between the surface treatment and the setting time. However, the different surface treatments did influence the SBS.
The present study did not find significant changes in the SBS between Biodentine® and Dyad FlowTM at 72 h and 7 days. This result may be explained by the final setting time of the bioceramic; in accordance with studies that evaluated the setting time of Biodentine®, Grech et al., [15] according to ISO standard 9917–1:2007 [25], concluded that the final setting time was 45 min; on the other hand, Kaup et al., [26] reported a setting time of 85.66 min, using ISO 6876:2012 standard [27]. Also, some studies that evaluated the physical and mechanical properties of Biodentine® reported that the initial setting reaction occurs at 12 min, and it takes up to 2 weeks to achieve complete maturation [6,20,28,29]. Moreover, Villat et al., [13] characterized the setting process of Biodentine® using impedance spectroscopy and found that at least 14 days were necessary so that the impedance values are stabilized for this calcium silicate-based cement.
It is important to note that the setting time of Biodentine® is linked to the reaction that starts after mixing the powder with the liquid. The calcium silicate particles of Biodentine® react with water to form a high-pH solution containing Ca2+, OH−, and silicate ions; subsequently, the hydration reaction between tricalcium silicate and dicalcium silicate forms a calcium hydroxide and calcium silicate hydrate gel (C-S-H), producing an alkaline pH due to the release of calcium hydroxide ions [3,6]. Afterwards, the crystallization of the C-S-H gel structure occurs through continuous hydration and results in the formation of calcium carbonate crystals in between the unreacted grains [3,6,14]. About this, Camilleri et al., [14] reported that the heat flux generated during tricalcium silicate hydration in water at 37 °C presented a strong exothermic peak starting at 90 min and passing through a maximum at 210 min. The first 90 min corresponded to the induction period, followed by the initial setting and then the hardening of the tricalcium silicate paste. Therefore, during this process, the structure of Biodentine® increases its hardness, reduces its porosity, and becomes relatively impermeable to water [14,20].
On the other hand, the root canals’ disinfection and the restorative process are important procedures for the success of the endodontic treatment [7,16,17,18]. In the disinfection, the bioceramic material gets in touch with irrigating solutions such as NaClO, CHX, and EDTA [16,17]. Furthermore, in the restorative process, the surface of the bioceramic may be in contact with H3PO4 [30,31].
In this study, irrigating solutions were applied on Biodentine® before the restorative procedure. The results demonstrated that the SBS at 24 h decreased with the application of EDTA at 72 h. Also, the SBS at 6 months decreased with EDTA after 7 days. This irrigating solution is a chelating agent, and its principal function is to demineralize. Consequently, this effect can enhance the loss of Ca+ ions on Biodentine®’s surface, as well as the dentine of the tooth [17]. For this reason, the SBS could have diminished [17,32]. Yan et al., [32] evaluated the effects of NaClO (5.25%), CHX (2%) and Glyde File Prep (15% EDTA and urea peroxide) on the bond strengths of the Mineral Trioxide Aggregate (MTA) dentine in vitro and suggested that Glyde File Prep could negatively affect the bond strengths of MTA to dentine. Furthermore, Lee et al., [33] evaluated the effects of EDTA on MTA and concluded that this solution was the cause of the poor crystallization of the C-S-H gel. Accordingly, some studies have reported that EDTA affected the properties of MTA and Biodentine®, such as the microhardness and flexural strength [33,34,35]. However, there is no scientific evidence that correlates the above properties with the bond strength.
When comparing the negative control group setting times, the SBS at 24 h presented statistically significant differences; SBS values at 7 days were lower than those observed at 72 h. This may be caused by the washout resistance of Biodentine®. In regard to this, Grench et al., [15] found that Biodentine® had a very high washout tendency, as the loss of material increased with every drop of fluid.
A decrease in the SBS at 6 months was observed when H3PO4 was applied at 72 h and 7 days. The bonding mechanism of Dyad FlowTM to bioceramic cements is similar to the way that self-etch adhesives bonds to calcium in the tooth structure; it relies on the adhesive monomer glycerol phosphate dimethacrylate (GPDM), which mainly binds to calcium ions, while its phosphate group is responsible for the acid etching [36,37,38]. However, some studies reported that the SBS of Dyad FlowTM on enamel and dentine presented significantly lower bond strengths than conventional composites applied with adhesives [36,38]. As a consequence, the application of a H3PO4 etchant for improved adhesion capability on enamel and dentine was suggested [39]. Additionally, Altunsoy et al., [40] observed that the SBS between Biodentine® and Dyad FlowTM was lower in comparison with other flowable composites. For this reason, in this study, H3PO4 was used for the etching conditioning on Biodentine®’s surface as a positive control group. Regarding this, Kayahan et al., [30] reported that the acid etching of MTA caused the loss of the matrix around the crystalline structure; this process favored the formation of a structure that could enhance the SBS. However, Hardan et al. [41], in the systematic review of bond strength of adhesive systems to calcium silicate, observed the low bond strength of aged Biodentine® and concluded that the surface hardness of Biodentine® increases with time, thus resulting in reduced micro-mechanical retention and a shallower etching pattern. Also, in another study, Camilleri et al., [14] reported that Biodentine® exhibited a reduction in the chloride peak height and a lower calcium-to-silicon ratio when etched with 37% H3PO4. Similarly, Meraji et al., [42] found that Biodentine® exhibited changes in the material microstructure in the total-etch method. In both cases, important structural changes occurred diminishing Biodentine®’s mechanical properties [14,40].
Even more, Elnaghy et al., [43] evaluated the surface microhardness, compressive strength, bond strength, and morphologic microstructures of Biodentine® after exposure to a range of acidic pH levels; they found that the microstructure of Biodentine®’s surfaces exposed to a pH value of 7.4 showed an amorphous, poorly crystallized superficial gel and concluded that this affected the physical properties of the bioceramic material. Hence, the explanation of these results could be that the acid pH value that is produced in the demineralization process with EDTA [33] or the acidic nature of H3PO4 can buffer the Biodentine®’s alkalinity [28], affecting the bonding between the bioceramic and the restorative material.
The analysis of failure from the specimens in this study demonstrated that the predominant failure type for all groups was the adhesive type. Hence, there was no physical or chemical interaction between the Biodentine® and the self-adhering flowable composite [28,32]. The possible causes of the adhesive failure were that the irrigating solutions altered the union between the substrates, or that the Dyad FlowTM bonding system, which has an all-in-one system that eliminates the need for etching, priming, and bonding prior to its placement, was not enough to resist failure [37,39].
One limitation of this study was that other bonding systems were not considered, since this study was performed only with a self-adhesive flowable composite; therefore, a comparison with other etch-and-rinse or self-etch adhesive systems was not considered. On the other hand, the present study did not include the evaluation of the surface morphology with the application of different irrigating solutions. Another limitation of this study is the absence of a comprehensive analysis using the Adhesive Remnant Index (ARI) to quantify the adhesive failures and the lack of fractographic images to visually confirm the failure modes. The exclusion of these assessments may lead to an incomplete understanding of the failure mechanisms, which could impact the interpretation of the bond strength results. Additionally, the study did not account for the potential variations in clinical conditions, such as moisture control and operator technique, which may influence the bond strength outcomes in a real-world setting. Future research should incorporate these elements to provide a more robust evaluation of the adhesive performance of bioceramic materials. Therefore, it is suggested to carry out future studies including these characteristics.
5. Conclusions
In conclusion, the findings of this study can be summarized:
- ○
- Adequate setting time: When the bioceramic material has a sufficient setting time, it does not significantly impact the SBS.
- ○
- Effect of EDTA and H3PO4: The application of EDTA as an irrigating solution or the use of H3PO4 on the surface of Biodentine® reduces the SBS.
- ○
- Surface treatment consideration: Proper surface treatment of Biodentine® is crucial to ensure the success of endodontic and restorative treatments.
Author Contributions
Conceptualization, A.A.-O. and C.E.C.-S.; methodology, R.B., C.E.C.-S., A.J.M.-Á., L.H., L.E.R.-V., A.F., B.I.F.-F. and N.K.; software, R.C.-B., R.B., Y.H. and N.K.; validation, A.A.-O. and C.E.C.-S.; formal analysis, R.C.-B., R.B., Y.H. and N.K.; investigation, A.J.M.-Á., L.H., L.E.R.-V., B.I.F.-F. and Y.H.; resources, R.C.-B., R.B., A.F., Y.H. and N.K.; data curation, A.A.-O. and C.E.C.-S.; writing—original draft preparation, A.A.-O., R.C.-B., R.B., Y.H. and N.K.; writing—review and editing, R.B., L.H., Y.H. and C.E.C.-S., visualization, R.B., supervision, C.E.C.-S.; project administration, N.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding authors.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Silva, L.A.B.; Pieroni, K.A.M.G.; Nelson-Filho, P.; Silva, R.A.B.; Hernandéz-Gatón, P.; Lucisano, M.P.; Paula-Silva, F.W.G.; de Queiroz, A.M. Furcation Perforation: Periradicular Tissue Response to Biodentine as a Repair Material by Histopathologic and Indirect Immunofluorescence Analyses. J. Endod. 2017, 43, 1137–1142. [Google Scholar] [CrossRef]
- Septodont. Biodentine Active Biosilicate Technology. 2022. Available online: http://www.septodont.co.uk/sites/uk/files/201608/brochure%20Biodentine%20HD%20UK.pdf (accessed on 20 August 2024).
- Kaur, M.; Singh, H.; Dhillon, J.S.; Batra, M.; Saini, M. MTA versus Biodentine: Review of Literature with a Comparative Analysis. J. Clin. Diagn. Res. 2017, 11, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Malkondu, Ö.; Kazandağ, M.K.; Kazazoğlu, E. A Review on Biodentine, a Contemporary Dentine Replacement and Repair Material. Biomed. Res. Int. 2014, 2014, 160951. [Google Scholar] [CrossRef] [PubMed]
- Laurent, P.; Camps, J.; About, I. Biodentine Induces TGF-β1 Release from Human Pulp Cells and Early Dental Pulp Mineralization. Int. Endod. J. 2012, 45, 439–448. [Google Scholar] [CrossRef] [PubMed]
- Bachoo, I.K.; Seymour, D.; Brunton, P. A Biocompatible and Bioactive Replacement for Dentine: Is This a Reality? The Properties and Uses of a Novel Calcium-Based Cement. Br. Dent. J. 2013, 214, E5. [Google Scholar] [CrossRef] [PubMed]
- Koubi, G.; Colon, P.; Franquin, J.-C.; Hartmann, A.; Richard, G.; Faure, M.-O.; Lambert, G. Clinical Evaluation of the Performance and Safety of a New Dentine Substitute, Biodentine, in the Restoration of Posterior Teeth-A Prospective Study. Clin. Oral Investig. 2013, 17, 243–249. [Google Scholar] [CrossRef]
- Al-Rayesse, R.; Al-Jabban, O.; Eid, A.; Kabtoleh, A.; Addiego, F.; Mancino, D.; Haikel, Y.; Kharouf, N. Influence of Bioceramic Cements on the Quality of Obturation of the Immature Tooth: An In Vitro Microscopic and Tomographic Study. Bioengineering 2024, 11, 213. [Google Scholar] [CrossRef]
- Ashi, T.; Mancino, D.; Hardan, L.; Bourgi, R.; Zghal, J.; Macaluso, V.; Al-Ashkar, S.; Alkhouri, S.; Haikel, Y.; Kharouf, N. Physicochemical and Antibacterial Properties of Bioactive Retrograde Filling Materials. Bioengineering 2022, 9, 624. [Google Scholar] [CrossRef]
- Mishra, S.; Taneja, S.; Bhalla, V.K.; Rathore, A. Outcome of Novel Pulp Capping Modalities after Full Pulpotomy in Teeth Diagnosed with Irreversible Pulpitis: A Prospective Randomized Clinical Trial. J. Conserv. Dent. Endod. 2024, 27, 205–213. [Google Scholar] [CrossRef]
- Agarwal, N.S.; Singh, S.; Chandrasekhar, P.; Kulkarni, G.; Podar, R. Conservative Nonsurgical Approach for Management of a Case of Type II Dens in Dente. Case Rep. Dent. 2024, 2024, 8843758. [Google Scholar] [CrossRef]
- Parmar, S.; Aggarwal, N.; Gupta, H.; Marwaha, J.; Pundir, P.; Saini, R. Comparative Evaluation of the Push-Out Bond Strength of Glass Ionomer Cement, Mineral Trioxide Aggregate, Biodentine, and Endosequence Root Repair Material in Repair of Furcation Perforations: An In Vitro Study. J. Pharm. Bioallied Sci. 2024, 16, S552–S554. [Google Scholar] [CrossRef] [PubMed]
- Villat, C.; Tran, V.X.; Pradelle-Plasse, N.; Villat, C.; Tran, V.X.; Pradelle-Plasse, N.; Ponthiaux, P.; Wenger, F.; Grosgogeat, B.; Colon, P. Impedance Methodology: A New Way to Characterize the Setting Reaction of Dental Cements. Dent. Mater. 2010, 26, 1127–1132. [Google Scholar] [CrossRef] [PubMed]
- Camilleri, J.; Sorrentino, F.; Damidot, D. Investigation of the Hydration and Bioactivity of Radiopacified Tricalcium Silicate Cement, Biodentine and MTA Angelus. Dent. Mater. 2013, 29, 580–593. [Google Scholar] [CrossRef] [PubMed]
- Grech, L.; Mallia, B.; Camilleri, J. Investigation of the Physical Properties of Tricalcium Silicate Cement-Based Root-End Filling Materials. Dent. Mater. 2013, 29, e20–e28. [Google Scholar] [CrossRef]
- Ercan, E.; Ozekinci, T.; Atakul, F.; Gül, K. Antibacterial Activity of 2% Chlorhexidine Gluconate and 5.25% Sodium Hypochlorite in Infected Root Canal: In Vivo Study. J. Endod. 2004, 30, 84–87. [Google Scholar] [CrossRef] [PubMed]
- Hülsmann, M.; Heckendorff, M.; Lennon, A. Chelating Agents in Root Canal Treatment: Mode of Action and Indications for Their Use. Int. Endod. J. 2003, 36, 810–830. [Google Scholar] [CrossRef]
- Guneser, M.B.; Akbulut, M.B.; Eldeniz, A.U. Effect of Various Endodontic Irrigants on the Push-out Bond Strength of Biodentine and Conventional Root Perforation Repair Materials. J. Endod. 2013, 39, 380–384. [Google Scholar] [CrossRef]
- Camilleri, J. Investigation of Biodentine as Dentine Replacement Material. J. Dent. 2013, 41, 600–610. [Google Scholar] [CrossRef]
- Hashem, D.F.; Foxton, R.; Manoharan, A.; Watson, T.F.; Banerjee, A. The Physical Characteristics of Resin Composite–Calcium Silicate Interface as Part of a Layered/Laminate Adhesive Restoration. Dent. Mater. 2014, 30, 343–349. [Google Scholar] [CrossRef]
- Kharouf, N.; Reitzer, F. Est-il possible de coller sur les biocéramique? Le point due vue du chercheur. CLINIC 2024, 45, 300–303. [Google Scholar]
- Cengiz, E.; Ulusoy, N. Microshear Bond Strength of Tri-Calcium Silicate-Based Cements to Different Restorative Materials. J. Adhes. Dent. 2016, 18, 231–237. [Google Scholar] [CrossRef]
- ISO/TS 11405:2015; Dentistry-Testing of Adhesion to Tooth Structure. International Organizazion for Standardization: Geneva, Switzerland, 2015.
- Ishibe, M.; Raigrodski, A.J.; Flinn, B.D.; Chung, K.H.; Spiekerman, C.; Winter, R.R. Shear bond strengths of pressed and layered veneering ceramics to high-noble alloy and zirconia cores. J. Prosthet. Dent. 2011, 106, 29–37. [Google Scholar] [CrossRef] [PubMed]
- ISO 9917-1:2007; Dentistry—Water-Based Cements. International Organizazion for Standardization: Geneva, Switzerland, 2007.
- Kaup, M.; Dammann, C.H.; Schäfer, E.; Dammaschke, T. Shear Bond Strength of Biodentine, ProRoot MTA, Glass Ionomer Cement and Composite Resin on Human Dentine Ex Vivo. Head Face Med. 2015, 11, 16. [Google Scholar] [CrossRef] [PubMed]
- ISO 6876:2012; Dentistry—Root Canal Sealing Materials. International Organizazion for Standardization: Geneva, Switzerland, 2012.
- Odabas, M.E.; Bani, M.; Tirali, R.E. Shear Bond Strengths of Different Adhesive Systems to Biodentine. Sci. World J. 2013, 2013, 1–5. [Google Scholar] [CrossRef]
- Mustafa, R.M.; Al-Nasrawi, S.J.; Aljdaimi, A.I. The Effect of Biodentine Maturation Time on Resin Bond Strength When Aged in Artificial Saliva. Int. J. Dent. 2020, 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kayahan, M.B.; Neekofar, M.H.; Kazanda, M. Effect of Acid-Etching Procedure on Selected Physical Properties of Mineral Trioxide Aggregate. Int. Endod. J. 2009, 42, 1004–1014. [Google Scholar] [CrossRef] [PubMed]
- Kayahan, M.B.; Nekoofar, M.H.; McCann, A.; Kazanda, M. Effect of Acid Etching Procedures on the Compressive Strength of 4 Calcium Silicate–Based Endodontic Cements. J. Endod. 2013, 39, 1646–1648. [Google Scholar] [CrossRef]
- Yan, P.; Peng, B.; Fan, B.; Fan, M.; Bian, Z. The Effects of Sodium Hypochlorite (5.25%), Chlorhexidine (2%), and Glyde File Prep on the Bond Strength of MTA-Dentin. J. Endod. 2006, 32, 58–60. [Google Scholar] [CrossRef]
- Lee, Y.L.; Lin, F.H.; Wang, W.H.; Ritchie, H.H. Effects of EDTA on the hydration mechanism of mineral trioxide aggregate. J. Dent. Res. 2007, 86, 534–538. [Google Scholar] [CrossRef]
- Aggarwal, V.; Jain, A.; Kabi, D. In vitro evaluation of effect of various endodontic solutions on selected physical properties of white mineral trioxide aggregate. Aust. Endod. J. 2011, 37, 61–64. [Google Scholar] [CrossRef]
- Ballal, V.; Marques, J.N.; Campos, C.N.; Gudipaneni, R.; Yeraballi, D. Effects of chelating agent and acids on Biodentine. Aust. Dent. J. 2018, 63, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Vichi, A.; Margvelashvili, M.; Goracci, C.; Papacchini, F.; Ferrari, M. Bonding and sealing ability of a new self-adhering flowable composite resin in class I restorations. Clin. Oral Investig. 2013, 17, 1497–1506. [Google Scholar] [CrossRef] [PubMed]
- Peterson, J.; Rizk, M.; Hoch, M.; Stansbury, J.; Gladys, S. Bonding performance of self-adhesive flowable composites to enamel, dentin and a nano-hybrid composite. Odontology. 2018, 106, 171–180. [Google Scholar] [CrossRef]
- David, C.; De Cardoso, G.C.; Insolan, C.P.; Melo, T.; Flores-Sahagun, T.H.; Cuevas-Suárez, C.E. Bond strength of self-adhesive flowable composite resins to dental tissues: A systematic review and meta-analysis of in vitro studies. J. Prosthet. Dent. 2021, 128, 1–10. [Google Scholar] [CrossRef]
- Taschner, M.; Nato, F.; Mazzoni, A.; Breschi, L.; Petschelt, A.; Breschi, L. Role of preliminary etching for one-step self-etch adhesives. Eur. J. Oral Sci. 2010, 118, 517–524. [Google Scholar] [CrossRef]
- Altunsoy, M.; Tanrıver, M.; Ok, E.; Kucukyilmaz, E. Shear bond strength of a self-adhering flowable composite and a flowable base composite to mineral trioxide aggregate, calcium-enriched mixture cement, and Biodentine. J. Endod. 2015, 41, 1691–1695. [Google Scholar] [CrossRef] [PubMed]
- Hardan, L.; Mancino, D.; Bourgi, R.; Alvarado-Orozco, A.; Rodriguez-Vilchis, L.E.; Flores-Ledesma, A.; Cuevas-Suarez, C.E.; Lukomska-Szymanska, M.; Eid, A.; Danhache, M.L.; et al. Bond Strength of Adhesive Systems to Calcium Silicate-Based Materials: A Systematic Review and Meta-Analysis of In Vitro Studies. Gels 2022, 8, 311. [Google Scholar] [CrossRef]
- Meraji, N.; Camilleri, J. Bonding over dentin replacement materials. J. Endod. 2017, 43, 1343–1349. [Google Scholar] [CrossRef]
- Elnaghy, A.M. Influence of acidic environment on properties of biodentine and white mineral trioxide aggregate: A comparative study. J. Endod. 2015, 40, 953–957. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).