Degradation of a Micro-Hybrid Dental Composite Reinforced with Polyaramide Fiber under the Influence of Cyclic Loads
Abstract
:Featured Application
Abstract
1. Introduction
2. Materials and Methods
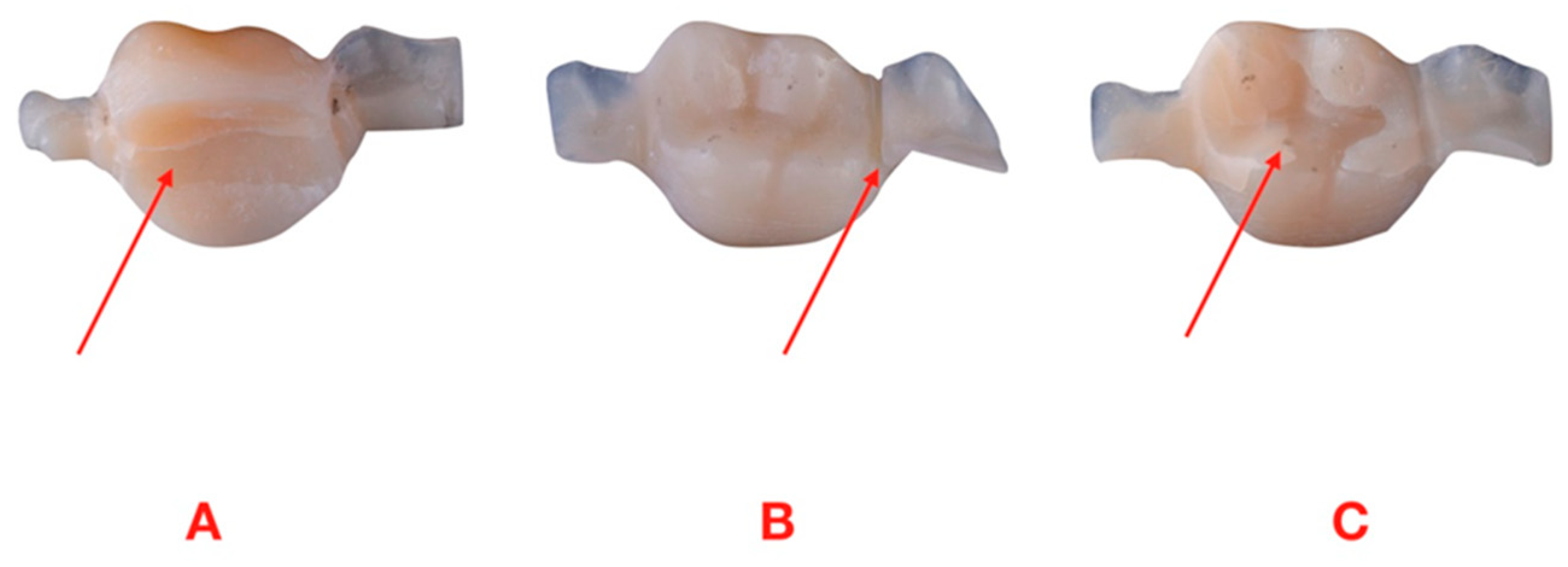
2.1. Preparation of the Test
2.2. Specimen Preparation
2.3. Fatigue Strength Test
2.4. Statistical Analysis
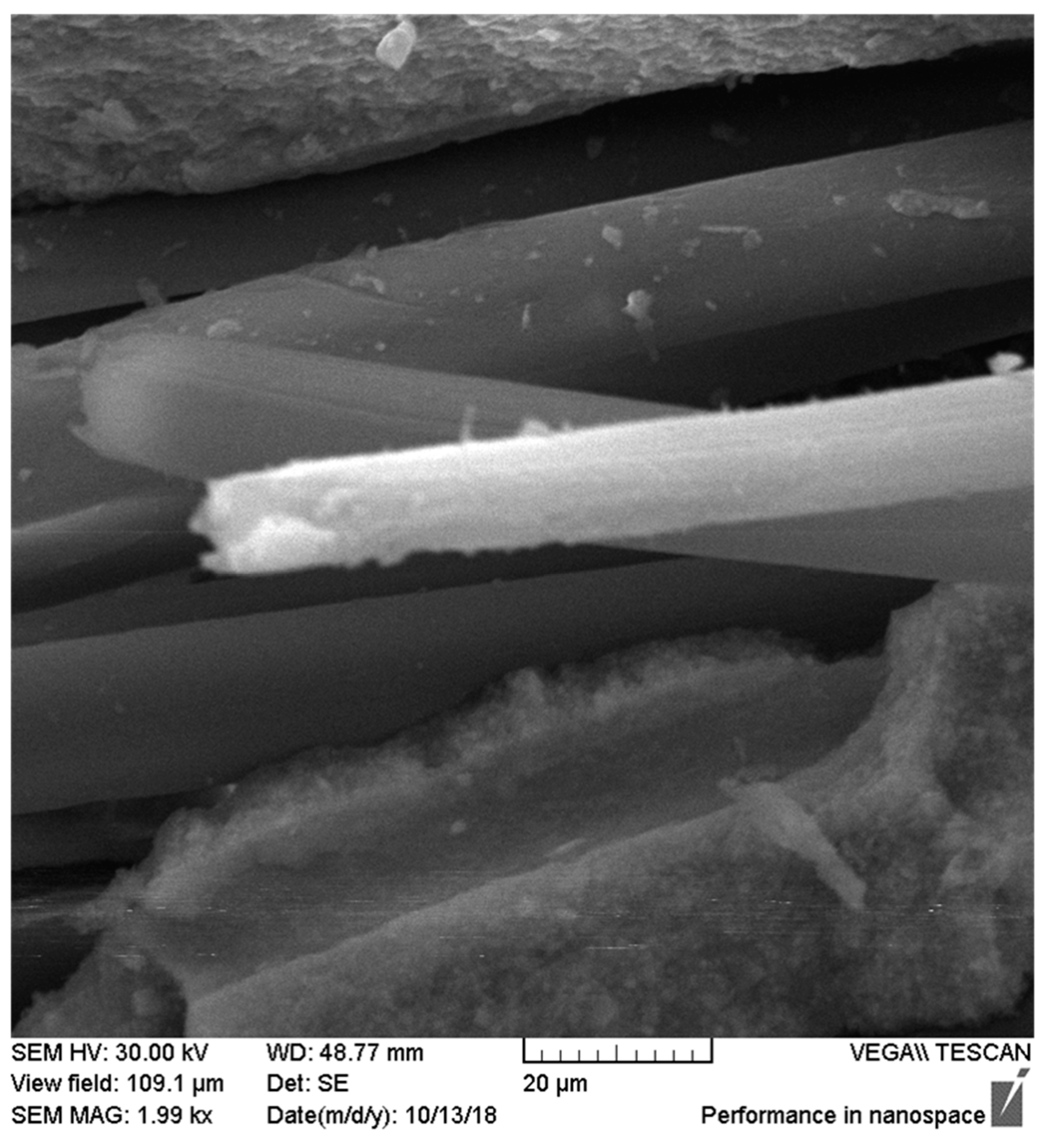
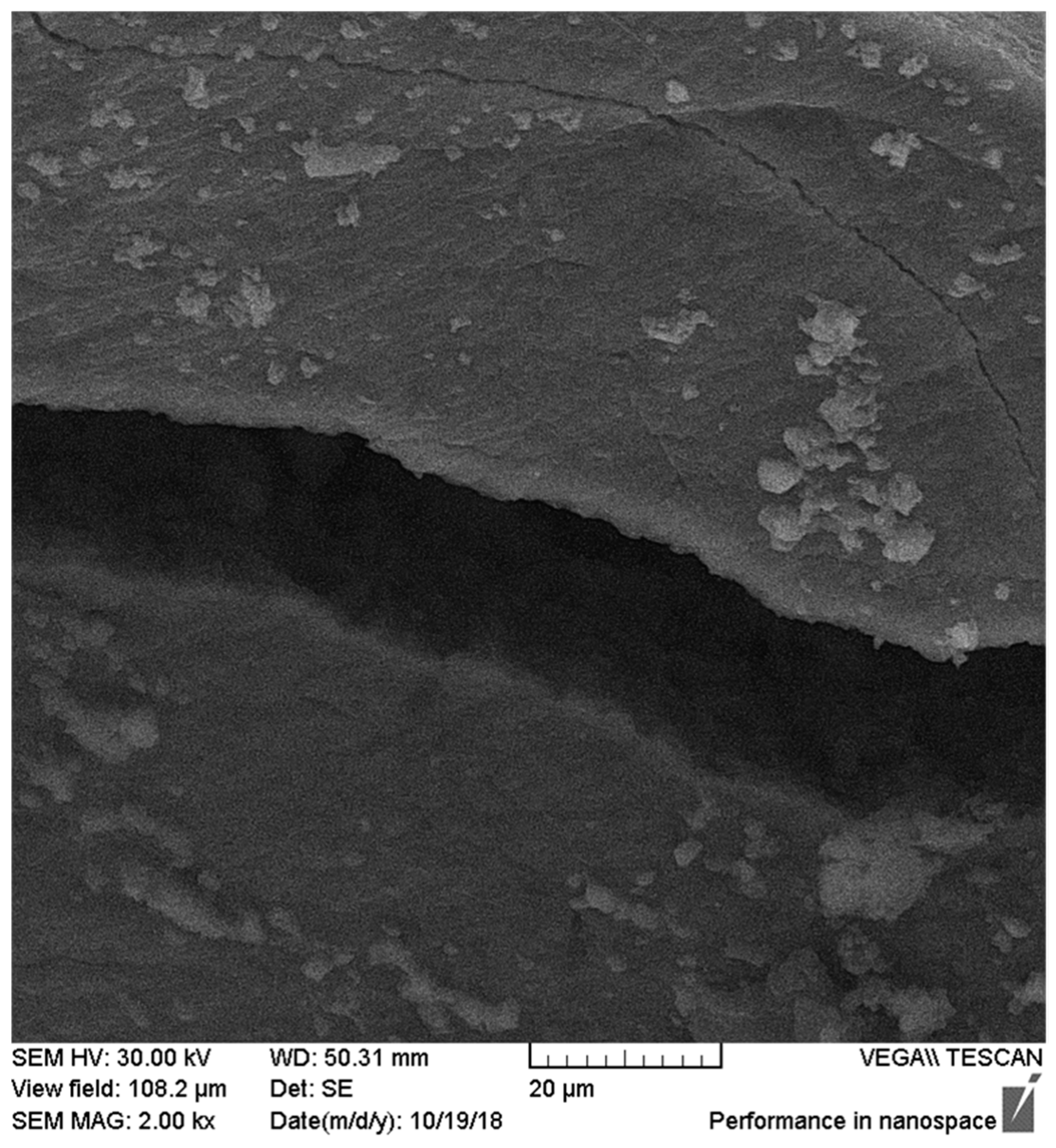
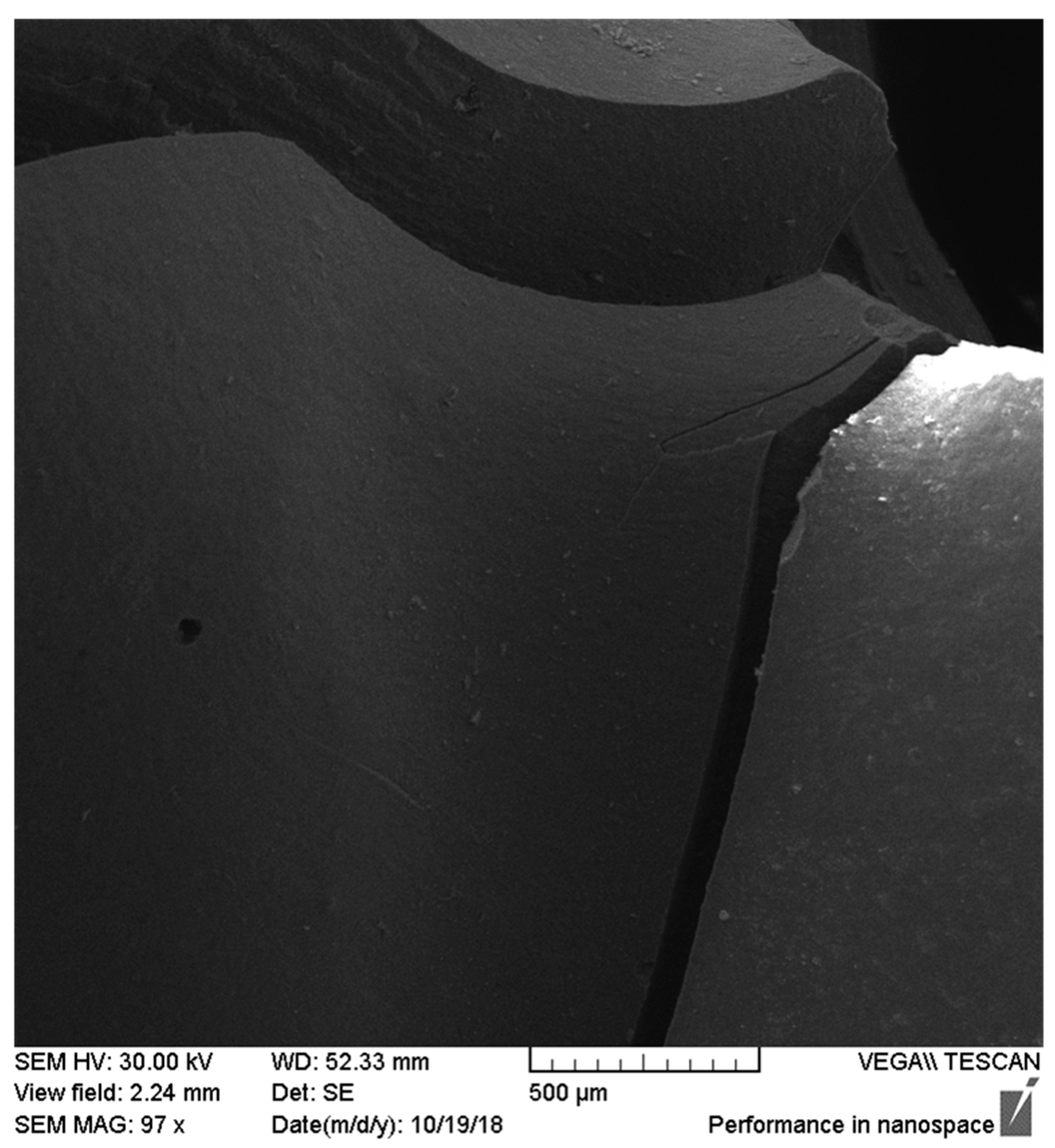
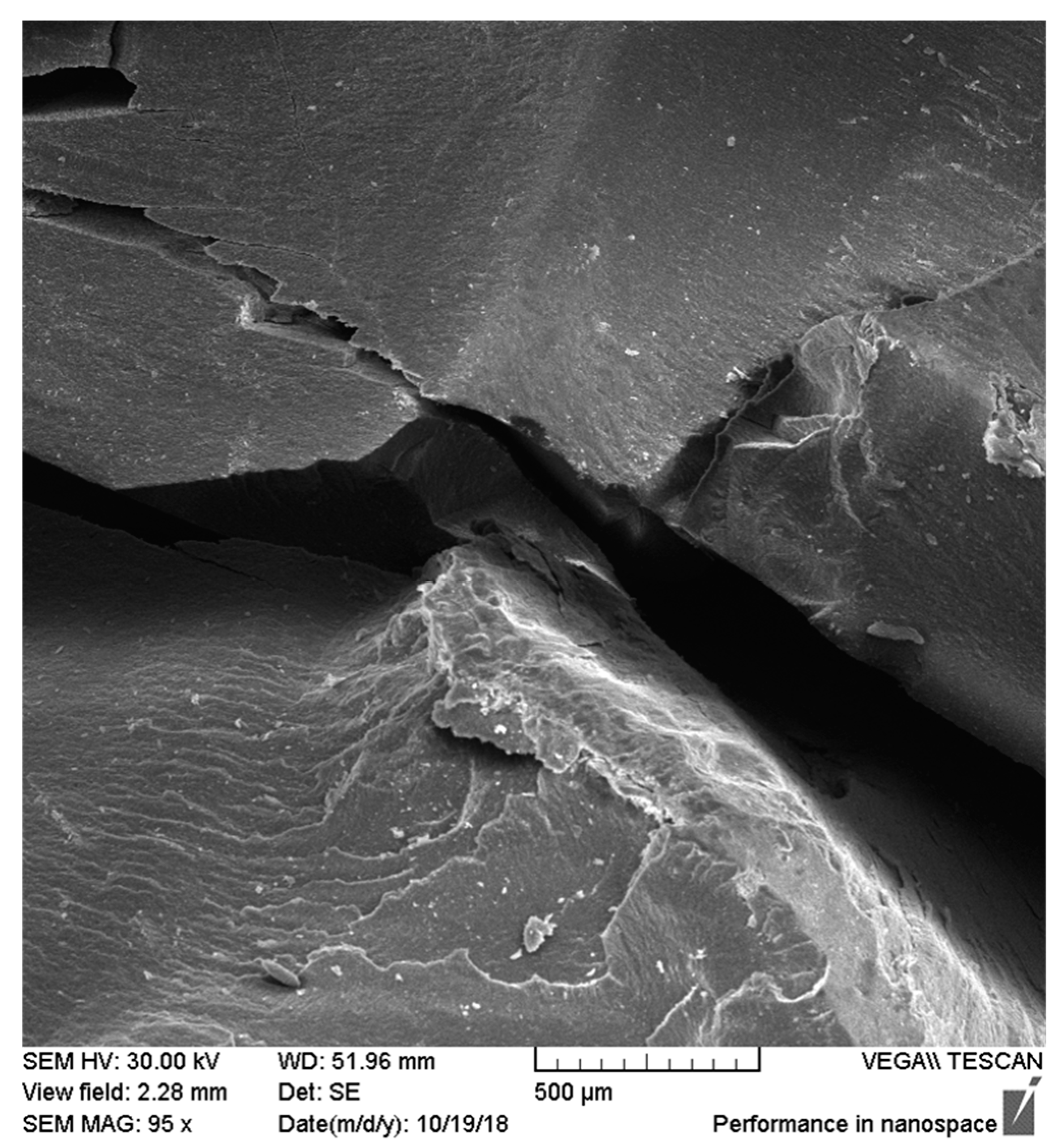
2.5. Microscope Observations
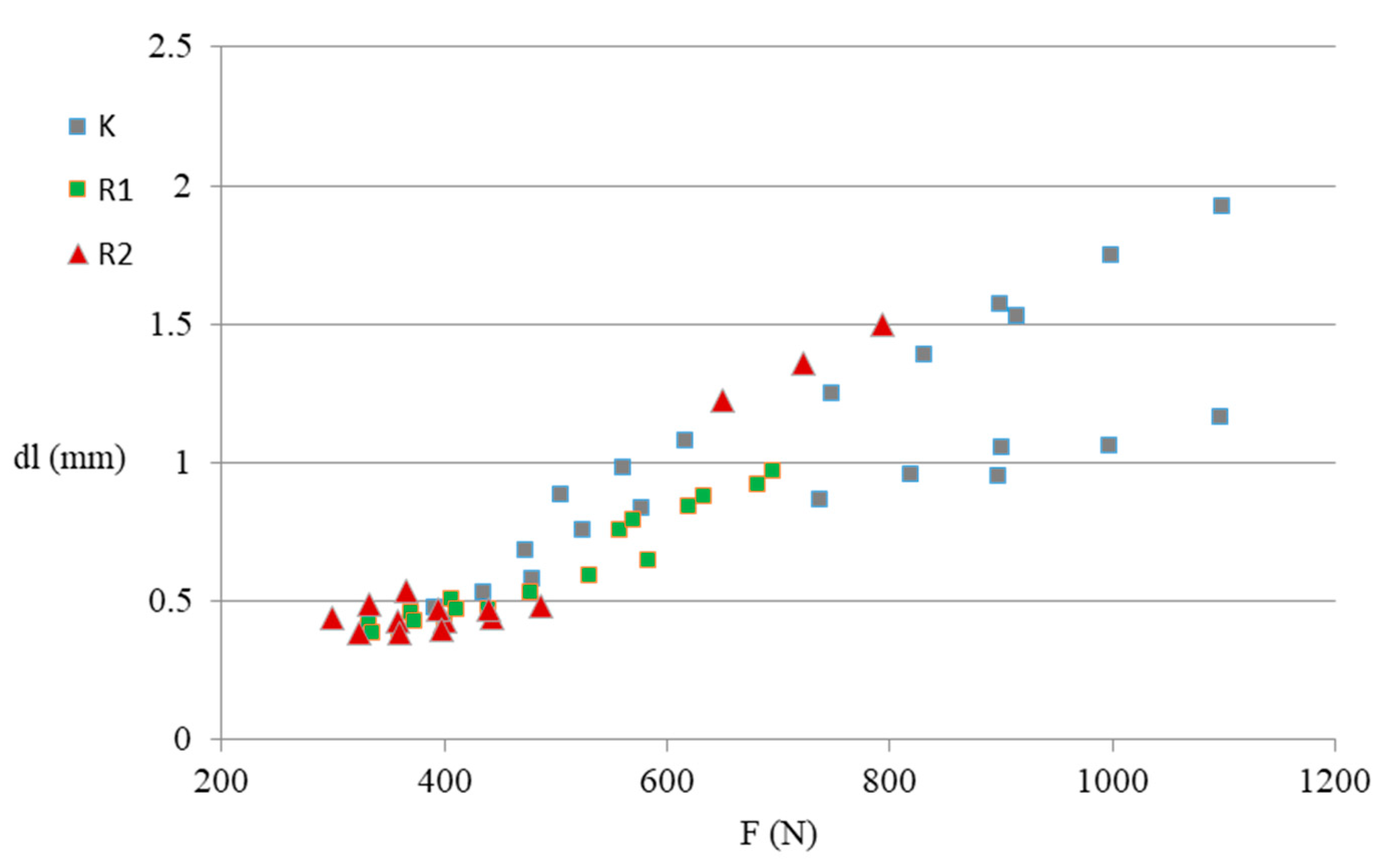
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Cramer, N.B.; Stansbury, J.W.; Bowman, C.N. Recent advances and developments in composite dental restorative materials. J. Dent. Res. 2011, 90, 402–416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khurshid, Z.; Zafar, M.; Qasim, S.; Shahab, S.; Naseem, M.; Abu Reqaiba, A. Advances in nanotechnology for restorative dentistry. Materials 2015, 8, 717–731. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wacławczyk, A.; Postek-Stefańska, L.; Pietraszewska, D.; Birkner, E.; Zalejska-Fiolka, J.; Wysoczańska-Jankowicz, I. TEGDMA and UDMA monomers released from composite dental material polymerized with diode and halogen lamps. Adv. Clin. Exp. Med. 2018, 27, 469–476. [Google Scholar] [CrossRef]
- Manojlovic, D.; Radisic, M.; Vasiljevic, T.; Zivkovic, S.; Lausevic, M.; Miletic, V. Monomer elution from nanohybrid and or mocer-based composites cured with different light sources. Dent. Mater. 2011, 27, 371–378. [Google Scholar] [CrossRef] [PubMed]
- LeSage, B.P. Aesthetic anterior composite restorations: A guide to direct placement. Dent. Clin. North. Am. 2007, 51, 359–378. [Google Scholar] [CrossRef] [PubMed]
- Sfondrini, M.F.; Massironi, S.; Pieraccini, G.; Scribante, A.; Vallittu, P.K.; Lassila, L.V.; Gandini, P. Flexural strengths of conventional and nanofilled fiber-reinforced composites: A three-point bending test. Dent. Traumatol. 2014, 30, 32–35. [Google Scholar] [CrossRef] [PubMed]
- Acharya, P.P.; Bhat, R. The physiochemical properties of dental resin composites reinforced with milled E-glass fibers. Silicon 2018, 10, 1999–2007. [Google Scholar]
- Akcalı, A.; Gümüş, P.; Özcan, M. Clinical comparison of fiber-reinforced composite and stainless-steelwire for splinting periodontally treated mobile teeth. Braz. Dent. Sci. 2014, 17, 39–49. [Google Scholar] [CrossRef]
- Albashaireh, Z.S.; Ghazal, M.; Kern, M. Effects of endodontic post surface treatment, dentin conditioning, and artificial aging on the retention of glass fiber-reinforced composite resin posts. J. Prosthet. Dent. 2010, 103, 31–39. [Google Scholar] [CrossRef]
- Bijelic-Donova, J.; Garoush, S.; Lassila, L.V.J.; Keulemans, F.; Vallittu, P.K. Mechanical and structural characterization of discontinuous fiber-reinforced dental resin composite. J. Dent. 2016, 52, 70–78. [Google Scholar] [CrossRef]
- Vallittu, P.K. An overview of development and status of fiber-reinforced composites as dental and medical biomaterials. Acta Biomater. Odontol. Scand. 2018, 4, 44–55. [Google Scholar] [CrossRef] [PubMed]
- Reglero Ruiz, J.A.; Trigo-López, M.; García, F.C.; García, J.M. Functional aromatic polyamides. Polymers 2017, 9, 414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Konarzewski, V.H.C.; Spiekemann, F.L.; Santana, R.M.C. Natural ageing of polyaramide fiber from ballistic armor. Polímeros 2019, 29, 1–7. [Google Scholar] [CrossRef]
- Vasanthan, N. Polyamide fiber formation: Structure, properties and characterization. In Handbook of Textile Fibre Structure; Woodhead Publishing: Sawston, UK, 2009; pp. 232–256. [Google Scholar]
- Digholkar, S.; Madhav, V.N.V.; Palaskar, J. Evaluation of the flexural strength and microhardness of provisional crown and bridge materials fabricated by different methods. J. Indian Prosthodont. Soc. 2016, 16, 328–334. [Google Scholar]
- Pieniak, D.; Niewczas, A. Phenomenological evaluation of fatigue cracking of dental restorations under conditions of cyclic mechanical loads. Acta. Bioeng. Biomech. 2012, 14, 9–17. [Google Scholar]
- Hunicz, J.; Niewczas, A.; Kordos, P.; Pieniak, D. Experimental test stand for analysis of composite dental fillings degradation. Eksploat. Niezawodn. Maint. Reliab. 2007, 37, 37–43. [Google Scholar]
- Sarveshkumar, J.; Jayalakshmi, S. Bond failure and its prevention in composite restoration—A review. J. Pharm. Sci. Res. 2016, 8, 627–631. [Google Scholar]
- Ramalho, A.; Antunes, P.V. Reciprocating wear test of dental composites against human teeth and glass. Wear 2007, 263, 1095–1104. [Google Scholar] [CrossRef] [Green Version]
- Koc, D.; Dogan, A.; Bek, B. Bite force and influential factors on bite force measurement a literature review. Eur. J. Dent. 2010, 4, 223–232. [Google Scholar] [CrossRef] [Green Version]
- Chitmongkolsuk, S.; Heydecke, G.; Stappert, C.; Strub, J.R. Fracture strength of all-ceramic lithium disilicate and porcelain-fused-to-metal bridges for molar replacement after dynamic loading. Eur. J. Prosthodont. Restor. Dent. 2002, 10, 15–22. [Google Scholar]
- Pereira, L.J.; Gaviao, M.B.D.; Bonjardim, L.R.; Castelo, P.M.; Van der Bilt, A. Muscle thickness, bite force, and craniofacial dimensions in adolescents with signs and symptoms of temporomandibular dysfunction. Eur. J. Orthod. 2007, 29, 72–78. [Google Scholar] [CrossRef]
- Rosa, L.B.; Bataglion, C.; Siéssere, S.; Palinkas, M.; Mestriner, W., Jr.; De Freitas, O.; de Rossi, M.; de Oliveira, L.F.; Regalo, S.C. Bite force and masticatory efficiency in individuals with different oral rehabilitations. Open J. Stomatol. 2012, 2, 21–22. [Google Scholar] [CrossRef] [Green Version]
- Bakke, M. Bite force and occlusion. Semin. Orthod. 2006, 12, 120–126. [Google Scholar] [CrossRef]
- Eng, C.M.; Lieberman, D.E.; Zink, K.D.; Peters, M.A. Bite force and occlusal stress production in hominin evolution. Am. J. Phys. Anthr. 2013, 151, 544–557. [Google Scholar] [CrossRef] [PubMed]
- Aida, N.; Shinya, A.; Yokoyama, D.; Lassila, L.V.J.; Gomi, H.; Vallittu, P.K.; Shinya, A. Three-dimensional finite element analysis of posterior fiber-reinforced composite fixed partial denture Part 2: Influence of fiber reinforcement on mesial and distal connectors. Dent. Mater. J. 2011, 30, 29–37. [Google Scholar] [CrossRef]
- Kuroda, S.; Shinya, A.; Vallittu, P.K.; Nakasone, Y.; Shinya, A. Effect of water temperature on cyclic fatigue properties of glass-fiber-reinforced hybrid composite resin and its fracture pattern after flexural testing. J. Adhes. Dent. 2013, 15, 19–26. [Google Scholar]
- Papadogiannis, Y.; Lakes, R.S.; Palaghias, G.; Helvatjoglu-Antoniades, M.; Papadogiannis, D. Fatigue of packable dental composites. Dent. Mater. 2007, 23, 235–242. [Google Scholar] [CrossRef]
- Lohbauer, U.; Frankenberger, R.; Krämer, N.; Petschelt, A. Strength and fatigue performance versus filler fraction of different types of direct dental restoratives. J. Biomed. Mater. Res. B Appl. Biomater. 2006, 76, 114–120. [Google Scholar] [CrossRef]
- IBM Corp. Released, IBM SPSS Statistics for Windows, Version 20.0; IBM Corp.: Armonk, NY, USA, 2011. [Google Scholar]
- Yanagida, H.; Tanoue, N.; Minesaki, Y.; Kamasaki, Y.; Fujiwara, T.; Minami, H. Effects of polymerization method on flexural and shear bond strengths of a fiber-reinforced composite resin. J. Oral. Sci. 2017, 59, 13–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garoushi, S.; Shinya, A. Fiber-reinforced onlay composite resin restoration: A case report. J. Contemp. Dent. Pr. 2009, 10, 104–110. [Google Scholar] [CrossRef]
- Garoushi, S.; Yokoyama, D.; Shinya, A.; Vallittu, P.K. Fiber-reinforced composite resin prosthesis to restore missing posterior teeth: A case report. Libyan. J. Med. 2007, 2, 139–141. [Google Scholar] [CrossRef] [PubMed]
- Lohbauer, U.; Frankenberger, R.; Krämer, N.; Petschelt, A. Time-dependent strength and fatigue resistance of dental direct restorative materials. J. Mater. Sci. Mater. Med. 2003, 14, 1047–1053. [Google Scholar] [CrossRef] [PubMed]
- Selvaraj, A.; Nachimuthu, L.; Manickam, M. Effect of polyaramid reinforced sisal epoxy composites: Tensile, impact, flexural and morphological properties. J. Mater. Res. Technol. 2020, 9, 7947–7954. [Google Scholar]
- Röhrle, O.; Saini, H.; Ackland, D.C. Occlusal loading during biting from an experimental and simulation point of view. Dent. Mater. 2018, 34, 58–68. [Google Scholar] [CrossRef]
- Umesh, S.; Padma, S.; Asokan, S.; Srinivas, T. Fiber Bragg Grating based bite force measurement. J. Biomech. 2016, 49, 2877–2881. [Google Scholar] [CrossRef] [PubMed]


| Parameter | K | R1 | R2 |
|---|---|---|---|
| Maximum force [N] | 738.1 a ± 50.3 | 487.8 b ± 28.8 | 451.4 b ± 40.5 |
| Deflection at maximum force [mm] | 1.204 a ± 0.115 | 0.605 b ± 0.049 | 0.630 b ± 0.106 |
| Deflection at yielding point [mm] | 0.907 a ± 0.075 | 0.483 b ± 0.043 | 0.436 b ± 0.018 |
| Post-yield displacement [mm] | 1.210 a ± 0.112 | 0.568 b ± 0.040 | 0.614 ab ± 0.107 |
| No. of Cycles | Maximum Force | Deflection at Maximum Force | Deflection at Yielding Point | |
|---|---|---|---|---|
| Maximum force | −0.577 ** | |||
| Deflection at maximum force | −0.608 ** | 0.853 ** | ||
| Deflection at yielding point | −0.703 ** | 0.747 ** | 0.759 ** | |
| Post-yield displacement | −0.666 ** | 0.822 ** | 0.979 ** | 0.780 ** |
| Group | F (N) | |||
|---|---|---|---|---|
| 500 | 600 | 800 | 1000 | |
| K | 0.659 | 0.799 | 1.079 | 1.359 |
| R1 | 0.606 | 0.766 | 1.086 | 1.406 |
| R2 | 0.76 | 1.01 | 1.51 | 2.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szalewski, L.; Kamińska, A.; Wallner, E.; Batkowska, J.; Warda, T.; Wójcik, D.; Borowicz, J. Degradation of a Micro-Hybrid Dental Composite Reinforced with Polyaramide Fiber under the Influence of Cyclic Loads. Appl. Sci. 2020, 10, 7296. https://doi.org/10.3390/app10207296
Szalewski L, Kamińska A, Wallner E, Batkowska J, Warda T, Wójcik D, Borowicz J. Degradation of a Micro-Hybrid Dental Composite Reinforced with Polyaramide Fiber under the Influence of Cyclic Loads. Applied Sciences. 2020; 10(20):7296. https://doi.org/10.3390/app10207296
Chicago/Turabian StyleSzalewski, Leszek, Aneta Kamińska, Eliza Wallner, Justyna Batkowska, Tomasz Warda, Dorota Wójcik, and Janusz Borowicz. 2020. "Degradation of a Micro-Hybrid Dental Composite Reinforced with Polyaramide Fiber under the Influence of Cyclic Loads" Applied Sciences 10, no. 20: 7296. https://doi.org/10.3390/app10207296





