- Article
Reverse Vaccinology and Immune Simulation of a Novel Multiepitope Vaccine Targeting Brucella Virulence
- Mostafa F. Abushahba
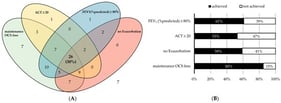
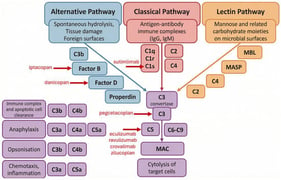
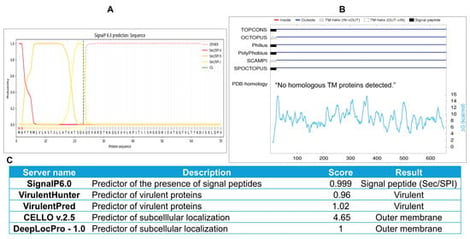
Background/Objectives: Brucella is a major global One Health threat, causing an estimated 2.1 million human infections and substantial livestock losses annually, with no vaccine currently available for humans, underscoring the urgent need for a safe and effective vaccine. Methods: Employing a reverse vaccinology approach, a novel 175-mer multiepitope vaccine (Mvax) targeting Brucella FrpB was computationally designed in this study, incorporating two B-cell, two MHC class I (MHC-I), and three MHC class II (MHC-II) epitopes selected for their high predicted antigenicity, safety, and IFN-γ-inducing potential. Human β-defensin-3 (hBD3) was fused to the N-terminus as an adjuvant, followed by comprehensive in silico evaluation of the construct. Results: Population coverage analysis predicted 99.59% global MHC class I/II coverage for selected epitopes. In silico analyses predicted that Mvax has high solubility (Protein-SOL score: 0.808), a high antigenicity score (VaxiJen: 1.06), and a negative GRAVY index (−0.881), indicating favorable predicted physicochemical characteristics. iMODS, CABS-Flex 3, and molecular dynamics simulations suggested theoretical stability trends for the modeled vaccine complexes. C-ImmSim immune simulations further predicted elevated Th1 cell populations and associated cytokines (IL-12, IFN-γ, IL-2) following both single and multiple simulated Mvax exposures. Conclusions: The computational analyses described here provide a theoretical modeling basis for an antivirulence multi-epitope vaccine design against human brucellosis, with predicted metrics and simulated immune responses requiring empirical validation.
3 February 2026



![Schematic representation of Classical and Trans-Signaling Interleukin-6 pathways. (A) Classical IL-6 signaling involves the binding of IL-6 to membrane-bound IL-6R, which promotes the assembly of a heterohexameric complex consisting of two molecules each of IL-6, IL-6R, and the signal-transducing subunit gp130. This complex triggers JAK/STAT3 pathway activation and drives the transcription of STAT3-dependent target genes. Beyond the JAK/STAT3 axis, the IL-6/IL-6R/gp130 complex can also stimulate the PI3K/AKT/mTOR and RAS/RAF/MEK/ERK pathways [6]. (B) In the IL-6 trans-signaling pathway, IL-6 interacts with the soluble form of IL-6R (sIL-6R), which is generated either through alternative splicing of IL-6R mRNA or by proteolytic cleavage of the membrane-bound receptor mediated by ADAM10 or ADAM17 [7]. The resulting IL-6/sIL-6R complex subsequently binds to gp130, inducing its dimerization and activating downstream signaling cascades analogous to those observed in classical IL-6 signaling.](https://mdpi-res.com/cdn-cgi/image/w=281,h=192/https://mdpi-res.com/biologics/biologics-06-00005/article_deploy/html/images/biologics-06-00005-ag-550.jpg)