Advances in Leukocyte Biology
A topical collection in Biomedicines (ISSN 2227-9059). This collection belongs to the section "Immunology and Immunotherapy".
Viewed by 34014Editors
Interests: neutrophils; leukotrienes; inflammation; apoptosis; oxidative stress
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
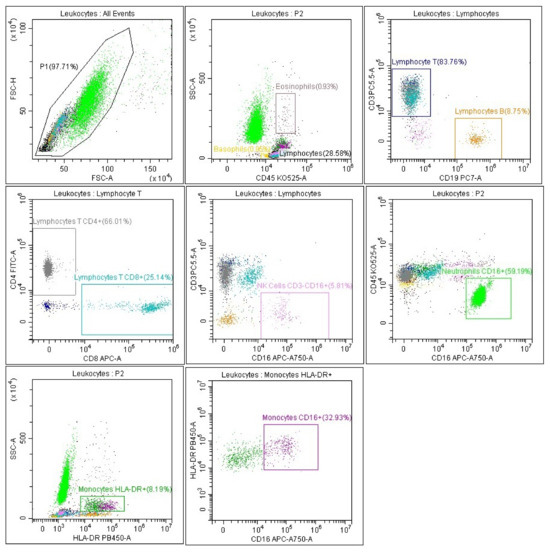
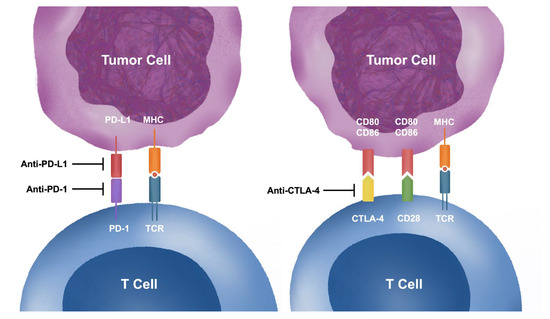
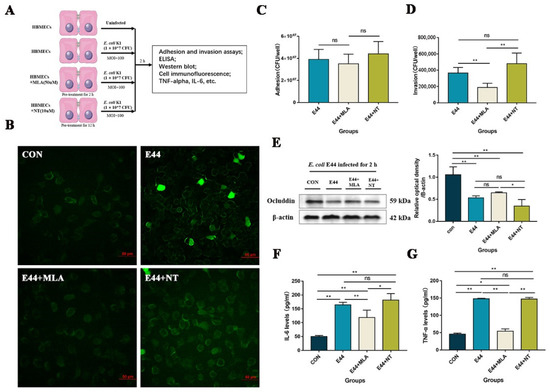
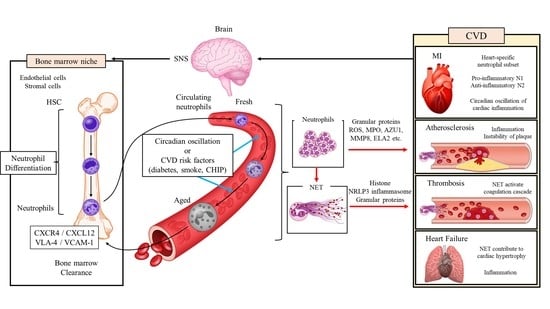
The immune system balances between homeostasis and inflammation, conditions associated with health and disease. For this, every organ and every cell of the body is adapted to perform one or more certain basic body functions. These regulatory mechanisms limit the entry of pathogens and limit immune reactivity against self and foreign antigens. White blood cells, also called leukocytes, are very important components of these orchestrated immune responses. Neutrophils are the largest subpopulation of human leukocytes (about 60% of human white blood cells), representing the innate immune system's first line of defense against a wide range of microorganisms. Neutrophils contribute to immunity by their unique antimicrobial ability, including phagocytosis and the secretion of hydrolytic enzymes, the formation of reactive oxygen and nitrogen species, and the release of antimicrobial proteins and peptides. In addition to phagocytosis, living neutrophils create a network of cytonemes to capture microorganisms, whereas dying neutrophils form neutrophil extracellular traps (NETs) equipped with bactericides from neutrophil granules adsorbed on DNA strands. Neutrophils, the main fraction of myeloid leukocytes is seen in the early stages of acute inflammation and play an important role in the innate immune response. Lymphocytes are presented by T and B cells, i.e., two major components of adaptive immunity and natural killer cells. Natural killer cells play central role in the antiviral response. B cells contribute to immunity by secreting antibodies and also promote the activation of T cells. T cells play a central role in adaptive immunity; these T cell responses are adapted to their respective cognate antigen and show a high degree of heterogeneity. T cells are essential for suppressing inflammatory immune responses. Our knowledge of the multifaceted functions of leukocytes in normal and pathological conditions is rapidly expanding. Recent biomedical research has shown that the neutrophil-to-lymphocyte ratio (NLR) is a useful prognostic marker in many diseases, including COVID-19. Addressing this and other key questions in leukocyte biology will provide a deeper understanding of the role of leukocytes in immunity, which will help develop effective therapeutic strategies.
Prof. Dr. Galina F. Sud’ina
Prof. Dr. Mihnea Zdrenghea
Collection Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Biomedicines is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2600 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- leukocyte
- immunity
- inflammation
- neutrophil
- eosinophil
- basophil
- monocyte
- B cell
- T cell
- natural killer cells
- lymphocyte