Commentaries from MedNews Week
A topical collection in Cancers (ISSN 2072-6694).
Viewed by 21678
Share This Topical Collection
Editor
 Dr. Jason Roszik
Dr. Jason Roszik
 Dr. Jason Roszik
Dr. Jason Roszik
E-Mail
Website
Guest Editor
Departments of Melanoma Medical Oncology and Genomic Medicine, Division of Cancer Medicine, The University of Texas MD Anderson Cancer Center, Houston, TX 77030, USA
Interests: computational cancer genomics; next generation sequencing; targeted therapy; immunotherapy; target discovery; drug repurposing; rare cancers
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
MedNews Week hosts biweekly conferences featuring internationally renowned experts working in precision oncology and immunotherapy. In addition, they host MedNews Week Around the World, which is a virtual roundtable discussing the latest advances made in medicine and described in research journals with special guests, including the authors and editors of the discussed article.
The aim of this Special Issue is to publish commentaries on the latest scientific papers and advancements made in precision oncology and immunotherapy presented and discussed in MedNews Week lectures. These Commentaries will be prepared by a team of medical professionals at MedNews Week, and reviewed by additional independent experts before publication in Cancers.
We heartily look forward to your receiving contributions, as well as feedback from our readers.
Dr. Jason Roszik
Guest Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Cancers is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript.
The Article Processing Charge (APC) for publication in this open access journal is 2900 CHF (Swiss Francs).
Submitted papers should be well formatted and use good English. Authors may use MDPI's
English editing service prior to publication or during author revisions.
Keywords
- cancer
- precision oncology
- personalized medicine
- immunotherapy
Published Papers (9 papers)
Open AccessCommentary
Advancing Pancreatic Cancer Surgical Treatments and Proposal of New Approaches
by
Viviana Cortiana, Harshitha Vallabhaneni, Jade Gambill, Soumiya Nadar, Kennedy Itodo, Chandler H. Park and Yan Leyfman
Viewed by 1667
Abstract
Pancreatic cancer is a significant challenge in oncology due to its aggressive nature and complex management, leading to high mortality rates and a dismally low 5-year survival rate. Approximately 85% of cases manifest as adenocarcinoma, while endocrine tumors constitute less than 5%. Borderline
[...] Read more.
Pancreatic cancer is a significant challenge in oncology due to its aggressive nature and complex management, leading to high mortality rates and a dismally low 5-year survival rate. Approximately 85% of cases manifest as adenocarcinoma, while endocrine tumors constitute less than 5%. Borderline resectable and locally advanced pancreatic cancers are particularly difficult to treat due to vascular involvement, which complicates complete resections and increases morbidity. Various therapeutic modalities aim to overcome these challenges and improve patient outcomes. Traditionally, upfront surgery was the standard for resectable tumors, with multimodal chemotherapy being central to treatment. Understanding surgical anatomy is pivotal in enhancing surgical outcomes and patient survival. Resectability challenges are several when seeking to achieve R0 resections, particularly for borderline resectable tumors. Various classification systems—the MD Anderson criteria, the NCCN criteria, the AHPA/SSAT/SSO consensus statement, and the Alliance definition—assess tumor involvement with major blood vessels, with the first of these systems being broadly accepted. Vascular staging integration is also important, with the Ishikawa staging system using preoperative imaging to assess venous involvement. Furthermore, neoadjuvant therapy enhances treatment effectiveness by addressing micro-metastatic disease early, increasing R0 resection chances, and downstaging tumors for optimal surgery. Insights from the Fox Chase Cancer Center’s neoadjuvant treatment approach highlight the importance of a multidisciplinary strategy when advancing therapy and improving patient prognosis. This commentary, inspired by Dr. Sanjay S. Reddy’s Keynote Conference during MedNews week, highlights current advancements and ongoing challenges in the treatment of pancreatic cancer, emphasizing the need for a comprehensive, multidisciplinary approach to improve outcomes.
Full article
►▼
Show Figures
Open AccessReview
Personalized Medicine in Pancreatic Cancer: The Promise of Biomarkers and Molecular Targeting with Dr. Michael J. Pishvaian
by
Viviana Cortiana, Rabab Hunaid Abbas, Harshal Chorya, Jade Gambill, Diksha Mahendru, Chandler H. Park and Yan Leyfman
Cited by 7 | Viewed by 3204
Abstract
Pancreatic cancer, with its alarming rising incidence, is predicted to become the second deadliest type of solid tumor by 2040, highlighting the urgent need for improved diagnostic and treatment strategies. Despite medical advancements, the five-year survival rate for pancreatic cancer remains about 14%,
[...] Read more.
Pancreatic cancer, with its alarming rising incidence, is predicted to become the second deadliest type of solid tumor by 2040, highlighting the urgent need for improved diagnostic and treatment strategies. Despite medical advancements, the five-year survival rate for pancreatic cancer remains about 14%, dropping further when metastasized. This review explores the promise of biomarkers for early detection, personalized treatment, and disease monitoring. Molecular classification of pancreatic cancer into subtypes based on genetic mutations, gene expression, and protein markers guides treatment decisions, potentially improving outcomes. A plethora of clinical trials investigating different strategies are currently ongoing. Targeted therapies, among which those against CLAUDIN 18.2 and inhibitors of Claudin 18.1, have shown promise. Next-generation sequencing (NGS) has emerged as a powerful tool for the comprehensive genomic analysis of pancreatic tumors, revealing unique genetic alterations that drive cancer progression. This allows oncologists to tailor therapies to target specific molecular abnormalities. However, challenges remain, including limited awareness and uptake of biomarker-guided therapies. Continued research into the molecular mechanisms of pancreatic cancer is essential for developing more effective treatments and improving patient survival rates.
Full article
►▼
Show Figures
Open AccessCommentary
Reimagining Colorectal Cancer Screening: Innovations and Challenges with Dr. Aasma Shaukat
by
Viviana Cortiana, Muskan Joshi, Harshal Chorya, Harshitha Vallabhaneni, Shreevikaa Kannan, Helena S. Coloma, Chandler H. Park and Yan Leyfman
Viewed by 1771
Abstract
Colorectal cancer (CRC) currently ranks as the third most common cancer and the second leading cause of cancer-related deaths worldwide, posing a significant global health burden to the population. Recent studies have reported the emergence of a new clinical picture of the disease,
[...] Read more.
Colorectal cancer (CRC) currently ranks as the third most common cancer and the second leading cause of cancer-related deaths worldwide, posing a significant global health burden to the population. Recent studies have reported the emergence of a new clinical picture of the disease, with a notable increase in CRC rates in younger populations of <50 years of age. The American Cancer Society (ACS) now recommends CRC screening starting at age 45 for average-risk individuals. Dr. Aasma Shaukat’s Keynote Conference highlights the critical need for updated screening strategies, with an emphasis on addressing the suboptimal adherence rates and the effective management of the growing burden of CRC. Lowering the adenoma detection screening age can facilitate early identification of adenomas in younger asymptomatic patients, altering the epidemiologic landscape. However, its implications may not be as profound unless a drastic shift in the age distribution of CRC is observed. Currently, various screening options are available in practice, including stool-based tests like multitarget stool DNA (mtDNA) tests, fecal immunochemical testing (FIT), and imaging-based tests. In addition to existing screening methods, blood-based tests are now emerging as promising tools for early CRC detection. These tests leverage innovative techniques along with AI and machine learning algorithms, aiding in tumor detection at a significantly earlier stage, which was not possible before. Medicare mandates specific criteria for national coverage of blood-based tests, including sensitivity ≥ 74%, specificity ≥ 90%, FDA approval, and inclusion in professional society guidelines. Ongoing clinical trials, such as Freenome, Guardant, and CancerSEEK, offer hope for further advancements in blood-based CRC screening. The development of multicancer early detection tests like GRAIL demonstrates a tremendous potential for detecting various solid tumors and hematologic malignancies. Despite these breakthroughs, the question of accessibility and affordability still stands. The ever-evolving landscape of CRC screening reflects the strength of the scientific field in light of an altered disease epidemiology. Lowering screening age along with the integration of blood-based tests with existing screening methods holds great potential in reducing the CRC-related burden. At the same time, it is increasingly important to address the challenges of adaptation of the healthcare system to this change in the epidemiologic paradigm.
Full article
►▼
Show Figures
Open AccessCommentary
PSMA-Targeted Therapy: Advancements in Detection and Treatment Modalities with Dr. Scott T. Tagawa
by
Viviana Cortiana, Jade Gambill, Harshal Chorya, Diksha Mahendru, Fabiha Amin, Chandler H. Park and Yan Leyfman
Cited by 1 | Viewed by 2171
Abstract
Prostate cancer is one of the most challenging malignancies due to its high incidence and prevalence, as it is the most frequently diagnosed non-skin cancer in men. The timely identification of prostate cancer and its metastasis is paramount for ensuring favorable outcomes for
[...] Read more.
Prostate cancer is one of the most challenging malignancies due to its high incidence and prevalence, as it is the most frequently diagnosed non-skin cancer in men. The timely identification of prostate cancer and its metastasis is paramount for ensuring favorable outcomes for patients. Prostate-specific membrane antigen (PSMA) emerges as a promising biomarker for its detection, due to its specificity. This makes it an ideal target for the early identification of a metastatic phenotype. Situated on the membrane of tumor cells, PSMA facilitates the attachment of PSMA-targeting particles, enabling their detection through positron emission tomography (PET) scans with relative ease. Utilizing these imaging agents in conjunction with PET scans enhances the accuracy of prostate cancer tumor detection compared to PET scans alone. The advancement in prostate cancer imaging has paved the way for innovative treatment modalities. Prostate-specific membrane antigen-targeted radionuclide therapies (PSMA-TRT) exploit PSMA imaging agents to target identified prostate cancer malignancies with precise radiation, thereby reducing or eliminating the tumor mass. PSMA-TRT exhibits significant promise in prostate cancer therapy, evident from the notable declines in prostate-specific antigen (PSA) levels post treatment. However, PSMA-TRT carries both beneficial and adverse effects. While it represents a substantial leap forward in tumor cell imaging, PSMA-based antigens, being larger particles than ligands, offer prolonged imaging capabilities. Yet, the long-term effects of PSMA-TRT remain unknown, with the short-term adverse ones including fatigue, nausea, pain flares, and potential radiation exposure to others.
Full article
►▼
Show Figures
Open AccessReview
Reviewing the Landscape of Cancer Survivorship: Insights from Dr. Lidia Schapira’s Programs and Beyond
by
Viviana Cortiana, Rabab Hunaid Abbas, Soumiya Nadar, Diksha Mahendru, Jade Gambill, Gayathri Pramil Menon, Chandler H. Park and Yan Leyfman
Cited by 3 | Viewed by 2986
Abstract
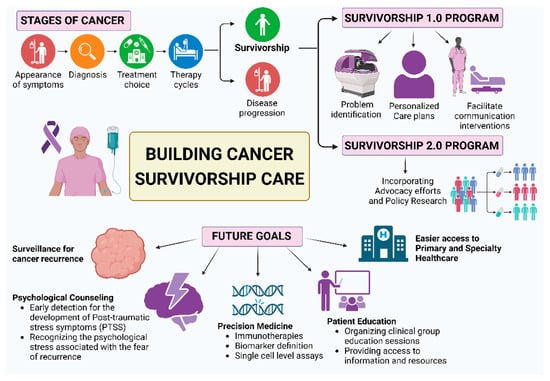
The constantly escalating population of cancer survivors worldwide has prompted a focused exploration of their unique needs and experiences within the context of healthcare medicine. This review initiates its analysis inspired by Dr. Lidia Schapira’s insightful keynote conference on the Survivorship 1.0 and
[...] Read more.
The constantly escalating population of cancer survivors worldwide has prompted a focused exploration of their unique needs and experiences within the context of healthcare medicine. This review initiates its analysis inspired by Dr. Lidia Schapira’s insightful keynote conference on the Survivorship 1.0 and Survivorship 2.0 Programs, shedding light on their implementation challenges and setting the stage for a comprehensive analysis of cancer survivorship initiatives. Within the transformed landscape of cancer care, patient-centric strategies embedded in cancer survivorship programs comprising vital elements such as connection, support, and education are presented. While placing cancer recurrence surveillance at the forefront, the review underlines concern regarding the potential oversight of the enduring impact on mental and physical health. Dr. Schapira’s insights further extend into the exploration of mental health challenges faced by survivors, promoting an examination of diverse strategies to address these concerns. Furthermore, the discussion continues toward promising areas of research, notably Precision Medicine’s role in de-escalating cancer therapies, and advocates for measures such as early cancer awareness and timely referrals to supportive services. Highlighting the significance of education, the role of online resources in enhancing the knowledge of healthcare practitioners and future generations in cancer care is then explored. The paper concludes by presenting some of the most prominent global current survivorship programs, identifying critical knowledge gaps in cancer care and projecting future developments aimed at delivering accurate and holistic care, improving the quality of life for survivors, and enhancing both mental and physical well-being. Drawing upon the insights from Dr. Schapira, this review lays the groundwork for a nuanced exploration of cancer survivorship and its multifaceted implications.
Full article
►▼
Show Figures
Open AccessCommentary
Innovations in Thoracic Oncology and the Promise of Liquid Biopsies with Dr. Luis Raez
by
Viviana Cortiana, Alexandra Van de Kieft, Harshal Chorya, Jade Gambill, Chandler H. Park and Yan Leyfman
Viewed by 1608
Abstract
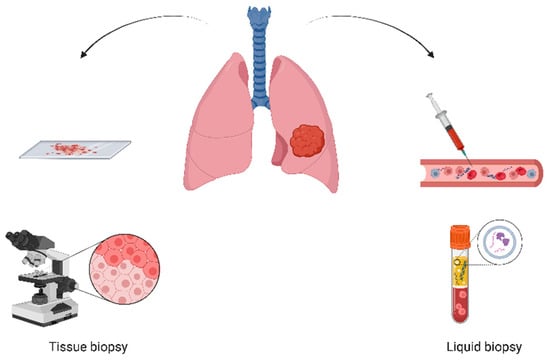
Thoracic oncology continues to pose a great threat to human health as one of the most common forms of cancer. Liquid biopsies present a transformative approach to treating patients affected by these types of diseases by providing a less invasive genetic overview of
[...] Read more.
Thoracic oncology continues to pose a great threat to human health as one of the most common forms of cancer. Liquid biopsies present a transformative approach to treating patients affected by these types of diseases by providing a less invasive genetic overview of the tumor, aiding in both diagnostic and treatment measures. The primary objective of this article is to examine the prospects of liquid biopsies in managing thoracic malignancies and to present barriers to their usage as demonstrated by Dr. Luis Raez. In examining why molecular diagnostics continue to be employed together with more traditional methods, this article presents the next steps in the clinical application of blood-based cancer screening. Future cancer diagnosis and treatment aim to prioritize circulating biomarker analyses based on their potential for the detection and monitoring of thoracic cancers. Liquid biopsies are favored thanks to their reduced invasiveness with respect to traditional treatments. The further study of clinical biomarkers and technological advancements are thus pivotal to enhance the clinical applicability of this method. In conclusion, this blood-based analysis offers a promising route by which the diagnosis, treatments, and outcomes of thoracic cancer can be improved.
Full article
►▼
Show Figures
Open AccessCommentary
Cholangiocarcinoma Insights: Established Foundations and Cutting-Edge Innovations from Dr. James Cleary’s Pioneering Research
by
Viviana Cortiana, Harshal Chorya, Muskan Joshi, Shreevikaa Kannan, Diksha Mahendru, Harshitha Vallabhaneni, Helena S. Coloma, Yan Leyfman and Chandler H. Park
Cited by 1 | Viewed by 2571
Abstract
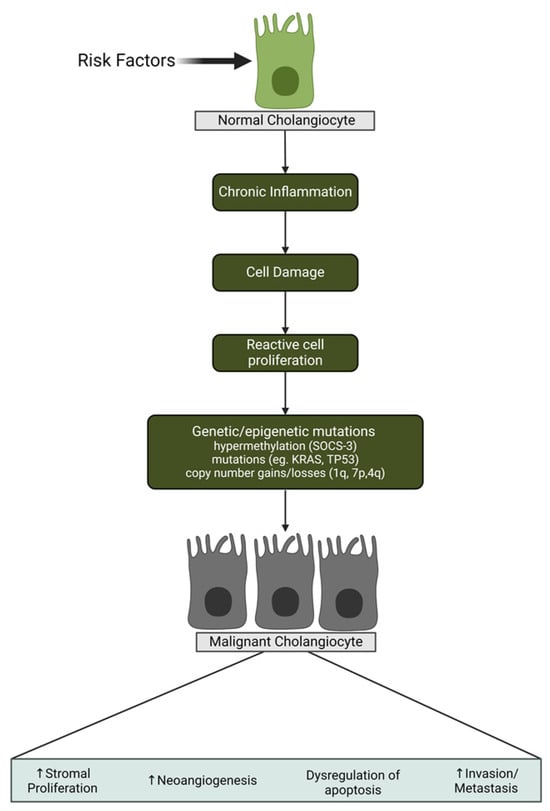
This paper provides insights into the conventional understanding of biliary tract malignancies, with a specific focus on cholangiocarcinoma (CCA). We then delve into the groundbreaking ideas presented by Dr. James Cleary. CCA, originating from biliary tree cells, manifests diverse subtypes contingent upon anatomical
[...] Read more.
This paper provides insights into the conventional understanding of biliary tract malignancies, with a specific focus on cholangiocarcinoma (CCA). We then delve into the groundbreaking ideas presented by Dr. James Cleary. CCA, originating from biliary tree cells, manifests diverse subtypes contingent upon anatomical localization and differentiation status. These variants exhibit discrete genetic aberrations, yielding disparate clinical phenotypes and therapeutic modalities. Intrahepatic, perihilar, and distal CCAs intricately involve distinct segments of the biliary tree, further categorized as well-differentiated, moderately differentiated, or poorly differentiated adenocarcinomas based on their histological differentiation. Understanding the etiological factors contributing to CCA development assumes paramount importance. Stratifying these factors into two groups, those unrelated to fluke infestations (e.g., viral hepatitis and fatty liver conditions) and those associated with fluke infestations (e.g., chronic liver inflammation), facilitates predictive modeling. The epidemiology of CCA exhibits global variability, with Southeast Asia notably displaying higher incidences attributed primarily to liver fluke infestations. Jaundice resulting from bile duct obstruction constitutes a prevalent clinical manifestation of CCA, alongside symptoms like malaise, weight loss, and abdominal pain. Diagnostic challenges arise due to the symptomatic overlap with other biliary disorders. Employing comprehensive liver function tests and imaging modalities such as computed tomography assumes a pivotal role in ensuring accurate diagnosis and staging. However, the definitive confirmation of CCA necessitates a biopsy. Treatment modalities, predominantly encompassing surgical resection and radiation therapy, hold curative potential, although a considerable subset of patients is deemed unresectable upon exploration. Challenges intensify, particularly in cases classified as cancer of unknown origin, underscoring the imperative for early intervention. Advancements in genomic sequencing have revolutionized precision medicine in CCA. Distinct genomic markers, including fibroblast growth factor receptor 2 (FGFR2) alterations and isocitrate dehydrogenase 1 (IDH1) mutations, have emerged as promising therapeutic targets. FGFR2 alterations, encompassing mutations and rearrangements, play pivotal roles in oncogenesis, with FGFR inhibitors demonstrating promise despite identified resistance mechanisms. Similarly, IDH1 inhibitors face challenges with resistance, despite encouraging early clinical trial results, prompting exploration of novel irreversible inhibitors. Dr. James Cleary’s illuminating discourse underscores the significance of diverse FGFR2 alterations and the potential of IDH1 inhibition in reshaping the treatment landscape for CCA. These findings unveil critical avenues for targeted therapeutic interventions, emphasizing the critical need for ongoing research to optimize outcomes in this challenging cancer subtype, incorporating innovative insights from Dr. Cleary.
Full article
►▼
Show Figures
Open AccessCommentary
The Potential of Lifestyle Medicine: Strategies to Optimize Health and Well-Being in Oncology Care with Dr. Amy Comander
by
Harshal Chorya, Helena S. Coloma, Viviana Cortiana, Muskan Joshi, Gayathri P. Menon, Maduri Balasubramanian, Chandler H. Park and Yan Leyfman
Viewed by 2005
Abstract
The field of lifestyle medicine in cancer care and survivorship is undergoing significant transformation, presenting both challenges and opportunities. This collection of insights and reflections by an esteemed speaker aims to address critical facets of this evolving landscape and the intersection of healthcare,
[...] Read more.
The field of lifestyle medicine in cancer care and survivorship is undergoing significant transformation, presenting both challenges and opportunities. This collection of insights and reflections by an esteemed speaker aims to address critical facets of this evolving landscape and the intersection of healthcare, lifestyle, and cancer. With a focus on optimizing the health of cancer survivors, the speaker emphasizes the correlation between general population health and strategies for mitigating cancer risk. Evidence-based resources have a key role in their comprehensive insights into lifestyle changes’ role in cancer prevention and survivorship. Lifestyle interventions also have a promising role in mitigating the late effects in the pediatric context. Therefore, encouraging the early adoption of healthy practices in childhood cancer survivors emerges as a pivotal strategy. Furthermore, challenges in enhancing education and access to lifestyle medicine are addressed. This highlights the importance of patient-centered communication, motivational interviewing, and personalized guidance in facilitating lifestyle changes with patients. Finally, the role of nutritionists in advising breast cancer patients to consider calorie restriction to lower IGF-1 levels is explored. This collection underscores the multifaceted nature of lifestyle medicine in cancer care, highlighting challenges, opportunities, and the transformative power of passion and curiosity in shaping healthcare careers.
Full article
Open AccessCommentary
The Evolving Landscape: Exploring the Future of Myelodysplastic Syndrome Treatment with Dr. Rami Komrokji
by
Sean Henry Jackewicz, Helena S. Coloma, Viviana Cortiana, Muskan Joshi, Gayathri P. Menon, Maduri Balasubramanian, Chandler H. Park and Yan Leyfman
Cited by 1 | Viewed by 1776
Abstract
This perspective delves into the evolving landscape of Myelodysplastic Syndrome (MDS) treatment. MDS presents a significant clinical challenge, often progressing to acute myeloid leukemia. For low-risk MDS, the emphasis is on personalized care through comprehensive risk assessment, clinical monitoring, and tailored interventions, including
[...] Read more.
This perspective delves into the evolving landscape of Myelodysplastic Syndrome (MDS) treatment. MDS presents a significant clinical challenge, often progressing to acute myeloid leukemia. For low-risk MDS, the emphasis is on personalized care through comprehensive risk assessment, clinical monitoring, and tailored interventions, including promising agents like erythropoiesis-stimulating agents, lenalidomide, and luspatercept, with the anticipation of an expanding therapeutic arsenal and early intervention for improved outcomes. In contrast, high-risk MDS treatment is evolving towards upfront doublet or triplet therapies with a focus on minimal residual disease (MRD) monitoring. A holistic approach integrates various modalities, including stem cell transplant and post-transplant maintenance, all guided by individual patient circumstances. Risk-adapted strategies are crucial for enhancing patient outcomes. Precision medicine for MDS treatment is budding, largely driven by Next Generation Sequencing (NGS). NGS aids in early diagnosis, prognostication, and the targeting of specific mutations, with molecular data increasingly informing treatment responses and allowing for tailored interventions. Clinical trials within homogeneous patient groups with similar molecular profiles are becoming more common, enhancing treatment precision. In conclusion, the future of MDS treatment is moving towards personalized medicine, leveraging advanced technologies like NGS and molecular insights to improve outcomes in the realm of hematological malignancies.
Full article