Faster Time to Treatment Decision of Viscoelastic Coagulation Test Results through Improved Perception with the Animated Visual Clot: A Multicenter Comparative Eye-Tracking Study
Abstract
:1. Introduction
2. Materials and Methods
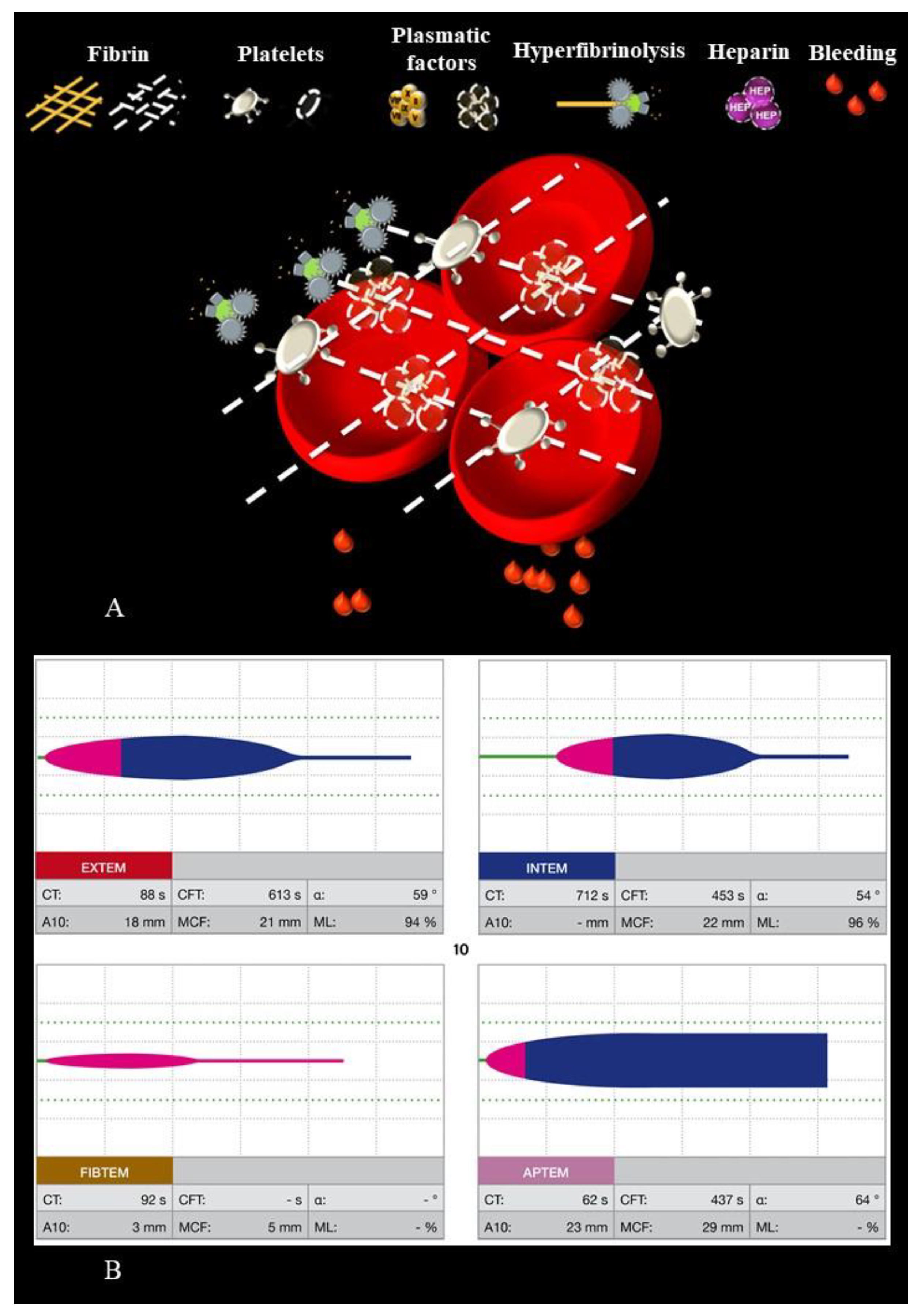
2.1. Description of the Visual Clot Technology
2.2. Study Design
2.3. Outcomes and Statistical Analyses
3. Results
3.1. Study and Participant Characteristics
3.2. Time to Treatment Decision
3.3. Time on Screen Surface
4. Discussion
4.1. Principal Findings
4.2. Future Perspectives
4.3. Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CI | Confidence interval |
| HR | Hazard Ratio |
| ROTEM | Rotational Thrombelastometry |
References
- Spahn, D.R.; Bouillon, B.; Cerny, V.; Duranteau, J.; Filipescu, D.; Hunt, B.J.; Komadina, R.; Maegele, M.; Nardi, G.; Riddez, L.; et al. The European guideline on management of major bleeding and coagulopathy following trauma: Fifth edition. Crit. Care 2019, 23, 98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wikkelsø, A.; Wetterslev, J.; Møller, A.M.; Afshari, A. Thromboelastography (TEG) or thromboelastometry (ROTEM) to monitor haemostatic treatment versus usual care in adults or children with bleeding. Cochrane Database Syst. Rev. 2016, 2016, Cd007871. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hartert, H. Blutgerinnungsstudien mit der Thrombelastographie, einem neuen Untersuchungsverfahren. Klin. Wochenschr. 1948, 26, 577–583. [Google Scholar] [CrossRef]
- Davenport, R.; Manson, J.; De’Ath, H.; Platton, S.; Coates, A.; Allard, S.; Hart, D.; Pearse, R.; Pasi, K.J.; MacCallum, P.; et al. Functional definition and characterization of acute traumatic coagulopathy. Crit. Care Med. 2011, 39, 2652–2658. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Serraino, G.F.; Murphy, G.J. Routine use of viscoelastic blood tests for diagnosis and treatment of coagulopathic bleeding in cardiac surgery: Updated systematic review and meta-analysis. BJA Br. J. Anaesth. 2017, 118, 823–833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stein, P.; Kaserer, A.; Spahn, G.H.; Spahn, D.R. Point-of-Care Coagulation Monitoring in Trauma Patients. Semin. Thromb. Hemost. 2017, 43, 367–374. [Google Scholar] [CrossRef]
- McNamara, H.; Kenyon, C.; Smith, R.; Mallaiah, S.; Barclay, P. Four years’ experience of a ROTEM(®) -guided algorithm for treatment of coagulopathy in obstetric haemorrhage. Anaesthesia 2019, 74, 984–991. [Google Scholar] [CrossRef]
- Hawkins, R.B.; Raymond, S.L.; Hartjes, T.; Efron, P.A.; Larson, S.D.; Andreoni, K.A.; Thomas, E.M. Review: The Perioperative Use of Thromboelastography for Liver Transplant Patients. Transplant. Proc. 2018, 50, 3552–3558. [Google Scholar] [CrossRef]
- Gregory, J.A.; Huitron, S.S.; George, A.A.; Simon, C.D. Optimizing Transfusion Ratios in Massive Transfusion Protocols: An Argument Against the 1:1:1 Dogma and Approach to Trauma Resuscitation. Lab. Med. 2015, 46, e46–e52. [Google Scholar] [CrossRef]
- Whiting, P.; Al, M.; Westwood, M.; Ramos, I.C.; Ryder, S.; Armstrong, N.; Misso, K.; Ross, J.; Severens, J.; Kleijnen, J. Viscoelastic point-of-care testing to assist with the diagnosis, management and monitoring of haemostasis: A systematic review and cost-effectiveness analysis. Health Technol. Assess. 2015, 19, 1–228. [Google Scholar] [CrossRef] [Green Version]
- Srivastava, A.; Kelleher, A. Point-of-care coagulation testing. Contin. Educ. Anaesth. Crit. Care Pain 2012, 13, 12–16. [Google Scholar] [CrossRef] [Green Version]
- Rössler, J.; Meybohm, P.; Spahn, D.R.; Zacharowski, K.; Braun, J.; Nöthiger, C.B.; Tscholl, D.W. Improving decision making through presentation of viscoelastic tests as a 3D animated blood clot: The Visual Clot. Anaesthesia 2020, 75, 1059–1069. [Google Scholar] [CrossRef] [PubMed]
- Endsley, M.R. Designing for Situation Awareness: An Approach to User-Centered Design, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2012; p. 396. [Google Scholar]
- Said, S.; Roche, T.R.; Braun, J.; Ganter, M.T.; Meybohm, P.; Herrmann, J.; Zacharowski, K.; Raimann, F.J.; Piekarski, F.; Rivas, E.; et al. Effects of an Animated Blood Clot Technology (Visual Clot) on the Decision-Making of Users Inexperienced in Viscoelastic Testing: Multicenter Trial. J. Med. Internet Res. 2021, 23, e27124. [Google Scholar] [CrossRef]
- Roche, T.R.; Said, S.; Rössler, J.; Gozdzik, M.; Meybohm, P.; Zacharowski, K.; Spahn, D.R.; Nöthiger, C.B.; Tscholl, D.W. Physicians’ Perceptions of a Situation Awareness-Oriented Visualization Technology for Viscoelastic Blood Coagulation Management (Visual Clot): Mixed Methods Study. JMIR Serious Games 2020, 8, e19036. [Google Scholar] [CrossRef] [PubMed]
- Just, M.A.; Carpenter, P.A. A theory of reading: From eye fixations to comprehension. Psychol. Rev. 1980, 87, 329–354. [Google Scholar] [CrossRef] [PubMed]
- Rayner, K.; Pollatsek, A. Eye movements and scene perception. Can. J. Psychol. 1992, 46, 342–376. [Google Scholar] [CrossRef] [PubMed]
- Harezlak, K.; Kasprowski, P. Application of eye tracking in medicine: A survey, research issues and challenges. Comput. Med. Imaging Graph. 2018, 65, 176–190. [Google Scholar] [CrossRef]
- Holmqvist, K.; Andersson, R. Eye-Tracking: A Comprehensive Guide to Methods, Paradigms and Measures; Oxford University: Oxford, UK, 2017. [Google Scholar]
- Endsley, M.R. Measurement of Situation Awareness in Dynamic Systems. Hum. Factors 1995, 37, 65–84. [Google Scholar] [CrossRef]
- De Winter, J.C.F.; Eisma, Y.B.; Cabrall, C.D.D.; Hancock, P.A.; Stanton, N.A. Situation awareness based on eye movements in relation to the task environment. Cogn. Technol. Work. 2019, 21, 99–111. [Google Scholar] [CrossRef] [Green Version]
- Stein, P.; Kaserer, A.; Sprengel, K.; Wanner, G.A.; Seifert, B.; Theusinger, O.M.; Spahn, D.R. Change of transfusion and treatment paradigm in major trauma patients. Anaesthesia 2017, 72, 1317–1326. [Google Scholar] [CrossRef] [Green Version]
- Tscholl, D.W.; Weiss, M.; Spahn, D.R.; Noethiger, C.B. How to Conduct Multimethod Field Studies in the Operating Room: The iPad Combined With a Survey App as a Valid and Reliable Data Collection Tool. JMIR Res. Protoc. 2016, 5, e4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meneses, E.; Boneva, D.; McKenney, M.; Elkbuli, A. Massive transfusion protocol in adult trauma population. Am. J. Emerg. Med. 2020, 38, 2661–2666. [Google Scholar] [CrossRef] [PubMed]
- Grier, R.A.; Warm, J.S.; Dember, W.N.; Matthews, G.; Galinsky, T.L.; Parasuraman, R. The vigilance decrement reflects limitations in effortful attention, not mindlessness. Hum. Factors 2003, 45, 349–359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tscholl, D.W.; Handschin, L.; Neubauer, P.; Weiss, M.; Seifert, B.; Spahn, D.R.; Noethiger, C.B. Using an animated patient avatar to improve perception of vital sign information by anaesthesia professionals. Br. J. Anaesth. 2018, 121, 662–671. [Google Scholar] [CrossRef] [Green Version]
- Tscholl, D.W.; Weiss, M.; Handschin, L.; Spahn, D.R.; Nöthiger, C.B. User perceptions of avatar-based patient monitoring: A mixed qualitative and quantitative study. BMC Anesthesiol. 2018, 18, 188. [Google Scholar] [CrossRef]
- Tscholl, D.W.; Rössler, J.; Handschin, L.; Seifert, B.; Spahn, D.R.; Nöthiger, C.B. The Mechanisms Responsible for Improved Information Transfer in Avatar-Based Patient Monitoring: Multicenter Comparative Eye-Tracking Study. J. Med. Internet Res. 2020, 22, e15070. [Google Scholar] [CrossRef]
- Ljubenovic, A.; Said, S.; Braun, J.; Grande, B.; Kolbe, M.; Spahn, D.R.; Nöthiger, C.B.; Tscholl, D.W.; Roche, T.R. Anesthesia providers’ visual attention in simulated anesthesia emergencies using conventional number-based and avatar-based patient monitoring: A prospective, eye-tracking study. JMIR Serious Games 2022, 10, e35642. [Google Scholar] [CrossRef]
- Engelken, E.J.; Stevens, K.W.; McQueen, W.J.; Enderle, J.D. Eye tracking performance variability in a homogeneous population. Biomed. Sci. Instrum. 1995, 31, 229–233. [Google Scholar]



| Characteristic | Number |
|---|---|
| Participants, n (%) | 35 (100) |
| University Hospital Zurich | 7 (20) |
| Cantonal Hospital Winterthur | 7 (20) |
| University Hospital Frankfurt | 7 (20) |
| University Hospital Wuerzburg | 7 (20) |
| Hospital Clinic de Barcelona | 7 (20 |
| Participants with successful eye-tracking recording, n (%) | 22 (63) |
| University Hospital Zurich | 6 (17) |
| Cantonal Hospital Winterthur | 5 (14) |
| University Hospital Frankfurt | 7 (20) |
| University Hospital Wuerzburg | 4 (11) |
| Hospital Clinic de Barcelona | 0 (0) |
| Gender, n (%) | 35 (100) |
| Female | 17 (49) |
| Male | 18 (51) |
| Age (years), median (IQR, range) | 28 (25–32, 24–36) |
| Job Experience, n (%) | 35 (100) |
| Fifth-year medical student | 3 (8) |
| Sixth-year medical student | 10 (29) |
| First-year resident | 19 (54) |
| Second-year resident | 2 (6) |
| Third-year resident | 1 (3) |
| Previously used ROTEM, n (%) | 35 (100) |
| Yes | 9 (26) |
| No | 26 (74) |
| Previously used Visual Clot, n (%) | 35 (100) |
| Yes | 1 (3) |
| No | 34 (97) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castellucci, C.; Braun, J.; Said, S.; Roche, T.R.; Nöthiger, C.B.; Spahn, D.R.; Tscholl, D.W.; Akbas, S. Faster Time to Treatment Decision of Viscoelastic Coagulation Test Results through Improved Perception with the Animated Visual Clot: A Multicenter Comparative Eye-Tracking Study. Diagnostics 2022, 12, 1269. https://doi.org/10.3390/diagnostics12051269
Castellucci C, Braun J, Said S, Roche TR, Nöthiger CB, Spahn DR, Tscholl DW, Akbas S. Faster Time to Treatment Decision of Viscoelastic Coagulation Test Results through Improved Perception with the Animated Visual Clot: A Multicenter Comparative Eye-Tracking Study. Diagnostics. 2022; 12(5):1269. https://doi.org/10.3390/diagnostics12051269
Chicago/Turabian StyleCastellucci, Clara, Julia Braun, Sadiq Said, Tadzio Raoul Roche, Christoph B. Nöthiger, Donat R. Spahn, David W. Tscholl, and Samira Akbas. 2022. "Faster Time to Treatment Decision of Viscoelastic Coagulation Test Results through Improved Perception with the Animated Visual Clot: A Multicenter Comparative Eye-Tracking Study" Diagnostics 12, no. 5: 1269. https://doi.org/10.3390/diagnostics12051269
APA StyleCastellucci, C., Braun, J., Said, S., Roche, T. R., Nöthiger, C. B., Spahn, D. R., Tscholl, D. W., & Akbas, S. (2022). Faster Time to Treatment Decision of Viscoelastic Coagulation Test Results through Improved Perception with the Animated Visual Clot: A Multicenter Comparative Eye-Tracking Study. Diagnostics, 12(5), 1269. https://doi.org/10.3390/diagnostics12051269








