Primary Esophageal Motility Disorders: Beyond Achalasia
Abstract
:1. Introduction
2. HRM Parameters
2.1. Contractile Vigor—Distal Contractile Integral
2.2. Peristalsis—Distal Latency
2.3. Lower Esophageal Sphincter Pressure
3. Esophageal Motility Disorders beyond Achalasia
Esophagogastric Junction Outflow Obstruction
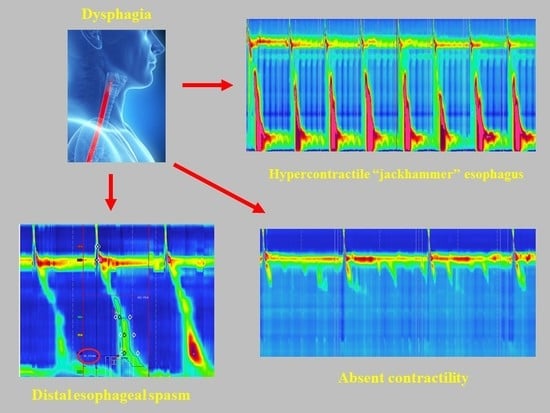
4. Major Disorders of Peristalsis
4.1. Distal Esophageal Spasm
4.2. Hypercontractile Esophagus
4.3. Absent Contractility
5. Minor Disorders of Peristalsis
5.1. Ineffective Esophageal Motility
5.2. Fragmented Peristalsis
6. Management of Motility Disorders beyond Achalasia
Esophagogastric Junction Outflow Obstruction
7. Major Disorders of Peristalsis
8. Minor Disorders of Peristalsis
9. Conclusions
Author Contributions
Conflicts of Interest
References
- Schlottmann, F.; Shaheen, N.J.; Madanick, R.D.; Patti, M.G. The role of Heller myotomy and POEM for nonachalasia motility disorders. Dis. Esophagus 2017, 30, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Herbella, F.A.M.; del Grande, J.C. New ambulatory techniques for assessment of esophageal motility and their applicability on achalasia study. Rev. CBC 2008, 35, 199–202. [Google Scholar]
- Kahrilas, P.J.; Ghosh, S.K.; Pandolfino, J.E. Esophageal motility disorders in terms of pressure topography: The Chicago Classification. J. Clin. Gastroenterol. 2008, 42, 627–635. [Google Scholar] [CrossRef] [PubMed]
- Kahrilas, P.J.; Bredenoord, A.J.; Fox, M.; Gyawali, C.P.; Roman, S.; Smout, A.J.; Pandolfino, J.E. International high resolution manometry working group. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol. Motil. 2015, 27, 160–174. [Google Scholar] [CrossRef] [PubMed]
- Van Hoeij, F.B.; Smout, A.J.; Bredenoord, A.J. Characterization of idiopathic esophagogastric junction outflow obstruction. Neurogastroenterol. Motil. 2015, 27, 1310–1316. [Google Scholar] [CrossRef] [PubMed]
- Scherer, J.R.; Kwiatek, M.A.; Soper, N.J.; Pandolfino, J.E.; Kahrilas, P.J. Functional esophagogastric junction obstruction with intact peristalsis: A heterogeneous syndrome sometimes akin to achalasia. J. Gastrointest. Surg. 2009, 13, 2219–2225. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Fernández, M.T.; Santander, C.; Marinero, A.; Burgos-Santamaría, D.; Chavarría-Herbozo, C. Characterization and follow-up of esophagogastric junction outflow obstruction detected by high resolution manometry. Neurogastroenterol. Motil. 2016, 28, 116–126. [Google Scholar] [CrossRef] [PubMed]
- DeLay, K.; Austin, G.L.; Menard-Katcher, P. Anatomic abnormalities are common potential explanations of manometric esophagogastric junction outflow obstruction. Neurogastroenterol. Motil. 2016, 28, 1166–1171. [Google Scholar] [CrossRef] [PubMed]
- Herbella, F.A.; Raz, D.J.; Nipomnick, I.; Patti, M.G. Primary versus secondary esophageal motility disorders: Diagnosis and implications for treatment. J. Laparaoendosc. Adv. Surg. Tech. A 2009, 19, 195–198. [Google Scholar] [CrossRef] [PubMed]
- Richter, J.E. Oesophageal motility disorders. Lancet 2001, 358, 823–828. [Google Scholar] [CrossRef]
- Patti, M.G.; Gorodner, M.V.; Galvani, C.; Tedesco, P.; Fisichella, P.M.; Ostroff, J.W.; Bagatelos, K.C.; Way, L.W. Spectrum of esophageal motility disorders: Implications for diagnosis and treatment. Arch. Surg. 2005, 140, 442. [Google Scholar] [CrossRef] [PubMed]
- Leconte, M.; Douard, R.; Gaudric, M.; Dumontier, I.; Chaussade, S.; Dousset, B. Functional results after extended myotomy for diffuse oesophageal spasm. Br. J. Surg. 2007, 94, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Roman, S.; Kahrilas, P.J. Distal esophageal spasm. Curr. Opin. Gastroenterol. 2015, 31, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.S.; Min, Y.W.; Rhee, P.L. Two distinct types of hypercontractile esophagus: Classic and spastic jackhammer. Gut Liver 2016, 10, 859–863. [Google Scholar] [CrossRef] [PubMed]
- Patti, M.G.; Pellegrini, C.A.; Arcerito, M.; Tong, J.; Mulvihill, S.J.; Way, L.W. Comparison of medical and minimally invasive surgical therapy for primary esophageal motility disorders. Arch. Surg. 1995, 130, 609–615. [Google Scholar] [CrossRef] [PubMed]
- Herbella, F.A.; Tineli, A.C.; Wilson, J.L., Jr.; del Grande, J.C. Surgical treatment of primary esophageal motility disorders. J. Gastrointest. Surg. 2008, 12, 604–608. [Google Scholar] [CrossRef] [PubMed]
- Menezes, M.A.; Herbella, F.A.; Patti, M.G. Laparoscopic antireflux surgery in patients with connective tissue diseases. J. Laparoendosc. Adv. Surg. Tech. A 2016, 26, 296–298. [Google Scholar] [CrossRef] [PubMed]
- Scheerens, C.; Tack, J.; Rommel, N. Buspirone, a new drug for the management of patients with ineffective esophageal motility? United Eur. Gastroenterol. J. 2015, 3, 261–265. [Google Scholar] [CrossRef] [PubMed]
- Herbella, F.A.; Tedesco, P.; Nipomnick, I.; Fisichella, P.M.; Patti, M.G. Effect of partial and total laparoscopic fundoplication on esophageal body motility. Surg. Endosc. 2007, 21, 285–288. [Google Scholar] [CrossRef] [PubMed]





© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schlottmann, F.; Patti, M.G. Primary Esophageal Motility Disorders: Beyond Achalasia. Int. J. Mol. Sci. 2017, 18, 1399. https://doi.org/10.3390/ijms18071399
Schlottmann F, Patti MG. Primary Esophageal Motility Disorders: Beyond Achalasia. International Journal of Molecular Sciences. 2017; 18(7):1399. https://doi.org/10.3390/ijms18071399
Chicago/Turabian StyleSchlottmann, Francisco, and Marco G. Patti. 2017. "Primary Esophageal Motility Disorders: Beyond Achalasia" International Journal of Molecular Sciences 18, no. 7: 1399. https://doi.org/10.3390/ijms18071399