The Retentive Strength of Laser-Sintered Cobalt-Chromium-Based Crowns after Pretreatment with a Desensitizing Paste Containing 8% Arginine and Calcium Carbonate
Abstract
1. Introduction
2. Results
3. Discussion
4. Materials and Methods
Statistical Analysis
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Rosenstiel, S.F.; Rashid, R.G. Postcementation hypersensitivity: Scientific data versus dentists’ perceptions. J. Prosthodont. 2003, 12, 73–81. [Google Scholar] [CrossRef]
- Johnson, G.H.; Powell, L.V.; DeRouen, T.A. Evaluation and control of post-cementation pulpal sensitivity: Zinc phosphate and glass ionomer luting cements. J. Am. Dent. Assoc. 1993, 124, 38–46. [Google Scholar] [CrossRef]
- Thylstrup, A.; Bille, J.; Qvist, V. Radiographic and observed tissue changes in approximal carious lesions at the time of operative treatment. Caries Res. 1986, 20, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Bernier, J.L.; Knapp, M.J. A new pulpal response to high-speed dental instruments. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 1958, 11, 167–183. [Google Scholar] [CrossRef]
- Richardson, D.; Tao, L.; Pashley, D.H. Dentin permeability: Effects of crown preparation. Int. J. Prosthodont. 1991, 4, 219–225. [Google Scholar]
- Langeland, K.; Langeland, L.K. Pulp reactions to crown preparation, impression, temporary crown fixation, and permanent cementation. J. Prosthet. Dent. 1965, 15, 129–143. [Google Scholar] [CrossRef]
- Zaimoglu, A.; Aydin, A.K. An evaluation of smear layer with various desensitizing agents after tooth preparation. J. Prosthet. Dent. 1992, 68, 450–457. [Google Scholar] [CrossRef]
- Sailer, I.; Tettamanti, S.; Stawarczyk, B.; Fischer, J.; Hammerle, C.H. In vitro study of the influence of dentin desensitizing and sealing on the shear bond strength of two universal resin cements. J. Adhes. Dent. 2010, 12, 381–392. [Google Scholar] [CrossRef]
- Sailer, I.; Oendra, A.E.; Stawarczyk, B.; Hammerle, C.H. The effects of desensitizing resin, resin sealing, and provisional cement on the bond strength of dentin luted with self-adhesive and conventional resincements. J. Prosthet. Dent. 2012, 107, 252–260. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Hartmann, R.; Hartmann, L.; Roos, M.; Ozcan, M.; Sailer, I.; Hammerle, C.H. The effect of dentin desensitizer on shear bond strength of conventional and self-adhesive resin luting cements after aging. Oper. Dent. 2011, 36, 492–501. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Hartmann, L.; Hartmann, R.; Roos, M.; Ender, A.; Ozcan, M.; Sailer, I.; Hammerle, C.H. Impact of gluma desensitizer on the tensile strength of zirconia crowns bonded to dentin: An in vitro study. Clin. Oral Investig. 2012, 16, 201–213. [Google Scholar] [CrossRef] [PubMed]
- Cobb, D.S.; Reinhardt, J.W.; Vargas, M.A. Effect of HEMA-containing dentin desensitizers on shear bond strength of a resin cement. Am. J. Dent. 1997, 10, 62–65. [Google Scholar] [PubMed]
- Soeno, K.; Taira, Y.; Matsumura, H.; Atsuta, M. Effect of desensitizers on bond strength of adhesive luting agents to dentin. J. Oral Rehabil. 2001, 28, 1122–1128. [Google Scholar] [CrossRef] [PubMed]
- Yim, N.H.; Rueggeberg, F.A.; Caughman, W.F.; Gardner, F.M.; Pashley, D.H. Effect of dentin desensitizers and cementing agents on retention of full crowns using standardized crown preparations. J. Prosthet. Dent. 2000, 83, 459–465. [Google Scholar] [CrossRef]
- Huh, J.B.; Kim, J.H.; Chung, M.K.; Lee, H.Y.; Choi, Y.G.; Shim, J.S. The effect of several dentin desensitizers on shear bond strength of adhesive resin luting cement using self-etching primer. J. Dent. 2008, 36, 1025–1032. [Google Scholar] [CrossRef] [PubMed]
- Aranha, A.C.; Siqueira Junior Ade, S.; Cavalcante, L.M.; Pimenta, L.A.; Marchi, G.M. Microtensile bond strengths of composite to dentin treated with desensitizer products. J. Adhes. Dent. 2006, 8, 85–90. [Google Scholar] [PubMed]
- Hamlin, D.; Williams, K.P.; Delgado, E.; Zhang, Y.P.; DeVizio, W.; Mateo, L.R. Clinical evaluation of the efficacy of a desensitizing paste containing 8% arginine and calcium carbonate for the in-office relief of dentin hypersensitivity associated with dental prophylaxis. Am. J. Dent. 2009, 22, 16A–20A. [Google Scholar]
- Schiff, T.; Delgado, E.; Zhang, Y.P.; Cummins, D.; DeVizio, W.; Mateo, L.R. Clinical evaluation of the efficacy of an in-office desensitizing paste containing 8% arginine and calcium carbonate in providing instant and lasting relief of dentin hypersensitivity. Am. J. Dent. 2009, 22, 8A–15A. [Google Scholar]
- Ayad, F.; Ayad, N.; Zhang, Y.P.; DeVizio, W.; Cummins, D.; Mateo, L.R. Comparing the efficacy in reducing dentin hypersensitivity of a new toothpaste containing 8.0% arginine, calcium carbonate, and 1450 ppm fluoride to a commercial sensitive toothpaste containing 2% potassium ion: An eight-week clinical study on Canadian adults. J. Clin. Dent. 2009, 20, 10–16. [Google Scholar]
- Docimo, R.; Montesani, L.; Maturo, P.; Costacurta, M.; Bartolino, M.; DeVizio, W.; Zhang, Y.P.; Cummins, D.; Dibart, S.; Mateo, L.R. Comparing the efficacy in reducing dentin hypersensitivity of a new toothpaste containing 8.0% arginine, calcium carbonate, and 1450 ppm fluoride to a commercial sensitive toothpaste containing 2% potassium ion: An eight-week clinical study in Rome, Italy. J. Clin. Dent. 2009, 20, 17–22. [Google Scholar]
- Nathoo, S.; Delgado, E.; Zhang, Y.P.; DeVizio, W.; Cummins, D.; Mateo, L.R. Comparing the efficacy in providing instant relief of dentin hypersensitivity of a new toothpaste containing 8.0% arginine, calcium carbonate, and 1450 ppm fluoride relative to a benchmark desensitizing toothpaste containing 2% potassium ion and 1450 ppm fluoride, and to a control toothpaste with 1450 ppm fluoride: A three-day clinical study in New Jersey, USA. J. Clin. Dent. 2009, 20, 123–130. [Google Scholar] [PubMed]
- Garcia-Godoy, A.; Garcia-Godoy, F. Effect of an 8.0% arginine and calcium carbonate in-office desensitizing paste on the shear bond strength of composites to human dental enamel. Am. J. Dent. 2010, 23, 324–326. [Google Scholar] [PubMed]
- Wang, Y.; Liu, S.; Pei, D.; Du, X.; Ouyang, X.; Huang, C. Effect of an 8.0% arginine and calcium carbonate in-office desensitizing paste on the microtensile bond strength of self-etching dental adhesives to human dentin. Am. J. Dent. 2012, 25, 281–286. [Google Scholar] [PubMed]
- Canares, G.; Salgado, T.; Pines, M.S.; Wolff, M.S. Effect of an 8.0% arginine and calcium carbonate desensitizing toothpaste on shear dentin bond strength. J. Clin. Dent. 2012, 23, 68–70. [Google Scholar] [PubMed]
- Chandavarkar, S.M.; Ram, S.M. A comparative evaluation of the effect of dentin desensitizers on the retention of complete cast metal crowns. Contemp. Clin. Dent. 2015, 6, S45–S50. [Google Scholar] [CrossRef] [PubMed]
- Pilo, R.; Harel, N.; Nissan, J.; Levartovsky, S. The retentive strength of cemented zirconium oxide crowns after dentin pretreatment with desensitizing paste containing 8% arginine and calcium carbonate. Int. J. Mol. Sci. 2016, 17, 426. [Google Scholar] [CrossRef] [PubMed]
- Quante, K.; Ludwig, K.; Kern, M. Marginal and internal fit of metal-ceramic crowns fabricated with a new laser melting technology. Dent. Mater. 2008, 24, 1311–1315. [Google Scholar] [CrossRef]
- Ucar, Y.; Akova, T.; Akyil, M.S.; Brantley, W.A. Internal fit evaluation of crowns prepared using a new dental crown fabrication technique: Laser-sintered Co-Cr crowns. J. Prosthet. Dent. 2009, 102, 253–259. [Google Scholar] [CrossRef]
- Tamac, E.; Toksavul, S.; Toman, M. Clinical marginal and internal adaptation of CAD/CAM milling, laser sintering, and cast metal ceramic crowns. J. Prosthet. Dent. 2014, 112, 909–913. [Google Scholar] [CrossRef]
- Lavender, S.A.; Petrou, I.; Heu, R.; Stranick, M.A.; Cummins, D.; Kilpatrick-Liverman, L.; Sullivan, R.J.; Santarpia, R.P., III. Mode of action studies on a new desensitizing dentifrice containing 8.0% arginine, a high cleaning calcium carbonate system and 1450 ppm fluoride. Am. J. Dent. 2010, 23, 14A–19A. [Google Scholar]
- Panagakos, F.; Schiff, T.; Guignon, A. Dentin hypersensitivity: Effective treatment with an in-office desensitizing paste containing 8% arginine and calcium carbonate. Am. J. Dent. 2009, 22, 3A–7A. [Google Scholar] [PubMed]
- Shetty, R.M.; Bhat, S.; Mehta, D.; Srivatsa, G.; Shetty, Y.B. Comparative analysis of postcementation hypersensitivity with glass ionomer cement and a resin cement: An in vivo study. J. Contemp. Dent. Pract. 2012, 13, 327–331. [Google Scholar] [PubMed]
- Rosenstiel, S.F.; Land, M.F.; Crispin, B.J. Dental luting agents: A review of the current literature. J. Prosthet. Dent. 1998, 80, 280–301. [Google Scholar] [CrossRef]
- Pattanaik, B.K.; Nagda, S.J. An evaluation of retention and marginal seating of Ni-Cr alloy cast restorations using three different luting cements: An in vitro study. Indian. J. Dent. Res. 2012, 23, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Wiskott, H.W.; Nicholls, J.I.; Belser, U.C. The relationship between abutment taper and resistance of cemented crowns to dynamic loading. Int. J. Prosthodont. 1996, 9, 117–139. [Google Scholar] [PubMed]
- Gorodovsky, S.; Zidan, O. Retentive strength, disintegration, and marginal quality of luting cements. J. Prosthet. Dent. 1992, 68, 269–274. [Google Scholar] [CrossRef]
- Behr, M.; Rosentritt, M.; Loher, H.; Kolbeck, C.; Trempler, C.; Stemplinger, B.; Kopzon, V.; Handel, G. Changes of cement properties caused by mixing errors: The therapeutic range of different cement types. Dent. Mater. 2008, 24, 1187–1193. [Google Scholar] [CrossRef] [PubMed]
- Pilo, R.; Lewinstein, I.; Ratzon, T.; Cardash, H.S.; Brosh, T. The influence of dentin and/or metal surface treatment on the retention of cemented crowns in teeth with an increased taper. Dent. Mater. 2008, 24, 1058–1064. [Google Scholar] [CrossRef] [PubMed]




| Cement Type | Treatment | Sample No. | Mean Retentive Value (MPa) | Standard Deviation |
|---|---|---|---|---|
| GIC | 1 | 10 | 6.39 | 1.06 |
| 2 | 10 | 5.73 | 1.10 | |
| Total | 20 | 6.04 | 1.10 | |
| ZPC | 1 | 10 | 2.39 | 0.99 |
| 2 | 10 | 3.10 | 1.44 | |
| Total | 20 | 2.75 | 1.25 | |
| Total | 1 | 20 | 4.29 | 2.27 |
| 2 | 20 | 4.41 | 1.83 | |
| Total | 40 | 4.36 | 2.03 |
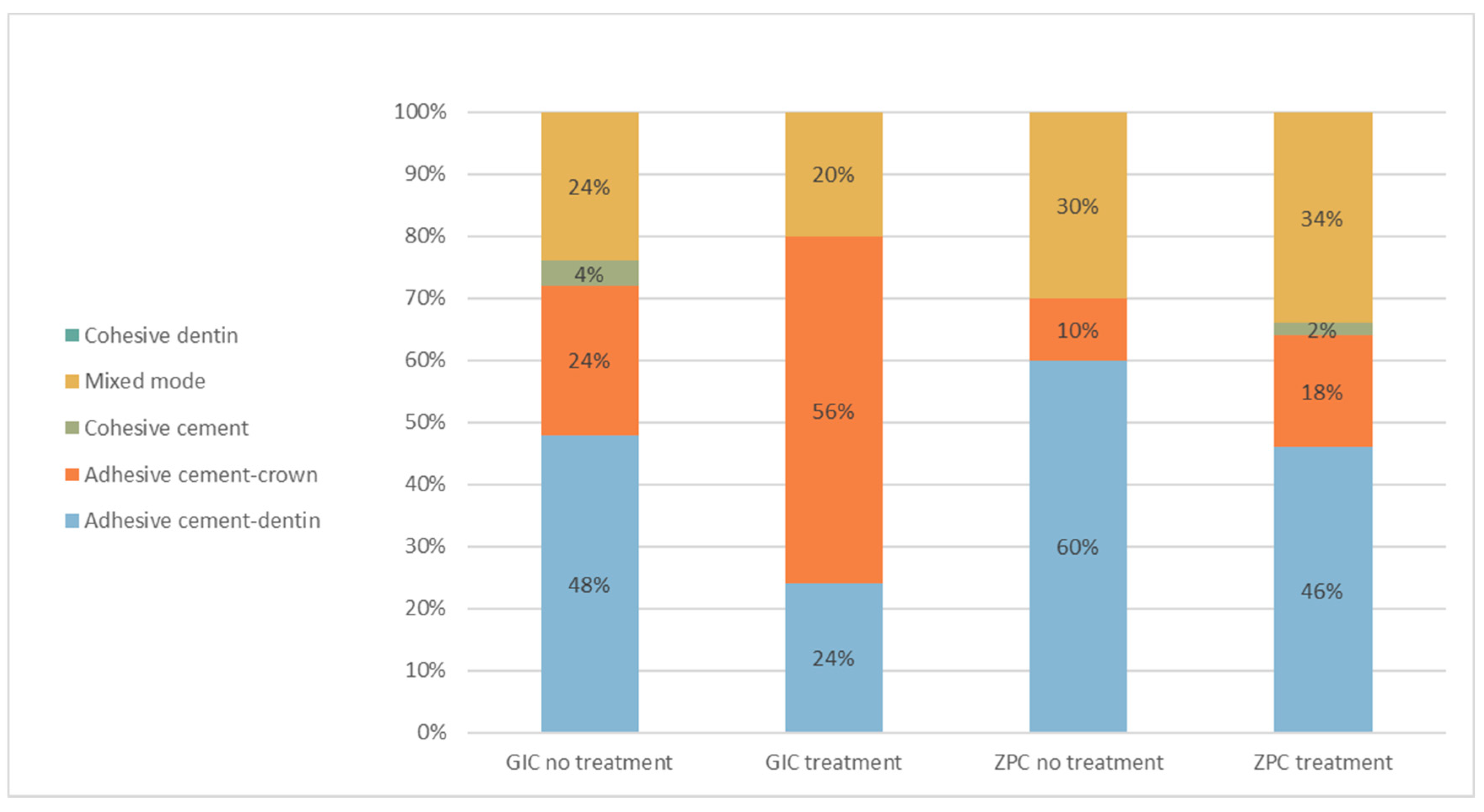
| Classification | Description | Criteria |
|---|---|---|
| 1 | Cement principally on crown surface | Adhesive cement-dentin |
| 2 | Cement principally on dentin surface | Adhesive cement-crown |
| 3 | Cement equally distributed on dentin & crown surfaces | Cohesive cement |
| 4 | Mixed mode | Adhesive & cohesive cement |
| 5 | Fracture of the tooth | Cohesive dentin |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pilo, R.; Agar-Zoizner, S.; Gelbard, S.; Levartovsky, S. The Retentive Strength of Laser-Sintered Cobalt-Chromium-Based Crowns after Pretreatment with a Desensitizing Paste Containing 8% Arginine and Calcium Carbonate. Int. J. Mol. Sci. 2018, 19, 4082. https://doi.org/10.3390/ijms19124082
Pilo R, Agar-Zoizner S, Gelbard S, Levartovsky S. The Retentive Strength of Laser-Sintered Cobalt-Chromium-Based Crowns after Pretreatment with a Desensitizing Paste Containing 8% Arginine and Calcium Carbonate. International Journal of Molecular Sciences. 2018; 19(12):4082. https://doi.org/10.3390/ijms19124082
Chicago/Turabian StylePilo, Raphael, Sharon Agar-Zoizner, Shaul Gelbard, and Shifra Levartovsky. 2018. "The Retentive Strength of Laser-Sintered Cobalt-Chromium-Based Crowns after Pretreatment with a Desensitizing Paste Containing 8% Arginine and Calcium Carbonate" International Journal of Molecular Sciences 19, no. 12: 4082. https://doi.org/10.3390/ijms19124082
APA StylePilo, R., Agar-Zoizner, S., Gelbard, S., & Levartovsky, S. (2018). The Retentive Strength of Laser-Sintered Cobalt-Chromium-Based Crowns after Pretreatment with a Desensitizing Paste Containing 8% Arginine and Calcium Carbonate. International Journal of Molecular Sciences, 19(12), 4082. https://doi.org/10.3390/ijms19124082






