A Meta-Analysis to Determine the Impact of Restaurant Menu Labeling on Calories and Nutrients (Ordered or Consumed) in U.S. Adults
Abstract
:1. Introduction
2. Materials and Methods
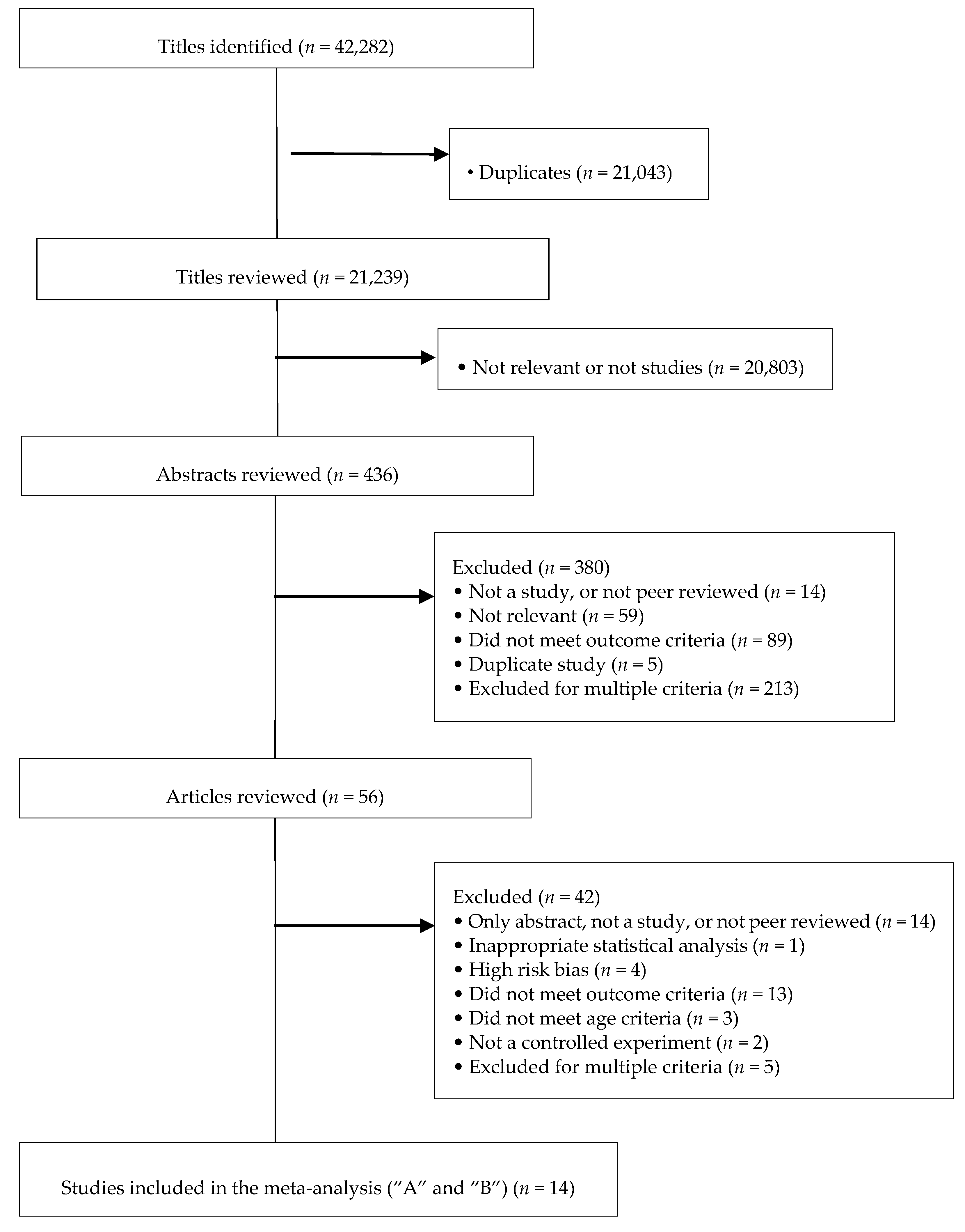
2.1. Study Identification and Selection
2.2. Data Collection
2.3. Statistics
3. Results
3.1. Selected Studies and Characteristics
3.2. Impact of Menu Labeling on Calories Ordered or Consumed
3.3. Impact of Menu Labeling on Carbohydrates, Fat, Saturated Fat, and Sodium Ordered or Consumed
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Benjamin, R.M. The Surgeon General’s vision for a healthy and fit nation. Public Health Rep. 2010, 125, 514–515. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. The Surgeon General’s Call to Action to Prevent and Decrease Overweight and Obesity; U.S. Department of Health and Human Services: Rockville, MD, USA, 2001.
- Burton, S.; Creyer, E.H.; Kees, J.; Huggins, K. Attacking the obesity epidemic: The potential health benefits of providing nutrition information in restaurants. Am. J. Public Health 2006, 96, 1669–1675. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; Doak, C.M. The obesity epidemic is a worldwide phenomenon. Nutr. Rev. 1998, 56, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Ogden, C.L.; Carroll, M.D.; Kit, B.K.; Flegal, K.M. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014, 311, 806–814. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Selected Health Conditions and Risk Factors: United States, Selected Years 1988–1994 through 2009–2010; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2011.
- Tsai, A.G.; Williamson, D.F.; Glick, H.A. Direct medical cost of overweight and obesity in the USA: A quantitative systematic review. Obes. Rev. 2011, 12, 50–61. [Google Scholar] [CrossRef] [PubMed]
- Stamler, R.; Stamler, J.; Riedlinger, W.F.; Algera, G.; Roberts, R.H. Weight and blood pressure. Findings in hypertension screening of 1 million Americans. JAMA 1978, 240, 1607–1610. [Google Scholar] [CrossRef] [PubMed]
- Criqui, M.H.; Mebane, I.; Wallace, R.B.; Heiss, G.; Holdbrook, M.J. Multivariate correlates of adult blood pressures in nine North American populations: The Lipid Research Clinics Prevalence Study. Prev. Med. 1982, 11, 391–402. [Google Scholar] [CrossRef]
- Dyer, A.R.; Elliott, P. The INTERSALT study: Relations of body mass index to blood pressure. INTERSALT Co-operative Research Group. J. Hum. Hypertens 1989, 3, 299–308. [Google Scholar] [PubMed]
- Brennan, P.J.; Simpson, J.M.; Blacket, R.B.; McGilchrist, C.A. The effects of body weight on serum cholesterol, serum triglycerides, serum urate and systolic blood pressure. Aust. N. Z. J. Med. 1980, 10, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Havlik, R.J.; Hubert, H.B.; Fabsitz, R.R.; Feinleib, M. Weight and hypertension. Ann. Intern. Med. 1983, 98, 855–859. [Google Scholar] [CrossRef] [PubMed]
- Colditz, G.A.; Willett, W.C.; Stampfer, M.J.; Manson, J.E.; Hennekens, C.H.; Arky, R.A.; Speizer, F.E. Weight as a Risk Factor for Clinical Diabetes in Women. Am. J. Epidemiol. 1990, 132, 501–513. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.M.; Rimm, E.B.; Colditz, G.A.; Stampfer, M.J.; Willett, W.C. Obesity, Fat Distribution, and Weight-Gain as Risk-Factors for Clinical Diabetes in Men. Diabetes Care 1994, 17, 961–969. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S.; Williamson, D.F.; Liu, S. Weight change and diabetes incidence: Findings from a national cohort of US adults. Am. J. Epidemiol. 1997, 146, 214–222. [Google Scholar] [CrossRef] [PubMed]
- Ohlson, L.O.; Larsson, B.; Svardsudd, K.; Welin, L.; Eriksson, H.; Wilhelmsen, L.; Björntorp, P.; Tibblin, G. The influence of body fat distribution on the incidence of diabetes mellitus. 13.5 years of follow-up of the participants in the study of men born in 1913. Diabetes 1985, 34, 1055–1058. [Google Scholar] [CrossRef] [PubMed]
- Hubert, H.B.; Feinleib, M.; McNamara, P.M.; Castelli, W.P. Obesity as an independent risk factor for cardiovascular-disease—A 26-year follow-up of participants in the Framingham heart-study. Circulation 1983, 67, 968–977. [Google Scholar] [CrossRef] [PubMed]
- Higgins, M.; Kannel, W.; Garrison, R.; Pinsky, J.; Stokes, J. Hazards of obesity-the Framingham experience. Acta Med. Scand. 1987, 222, 23–36. [Google Scholar] [CrossRef]
- Lapidus, L.; Bengtsson, C.; Larsson, B.; Pennert, K.; Rybo, E.; Sjostrom, L. Distribution of adipose tissue and risk of cardiovascular disease and death: A 12 year follow up of participants in the population study of women in Gothenburg, Sweden. Br. Med. J. (Clin. Res. Ed.) 1984, 289, 1257–1261. [Google Scholar] [CrossRef]
- Larsson, B.; Svardsudd, K.; Welin, L.; Wilhelmsen, L.; Bjorntorp, P.; Tibblin, G. Abdominal adipose tissue distribution, obesity, and risk of cardiovascular disease and death: 13 year follow up of participants in the study of men born in 1913. Br. Med. J. (Clin. Res. Ed.) 1984, 288, 1401–1404. [Google Scholar] [CrossRef]
- Wilding, J.P.H. Causes of obesity. Pract. Diabetes Int. 2001, 18, 288–292. [Google Scholar] [CrossRef]
- NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults (U.S.). Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults; The Evidence Report; National Heart, Lung and Blood Institute: Bethesda, MD, USA, 1998.
- Lin, B.; Guthrie, J. Nutritional Quality of Food Prepared at Home and Away From Home, 1977–2008; Report Number 105; United States Department of Agriculture, Economic Research Service: Washington, DC, USA, 2012.
- Stewart, H.; Blisard, N.; Bhuyan, S.; Nayga, R.M. The Demand for Food Away from Home Full-Service or Fast Food? Report Number 829; United States Department of Agriculture, Economic Research Service: Washington, DC, USA, 2004.
- Saelens, B.E.; Glanz, K.; Sallis, J.F.; Frank, L.D. Nutrition Environment Measures Study in Restaurants (NEMS-R): Development and evaluation. Am. J. Prev. Med. 2007, 32, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Deierlein, A.L.; Peat, K.; Claudio, L. Comparison of the nutrient content of children’s menu items at U.S. restaurant chains, 2010–2014. Nutr. J. 2015, 14, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.W.; Sturm, R. What’s on the menu? A review of the energy and nutritional content of U.S. chain restaurant menus. Public Health Nutr. 2013, 16, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Beydoun, M.A.; Powell, L.M.; Wang, Y.F. Reduced away-from-home food expenditure and better nutrition knowledge and belief can improve quality of dietary intake among U.S. adults. Public Health Nutr. 2009, 12, 369–381. [Google Scholar] [PubMed]
- Clemens, L.H.; Slawson, D.L.; Klesges, R.C. The effect of eating out on quality of diet in premenopausal women. J. Am. Diet. Assoc. 1999, 99, 442–444. [Google Scholar] [CrossRef]
- Guthrie, J.F.; Lin, B.H.; Frazao, E. Role of food prepared away from home in the American diet, 1977–1978 versus 1994–1996: Changes and consequences. J. Nutr. Educ. Behav. 2002, 34, 140–150. [Google Scholar] [CrossRef]
- Mancino, L.; Todd, J.; Lin, B.H. Separating what we eat from where: Measuring the effect of food away from home on diet quality. Food Policy 2009, 34, 557–562. [Google Scholar] [CrossRef]
- Jeffery, R.W.; French, S.A. Epidemic obesity in the United States: Are fast foods and television viewing contributing? Am. J. Public Health 1998, 88, 277–280. [Google Scholar] [CrossRef] [PubMed]
- McCrory, M.A.; Fuss, P.J.; Hays, N.P.; Vinken, A.G.; Greenberg, A.S.; Roberts, S.B. Overeating in America: Association between restaurant food consumption and body fatness in healthy adult men and women ages 19 to 80. Obes. Res. 1999, 7, 564–571. [Google Scholar] [CrossRef] [PubMed]
- Bowman, S.A.; Gortmaker, S.L.; Ebbeling, C.B.; Pereira, M.A.; Ludwig, D.S. Effects of fast-food consumption on energy intake and diet quality among children in a national household survey. Pediatrics 2004, 113, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Bowman, S.A.; Vinyard, B.T. Fast food consumption of U.S. adults: Impact on energy and nutrient intakes and overweight status. J. Am. Coll. Nutr. 2004, 23, 163–168. [Google Scholar] [CrossRef] [PubMed]
- Elbel, B.; Gyamfi, J.; Kersh, R. Child and adolescent fast-food choice and the influence of calorie labeling: A natural experiment. Int. J. Obes. 2011, 35, 493–500. [Google Scholar] [CrossRef] [PubMed]
- Roberto, C.A.; Haynos, A.F.; Schwartz, M.B.; Brownell, K.D.; White, M.A. Calorie estimation accuracy and menu labeling perceptions among individuals with and without binge eating and/or purging disorders. Eat Weight Disord 2013, 18, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Block, J.P.; Condon, S.K.; Kleinman, K.; Mullen, J.; Linakis, S.; Rifas-Shiman, S.; Gillman, M.W. Consumers’ estimation of calorie content at fast food restaurants: Cross sectional observational study. BMJ 2013, 346, f2907. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Todd, J.E.; Variyam, J.N. The Decline in Consumer Use of Food Nutrition Labels, 1995–2006; United States Department of Agriculture, Economic Research Service: Washington, DC, USA, 2008.
- U.S. Food & Drug Administration. Calories Count: Report of the Working Group on Obesity; U.S. Food & Drug Administration: Silver Spring, MD, USA, 2004.
- Patient Protection and Affordable Care Act, Public Law 111–14, 2 March 2010.
- Long, M.W.; Tobias, D.K.; Cradock, A.L.; Batchelder, H.; Gortmaker, S.L. Systematic review and meta-analysis of the impact of restaurant menu calorie labeling. Am. J. Public Health 2015, 105, e11–e24. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, S.E.; Cooper, M.; Mansfield, E.D. The influence of menu labeling on calories selected or consumed: A systematic review and meta-analysis. J. Acad. Nutr. Diet. 2014, 114, 1375–1388.e15. [Google Scholar] [CrossRef] [PubMed]
- Swartz, J.J.; Braxton, D.; Viera, A.J. Calorie menu labeling on quick-service restaurant menus: An updated systematic review of the literature. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 135. [Google Scholar] [CrossRef] [PubMed]
- Sarink, D.; Peeters, A.; Freak-Poli, R.; Beauchamp, A.; Woods, J.; Ball, K.; Backholer, K. The impact of menu energy labelling across socioeconomic groups: A systematic review. Appetite 2016, 99, 59–75. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, A.C.; Oliveira, R.C.; Proença, R.P.; Curioni, C.C.; Rodrigues, V.M.; Fiates, G.M. Influence of menu labeling on food choices in real-life settings: A systematic review. Nutr. Rev. 2016, 74, 534–548. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Crockett, R.A.; Hollands, G.J.; Jebb, S.A.; Marteau, T.M. Nutritional labelling for promoting healthier food purchasing and consumption. Cochrane Libr. 2011. [Google Scholar] [CrossRef]
- Ryan, R.; Hill, S.; Broclain, D.; Horey, D.; Oliver, S.; Prictor, M.; Cochrane Consumers and Communication Review Group. Study Design Guide. 2013. Available online: https://cccrg.cochrane.org/sites/cccrg.cochrane.org/files/public/uploads/Study_design_guide2013.pdf (accessed on 31 July 2017).
- Brissette, I.; Lowenfels, A.; Noble, C.; Spicer, D. Predictors of Total Calories Purchased at Fast-food Restaurants: Restaurant Characteristics, Calorie Awareness, and Use of Calorie Information. J. Nutr. Educ. Behav. 2013, 45, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Harnack, L.J.; French, S.A.; Oakes, J.M.; Story, M.T.; Jeffery, R.W.; Rydell, S.A. Effects of calorie labeling and value size pricing on fast food meal choices: Results from an experimental trial. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 63. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Altman, D.; Sterne, J. Assessing Risk of Bias in Included Studies. The Cochrane Collaboration. 2011. Available online: http://methods.cochrane.org/bias/sites/methods.cochrane.org.bias/files/public/uploads/6.%20Assessing%20risk%20of%20bias%20in%20included%20studies%20v1.0%20Standard%20author%20slides.pdf (accessed on 31 July 2017).
- Cochrane Public Health Group. Guide for Developing a Cochrane Protocol. November 2011. Available online: http://ph.cochrane.org/sites/ph.cochrane.org/files/public/uploads/Guide%20for%20PH%20protocol_Nov%202011_final%20for%20website.pdf (accessed on 31 July 2017).
- Egger., M.; Smith, G.D.; Phillips, A.N. Meta-analysis: Principles and procedures. BMJ 1997, 315, 1533–1537. [Google Scholar] [CrossRef] [PubMed]
- Hedges, L.V.; Olkin, I. Statistical Methods for Meta-Analysis; Academic Press: New York, NY, USA, 1985. [Google Scholar]
- Gi, L.; Behnke, C.; Almanza, B. An Evaluation of Three Nutrition Labeling Formats for Restaurant Menus. FIU Hosp. Rev. 2014, 31, 3. [Google Scholar]
- Chu, Y.H.; Frongillo, E.A.; Jones, S.J.; Kaye, G.L. Improving patrons’ meal selections through the use of point-of-selection nutrition labels. Am. J. Public Health 2009, 99, 2001–2005. [Google Scholar] [CrossRef] [PubMed]
- Wisdom, J.; Downs, J.S.; Loewenstein, G. Promoting healthy choices: Information versus convenience. Am. Econ. J. Appl. Econ. 2010, 2, 164–178. [Google Scholar] [CrossRef]
- Boonme, K.; Hanus, B.; Prybutok, V.R.; Peak, D.A.; Ryan, C. Visual information influences consumer fast-food choices. Nutr. Food Sci. 2014, 44, 279–293. [Google Scholar] [CrossRef]
- Stubenitsky, K.; Aaron, J.; Catt, S.; Mela, D. The influence of recipe modification and nutritional information on restaurant food acceptance and macronutrient intakes. Public Health Nutr. 2000, 3, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Yoon., H.J.; George, T. Nutritional information disclosure on the menu: Focusing on the roles of menu context, nutritional knowledge and motivation. Int. J. Hosp. Manag. 2012, 31, 1187–1194. [Google Scholar] [CrossRef]
- Conklin, M.T.; Lambert, C.U.; Cranage, D.A. Nutrition information at point of selection could benefit college students. Top. Clin. Nutr. 2005, 20, 90–96. [Google Scholar] [CrossRef]
- Vargas-Bustamante, A. Menu labeling perception and health behaviors among immigrant and U.S. born minority populations: Assessment in two Los Angeles public markets. Salud Pública Méx 2013, 55, s515–s522. [Google Scholar] [CrossRef] [PubMed]
- Kozup, J.C.; Creyer, E.H.; Burton, S. Making healthful food choices: The influence of health claims and nutrition information on consumers’ evaluations of packaged food products and restaurant menu items. J. Mark. 2003, 67, 19–34. [Google Scholar] [CrossRef]
- Gallicano, R.; Blomme, R.J.; van Rheede, A. Consumer response to nutrition information menu labeling in full-service restaurants: Making the healthy choice. Adv. Hosp. Leis. 2012, 8, 109–125. [Google Scholar]
- Lin, C.A.; Mou, Y.; Lagoe, C. Communicating nutrition information: Usability and usefulness of the interactive menus of national fast food chain restaurants. J. Commun. Health 2011, 4, 187–199. [Google Scholar] [CrossRef]
- Heiman, A.; Lowengart, O. Calorie information effects on consumers’ food choices: Sources of observed gender heterogeneity. J. Bus. Res. 2014, 67, 964–973. [Google Scholar] [CrossRef]
- Lucy, K.; Henderson, K. The Impact of Food Nutrition Information on Dining Hall Food Choices in College Students. Obes. Res. 2003. Available online: https://xue.glgoo.net/scholar?hl=zh-CN&q=The+Impact+of+Food+Nutrition+Information+on+Dining+Hall+Food+Choices+in+College+Students&btnG=&lr= (accessed on 31 July 2017).
- Almanza, B.A.; Mason, A.C.; Widdows, R.; Girard, F.J. Consumer responses to nutrition guidelines labeling in a university restaurant. J. Am. Diet. Assoc. 1993, 93, 580–581. [Google Scholar] [CrossRef]
- Dumanovsky, T.; Huang, C.Y.; Nonas, C.A.; Matte, T.D.; Bassett, M.T.; Silver, L.D. Changes in energy content of lunchtime purchases from fast food restaurants after introduction of calorie labelling: Cross sectional customer surveys. BMJ 2011, 343, d4464. [Google Scholar] [CrossRef] [PubMed]
- Aron, J.I.; Evans, R.E.; Mela, D.J. Paradoxical effect of a nutrition labelling scheme in a student cafeteria. Nutr. Res. 1995, 15, 1251–1261. [Google Scholar] [CrossRef]
- Bassett, M.T.; Dumanovsky, T.; Huang, C.; Silver, L.D.; Young, C.; Nonas, C.; Matte, T.D.; Chideya, S.; Frieden, T.R. Purchasing behavior and calorie information at fast-food chains in New York City, 2007. Am. J. Public Health 2008, 98, 1457–1459. [Google Scholar] [CrossRef] [PubMed]
- Bollinger, B.; Leslie, P.; Sorensen, A. Calorie posting in chain restaurants. Am. Econ. J. Econ. Policy 2011, 3, 91–128. [Google Scholar] [CrossRef]
- Downs, J.S.; Loewenstein, G.; Wisdom, J. Strategies for promoting healthier food choices. Am. Econ. Rev. 2009, 99, 159–164. [Google Scholar] [CrossRef]
- Dumanovsky, T.; Huang, C.Y.; Bassett, M.T.; Silver, L.D. Consumer awareness of fast-food calorie information in New York City after implementation of a menu labeling regulation. Am. J. Public Health 2010, 100, 2520–2525. [Google Scholar] [CrossRef] [PubMed]
- Girz, L.; Polivy, J.; Herman, C.; Lee, H. The effects of calorie information on food selection and intake. Int. J. Obes. 2012, 36, 1340–1345. [Google Scholar] [CrossRef] [PubMed]
- Ellison, B.; Lusk, J.L.; Davis, D. Looking at the label and beyond: The effects of calorie labels, health consciousness, and demographics on caloric intake in restaurants. Int. J. Behav. Nutr. Phys. Act. 2013, 10. [Google Scholar] [CrossRef] [PubMed]
- Gerend, M.A. Does calorie information promote lower calorie fast food choices among college students? J. Adolesc. Health 2009, 44, 84–86. [Google Scholar] [CrossRef] [PubMed]
- Dowray, S.; Swartz, J.J.; Braxton, D.; Viera, A.J. Potential effect of physical activity based menu labels on the calorie content of selected fast food meals. Appetite 2013, 62, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.J.; Roberto, C.A.; Liu, L.J.; Brownell, K.D. A test of different menu labeling presentations. Appetite 2012, 59, 770–777. [Google Scholar] [CrossRef] [PubMed]
- Morley, B.; Scully, M.; Martin, J.; Niven, P.; Dixon, H.; Wakefield, M. What types of nutrition menu labelling lead consumers to select less energy-dense fast food? An experimental study. Appetite 2013, 67, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Roseman, M.G.; Mathe-Soulek, K.; Higgins, J.A. Relationships among grocery nutrition label users and consumers’ attitudes and behavior toward restaurant menu labeling. Appetite 2013, 71, 274–278. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Miao, L. Effects of calorie information disclosure on consumers’ food choices at restaurants. Int. J. Hosp. Manag. 2013, 33, 106–117. [Google Scholar] [CrossRef]
- Sharma, S.; Wagle, A.; Sucher, K.; Bugwadia, N. Impact of point of selection nutrition information on meal choices at a table-service restaurant. J. Food Bus. Res. 2011, 14, 146–161. [Google Scholar] [CrossRef]
- Albright, C.L.; Flora, J.A.; Fortmann, S.P. Restaurant menu labeling: Impact of nutrition information on entree sales and patron attitudes. Health Educ. Behav. 1990, 17, 157–167. [Google Scholar] [CrossRef]
- Eldridge, A.L.; Snyder, M.P.; Faus, N.G.; Kotz, K. Development and evaluation of a labeling program for low-fat foods in a discount department store foodservice area. J. Nutr. Educ. 1997, 29, 159–161. [Google Scholar] [CrossRef]
- Anderson, J.; Haas, M.H. Impact of a nutrition education program on food sales in restaurants. J. Nur. Educ. 1990, 22, 232–238. [Google Scholar] [CrossRef]
- Freedman, M.R. Point-of-selection nutrition information influences choice of portion size in an all-you-can-eat university dining hall. J. Food Bus. Res. 2011, 14, 86–98. [Google Scholar] [CrossRef]
- Cinciripini, P.M. Changing food selections in a public cafeteria an applied behavior analysis. Behav. Modif. 1984, 8, 520–539. [Google Scholar] [CrossRef]
- Davis-Chervin, D.; Rogers, T.; Clark, M. Influencing food selection with point-of-choice nutrition information. J. Nutr. Educ. 1985, 17, 18–22. [Google Scholar] [CrossRef]
- Webb, K.L.; Solomon, L.S.; Sanders, J.; Akiyama, C.; Crawford, P.B. Menu labeling responsive to consumer concerns and shows promise for changing patron purchases. J. Hunger Environ. Nutr. 2011, 6, 166–178. [Google Scholar] [CrossRef]
- Milich, R.; Anderson, J.; Mills, M. Effects of visual presentation of caloric values on food buying by normal and obese persons. Percept. Mot. Skills 1976, 42, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Sato, J.N.; Wagle, A.; McProud, L.; Lee, L. Food Label Effects on Customer Purchases in a Hospital Cafeteria in Northern California. J. Food Bus. Res. 2013, 16, 155–168. [Google Scholar] [CrossRef]
- Levin, S. Pilot study of a cafeteria program relying primarily on symbols to promote healthy choices. J. Nutr. Educ. 1996, 28, 282–285. [Google Scholar] [CrossRef]
- Dubbert, P.M.; Johnson, W.G.; Schlundt, D.G.; Montague, N.W. The influence of caloric information on cafeteria food choices. J. Appl. Behav. Anal. 1984, 17, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Sproul, A.D.; Canter, D.D.; Schmidt, J.B. Does point-of-purchase nutrition labeling influence meal selections? A test in an Army cafeteria. Mil. Med. 2003, 168, 556. [Google Scholar] [PubMed]
- Elbel, B.; Kersh, R.; Brescoll, V.L.; Dixon, L.B. Calorie labeling and food choices: A first look at the effects on low-income people in New York City. Health Aff. 2009, 28, w1110–w1121. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, E.A.; Strombotne, K.L.; Chan, N.L.; Krieger, J. Mandatory menu labeling in one fast-food chain in King County, Washington. Am. J. Prev. Med. 2011, 40, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Roberto, C.A.; Larsen, P.D.; Agnew, H.; Baik, J.; Brownell, K.D. Evaluating the impact of menu labeling on food choices and intake. Am. J. Public Health 2010, 100, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Temple, J.L.; Johnson, K.; Recupero, K.; Suders, H. Nutrition labels decrease energy intake in adults consuming lunch in the laboratory. J. Acad. Nutr. Diet. 2010, 111, S52–S55. [Google Scholar] [CrossRef] [PubMed]
- Auchincloss, A.H.; Mallya, G.G.; Leonberg, B.L.; Ricchezza, A.; Glanz, K.; Schwarz, D.F. Customer responses to mandatory menu labeling at full-service restaurants. Am. J. Prev. Med. 2013, 45, 710–719. [Google Scholar] [CrossRef] [PubMed]
- Downs, J.S.; Wisdom, J.; Wansink, B.; Loewenstein, G. Supplementing menu labeling with calorie recommendations to test for facilitation effects. Am. J. Public Health 2013, 103, 1604–1609. [Google Scholar] [CrossRef] [PubMed]
- Krieger, J.W.; Chan, N.L.; Saelens, B.E.; Ta, M.L.; Solet, D.; Fleming, D.W. Menu Labeling Regulations and Calories Purchased at Chain Restaurants. Am. J. Prev. Med. 2013, 44, 595–604. [Google Scholar] [CrossRef] [PubMed]
- Nelson, D.C.; Almanza, B.A.; Jaffe, W.F. The effect of point-of-sales nutrition information on the entree selection of patrons of a university foodservice operation. J. Nutr. Recipe Menu Dev. 1996, 2, 29–50. [Google Scholar] [CrossRef]
- Platkin, C.; Yeh, M.-C.; Hirsch, K.; Wiewel, E.W.; Lin, C.-Y.; Tung, H.-J.; Castellanos, V.H. The effect of menu labeling with calories and exercise equivalents on food selection and consumption. BMC Obes. 2014, 1, 1. [Google Scholar] [CrossRef] [PubMed]
- Pulos, E.; Leng, K. Evaluation of a voluntary menu-labeling program in full-service restaurants. Am. J. Public Health 2010, 100, 1035–1039. [Google Scholar] [CrossRef] [PubMed]
- Tandon, P.S.; Zhou, C.; Chan, N.L.; Lozano, P.; Couch, S.C.; Glanz, K.; Krieger, J.; Saelens, B.E. The impact of menu labeling on fast-food purchases for children and parents. Am. J. Prev. Med. 2011, 41, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Temple, J.L.; Johnson, K.M.; Archer, K.; LaCarte, A.; Yi, C.; Epstein, L.H. Influence of simplified nutrition labeling and taxation on laboratory energy intake in adults. Appetite 2011, 57, 184–192. [Google Scholar] [CrossRef] [PubMed]
- List, J.A.; Levitt, S.D. What Do Laboratory Experiments Tell Us About the Real World. NBER Working Paper. 2005. Available online: http://pricetheory.uchicago.edu/levitt/Papers/LevittList2005.pdf (accessed on 31 July 2017).
- Glanz, K.; Basil, M.; Maibach, E.; Goldberg, J.; Snyder, D. Why Americans eat what they do: Taste, nutrition, cost, convenience, and weight control concerns as influences on food consumption. J. Am. Diet. Assoc. 1998, 98, 1118–1126. [Google Scholar] [CrossRef]
- Rydell, S.A.; Harnack, L.J.; Oakes, J.M.; Story, M.; Jeffery, R.W.; French, S.A. Why eat at fast-food restaurants: Reported reasons among frequent consumers. J. Acad. Nutr. Diet. 2008, 108, 2066–2070. [Google Scholar] [CrossRef] [PubMed]
- Mohr, P.; Wilson, C.; Dunn, K.; Brindal, E.; Wittert, G. Personal and lifestyle characteristics predictive of the consumption of fast foods in Australia. Public Health Nutr. 2007, 10, 1456–1463. [Google Scholar] [CrossRef] [PubMed]
- Bruemmer, B.; Krieger, J.; Saelens, B.E.; Chan, N. Energy, saturated fat, and sodium were lower in entrées at chain restaurants at 18 months compared with 6 months following the implementation of mandatory menu labeling regulation in King County, Washington. J. Acad. Nutr. Diet. 2012, 112, 1169–1176. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Agriculture; U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 7th ed.; Government Printing Office: Washington, DC, USA, 2010; pp. 1–112.
- Dall, T.M.; Fulgoni, V.L., 3rd; Zhang, Y.; Reimers, K.J.; Packard, P.T.; Astwood, J.D. Potential health benefits and medical cost savings from calorie, sodium, and saturated fat reductions in the American diet. Am. J. Health Promot. 2009, 23, 412–422. [Google Scholar] [CrossRef] [PubMed]
- Bibbins-Domingo, K.; Chertow, G.M.; Coxson, P.G.; Chertow, G.M.; Coxson, P.G.; Moran, A.; Lightwood, J.M.; Pletcher, M.J.; Goldman, L. Projected effect of dietary salt reductions on future cardiovascular disease. N. Engl. J. Med. 2010, 362, 590–599. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.C.; Coxson, P.; Shen, Y.M.; Goldman, L.; Bibbins-Domingo, K. A penny-per-ounce tax on sugar-sweetened beverages would cut health and cost burdens of diabetes. Health Aff. (Millwood) 2012, 31, 199–207. [Google Scholar] [CrossRef] [PubMed]

| Study Design a | Criteria | Study Classification | |
|---|---|---|---|
| All Criteria Fulfilled | All but ≤1 Criteria Fulfilled | ||
| Randomized Controlled Trial (RCT) b | • Unique groups of participants in experimental and controlled conditions (not crossed over) | A | B |
| Quasi-Randomized Controlled Trial (Quasi-RCT) | • Unique groups of participants in experimental and controlled conditions (not crossed over) | A | B |
| Controlled Before-and-After (CBA) study |
| A | B c |
| Interrupted Time Series (ITS) Study |
| A | B |
| Cross-Sectional Study |
| B | Exclude |
| Study | Sample Characteristics | Study Design ** | Study Design Classification | Setting *** | Meal Type | Outcomes of Interest Assessed **** | |||
|---|---|---|---|---|---|---|---|---|---|
| N * | Unit of Analysis | Age (Years) | Other | ||||||
| Auchincloss et al., 2013 [101] | 648 | Number of participants | >18 | 60% female; 50% black/African American; 15 years mean education; 40–50% overweight; >41% income over $60,000 | Cross-sectional | B | Full-service restaurants f | Dinner | Ordered calories; total carbohydrate; saturated fat; sodium |
| Brissette et al., 2013 [50] | 1094 | Number of participants | >15 | 71% non-Hispanic white; 59% male; 42% ≤ high school education; | Cross-sectional | B | Fast-food restaurants | Lunch (92%) and dinner (8%) | Ordered calories |
| Downs et al., 2013 [102] | 1094 | Number of participants | >18 | 36% African American, 53% female; 49% had a BMI > 25 kg/m2 | BA (not controlled) | B | Fast-food restaurants | Lunch | Ordered calories |
| Elbel et al., 2009 [97] | 1156 | Number of participants | >18 | 66% black; 38% male; almost 50% with ≤ high school diploma; low income community | CBA | A | Fast-food restaurants | Lunch and dinner | Ordered calories; saturated fat; sodium |
| Finkelstein et al., 2011 [98] | 540,552 | Number of transactions | n.a. | King County and adjacent county Taco Time Northwest customers in Washington, U.S. | CBA | A | Fast-food restaurants | Various meals | Ordered calories |
| Harnack et al., 2008 [51] | 301 a | Number of participants | >16 | About 75% white; 61% female; 37% with some college education; 56% had a BMI > 25 kg/m2 | Quasi-RCT | A | Laboratory setting | Dinner | Ordered and consumed calories; total carbohydrate; total fat; saturated fat |
| Krieger et al., 2013 [103] | 2746 b | Number of participants | >40 | 76% non-Hispanic white; 59% male; 32% from a low income/diverse area | BA (not controlled) | B | Fast-food restaurants | Lunch | Ordered calories |
| Nelson et al., 1996 [104] | 3234 | Number of purchased entrees | 18–81 | >53% male; Recruited from University restaurant, >60% with master’s degree or higher | ITS (Only four data collection points) | B | Full-service restaurant g | Lunch | Ordered calories, fat and sodium (calculated from Appendix B in Nelson et al.) |
| Platkin et al., 2014 [105] | 104 c | Number of participants | 18–34 | 71% black or Hispanic; female; recruited on college campus; mean BMI 28 kg/m2 | BA (single-location) | B | Laboratory setting | Lunch | Ordered calories |
| Pulos and Leng, 2010 [106] | 206 | Number of purchased entrees | >18 | 55% female | BA (not controlled) | B | Full-service restaurant h | Lunch and Dinner | Ordered calories, total carbohydrate, total fat, sodium |
| Roberto et al., 2010 [99] | 293 | Number of participants | >18 | 50% female; 55% white; 85% with some college or higher; mean BMI 25 kg/m2 | RCT | A | Laboratory setting | Dinner | Ordered and consumed calories |
| Tandon et al., 2011 [107] | 242 d | Number of participants | n.a. | 80% females; 70% college degree or higher; 39–70% with income >$90,000; 64% with a BMI > 25 kg/m2 | BA (single-location) | B | Fast-food restaurant | Various meals | Ordered calories |
| Temple et al., 2010 [100] | 47 | Number of participants | 18–50 | 51% female; 91% completed some college or higher; 43% with income <$10,000; mean BMI 26 kg/m2 | Quasi-RCT | A | Laboratory setting | Lunch | Consumed calories |
| Temple et al., 2011 [108] | 102 e | Number of participants | Adults | 55% female recruited from University; 47% white; 51% with income <$9999; 53% completed some college; 68% had a BMI > 25 kg/m2 | Quasi-RCT (crossed-over) | B | Laboratory setting | Lunch | Consumed calories |
| Nutrient | Mean (SD) | Mean Difference (95% CI) | |
|---|---|---|---|
| Control | Treatment | ||
| Total Carbohydrates (g) | |||
| Harnack et al., 2008 [51] | 105.7 (39.2) | 110.3 (63.3) | 4.6 (−7.3, 16.5) |
| Auchincloss et al., 2013 [101] | 131 (72) | 115 (64) | −16 (−26.5, −5.5) * |
| Pulos and Leng, 2010 [106] | n.a. a | n.a. | −0.2 (−1.1, 0.8) |
| Overall | −0.1 (−0.6, 0.5) | ||
| Total Fat (g) | |||
| Harnack et al., 2008 [51] | 32.5 (18.6) | 34.3 (19.3) | 1.8 (−2.5, 6.1) |
| Nelson et al., 1996 [104] | 36.8 (10.5) | 34.4 (8.9) | −2.4 (−3.1, −1.8) * |
| Pulos and Leng, 2010 [106] | n.a. | n.a. | −1.6 (−2.2, −1.0) * |
| Overall | <0.1 (−0.0, 0.0) | ||
| Saturated Fat (g) | |||
| Harnack et al., 2008 [51] | 9.7 (6.7) | 10.7 (7.6) | 1.0 (−0.6, 2.6) |
| Auchincloss et al., 2013 [101] b | 36.5 (23.9) | 33.5 (22.1) | −3.0 (−6.5, 0.5) |
| Elbel et al., 2009 [97] | 11.8 (19.7) | 11.4 (19.7) | −0.4 (−2.0, 1.2) |
| Overall | <0.1 (−0.1, 0.1) | ||
| Sodium (mg) | |||
| Auchincloss et al., 2013 [101] b | 3315 (1389) | 3111 (1460) | −204 (−423.8, 15.8) |
| Nelson et al., 1996 [104] | 2077 (1032) | 2113 (1045) | 36 (−34, 106) |
| Pulos and Leng, 2010 [106] | n.a. | n.a. | −45.7 (−74.5, −16.8) * |
| Elbel et al., 2009 [97] | 1392 (1925) | 1476 (2396) | 84 (−96, 264) |
| Overall | −0.6 (−3.7, 2.5) | ||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cantu-Jungles, T.M.; McCormack, L.A.; Slaven, J.E.; Slebodnik, M.; Eicher-Miller, H.A. A Meta-Analysis to Determine the Impact of Restaurant Menu Labeling on Calories and Nutrients (Ordered or Consumed) in U.S. Adults. Nutrients 2017, 9, 1088. https://doi.org/10.3390/nu9101088
Cantu-Jungles TM, McCormack LA, Slaven JE, Slebodnik M, Eicher-Miller HA. A Meta-Analysis to Determine the Impact of Restaurant Menu Labeling on Calories and Nutrients (Ordered or Consumed) in U.S. Adults. Nutrients. 2017; 9(10):1088. https://doi.org/10.3390/nu9101088
Chicago/Turabian StyleCantu-Jungles, Thaisa M., Lacey A. McCormack, James E. Slaven, Maribeth Slebodnik, and Heather A. Eicher-Miller. 2017. "A Meta-Analysis to Determine the Impact of Restaurant Menu Labeling on Calories and Nutrients (Ordered or Consumed) in U.S. Adults" Nutrients 9, no. 10: 1088. https://doi.org/10.3390/nu9101088
APA StyleCantu-Jungles, T. M., McCormack, L. A., Slaven, J. E., Slebodnik, M., & Eicher-Miller, H. A. (2017). A Meta-Analysis to Determine the Impact of Restaurant Menu Labeling on Calories and Nutrients (Ordered or Consumed) in U.S. Adults. Nutrients, 9(10), 1088. https://doi.org/10.3390/nu9101088






