A Glimpse into Humoral Response and Related Therapeutic Approaches of Takayasu’s Arteritis
Abstract
1. Introduction
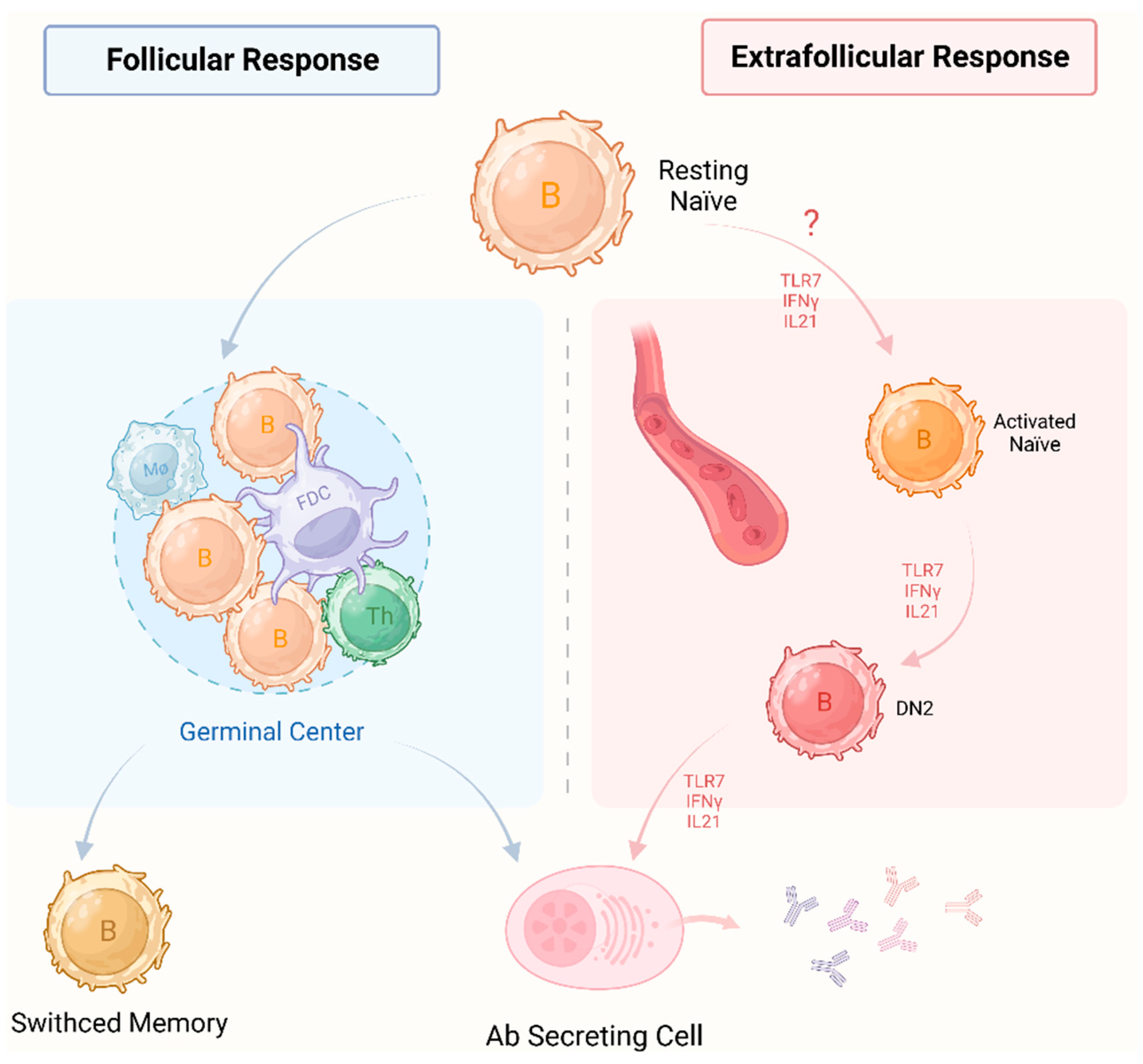
2. The Role of Autoreactive B Cells
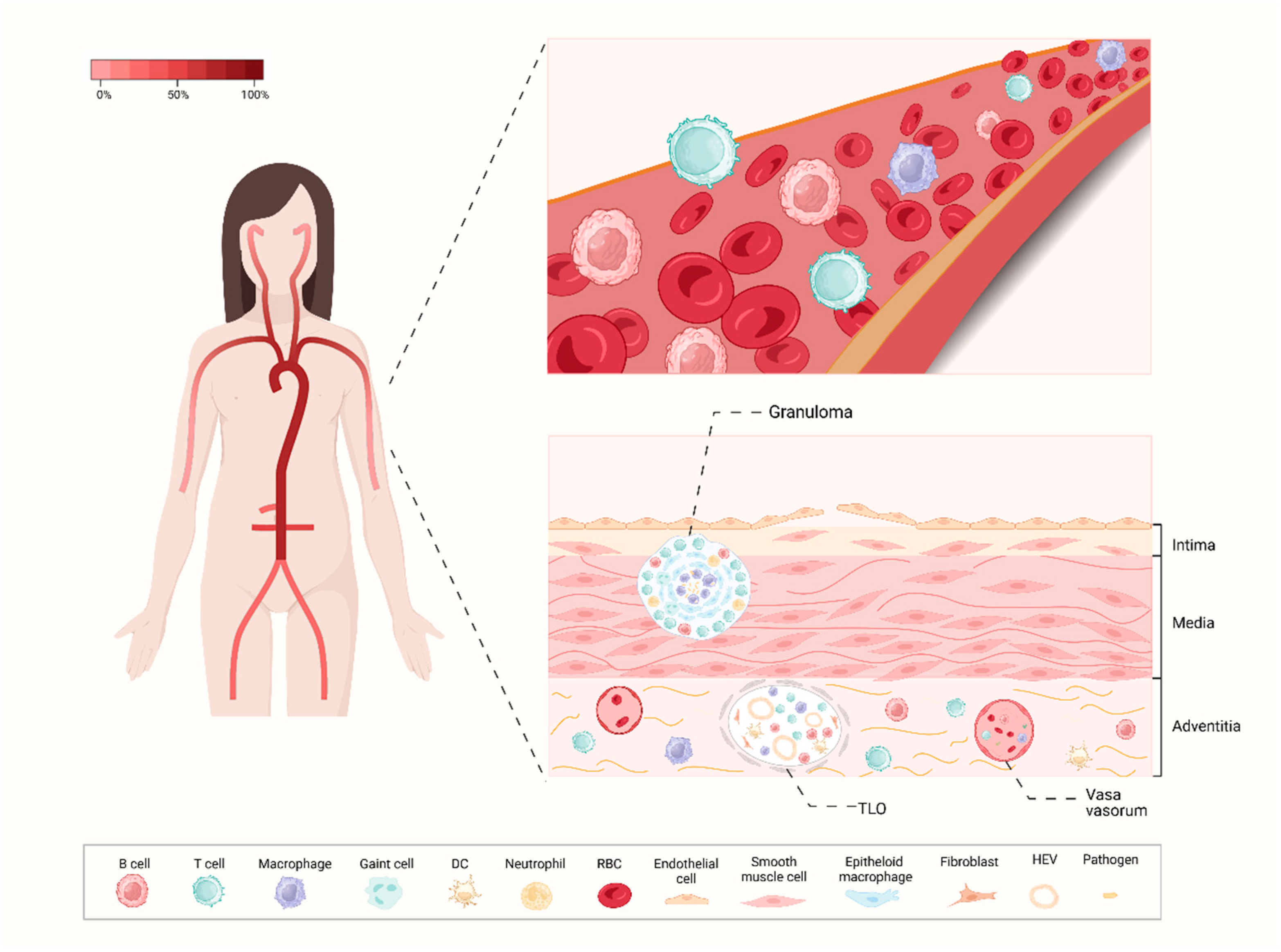
3. Tertiary Lymphoid Organs
4. Autoantibody Production
4.1. Non-Specific Autoantibodies
4.2. Specific Autoantibodies
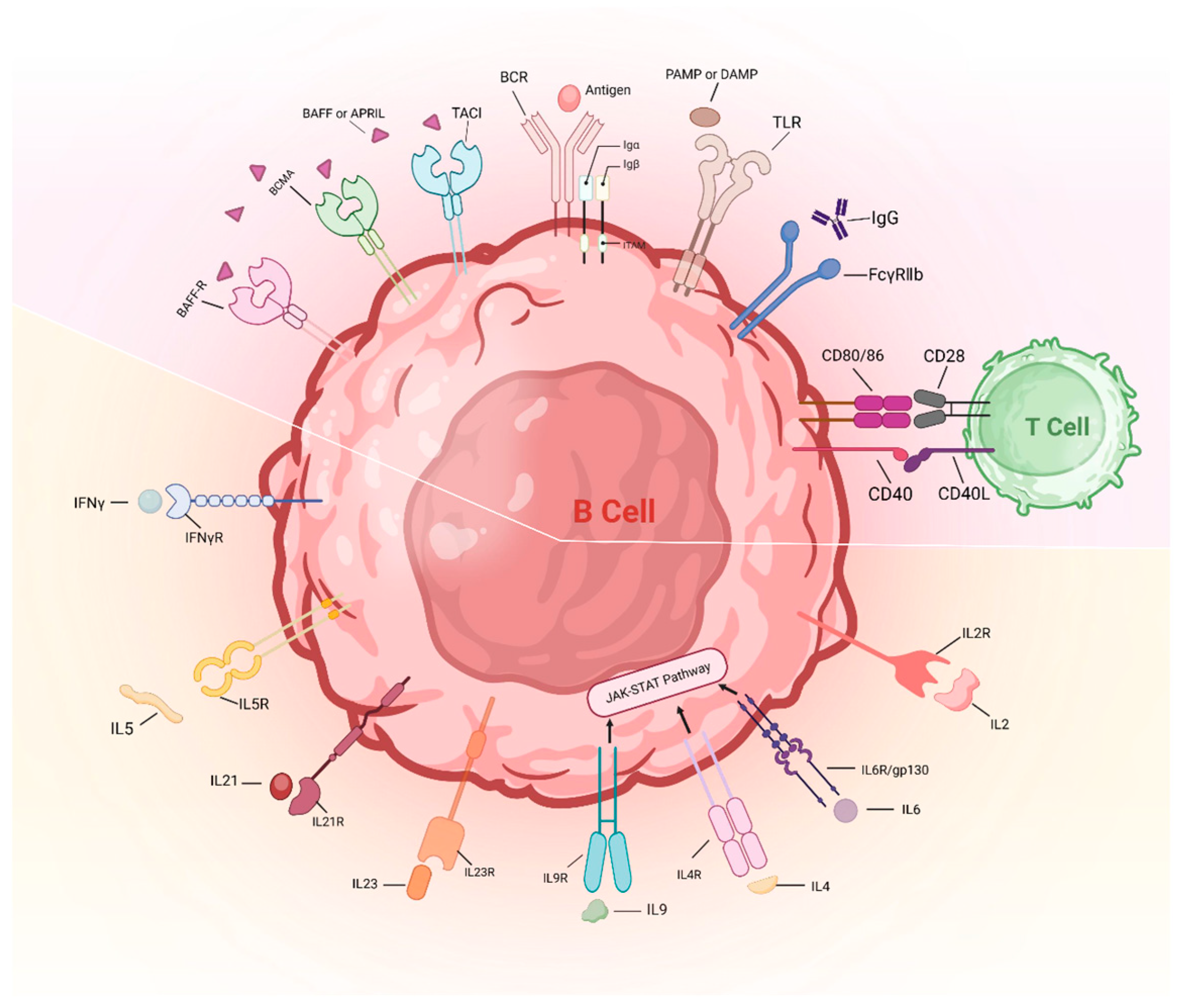
5. B Cell Checkpoints in TAK
6. Th Cell Profiles in Humoral Immunity and Pathogenicity
6.1. Th1 Response
6.2. Th2 Response
6.3. Th17 Response
6.4. Tfh Response
7. Therapeutic Approaches Related to Humoral Response
7.1. B Cell Depletion Therapy
7.2. IL-6R Inhibitors
7.3. JAK Inhibitors
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Tombetti, E.; Mason, J.C. Takayasu arteritis: Advanced understanding is leading to new horizons. Rheumatology 2019, 58, 206–219. [Google Scholar] [CrossRef] [PubMed]
- Koide, K. Takayasu arteritis in Japan. Heart Vessel. Suppl. 1992, 7, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Watts, R.; Al-Taiar, A.; Mooney, J.; Scott, D.; Macgregor, A. The epidemiology of Takayasu arteritis in the UK. Rheumatology 2009, 48, 1008–1011. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, A.J.; Mandl, T. Takayasu arteritis in southern Sweden. J. Rheumatol. 2015, 42, 853–858. [Google Scholar] [CrossRef] [PubMed]
- Gudbrandsson, B.; Molberg, O.; Garen, T.; Palm, O. Prevalence, Incidence, and Disease Characteristics of Takayasu Arteritis by Ethnic Background: Data From a Large, Population-Based Cohort Resident in Southern Norway. Arthritis Care Res. 2017, 69, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Tomelleri, A.; Campochiaro, C.; Sartorelli, S.; Cavalli, G.; De Luca, G.; Baldissera, E.; Dagna, L. Gender differences in clinical presentation and vascular pattern in patients with Takayasu arteritis. Scand. J. Rheumatol. 2019, 48, 482–490. [Google Scholar] [CrossRef] [PubMed]
- Danda, D.; Goel, R.; Joseph, G.; Kumar, S.T.; Nair, A.; Ravindran, R.; Jeyaseelan, L.; Merkel, P.A.; Grayson, P.C. Clinical course of 602 patients with Takayasu’s arteritis: Comparison between Childhood-onset versus adult onset disease. Rheumatology 2021, 60, 2246–2255. [Google Scholar] [CrossRef] [PubMed]
- Aeschlimann, F.A.; Barra, L.; Alsolaimani, R.; Benseler, S.M.; Hebert, D.; Khalidi, N.; Laxer, R.M.; Noone, D.; Pagnoux, C.; Twilt, M.; et al. Presentation and Disease Course of Childhood-Onset Versus Adult-Onset Takayasu Arteritis. Arthritis Rheumatol. 2019, 71, 315–323. [Google Scholar] [CrossRef]
- Quinn, K.A.; Gribbons, K.B.; Carette, S.; Cuthbertson, D.; Khalidi, N.A.; Koening, C.L.; Langford, C.A.; McAlear, C.A.; Monach, P.A.; Moreland, L.W.; et al. Patterns of clinical presentation in Takayasu’s arteritis. Semin. Arthritis Rheum. 2020, 50, 576–581. [Google Scholar] [CrossRef]
- Tian, X.; Zeng, X. Early diagnosis and standardized treatment are critical to improve the prognosis of patients with Takayasu’s arteritis. Rheumatol. Immunol. Res. 2024, 5, 1–4. [Google Scholar] [CrossRef]
- Tian, X.; Zeng, X. Chinese guideline for the diagnosis and treatment of Takayasu’s arteritis (2023). Rheumatol. Immunol. Res. 2024, 5, 5–26. [Google Scholar] [CrossRef] [PubMed]
- Langford, C.A.; Cuthbertson, D.; Ytterberg, S.R.; Khalidi, N.; Monach, P.A.; Carette, S.; Seo, P.; Moreland, L.W.; Weisman, M.; Koening, C.L.; et al. A Randomized, Double-Blind Trial of Abatacept (CTLA-4Ig) for the Treatment of Takayasu Arteritis. Arthritis Rheumatol. 2017, 69, 846–853. [Google Scholar] [CrossRef] [PubMed]
- Wen, X.; Song, G.; Hu, C.; Pan, J.; Wu, Z.; Li, L.; Liu, C.; Tian, X.; Zhang, F.; Qian, J.; et al. Identification of Novel Serological Autoantibodies in Takayasu Arteritis Patients Using HuProt Arrays. Mol. Cell Proteom. 2021, 20, 100036. [Google Scholar] [CrossRef] [PubMed]
- Inder, S.J.; Bobryshev, Y.V.; Cherian, S.M.; Wang, A.Y.; Lord, R.S.; Masuda, K.; Yutani, C. Immunophenotypic analysis of the aortic wall in Takayasu’s arteritis: Involvement of lymphocytes, dendritic cells and granulocytes in immuno-inflammatory reactions. Cardiovasc. Surg. 2000, 8, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Desbois, A.C.; Régnier, P.; Quiniou, V.; Lejoncour, A.; Maciejewski-Duval, A.; Comarmond, C.; Vallet, H.; Rosenzwag, M.; Darrasse-Jèze, G.; Derian, N.; et al. Specific Follicular Helper T Cell Signature in Takayasu Arteritis. Arthritis Rheumatol. 2021, 73, 1233–1243. [Google Scholar] [CrossRef] [PubMed]
- Hoyer, B.F.; Mumtaz, I.M.; Loddenkemper, K.; Bruns, A.; Sengler, C.; Hermann, K.G.; Maza, S.; Keitzer, R.; Burmester, G.R.; Buttgereit, F.; et al. Takayasu arteritis is characterised by disturbances of B cell homeostasis and responds to B cell depletion therapy with rituximab. Ann. Rheum. Dis. 2012, 71, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Caltran, E.; Di Colo, G.; Ghigliotti, G.; Capecchi, R.; Catarsi, E.; Puxeddu, I.; Migliorini, P.; Tavoni, A. Two Takayasu arteritis patients successfully treated with rituximab. Clin. Rheumatol. 2014, 33, 1183–1184. [Google Scholar] [CrossRef] [PubMed]
- Pugh, D.; Karabayas, M.; Basu, N.; Cid, M.C.; Goel, R.; Goodyear, C.S.; Grayson, P.C.; McAdoo, S.P.; Mason, J.C.; Owen, C.; et al. Large-vessel vasculitis. Nat. Rev. Dis. Primers 2022, 7, 93. [Google Scholar] [CrossRef] [PubMed]
- Nishimoto, N.; Nakahara, H.; Yoshio-Hoshino, N.; Mima, T. Successful treatment of a patient with Takayasu arteritis using a humanized anti-interleukin-6 receptor antibody. Arthritis Rheum. 2008, 58, 1197–1200. [Google Scholar] [CrossRef]
- Nishino, Y.; Tamai, M.; Kawakami, A.; Koga, T.; Makiyama, J.; Maeda, Y.; Jiuchi, Y.; Miyashita, T.; Izumi, Y.; Eguchi, K.; et al. Serum levels of BAFF for assessing the disease activity of Takayasu arteritis. Clin. Exp. Rheumatol. 2010, 28 (Suppl. S57), S14–S17. [Google Scholar]
- Navarra, S.V.; Guzmán, R.M.; Gallacher, A.E.; Hall, S.; Levy, R.A.; Jimenez, R.E.; Li, E.K.; Thomas, M.; Kim, H.Y.; León, M.G.; et al. Efficacy and safety of belimumab in patients with active systemic lupus erythematosus: A randomised, placebo-controlled, phase 3 trial. Lancet 2011, 377, 721–731. [Google Scholar] [CrossRef] [PubMed]
- Espinoza, J.L.; Ai, S.; Matsumura, I. New Insights on the Pathogenesis of Takayasu Arteritis: Revisiting the Microbial Theory. Pathogens 2018, 7, 73. [Google Scholar] [CrossRef] [PubMed]
- Brunner, J.; Feldman, B.M.; Tyrrell, P.N.; Kuemmerle-Deschner, J.B.; Zimmerhackl, L.B.; Gassner, I.; Benseler, S.M. Takayasu arteritis in children and adolescents. Rheumatology 2010, 49, 1806–1814. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Ma, J.; Wu, Q.; Luo, X.; Chen, Z.; Kou, L. Circulating B lymphocytes producing autoantibodies to endothelial cells play a role in the pathogenesis of Takayasu arteritis. J. Vasc. Surg. 2011, 53, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Rubtsov, A.V.; Rubtsova, K.; Fischer, A.; Meehan, R.T.; Gillis, J.Z.; Kappler, J.W.; Marrack, P. Toll-like receptor 7 (TLR7)-driven accumulation of a novel CD11c⁺ B-cell population is important for the development of autoimmunity. Blood 2011, 118, 1305–1315. [Google Scholar] [CrossRef] [PubMed]
- Phalke, S.; Rivera-Correa, J.; Jenkins, D.; Flores Castro, D.; Giannopoulou, E.; Pernis, A.B. Molecular mechanisms controlling age-associated B cells in autoimmunity. Immunol. Rev. 2022, 307, 79–100. [Google Scholar] [CrossRef] [PubMed]
- Jenks, S.A.; Cashman, K.S.; Zumaquero, E.; Marigorta, U.M.; Patel, A.V.; Wang, X.; Tomar, D.; Woodruff, M.C.; Simon, Z.; Bugrovsky, R.; et al. Distinct Effector B Cells Induced by Unregulated Toll-like Receptor 7 Contribute to Pathogenic Responses in Systemic Lupus Erythematosus. Immunity 2018, 49, 725–739.e6. [Google Scholar] [CrossRef] [PubMed]
- Pitzalis, C.; Jones, G.W.; Bombardieri, M.; Jones, S.A. Ectopic lymphoid-like structures in infection, cancer and autoimmunity. Nat. Rev. Immunol. 2014, 14, 447–462. [Google Scholar] [CrossRef] [PubMed]
- Fridman, W.H.; Meylan, M.; Petitprez, F.; Sun, C.M.; Italiano, A.; Sautès-Fridman, C. B cells and tertiary lymphoid structures as determinants of tumour immune contexture and clinical outcome. Nat. Rev. Clin. Oncol. 2022, 19, 441–457. [Google Scholar] [CrossRef]
- Inder, S.J.; Bobryshev, Y.V.; Cherian, S.M.; Lord, R.S.; Masuda, K.; Yutani, C. Accumulation of lymphocytes, dendritic cells, and granulocytes in the aortic wall affected by Takayasu’s disease. Angiology 2000, 51, 565–579. [Google Scholar] [CrossRef]
- Clement, M.; Galy, A.; Bruneval, P.; Morvan, M.; Hyafil, F.; Benali, K.; Pasi, N.; Deschamps, L.; Pellenc, Q.; Papo, T.; et al. Tertiary Lymphoid Organs in Takayasu Arteritis. Front. Immunol. 2016, 7, 158. [Google Scholar] [CrossRef] [PubMed]
- Clement, M.; Guedj, K.; Andreata, F.; Morvan, M.; Bey, L.; Khallou-Laschet, J.; Gaston, A.T.; Delbosc, S.; Alsac, J.M.; Bruneval, P.; et al. Control of the T follicular helper-germinal center B-cell axis by CD8⁺ regulatory T cells limits atherosclerosis and tertiary lymphoid organ development. Circulation 2015, 131, 560–570. [Google Scholar] [CrossRef] [PubMed]
- Eivazi, S.; Bagheri, S.; Hashemzadeh, M.S.; Ghalavand, M.; Qamsari, E.S.; Dorostkar, R.; Yasemi, M. Development of T follicular helper cells and their role in disease and immune system. Biomed. Pharmacother. 2016, 84, 1668–1678. [Google Scholar] [CrossRef] [PubMed]
- Decker, P.; Olivier, P.; Risse, J.; Zuily, S.; Wahl, D. Tocilizumab and refractory Takayasu disease: Four case reports and systematic review. Autoimmun. Rev. 2018, 17, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Trimm, E.; Red-Horse, K. Vascular endothelial cell development and diversity. Nat. Rev. Cardiol. 2023, 20, 197–210. [Google Scholar] [CrossRef] [PubMed]
- Legendre, P.; Régent, A.; Thiebault, M.; Mouthon, L. Anti-endothelial cell antibodies in vasculitis: A systematic review. Autoimmun. Rev. 2017, 16, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Eichhorn, J.; Sima, D.; Thiele, B.; Lindschau, C.; Turowski, A.; Schmidt, H.; Schneider, W.; Haller, H.; Luft, F.C. Anti-endothelial cell antibodies in Takayasu arteritis. Circulation 1996, 94, 2396–2401. [Google Scholar] [CrossRef] [PubMed]
- Nityanand, S.; Mishra, K.; Shrivastava, S.; Holm, G.; Lefvert, A.K. Autoantibodies against cardiolipin and endothelial cells in Takayasu’s arteritis: Prevalence and isotype distribution. Br. J. Rheumatol. 1997, 36, 923–924. [Google Scholar] [CrossRef] [PubMed]
- Sima, D.; Thiele, B.; Turowski, A.; Wilke, K.; Hiepe, F.; Volk, D.; Sönnichsen, N. Anti-endothelial antibodies in Takayasu arteritis. Arthritis Rheum. 1994, 37, 441–443. [Google Scholar] [CrossRef]
- Park, M.C.; Park, Y.B.; Jung, S.Y.; Lee, K.H.; Lee, S.K. Anti-endothelial cell antibodies and antiphospholipid antibodies in Takayasu’s arteritis: Correlations of their titers and isotype distributions with disease activity. Clin. Exp. Rheumatol. 2006, 24, S10–S16. [Google Scholar]
- Praprotnik, S.; Blank, M.; Meroni, P.L.; Rozman, B.; Eldor, A.; Shoenfeld, Y. Classification of anti-endothelial cell antibodies into antibodies against microvascular and macrovascular endothelial cells—The pathogenic and diagnostic implications. Arthritis Rheum.-Us 2001, 44, 1484–1494. [Google Scholar] [CrossRef]
- Sharma, B.K.; Jain, S.; Radotra, B.D. An autopsy study of Takayasu arteritis in India. Int. J. Cardiol. 1998, 66 (Suppl. S1), S85–S90; discussion S91. [Google Scholar] [CrossRef] [PubMed]
- Sgonc, R.; Gruschwitz, M.S.; Boeck, G.; Sepp, N.; Gruber, J.; Wick, G. Endothelial cell apoptosis in systemic sclerosis is induced by antibody-dependent cell-mediated cytotoxicity via CD95. Arthritis Rheum.-Us 2000, 43, 2550–2562. [Google Scholar] [CrossRef]
- Bordron, A.; Dueymes, M.; Levy, Y.; Jamin, C.; Leroy, J.P.; Piette, J.C.; Shoenfeld, Y.; Youinou, P.Y. The binding of some human anti-endothelial cell antibodies induces endothelial cell apoptosis. J. Clin. Investig. 1998, 101, 2029–2035. [Google Scholar] [CrossRef] [PubMed]
- Blank, M.; Krause, I.; Goldkorn, T.; Praprotnik, S.; Livneh, A.; Langevitz, P.; Kaganovsky, E.; Morgenstern, S.; Cohen, S.; Barak, V.; et al. Monoclonal anti-endothelial cell antibodies from a patient with Takayasu arteritis activate endothelial cells from large vessels. Arthritis Rheum. 1999, 42, 1421–1432. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, S.K.; Tripathy, N.K.; Nityanand, S. Antigenic targets and pathogenicity of anti-aortic endothelial cell antibodies in Takayasu arteritis. Arthritis Rheum. 2006, 54, 2326–2333. [Google Scholar] [CrossRef] [PubMed]
- Jamin, C.; Dugue’, C.; Alard, J.-E.; Jousse, S.; Saraux, A.; Guillevin, L.C.; Piette, J.-C.; Youinou, P. Induction of endothelial cell apoptosis by the binding of anti-endothelial cell antibodies to Hsp60 in vasculitis-associated systemic autoimmune diseases. Arthritis Rheum.-Us 2005, 52, 4028–4038. [Google Scholar] [CrossRef] [PubMed]
- Tripathy, N.K.; Sinha, N.; Nityanand, S. Anti-annexin V antibodies in Takayasu’s arteritis: Prevalence and relationship with disease activity. Clin. Exp. Immunol. 2003, 134, 360–364. [Google Scholar] [CrossRef] [PubMed]
- Karasawa, R.; Kurokawa, M.S.; Yudoh, K.; Masuko, K.; Ozaki, S.; Kato, T. Peroxiredoxin 2 is a novel autoantigen for anti-endothelial cell antibodies in systemic vasculitis. Clin. Exp. Immunol. 2010, 161, 459–470. [Google Scholar] [CrossRef]
- Haller, H.; Bertram, A.; Nadrowitz, F.; Menne, J. Monocyte chemoattractant protein-1 and the kidney. Curr. Opin. Nephrol. Hypertens 2016, 25, 42–49. [Google Scholar] [CrossRef]
- He, G.; Karin, M. NF-κB and STAT3—Key players in liver inflammation and cancer. Cell Res. 2011, 21, 159–168. [Google Scholar] [CrossRef]
- Kornberg, A.; Renaudineau, Y.; Blank, M.; Youinou, P.; Shoenfeld, Y. Anti-beta 2-glycoprotein I antibodies and anti-endothelial cell antibodies induce tissue factor in endothelial cells. Isr Med. Assoc. J. 2000, 2, 27–31. [Google Scholar] [PubMed]
- Garcia, D.; Erkan, D. Diagnosis and Management of the Antiphospholipid Syndrome. N. Engl. J. Med. 2018, 378, 2010–2021. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Zhou, M.L.; Liang, D.D.; Wang, J.J.; Yang, J.; Zeng, C.H.; Liu, Z.H.; Zhang, H.T. Treatment and clinicopathological characteristics of lupus nephritis with anti-neutrophil cytoplasmic antibody positivity: A case-control study. BMJ Open 2017, 7, e015668. [Google Scholar] [CrossRef]
- Ueda, H.; Ishimura, E.; Yunoki, T.; Tsuchida, T.; Matsumoto, N.; Jono, S.; Imanishi, Y.; Inaba, M.; Nishizawa, Y. Cimetidine-induced tubulointerstitial nephritis with both MPO-ANCA and PR3-ANCA. Clin. Exp. Nephrol. 2005, 9, 332–334. [Google Scholar] [CrossRef]
- Ferraz-Amaro, I.; Herrero, M.J.; Jurado, A.; Díaz-González, F. Dual positivity for cytoplasmic and perinuclear anti-neutrophil antibodies in a patient with Henoch-Schönlein purpura. Clin. Exp. Rheumatol. 2004, 22, 233–234. [Google Scholar] [PubMed]
- Tiliakos, A.M.; Tiliakos, N.A. Dual ANCA positivity in subacute bacterial endocarditis. J. Clin. Rheumatol. Pract. Rep. Rheum. Musculoskelet. Dis. 2008, 14, 38–40. [Google Scholar] [CrossRef] [PubMed]
- Baier, E.; Olgemöller, U.; Biggemann, L.; Buck, C.; Tampe, B. Dual-Positive MPO- and PR3-ANCA-Associated Vasculitis Following SARS-CoV-2 mRNA Booster Vaccination: A Case Report and Systematic Review. Vaccines 2022, 10, 653. [Google Scholar] [CrossRef]
- Jishi, A.A.; Krishnan, P.R.; Almawi, W.Y. Takayasu arteritis with high titre of antiphospholipid antibodies and MTHFR Polymorphism. J. Thromb. Thrombolysis 2005, 20, 47–50. [Google Scholar] [CrossRef]
- Lee, H.J.; Hwang, J.P.; Kim, H.S. Takayasu arteritis and antiphospholipid antibody syndrome in an elderly woman. Korean J. Intern. Med. 2015, 30, 934–937. [Google Scholar] [CrossRef]
- Haviv, Y.S. Association of anticardiolipin antibodies with vascular injury: Possible mechanisms. Postgrad. Med. J. 2000, 76, 625–628. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.; Kwon, H.C.; Song, J.J.; Park, Y.B.; Lee, S.W. Association between the antineutrophil cytoplasmic antibody and late coronary arterial occlusive disease in patients with Takayasu arteritis. J. Cardiol. 2020, 76, 407–412. [Google Scholar] [CrossRef] [PubMed]
- Hu, C.J.; Pan, J.B.; Song, G.; Wen, X.T.; Wu, Z.Y.; Chen, S.; Mo, W.X.; Zhang, F.C.; Qian, J.; Zhu, H.; et al. Identification of Novel Biomarkers for Behcet Disease Diagnosis Using Human Proteome Microarray Approach. Mol. Cell Proteom. 2017, 16, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Hu, C.J.; Song, G.; Huang, W.; Liu, G.Z.; Deng, C.W.; Zeng, H.P.; Wang, L.; Zhang, F.C.; Zhang, X.; Jeong, J.S.; et al. Identification of new autoantigens for primary biliary cirrhosis using human proteome microarrays. Mol. Cell Proteom. 2012, 11, 669–680. [Google Scholar] [CrossRef]
- Guilpain, P.; Mouthon, L. Antiendothelial cells autoantibodies in vasculitis-associated systemic diseases. Clin. Rev. Allergy Immunol. 2008, 35, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Shirai, T.; Fujii, H.; Ono, M.; Nakamura, K.; Watanabe, R.; Tajima, Y.; Takasawa, N.; Ishii, T.; Harigae, H. A novel autoantibody against fibronectin leucine-rich transmembrane protein 2 expressed on the endothelial cell surface identified by retroviral vector system in systemic lupus erythematosus. Arthritis Res. Ther. 2012, 14, R157. [Google Scholar] [CrossRef]
- Shirai, T.; Fujii, H.; Ono, M.; Watanabe, R.; Ishii, T.; Harigae, H. An innovative method to identify autoantigens expressed on the endothelial cell surface: Serological identification system for autoantigens using a retroviral vector and flow cytometry (SARF). Clin. Dev. Immunol. 2013, 2013, 453058. [Google Scholar] [CrossRef] [PubMed]
- Shirai, T.; Fujii, H.; Ono, M.; Watanabe, R.; Shirota, Y.; Saito, S.; Ishii, T.; Nose, M.; Harigae, H. A novel autoantibody against ephrin type B receptor 2 in acute necrotizing encephalopathy. J. Neuroinflammation 2013, 10, 128. [Google Scholar] [CrossRef]
- Mutoh, T.; Shirai, T.; Ishii, T.; Shirota, Y.; Fujishima, F.; Takahashi, F.; Kakuta, Y.; Kanazawa, Y.; Masamune, A.; Saiki, Y.; et al. Identification of two major autoantigens negatively regulating endothelial activation in Takayasu arteritis. Nat. Commun. 2020, 11, 1253. [Google Scholar] [CrossRef]
- Griffin, J.H.; Zlokovic, B.V.; Mosnier, L.O. Activated protein C, protease activated receptor 1, and neuroprotection. Blood 2018, 132, 159–169. [Google Scholar] [CrossRef]
- Ren, K.; Lu, Y.J.; Mo, Z.C.; Liu, X.; Tang, Z.L.; Jiang, Y.; Peng, X.S.; Li, L.; Zhang, Q.H.; Yi, G.H. ApoA-I/SR-BI modulates S1P/S1PR2-mediated inflammation through the PI3K/Akt signaling pathway in HUVECs. J. Physiol. Biochem. 2017, 73, 287–296. [Google Scholar] [CrossRef] [PubMed]
- Zanoni, P.; Khetarpal, S.A.; Larach, D.B.; Hancock-Cerutti, W.F.; Millar, J.S.; Cuchel, M.; DerOhannessian, S.; Kontush, A.; Surendran, P.; Saleheen, D.; et al. Rare variant in scavenger receptor BI raises HDL cholesterol and increases risk of coronary heart disease. Science 2016, 351, 1166–1171. [Google Scholar] [CrossRef] [PubMed]
- Giltiay, N.V.; Chappell, C.P.; Clark, E.A. B-cell selection and the development of autoantibodies. Arthritis Res. Ther. 2012, 14 (Suppl. S4), S1. [Google Scholar] [CrossRef] [PubMed]
- Wardemann, H.; Yurasov, S.; Schaefer, A.; Young, J.W.; Meffre, E.; Nussenzweig, M.C. Predominant autoantibody production by early human B cell precursors. Science 2003, 301, 1374–1377. [Google Scholar] [CrossRef] [PubMed]
- Jackson, S.W.; Kolhatkar, N.S.; Rawlings, D.J. B cells take the front seat: Dysregulated B cell signals orchestrate loss of tolerance and autoantibody production. Curr. Opin. Immunol. 2015, 33, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Rawlings, D.J.; Metzler, G.; Wray-Dutra, M.; Jackson, S.W. Altered B cell signalling in autoimmunity. Nat. Rev. Immunol. 2017, 17, 421–436. [Google Scholar] [CrossRef] [PubMed]
- Huang, B.Q.; Li, J.; Tian, X.P.; Zeng, X.F. Analysis of differentially expressed microRNA and protein expression profiles carried by exosomes in the plasma of patients with Takayasu’s arteritis. Zhonghua Nei Ke Za Zhi 2023, 62, 61–69. [Google Scholar] [PubMed]
- Habib, T.; Funk, A.; Rieck, M.; Brahmandam, A.; Dai, X.; Panigrahi, A.K.; Luning Prak, E.T.; Meyer-Bahlburg, A.; Sanda, S.; Greenbaum, C.; et al. Altered B cell homeostasis is associated with type I diabetes and carriers of the PTPN22 allelic variant. J. Immunol. 2012, 188, 487–496. [Google Scholar] [CrossRef] [PubMed]
- Menard, L.; Saadoun, D.; Isnardi, I.; Ng, Y.S.; Meyers, G.; Massad, C.; Price, C.; Abraham, C.; Motaghedi, R.; Buckner, J.H.; et al. The PTPN22 allele encoding an R620W variant interferes with the removal of developing autoreactive B cells in humans. J. Clin. Investig. 2011, 121, 3635–3644. [Google Scholar] [CrossRef] [PubMed]
- Soto, M.E.; Montufar-Robles, I.; Jiménez-Morales, S.; Gamboa, R.; Huesca-Gómez, C.; Ramírez-Bello, J. An association study in PTPN22 suggests that is a risk factor to Takayasu’s arteritis. Inflamm. Res. 2019, 68, 195–201. [Google Scholar] [CrossRef]
- Metzler, G.; Dai, X.; Thouvenel, C.D.; Khim, S.; Habib, T.; Buckner, J.H.; Rawlings, D.J. The Autoimmune Risk Variant PTPN22 C1858T Alters B Cell Tolerance at Discrete Checkpoints and Differentially Shapes the Naive Repertoire. J. Immunol. 2017, 199, 2249–2260. [Google Scholar] [CrossRef] [PubMed]
- Rawlings, D.J.; Schwartz, M.A.; Jackson, S.W.; Meyer-Bahlburg, A. Integration of B cell responses through Toll-like receptors and antigen receptors. Nat. Rev. Immunol. 2012, 12, 282–294. [Google Scholar] [CrossRef]
- Fillatreau, S.; Manfroi, B.; Dörner, T. Toll-like receptor signalling in B cells during systemic lupus erythematosus. Nat. Rev. Rheumatol. 2021, 17, 98–108. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; Huang, B.; Li, J.; Tian, X.; Zeng, X. Identification of the Association Between Toll-Like Receptors and T-Cell Activation in Takayasu’s Arteritis. Front. Immunol. 2021, 12, 792901. [Google Scholar] [CrossRef] [PubMed]
- Kabeerdoss, J.; Goel, R.; Mohan, H.; Danda, D. High expression of pro-inflammatory cytokine genes IL-1β and IL-1R2 upon TLR4 activation in Takayasu arteritis. Rheumatol. Int. 2022, 42, 535–543. [Google Scholar] [CrossRef]
- Kawabe, T.; Naka, T.; Yoshida, K.; Tanaka, T.; Fujiwara, H.; Suematsu, S.; Yoshida, N.; Kishimoto, T.; Kikutani, H. The immune responses in CD40-deficient mice: Impaired immunoglobulin class switching and germinal center formation. Immunity 1994, 1, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Armitage, R.J.; Fanslow, W.C.; Strockbine, L.; Sato, T.A.; Clifford, K.N.; Macduff, B.M.; Anderson, D.M.; Gimpel, S.D.; Davis-Smith, T.; Maliszewski, C.R.; et al. Molecular and biological characterization of a murine ligand for CD40. Nature 1992, 357, 80–82. [Google Scholar] [CrossRef] [PubMed]
- Ramanujam, M.; Steffgen, J.; Visvanathan, S.; Mohan, C.; Fine, J.S.; Putterman, C. Phoenix from the flames: Rediscovering the role of the CD40-CD40L pathway in systemic lupus erythematosus and lupus nephritis. Autoimmun. Rev. 2020, 19, 102668. [Google Scholar] [CrossRef] [PubMed]
- Karnell, J.L.; Rieder, S.A.; Ettinger, R.; Kolbeck, R. Targeting the CD40-CD40L pathway in autoimmune diseases: Humoral immunity and beyond. Adv. Drug Deliv. Rev. 2019, 141, 92–103. [Google Scholar] [CrossRef] [PubMed]
- Seko, Y.; Takahashi, N.; Tada, Y.; Yagita, H.; Okumura, K.; Nagai, R. Restricted usage of T-cell receptor Vgamma-Vdelta genes and expression of costimulatory molecules in Takayasu’s arteritis. Int. J. Cardiol. 2000, 75 (Suppl. S1), S77–S83; discussion S85–S87. [Google Scholar] [CrossRef]
- Tian, Y.; Li, J.; Tian, X.; Zeng, X. Using the co-expression network of T cell-activation-related genes to assess the disease activity in Takayasu’s arteritis patients. Arthritis Res. Ther. 2021, 23, 303. [Google Scholar] [CrossRef] [PubMed]
- Krill, K.T.; Csencsits-Smith, K.; Wood, S.C.; Faust, S.; Lu, G.; Bishop, D.K. Glucocorticoid-induced TNFR-related protein stimulation reverses cardiac allograft acceptance induced by CD40-CD40L blockade. Clin. Dev. Immunol. 2013, 2013, 986859. [Google Scholar] [CrossRef] [PubMed]
- Mackay, F.; Schneider, P. Cracking the BAFF code. Nat. Rev. Immunol. 2009, 9, 491–502. [Google Scholar] [CrossRef] [PubMed]
- Ferraccioli, G.; Gremese, E. B cell activating factor (BAFF) and BAFF receptors: Fakes and facts. Clin. Exp. Immunol. 2017, 190, 291–292. [Google Scholar] [CrossRef] [PubMed]
- Thien, M.; Phan, T.G.; Gardam, S.; Amesbury, M.; Basten, A.; Mackay, F.; Brink, R. Excess BAFF rescues self-reactive B cells from peripheral deletion and allows them to enter forbidden follicular and marginal zone niches. Immunity 2004, 20, 785–798. [Google Scholar] [CrossRef] [PubMed]
- Zanwar, A.; Jain, A.; Gupta, L.; Chaurasia, S.; Kumar, S.; Misra, D.P.; Misra, R. Serum BAFF and APRIL levels in Indian patients with Takayasu arteritis. Clin. Rheumatol. 2018, 37, 3439–3442. [Google Scholar] [CrossRef] [PubMed]
- Eslami, M.; Schneider, P. Function, occurrence and inhibition of different forms of BAFF. Curr. Opin. Immunol. 2021, 71, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Michailidou, D.; Duvvuri, B.; Kuley, R.; Cuthbertson, D.; Grayson, P.C.; Khalidi, N.A.; Koening, C.L.; Langford, C.A.; McAlear, C.A.; Moreland, L.W.; et al. Neutrophil activation in patients with anti-neutrophil cytoplasmic autoantibody-associated vasculitis and large-vessel vasculitis. Arthritis Res. Ther. 2022, 24, 160. [Google Scholar] [CrossRef] [PubMed]
- Michailidou, D.; Kuley, R.; Wang, T.; Hermanson, P.; Grayson, P.C.; Cuthbertson, D.; Khalidi, N.A.; Koening, C.L.; Langford, C.A.; McAlear, C.A.; et al. Neutrophil extracellular trap formation in anti-neutrophil cytoplasmic antibody-associated and large-vessel vasculitis. Clin. Immunol. 2023, 249, 109274. [Google Scholar] [CrossRef]
- Scapini, P.; Bazzoni, F.; Cassatella, M.A. Regulation of B-cell-activating factor (BAFF)/B lymphocyte stimulator (BLyS) expression in human neutrophils. Immunol. Lett. 2008, 116, 1–6. [Google Scholar] [CrossRef]
- Savioli, B.; Abdulahad, W.H.; Brouwer, E.; Kallenberg, C.G.M.; de Souza, A.W.S. Are cytokines and chemokines suitable biomarkers for Takayasu arteritis? Autoimmun. Rev. 2017, 16, 1071–1078. [Google Scholar] [CrossRef] [PubMed]
- Dong, C. Cytokine Regulation and Function in T Cells. Annu. Rev. Immunol. 2021, 39, 51–76. [Google Scholar] [CrossRef]
- Saadoun, D.; Garrido, M.; Comarmond, C.; Desbois, A.C.; Domont, F.; Savey, L.; Terrier, B.; Geri, G.; Rosenzwajg, M.; Klatzmann, D.; et al. Th1 and Th17 cytokines drive inflammation in Takayasu arteritis. Arthritis Rheumatol. 2015, 67, 1353–1360. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, K.; Suzuki, K.; Yoshimoto, K.; Seki, N.; Tsujimoto, H.; Chiba, K.; Takeuchi, T. Significant association between clinical characteristics and changes in peripheral immuno-phenotype in large vessel vasculitis. Arthritis Res. Ther. 2019, 21, 304. [Google Scholar] [CrossRef] [PubMed]
- Domeier, P.P.; Chodisetti, S.B.; Soni, C.; Schell, S.L.; Elias, M.J.; Wong, E.B.; Cooper, T.K.; Kitamura, D.; Rahman, Z.S. IFN-γ receptor and STAT1 signaling in B cells are central to spontaneous germinal center formation and autoimmunity. J. Exp. Med. 2016, 213, 715–732. [Google Scholar] [CrossRef]
- Singh, K.; Rathore, U.; Rai, M.K.; Behera, M.R.; Jain, N.; Ora, M.; Bhadauria, D.; Sharma, S.; Pande, G.; Gambhir, S.; et al. Novel Th17 Lymphocyte Populations, Th17.1 and PD1+Th17, are Increased in Takayasu Arteritis, and Both Th17 and Th17.1 Sub-Populations Associate with Active Disease. J. Inflamm. Res. 2022, 15, 1521–1541. [Google Scholar] [CrossRef]
- Park, M.C.; Lee, S.W.; Park, Y.B.; Lee, S.K. Serum cytokine profiles and their correlations with disease activity in Takayasu’s arteritis. Rheumatology 2006, 45, 545–548. [Google Scholar] [CrossRef]
- Kong, X.; Sun, Y.; Ma, L.; Chen, H.; Wei, L.; Wu, W.; Ji, Z.; Ma, L.; Zhang, Z.; Zhang, Z.; et al. The critical role of IL-6 in the pathogenesis of Takayasu arteritis. Clin. Exp. Rheumatol. 2016, 34 (Suppl. S97), S21–S27. [Google Scholar]
- Tripathy, N.K.; Chauhan, S.K.; Nityanand, S. Cytokine mRNA repertoire of peripheral blood mononuclear cells in Takayasu’s arteritis. Clin. Exp. Immunol. 2004, 138, 369–374. [Google Scholar] [CrossRef]
- Goel, R.; Kabeerdoss, J.; Ram, B.; Prakash, J.A.; Babji, S.; Nair, A.; Jeyaseelan, L.; Jeyaseelan, V.; Mathew, J.; Balaji, V.; et al. Serum Cytokine Profile in Asian Indian Patients with Takayasu Arteritis and its Association with Disease Activity. Open Rheumatol. J. 2017, 11, 23–29. [Google Scholar] [CrossRef]
- Savioli, B.; Salu, B.R.; de Brito, M.V.; Vilela Oliva, M.L.; de Souza, A.W.S. Silent arterial inflammation during the apparent remission state of Takayasu’s arteritis. What do cytokines tell us? Clin. Exp. Rheumatol. 2018, 36 (Suppl. S111), 33–39. [Google Scholar] [PubMed]
- Misra, D.P.; Chaurasia, S.; Misra, R. Increased Circulating Th17 Cells, Serum IL-17A, and IL-23 in Takayasu Arteritis. Autoimmune Dis. 2016, 2016, 7841718. [Google Scholar] [CrossRef] [PubMed]
- Gao, N.; Cui, W.; Zhao, L.M.; Li, T.T.; Zhang, J.H.; Pan, L.L. Contribution of Th2-like Treg cells to the pathogenesis of Takayasu’s arteritis. Clin. Exp. Rheumatol. 2020, 38 (Suppl. S124), 48–54. [Google Scholar] [PubMed]
- Jia, W.; Fu, Z.L.; Wang, X.; Luo, J.; Yan, C.L.; Cao, J.P.; Yan, L.; Xie, J.F.; Liu, G.Y.; Gao, C.; et al. Decreased Absolute Number of Circulating Regulatory T Cells in Patients with Takayasu’s Arteritis. Front. Immunol. 2021, 12, 768244. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, K.G.; Dawson, N.A.J.; Huang, Q.; Dunne, J.V.; Levings, M.K.; Broady, R. Regulatory T cells produce profibrotic cytokines in the skin of patients with systemic sclerosis. J. Allergy Clin. Immunol. 2015, 135, 946–955.e9. [Google Scholar] [CrossRef] [PubMed]
- Saigusa, R.; Asano, Y.; Taniguchi, T.; Hirabayashi, M.; Nakamura, K.; Miura, S.; Yamashita, T.; Takahashi, T.; Ichimura, Y.; Toyama, T.; et al. Fli1-haploinsufficient dermal fibroblasts promote skin-localized transdifferentiation of Th2-like regulatory T cells. Arthritis Res. Ther. 2018, 20, 23. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Yang, W.; Gupta, S.; Biswas, P.; Smith, P.; Bhagat, G.; Pernis, A.B. IRF-4-binding protein inhibits interleukin-17 and interleukin-21 production by controlling the activity of IRF-4 transcription factor. Immunity 2008, 29, 899–911. [Google Scholar] [CrossRef] [PubMed]
- Alibaz-Oner, F.; Yentür, S.P.; Saruhan-Direskeneli, G.; Direskeneli, H. Serum cytokine profiles in Takayasu’s arteritis: Search for biomarkers. Clin. Exp. Rheumatol. 2015, 33 (Suppl. S89), S-32–S-35. [Google Scholar]
- McGeachy, M.J.; Cua, D.J.; Gaffen, S.L. The IL-17 Family of Cytokines in Health and Disease. Immunity 2019, 50, 892–906. [Google Scholar] [CrossRef]
- Danda, D.; Goel, R.; Danda, S.; Mohan, H.; Joseph, G.; Kabeerdoss, J.; Nath, S.K. Interleukin-17F and interleukin-6 gene polymorphisms in Asian Indian patients with Takayasu arteritis. Hum. Immunol. 2017, 78, 515–520. [Google Scholar] [CrossRef]
- Fukui, S.; Iwamoto, N.; Shimizu, T.; Umeda, M.; Nishino, A.; Koga, T.; Kawashiri, S.Y.; Ichinose, K.; Hirai, Y.; Tamai, M.; et al. Fewer subsequent relapses and lower levels of IL-17 in Takayasu arteritis developed after the age of 40 years. Arthritis Res. Ther. 2016, 18, 293. [Google Scholar] [CrossRef]
- Kim, H.O.; Kim, H.S.; Youn, J.C.; Shin, E.C.; Park, S. Serum cytokine profiles in healthy young and elderly population assessed using multiplexed bead-based immunoassays. J. Transl. Med. 2011, 9, 113. [Google Scholar] [CrossRef] [PubMed]
- Potekhina, A.V.; Pylaeva, E.; Provatorov, S.; Ruleva, N.; Masenko, V.; Noeva, E.; Krasnikova, T.; Arefieva, T. Treg/Th17 balance in stable CAD patients with different stages of coronary atherosclerosis. Atherosclerosis 2015, 238, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Saruhan-Direskeneli, G.; Biçakçigil, M.; Yilmaz, V.; Kamali, S.; Aksu, K.; Fresko, I.; Akkoç, N.; Kiraz, S.; Ozer, H.T.; Tunç, E.; et al. Interleukin (IL)-12, IL-2, and IL-6 gene polymorphisms in Takayasu’s arteritis from Turkey. Hum. Immunol. 2006, 67, 735–740. [Google Scholar] [CrossRef] [PubMed]
- Saruhan-Direskeneli, G.; Hughes, T.; Aksu, K.; Keser, G.; Coit, P.; Aydin, S.Z.; Alibaz-Oner, F.; Kamalı, S.; Inanc, M.; Carette, S.; et al. Identification of multiple genetic susceptibility loci in Takayasu arteritis. Am. J. Hum. Genet. 2013, 93, 298–305. [Google Scholar] [CrossRef] [PubMed]
- Lai, Y.; Dong, C. Therapeutic antibodies that target inflammatory cytokines in autoimmune diseases. Int. Immunol. 2016, 28, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Deng, J.; Younge, B.R.; Olshen, R.A.; Goronzy, J.J.; Weyand, C.M. Th17 and Th1 T-cell responses in giant cell arteritis. Circulation 2010, 121, 906–915. [Google Scholar] [CrossRef] [PubMed]
- Weyand, C.M.; Younge, B.R.; Goronzy, J.J. IFN-γ and IL-17: The two faces of T-cell pathology in giant cell arteritis. Curr. Opin. Rheumatol. 2011, 23, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Deng, J.; Ma-Krupa, W.; Gewirtz, A.T.; Younge, B.R.; Goronzy, J.J.; Weyand, C.M. Toll-like receptors 4 and 5 induce distinct types of vasculitis. Circ. Res. 2009, 104, 488–495. [Google Scholar] [CrossRef]
- Maz, M.; Chung, S.A.; Abril, A.; Langford, C.A.; Gorelik, M.; Guyatt, G.; Archer, A.M.; Conn, D.L.; Full, K.A.; Grayson, P.C.; et al. 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Giant Cell Arteritis and Takayasu Arteritis. Arthritis Rheumatol. 2021, 73, 1349–1365. [Google Scholar] [CrossRef]
- Régnier, P.; Le Joncour, A.; Maciejewski-Duval, A.; Desbois, A.C.; Comarmond, C.; Rosenzwajg, M.; Klatzmann, D.; Cacoub, P.; Saadoun, D. Targeting JAK/STAT pathway in Takayasu’s arteritis. Ann. Rheum. Dis. 2020, 79, 951–959. [Google Scholar] [CrossRef] [PubMed]
- Tian, X.; Li, M.; Jiang, N.; Zhao, Y.; Li, J.; Zhou, Y.; Wang, Y.; Wang, Y.; Li, T.; Yang, Y.; et al. Comparative Efficacy of Secukinumab Versus Tumor Necrosis Factor Inhibitors for the Treatment of Takayasu Arteritis. Arthritis Rheumatol. 2023, 75, 1415–1423. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.H.; Rott, L.S.; Clark-Lewis, I.; Campbell, D.J.; Wu, L.; Butcher, E.C. Subspecialization of CXCR5+ T cells: B helper activity is focused in a germinal center-localized subset of CXCR5+ T cells. J. Exp. Med. 2001, 193, 1373–1381. [Google Scholar] [CrossRef]
- Ueno, H.; Banchereau, J.; Vinuesa, C.G. Pathophysiology of T follicular helper cells in humans and mice. Nat. Immunol. 2015, 16, 142–152. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J. T Helper Cell Differentiation, Heterogeneity, and Plasticity. Cold Spring Harb. Perspect. Biol. 2018, 10, a030338. [Google Scholar] [CrossRef] [PubMed]
- Vinuesa, C.G.; Cook, M.C.; Angelucci, C.; Athanasopoulos, V.; Rui, L.; Hill, K.M.; Yu, D.; Domaschenz, H.; Whittle, B.; Lambe, T.; et al. A RING-type ubiquitin ligase family member required to repress follicular helper T cells and autoimmunity. Nature 2005, 435, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Linterman, M.A.; Rigby, R.J.; Wong, R.; Silva, D.; Withers, D.; Anderson, G.; Verma, N.K.; Brink, R.; Hutloff, A.; Goodnow, C.C.; et al. Roquin differentiates the specialized functions of duplicated T cell costimulatory receptor genes CD28 and ICOS. Immunity 2009, 30, 228–241. [Google Scholar] [CrossRef] [PubMed]
- Morita, R.; Schmitt, N.; Bentebibel, S.E.; Ranganathan, R.; Bourdery, L.; Zurawski, G.; Foucat, E.; Dullaers, M.; Oh, S.; Sabzghabaei, N.; et al. Human blood CXCR5(+)CD4(+) T cells are counterparts of T follicular cells and contain specific subsets that differentially support antibody secretion. Immunity 2011, 34, 108–121. [Google Scholar] [CrossRef] [PubMed]
- Hirota, K.; Turner, J.E.; Villa, M.; Duarte, J.H.; Demengeot, J.; Steinmetz, O.M.; Stockinger, B. Plasticity of Th17 cells in Peyer’s patches is responsible for the induction of T cell-dependent IgA responses. Nat. Immunol. 2013, 14, 372–379. [Google Scholar] [CrossRef]
- Tuzlak, S.; Dejean, A.S.; Iannacone, M.; Quintana, F.J.; Waisman, A.; Ginhoux, F.; Korn, T.; Becher, B. Repositioning T(H) cell polarization from single cytokines to complex help. Nat. Immunol. 2021, 22, 1210–1217. [Google Scholar] [CrossRef]
- Ramesh, R.; Kozhaya, L.; McKevitt, K.; Djuretic, I.M.; Carlson, T.J.; Quintero, M.A.; McCauley, J.L.; Abreu, M.T.; Unutmaz, D.; Sundrud, M.S. Pro-inflammatory human Th17 cells selectively express P-glycoprotein and are refractory to glucocorticoids. J. Exp. Med. 2014, 211, 89–104. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, K.; Saito, K.; Tsujimura, S.; Nakayamada, S.; Yamaoka, K.; Sawamukai, N.; Iwata, S.; Nawata, M.; Nakano, K.; Tanaka, Y. Tacrolimus, a calcineurin inhibitor, overcomes treatment unresponsiveness mediated by P-glycoprotein on lymphocytes in refractory rheumatoid arthritis. J. Rheumatol. 2010, 37, 512–520. [Google Scholar] [CrossRef] [PubMed]
- Crotty, S. A brief history of T cell help to B cells. Nat. Rev. Immunol. 2015, 15, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Ernst, D.; Greer, M.; Stoll, M.; Meyer-Olson, D.; Schmidt, R.E.; Witte, T. Remission achieved in refractory advanced takayasu arteritis using rituximab. Case Rep. Rheumatol. 2012, 2012, 406963. [Google Scholar] [CrossRef][Green Version]
- Walters, H.M.; Aguiar, C.L.; Macdermott, E.J.; Adams, A.; Barinstein, L.; Dayton, J.D.; Salvatore, C.; Thimmappa, N.; Lehman, T.J. Takayasu arteritis presenting in the context of active tuberculosis: A pediatric case. J. Clin. Rheumatol. Pract. Rep. Rheum. Musculoskelet. Dis. 2013, 19, 344–347. [Google Scholar] [CrossRef] [PubMed]
- O‘Connor, M.B.; O‘Donovan, N.; Bond, U.; Phelan, M.J. Successful treatment of Takayasu arteritis with rituximab as a first-line immunosuppressant. BMJ Case Rep. 2017, 2017, bcr2016217313. [Google Scholar] [CrossRef] [PubMed]
- Pazzola, G.; Muratore, F.; Pipitone, N.; Crescentini, F.; Cacoub, P.; Boiardi, L.; Spaggiari, L.; Comarmond, C.; Croci, S.; Saadoun, D.; et al. Rituximab therapy for Takayasu arteritis: A seven patients experience and a review of the literature. Rheumatology 2018, 57, 1151–1155. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Ahn, S.J.; Lee, H.S.; Lee, W.J.; Moon, J.; Park, J.K.; Chu, K. Direct brain involvement of Takayasu arteritis treated with rituximab and infliximab: A case report. Encephalitis 2022, 2, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Galarza, C.; Valencia, D.; Tobón, G.J.; Zurita, L.; Mantilla, R.D.; Pineda-Tamayo, R.; Rojas-Villarraga, A.; Rueda, J.C.; Anaya, J.M. Should rituximab be considered as the first-choice treatment for severe autoimmune rheumatic diseases? Clin. Rev. Allergy Immunol. 2008, 34, 124–128. [Google Scholar] [CrossRef]
- Ahmed, M.; Mansoor, S.; Assad, S.; Khan, S.Y.; Khan, R.; Ghani, U.; Mansoor, T.; Rehman, A. Refractory Case of Takayasu Arteritis in a Young Woman: A Clinical Challenge. Cureus 2016, 8, e872. [Google Scholar] [CrossRef]
- Nakagomi, D.; Kronbichler, A.; Witte, T.; Mohammad, A.J.; Jayne, D.R.W. Comment on: Rituximab therapy for Takayasu arteritis: A seven patients experience and a review of the literature. Rheumatology 2018, 57, 1309–1310. [Google Scholar] [CrossRef]
- Mutoh, T.; Ishii, T.; Shirai, T.; Akita, K.; Kamogawa, Y.; Fujita, Y.; Sato, H.; Shirota, Y.; Fujii, H.; Harigae, H. Refractory Takayasu arteritis successfully treated with rituximab: Case-based review. Rheumatol. Int. 2019, 39, 1989–1994. [Google Scholar] [CrossRef] [PubMed]
- Campochiaro, C.; Tomelleri, A.; Sartorelli, S.; Cavalli, G.; De Luca, G.; Baldissera, E.; Dagna, L. Drug retention and discontinuation reasons between seven biologics in patients with Takayasu arteritis. Semin. Arthritis Rheum. 2020, 50, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.A.; Jenkins, B.J. Recent insights into targeting the IL-6 cytokine family in inflammatory diseases and cancer. Nat. Rev. Immunol. 2018, 18, 773–789. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.S.; Deenick, E.K.; Batten, M.; Tangye, S.G. The origins, function, and regulation of T follicular helper cells. J. Exp. Med. 2012, 209, 1241–1253. [Google Scholar] [CrossRef]
- Arkatkar, T.; Du, S.W.; Jacobs, H.M.; Dam, E.M.; Hou, B.; Buckner, J.H.; Rawlings, D.J.; Jackson, S.W. B cell-derived IL-6 initiates spontaneous germinal center formation during systemic autoimmunity. J. Exp. Med. 2017, 214, 3207–3217. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Sun, Y.; Cui, X.; Ji, Z.; Kong, X.; Wu, S.; Huang, Q.; Dai, X.; Zhang, S.; Ma, L.; et al. Autophagy promotes aortic adventitial fibrosis via the IL-6/Jak1 signaling pathway in Takayasu’s arteritis. J. Autoimmun. 2019, 99, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Nakaoka, Y.; Higuchi, K.; Arita, Y.; Otsuki, M.; Yamamoto, K.; Hashimoto-Kataoka, T.; Yasui, T.; Ikeoka, K.; Ohtani, T.; Sakata, Y.; et al. Tocilizumab for the treatment of patients with refractory Takayasu arteritis. Int. Heart J. 2013, 54, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Unizony, S.; Arias-Urdaneta, L.; Miloslavsky, E.; Arvikar, S.; Khosroshahi, A.; Keroack, B.; Stone, J.R.; Stone, J.H. Tocilizumab for the treatment of large-vessel vasculitis (giant cell arteritis, Takayasu arteritis) and polymyalgia rheumatica. Arthritis Care Res. 2012, 64, 1720–1729. [Google Scholar] [CrossRef]
- Tombetti, E.; Franchini, S.; Papa, M.; Sabbadini, M.G.; Baldissera, E. Treatment of refractory Takayasu arteritis with tocilizumab: 7 Italian patients from a single referral center. J. Rheumatol. 2013, 40, 2047–2051. [Google Scholar] [CrossRef]
- Abisror, N.; Mekinian, A.; Lavigne, C.; Vandenhende, M.A.; Soussan, M.; Fain, O. Tocilizumab in refractory Takayasu arteritis: A case series and updated literature review. Autoimmun. Rev. 2013, 12, 1143–1149. [Google Scholar] [CrossRef] [PubMed]
- Goel, R.; Danda, D.; Kumar, S.; Joseph, G. Rapid control of disease activity by tocilizumab in 10 ‘difficult-to-treat’ cases of Takayasu arteritis. Int. J. Rheum. Dis. 2013, 16, 754–761. [Google Scholar] [CrossRef]
- Salvarani, C.; Magnani, L.; Catanoso, M.G.; Pipitone, N.; Versari, A.; Dardani, L.; Pulsatelli, L.; Meliconi, R.; Boiardi, L. Rescue treatment with tocilizumab for Takayasu arteritis resistant to TNF-α blockers. Clin. Exp. Rheumatol. 2012, 30 (Suppl. S70), S90–S93. [Google Scholar]
- Kang, L.; Liu, Y.; Luo, Z.; Zhou, Y.; Chen, B.; Yin, G.; Xie, Q. Systematic review and meta-analysis of the current literature on tocilizumab in patients with refractory Takayasu arteritis. Front. Immunol. 2023, 14, 1084558. [Google Scholar] [CrossRef]
- Misra, D.P.; Singh, K.; Rathore, U.; Patro, P.; Tomelleri, A.; Campochiaro, C.; Agarwal, V.; Sharma, A. The effectiveness of tocilizumab and its comparison with tumor necrosis factor alpha inhibitors for Takayasu Arteritis: A systematic review and meta-analysis. Autoimmun. Rev. 2023, 22, 103275. [Google Scholar] [CrossRef] [PubMed]
- Nakaoka, Y.; Isobe, M.; Takei, S.; Tanaka, Y.; Ishii, T.; Yokota, S.; Nomura, A.; Yoshida, S.; Nishimoto, N. Efficacy and safety of tocilizumab in patients with refractory Takayasu arteritis: Results from a randomised, double-blind, placebo-controlled, phase 3 trial in Japan (the TAKT study). Ann. Rheum. Dis. 2018, 77, 348–354. [Google Scholar] [CrossRef]
- Nakaoka, Y.; Isobe, M.; Tanaka, Y.; Ishii, T.; Ooka, S.; Niiro, H.; Tamura, N.; Banno, S.; Yoshifuji, H.; Sakata, Y.; et al. Long-term efficacy and safety of tocilizumab in refractory Takayasu arteritis: Final results of the randomized controlled phase 3 TAKT study. Rheumatology 2020, 59, 2427–2434. [Google Scholar] [CrossRef]
- Nakaoka, Y.; Yanagawa, M.; Hata, A.; Yamashita, K.; Okada, N.; Yamakido, S.; Hayashi, H.; Jayne, D. Vascular imaging of patients with refractory Takayasu arteritis treated with tocilizumab: Post hoc analysis of a randomized controlled trial. Rheumatology 2022, 61, 2360–2368. [Google Scholar] [CrossRef] [PubMed]
- Kong, X.; Sun, Y.; Dai, X.; Wang, L.; Ji, Z.; Chen, H.; Jin, X.; Ma, L.; Jiang, L. Treatment efficacy and safety of tofacitinib versus methotrexate in Takayasu arteritis: A prospective observational study. Ann. Rheum. Dis. 2022, 81, 117–123. [Google Scholar] [CrossRef]
- Wang, J.; Dai, X.; Ma, L.; Wu, S.; Jin, X.; Ji, Z.; Chen, H.; Ma, L.; Ding, Z.; Jiang, L.; et al. Efficacy and safety of tofacitinib versus leflunomide with glucocorticoids treatment in Takayasu arteritis: A prospective study. Semin. Arthritis Rheum. 2022, 55, 152018. [Google Scholar] [CrossRef]
- Burmester, G.R.; Lin, Y.; Patel, R.; van Adelsberg, J.; Mangan, E.K.; Graham, N.M.; van Hoogstraten, H.; Bauer, D.; Ignacio Vargas, J.; Lee, E.B. Efficacy and safety of sarilumab monotherapy versus adalimumab monotherapy for the treatment of patients with active rheumatoid arthritis (MONARCH): A randomised, double-blind, parallel-group phase III trial. Ann. Rheum. Dis. 2017, 76, 840–847. [Google Scholar] [CrossRef] [PubMed]
- Boyapati, A.; Msihid, J.; Fiore, S.; van Adelsberg, J.; Graham, N.M.; Hamilton, J.D. Sarilumab plus methotrexate suppresses circulating biomarkers of bone resorption and synovial damage in patients with rheumatoid arthritis and inadequate response to methotrexate: A biomarker study of MOBILITY. Arthritis Res. Ther. 2016, 18, 225. [Google Scholar] [CrossRef] [PubMed]
- Taylor, P.C.; Schiff, M.H.; Wang, Q.; Jiang, Y.; Zhuang, Y.; Kurrasch, R.; Daga, S.; Rao, R.; Tak, P.P.; Hsu, B. Efficacy and safety of monotherapy with sirukumab compared with adalimumab monotherapy in biologic-naïve patients with active rheumatoid arthritis (SIRROUND-H): A randomised, double-blind, parallel-group, multinational, 52-week, phase 3 study. Ann. Rheum. Dis. 2018, 77, 658–666. [Google Scholar] [CrossRef] [PubMed]
- Genovese, M.C.; Fleischmann, R.; Furst, D.; Janssen, N.; Carter, J.; Dasgupta, B.; Bryson, J.; Duncan, B.; Zhu, W.; Pitzalis, C.; et al. Efficacy and safety of olokizumab in patients with rheumatoid arthritis with an inadequate response to TNF inhibitor therapy: Outcomes of a randomised Phase IIb study. Ann. Rheum. Dis. 2014, 73, 1607–1615. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, D.M.; Bonelli, M.; Gadina, M.; O‘Shea, J.J. Type I/II cytokines, JAKs, and new strategies for treating autoimmune diseases. Nat. Rev. Rheumatol. 2016, 12, 25–36. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Li, M.; Tian, X.; Zeng, X. Tofacitinib in patients with refractory Takayasu’s arteritis. Rheumatology 2020, 59, e95–e98. [Google Scholar] [CrossRef] [PubMed]
- Sato, S.; Matsumoto, H.; Temmoku, J.; Fujita, Y.; Matsuoka, N.; Furuya, M.; Gunji, N.; Fujiwara, T.; Asano, T.; Onizawa, M.; et al. A case of Takayasu arteritis complicated by refractory ulcerative colitis successfully treated with tofacitinib. Rheumatology 2020, 59, 1773–1775. [Google Scholar] [CrossRef] [PubMed]
- Sy, A.; Khalidi, N.; Dehghan, N.; Barra, L.; Carette, S.; Cuthbertson, D.; Hoffman, G.S.; Koening, C.L.; Langford, C.A.; McAlear, C.; et al. Vasculitis in patients with inflammatory bowel diseases: A study of 32 patients and systematic review of the literature. Semin. Arthritis Rheum. 2016, 45, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Terao, C.; Matsumura, T.; Yoshifuji, H.; Kirino, Y.; Maejima, Y.; Nakaoka, Y.; Takahashi, M.; Amiya, E.; Tamura, N.; Nakajima, T.; et al. Takayasu arteritis and ulcerative colitis: High rate of co-occurrence and genetic overlap. Arthritis Rheumatol. 2015, 67, 2226–2232. [Google Scholar] [CrossRef]
- Lee, J.C.; Cevallos, A.M.; Naeem, A.; Lennard-Jones, J.E.; Farthing, M.J. Detection of anti-colon antibodies in inflammatory bowel disease using human cultured colonic cells. Gut 1999, 44, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.R.; Tsai, Y.S.; Liu, Y.W.; Li, Y.H. Extended-release tofacitinib improves refractory Takayasu’s arteritis. Scand. J. Rheumatol. 2022, 51, 72–75. [Google Scholar] [CrossRef] [PubMed]
- Kuwabara, S.; Tanimura, S.; Matsumoto, S.; Nakamura, H.; Horita, T. Successful remission with tofacitinib in a patient with refractory Takayasu arteritis complicated by ulcerative colitis. Ann. Rheum. Dis. 2020, 79, 1125–1126. [Google Scholar] [CrossRef]
- Palermo, A.; Marvisi, C.; Casali, M.; Pipitone, N.; Muratore, F.; Salvarani, C. Tofacitinib for the treatment of refractory Takayasu’s arteritis: Description of 2 cases. Clin. Exp. Rheumatol. 2020, 38 (Suppl. S124), 234–235. [Google Scholar]
- Zhou, Z.; Fang, C.; Wang, L.; Li, J.; Yang, Y.; Zhang, L.; Jin, S.; Zeng, X.; Tian, X. Baricitinib for refractory Takayasu arteritis: A prospective cohort study in a tertiary referral centre. RMD Open 2024, 10, e003985. [Google Scholar] [CrossRef]
- Terao, C.; Yoshifuji, H.; Kimura, A.; Matsumura, T.; Ohmura, K.; Takahashi, M.; Shimizu, M.; Kawaguchi, T.; Chen, Z.; Naruse, T.K.; et al. Two susceptibility loci to Takayasu arteritis reveal a synergistic role of the IL12B and HLA-B regions in a Japanese population. Am. J. Hum. Genet. 2013, 93, 289–297. [Google Scholar] [CrossRef]
- Terao, C.; Yoshifuji, H.; Matsumura, T.; Naruse, T.K.; Ishii, T.; Nakaoka, Y.; Kirino, Y.; Matsuo, K.; Origuchi, T.; Shimizu, M.; et al. Genetic determinants and an epistasis of LILRA3 and HLA-B*52 in Takayasu arteritis. Proc. Natl. Acad. Sci. USA 2018, 115, 13045–13050. [Google Scholar] [CrossRef] [PubMed]
- Kadoba, K.; Watanabe, R.; Iwasaki, T.; Nakajima, T.; Kitagori, K.; Akizuki, S.; Murakami, K.; Nakashima, R.; Hashimoto, M.; Tanaka, M.; et al. A susceptibility locus in the IL12B but not LILRA3 region is associated with vascular damage in Takayasu arteritis. Sci. Rep. 2021, 11, 13667. [Google Scholar] [CrossRef]
- Nakajima, T.; Yoshifuji, H.; Shimizu, M.; Kitagori, K.; Murakami, K.; Nakashima, R.; Imura, Y.; Tanaka, M.; Ohmura, K.; Matsuda, F.; et al. A novel susceptibility locus in the IL12B region is associated with the pathophysiology of Takayasu arteritis through IL-12p40 and IL-12p70 production. Arthritis Res. Ther. 2017, 19, 197. [Google Scholar] [CrossRef] [PubMed]
- Watford, W.T.; Hissong, B.D.; Bream, J.H.; Kanno, Y.; Muul, L.; O’Shea, J.J. Signaling by IL-12 and IL-23 and the immunoregulatory roles of STAT4. Immunol. Rev. 2004, 202, 139–156. [Google Scholar] [CrossRef]
| References | Patient Number | Median Age (Years)/ Gender | Median Disease Duration (Months) | Follow-Up Duration (Months) | Therapies with or after RTX | Unsuccessful Therapies before RTX | Clinical Response | Imaging Response |
|---|---|---|---|---|---|---|---|---|
| [149] | 2 | 27/2 F | 90 | NA | None | MTX (2), TNFi (2) | 1/2 | NA |
| [16] | 3 | 18/3 F | 48 | NA | MMF (2), CYC (1) | MTX (2), TNFi (2), MMF (2), CYC (3), HCQ (1) | 3/3 | 1/1 (NA in 2 cases) |
| [144] | 1 | 25/F | NA | 14 | CYC | AZA, CYC | 1/1 | 1/1 |
| [145] | 1 | 16/F | 3 | ≥3 | MTX | MTX | 1/1 | NA |
| [17] | 2 | 32.5/2 F | NA | 42 (2) | MMF | CYC (2), MTX (1), ADA (1), IFX (2) | 2/2 | 2/2 |
| [150] | 1 | 42/F | NA | ≥6 | NA | AZA, CYC, ETN, TCZ | 0/1 | 0/1 |
| [146] | 1 | 39/F | NA | ≥36 | AZA | None | 1/1 | 1/1 |
| [147] | 7 | 22/1M, 6 F | 24 | 24 | MTX (1), MMF (2) | AZA (2), MTX (5), MMF (2), IFX (2), ADA (2), TCZ (2) | 3/7 | 4/7 |
| [151] | 8 | 38/NA | 66 | 12 | AZA (2), MTX (1) | AZA (6), CYC (4), MTX (4), MMF (3), CYA (1), IFX: (3), ADA (1) | 7/8 | NA |
| [152] | 1 | 34/M | 96 | 36 | MTX | MTX, ABT, TCZ, IFX, ETN | 1/1 | 1/1 |
| [153] | 2 | 34.5/F | 89.1 | NA | MTX (1) | NA | 0/2 | NA |
| [148] | 1 | 39/M | 11 | 26 | TNFi | CYC | 1/1 | 0/1 |
| Treatment (Mechanism of Action) | Study Type | Patient Number | Follow-Up Time (Weeks) | Control | Main Results | References |
|---|---|---|---|---|---|---|
| Tocilizumab (IL-6R inhibitors) | Phase 3 | 36 | ≥16 | Placebo | The results suggested a preference for tocilizumab over placebo concerning the duration until TAK relapse, with no additional safety issues identified, supporting tocilizumab’s effectiveness in managing refractory TAK cases. | [166] |
| Tocilizumab (IL-6R inhibitors) | Phase 3 | 28 | 96 | Placebo | It yielded evidence of steroid-sparing effects and enhancements in overall well-being over extended periods of tocilizumab therapy, with no emergence of safety concerns. | [167] |
| Tocilizumab (IL-6R inhibitors) | Phase 3 | 28 | 96 | Placebo | Following the initiation of tocilizumab treatment, approximately 60% of TAK patients displayed no advancement in vessel wall thickness. Minimal incidences of dilation/aneurysm progression or stenosis/occlusion were observed among the patient cohort. | [168] |
| Tofacitinib (JAK inhibitor) | Phase 4 | 53 | 36 | Methotrexate | Tocilizumab demonstrated superiority over methotrexate in inducing complete remission, displayed a propensity for relapse prevention and facilitate glucocorticoid dose reduction in TAK treatment. The safety of tocilizumab was also confirmed. | [169] |
| Tofacitinib (JAK inhibitor) | Interventional | 67 | 36 | Leflunomide | Tocilizumab and leflunomide were comparable for TAK treatment. Tocilizumab group showed lower side-effect prevalence and higher imaging improvement, as well as a low dose of glucocorticoids to maintain disease remission. | [170] |
| Treatment (Mechanism of Action) | Study Title | Study Type | Current Status | Study Phase | Estimated Completion Date | Clinical Trail Number |
|---|---|---|---|---|---|---|
| Tofacitinib (JAK inhibitor) | Comparison of tofacitinib and prednisolone in the treatment of active Takayasu’s arteritis | Interventional | Recruiting | Phase 3 | July 2025 | NCT05749666 |
| Upadacitinib (JAK inhibitor) | A study to evaluate the efficacy and safety of upadacitinib in participants with Takayasu’s arteritis | Interventional | Recruiting | Phase 3 | August 2027 | NCT04161898 |
| Tocilizumab (IL-6R inhibitors) | Multicentre, randomized, prospective trial evaluating the efficacy and safety of infliximab to tocilizumab in refractory or relapsing Takayasu’s arteritis | Interventional | Recruiting | Phase 2 | September 2023 | NCT04564001 |
| Tocilizumab (IL-6R inhibitors) | A pilot study in severe patients with Takayasu’s arteritis | Interventional | Recruiting | Phase 4 | December 2023 | NCT04300686 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guo, S.; Tian, Y.; Li, J.; Zeng, X. A Glimpse into Humoral Response and Related Therapeutic Approaches of Takayasu’s Arteritis. Int. J. Mol. Sci. 2024, 25, 6528. https://doi.org/10.3390/ijms25126528
Guo S, Tian Y, Li J, Zeng X. A Glimpse into Humoral Response and Related Therapeutic Approaches of Takayasu’s Arteritis. International Journal of Molecular Sciences. 2024; 25(12):6528. https://doi.org/10.3390/ijms25126528
Chicago/Turabian StyleGuo, Shuning, Yixiao Tian, Jing Li, and Xiaofeng Zeng. 2024. "A Glimpse into Humoral Response and Related Therapeutic Approaches of Takayasu’s Arteritis" International Journal of Molecular Sciences 25, no. 12: 6528. https://doi.org/10.3390/ijms25126528
APA StyleGuo, S., Tian, Y., Li, J., & Zeng, X. (2024). A Glimpse into Humoral Response and Related Therapeutic Approaches of Takayasu’s Arteritis. International Journal of Molecular Sciences, 25(12), 6528. https://doi.org/10.3390/ijms25126528








