Abstract
Background and Objectives: Starting in early December 2019, the novel Coronavirus Disease (COVID-19) from infection with COVID-19 has caused a global pandemic. Many aspects of its pathogenesis and related clinical consequences are still unclear. Early diagnosis and dynamic monitoring of prognostic factors are essential to improve the ability to manage COVID-19 infection. This study aimed to provide an account of the role played by vitamins C and D on the onset, progression and severity of COVID-19. Clinical features and infection-related risk factors are also briefly discussed. Material and Methods: In March 2022, the main online databases were accessed. All the articles that investigate the possible role of vitamins C and D on COVID-19 susceptibility, severity and progression were considered. Results: The current evidence on vitamin C and D supplementation in patients with COVID-19 infection is inconsistent and controversial. In some studies, vitamins were used as coadjuvant of a formal experimental therapy, while in others as main treatment. Ethnicity and hospital setting (inpatient/outpatient) were also variable. Moreover, there was no consensus between studies in administration protocol: high heterogeneity in dosage, administration, and duration of the treatment were evident. Finally, some studies administered vitamins pre- and/or during COVID infection, in patients with different risk factors and infection severity. Conclusions: While waiting to develop a targeted, safe and effective therapy, it is important to investigate individual predisposition and proper disease management. Concluding, available data on the use of nutraceuticals in COVID-19 are inconsistent. However, there is a lack of evidence-based guidelines which recommend vitamin C and D supplementation in patients with COVID-19, and results from high quality randomised controlled trials (RCTs) are inconsistent. Current investigations so far are mostly observational, and include a relatively small sample size which can lead to biased results. Large-scale multicentre studies are therefore needed.
1. Introduction
The origins of COVID-19 remain still unclear, with consensus on diagnostic and therapeutic standards [1,2]. In some patients, COVID-19 infection precipitously progresses, and respiratory failure can occur [3]. Therefore, prognostic factors for COVID-19 progression were investigated to provide a basis on which to optimize hospital efforts, further improve patient management and make therapy more effective, hoping to reduce mortality [4,5]. Gender, age, underlying comorbidities (diabetes, hypertension, cardiovascular disease), respiratory rate, temperature, neutrophil and lymphocyte counts, D-dimer, albumin and procalcitonin are all predictors of COVID-19 severity, and therefore can be considered risk factors for admission to intensive care unit (ICU) [6,7,8,9,10,11]. Compared to non-ICU patients, ICU patients had higher plasma levels of IL2, IL7, IL10, GSCF, IP10, MCP1, MIP1A and TNFα [12]. Several risk factors for the progression of COVID-19 pneumonia have been reported, including older age: elderly people are frail, and they are likely to present several comorbidities. These not only increase the risk of pneumonia [13], but also affect prognosis [14]. The assessment of comorbidities is an essential component in determining the prognosis of various diseases, particularly pneumonia [15]. Other risk factors for severity progression are smoking, allergic conditions, asthma, and chronic obstructive pulmonary disease (COPD) [16]. At admission, high fever, dyspnoea, increased C reactive protein, creatinine, and procalcitonin, hypoalbuminemia, leucopoenia, and eosinopenia have been associated with disease progression [17,18,19,20]. Elevated plasmin levels are also common in COVID-19 patients, especially in those with comorbidities [21]. Plasmin or other proteases can increase COVID-19 severity by accelerating the entry, fusion, duplication and release of the virus in respiratory cells. Elevated plasmin could be an independent factor for risk stratification of patients with COVID-19 [22,23]. Therefore, patients presenting with these characteristics need to be monitored more carefully to avoid complications and poor prognosis. COVID-19 pneumonia is characterized by acute onset and rapid progression [24]. Lung damage caused by such infections can progress to acute respiratory distress syndrome (ARDS) [25]. Recently, vitamin C and D supplementation in patients with COVID-19 has gained interest. However, their role in the onset, progression and severity of the disease in COVID-19 is still unclear. Therefore, this systematic review investigated whether vitamin C and D supplementation may play a role in reducing the susceptibility, severity and progression of COVID-19 infection. The hypothesis of the present investigation is that the administration of vitamins C and D in COVID-19 patients might positively impact disease susceptibility, severity and progression.
1.1. The Role of Vitamin D
Vitamin D plays a major role in calcium regulation and bone health [22]. Vitamin D also acts on immune cells, and is generally able to reduce inflammation [26,27]. Vitamin D is a potent epigenetic regulator, affecting more than 2500 genes [28] and playing a role in a variety of diseases, including cancer [29,30], diabetes mellitus [31], acute respiratory tract infections [32] and autoimmune diseases such as multiple sclerosis [33]. According to the World Health Organisation (WHO), the world has recorded more than 140 million cases and more than 3 million deaths related to COVID-19 since its outbreak [34]. Some aspects suggest a potential association between vitamin D and COVID-19 [35]. The first is seasonality, as the infection started in winter in the Northern Hemisphere and mortality rates were lower in the summer, especially in Europe, only to pick up again in September in various European countries: mortality appears to be inversely related to solar ultraviolet-B (UVB) doses and vitamin D production [36,37]. The second is ethnic group: African and Hispanic Americans experienced higher rates of COVID-19 infection and death rates than European Americans [38,39], possibly from darker skin pigmentation and lower concentrations of 25(OH)D [40]. Further aspects are systemic inflammation and immune dysregulation mediated by COVID-19, which are associated with vitamin D on the immune system [41,42]. Vitamin D modulates the innate immune response and has antiviral activity and is therefore recommended to prevent acute respiratory infections [43,44]. Hypovitaminosis D increases the risk of infectious diseases, supported by the hypothesis that seasonal variations in acute respiratory infections could be related to seasonal variations in vitamin D levels [45,46,47,48].
1.2. The Role of Vitamin C
The investigation into the role of vitamin C in the prevention and treatment of pneumonia and sepsis has been ongoing for many decades. This research has laid a solid foundation to transpose the findings to patients with severe COVID-19 [49]. Patients with pneumonia, sepsis and multiple organ failure have low vitamin C status and high oxidative stress [50,51,52]. These critically ill patients have a higher requirement for vitamin C, requiring gram doses to normalize their blood levels [53,54], 20–30 times greater than what is required for the general population. Intravenous administration of vitamin C to patients with pneumonia to normalize plasma levels is an intervention which, as suggested by some studies, is able to reduce the severity (days spent in ICU) and duration (hospital stay) of the disease [55,56,57,58,59,60]. Despite these findings, critically ill patients with sepsis continue to receive milligram amounts of vitamin C, which is insufficient to replenish their vitamin C status [61]. Vitamin C has pleiotropic physiological functions, many of which are relevant to COVID-19. These include antioxidant, anti-inflammatory, antithrombotic and immunomodulatory functions [62]. Many of the functions of vitamin C seem relevant for the cytokine storm, sepsis and ARDS related to COVID-19 [63,64,65,66,67,68].
2. Materials and Methods
2.1. Search Strategy
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the 2020 PRISMA statement [69]. The literature search was conducted following this protocol:
- Patients: COVID-19 infection;
- Comparison: vitamins C and D;
- Outcomes: susceptibility, severity and progression of COVID-19.
2.2. Eligibility Criteria
All the comparative clinical studies which investigated the role of vitamin C and D supplementation or deficiency in COVID-19 susceptibility, severity and progression were considered in the present systematic review. The studies were eligible irrespective of the clinical severity of the infection and/or of the presence and severity of patients’ comorbidities and/or protocol of vitamins administration. Studies level I to IV of evidence, according to the Oxford Centre of Evidence-Based Medicine [70], were considered. Grey literature, abstracts and posters, comments, expert opinion and editorials were not considered in the quantitative analysis. Given the authors’ language capabilities, articles in English, French, German, Italian and Spanish were considered. Disagreements were solved by a third author (N.M.).
2.3. Literature Search
In May 2022, the following databases were accessed: Pubmed, Embase, Scopus and Google Scholar. The following keywords were used for the search using the Boolean operator AND/OR: (coronavirus OR COVID-19 OR SARS-CoV-2 OR SARS-CoV-1 OR pandemic) AND (vitamins OR vitamin C OR vitamin D) AND (administration OR supplementation OR exogenous OR factors OR predictors OR susceptibility OR prognosis OR diagnosis OR role OR therapy) AND (onset OR severity OR progression OR outcome OR sepsis OR pneumonia OR lung OR cytokines OR pneumonia OR pathogenesis OR response OR risk OR death OR mortality OR morbidity OR inflammatory OR nutraceutical OR immune system). The database search was performed without time constrains. If title and abstract matched the topic, the full text was accessed. The bibliographies of the full-text articles were also screened for inclusion.
2.4. Methodology Quality Assessment
The Newcastle–Ottawa Scale (NOS) was used to assess the quality of non-randomized studies. The NOS uses a ‘star’ rating system to judge the quality of studies, and is based on selection, comparability and assessment of outcome. The maximum number of stars a study may receive is nine, attributed as follows: zero to four stars for selection, zero to two stars for comparability and zero to three stars for the outcome. A final score 6 stars indicated a good quality. The Jadad composite scale was used to assess the methodological quality of the clinical trials based on randomization, blinding and withdrawals. The scale ranged from zero to five points. A final score 3 stars indicate low risk of bias.
3. Results
3.1. Search Results
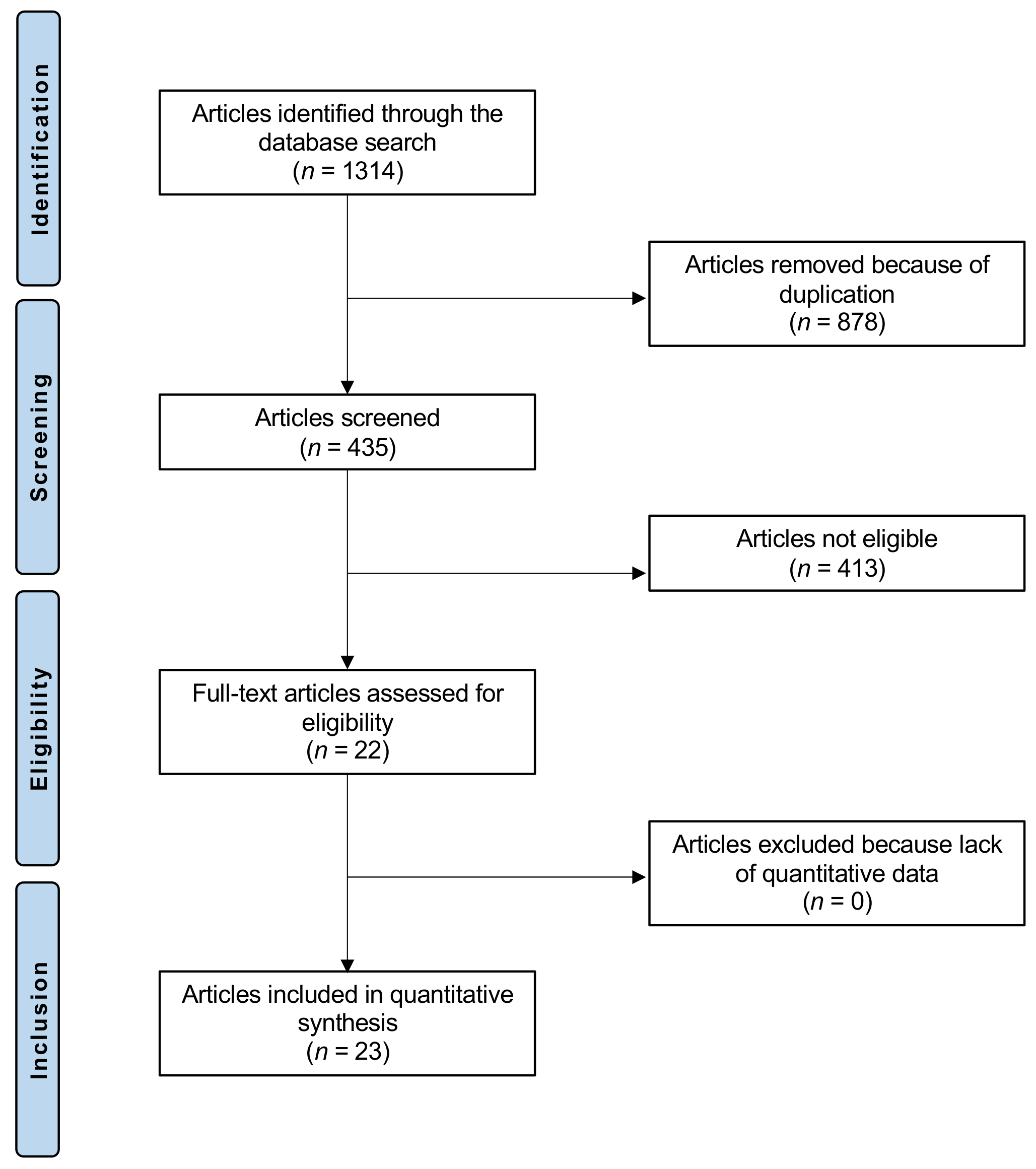
The literature search resulted in 1314 articles. Of them, 878 were excluded, as they were duplicates. A further 413 were excluded with reason: not clinical investigation (n = 174), not focusing on Vitamin D or C (n = 201), not focusing on COVID (n = 30), language limitation (n = 8). This left 23 studies for the present investigation (Figure 1).
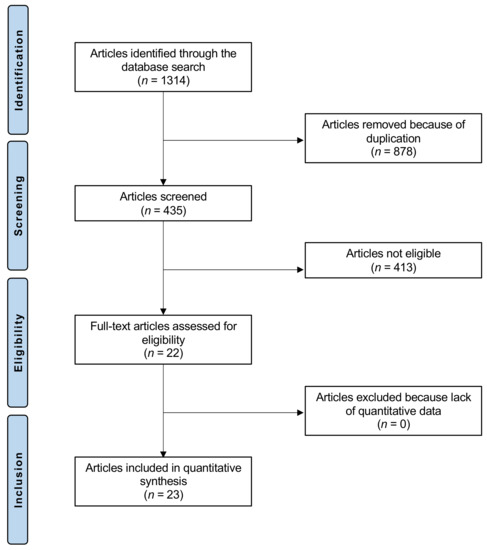
Figure 1.
Flow chart of the literature search.
3.2. Syntheses of Results
Thirteen studies compared Vit D supplementation in patients with COVID (Table 1). Overall, 3443 patients were included: 830 in the treatment group and 2581 in the control group. Men made up 50% (1722 of 3443). The mean age of the patients was 59.6 ± 13.9 years old. Several clinical investigations found that in patients hospitalized with COVID-19, administration of vitamin D was associated with lower in-hospital mortality compared to a control group who did not receive supplementation or received low-dose supplementation [71]. These results were also confirmed in the elderly, along with a reduced severity progression compared to a control group who did not receive the vitamin supplementation [72,73,74,75]. Other studies found that vitamin D supplementation improved oxygenation [76] and reduced the need of ICU in inpatient regimes [77]. On the other hand, other clinical investigations found no difference in the outcome in patients who received Vitamin D supplementation in terms of severity of disease in need of mechanical ventilation, length of hospital stay and in-hospital mortality compared to those who did not [78,79,80,81].

Table 1.
Studies which investigated Vit D implementation in COVID.
Nine studies compared Vit C supplementation in patients with COVID (Table 2). Overall, 1488 patients were included: 605 in the treatment group and 883 in the control group. Men made up 52% (774 of 1488). The mean age of the patients was 59.8 ± 7.4 years old. High-dose vitamin C may reduce the mortality [85] and the rate of thrombosis [86], and improve oxygenation [85,87], in patients with COVID-2019. Other studies did not find benefits for vitamin C in addition to the main treatment regimen in inpatient and outpatient regimes [86,88,89,90,91,92,93], with no impact on mortality, need for mechanical ventilation [89], nor vasopressor requirements or Sequential Organ Failure Assessment (SOFA) scores [90].

Table 2.
Studies which investigated Vit C implementation in COVID.
3.3. Methodological Quality Assessment
The NOS resulted 6 stars in all studies, and the Jadad composite scale 3 in most studies. These results attested to the present study’s good quality concerning the methodological assessment.
The methodological quality assessment of the non-randomized investigations is shown in Table 3 and that of the randomised controlled trials in Table 4.

Table 3.
Newcastle–Ottawa Scale.

Table 4.
Jadad Composite Scale.
4. Discussion
According to the main findings of the present study, our hypothesis that the administration of vitamins C and D in COVID-19 patients impacts positively on disease susceptibility, severity and progression was not supported by the current evidence. The current evidence on vitamin C and D supplementation in patients with COVID-19 infection is heterogeneous. Although most studies focused on the same endpoints, such as infection progression, hospitalisation length, oxygenation, need of ICU and mechanical ventilation, and mortality, the results of these studies are controversial, and no consistent recommendation can be inferred. The current clinical investigations evidenced high variability in eligibility criteria, patient comorbidities and age, and associated therapies. In some studies, vitamins were used as coadjuvant of a formal experimental therapy, while in others as main treatment. Ethnicity and hospital setting (inpatient/outpatient) were also variable. Moreover, there was no consensus between studies in administration protocol: high heterogeneity in dosage, administration and duration of the treatment were evident. Finally, some studies administered vitamins pre- and/or during COVID infection, in patients with different risk factors and infection severity.
The improved metabolism of vitamins in diseases and inflammatory processes may justify vitamin C and D supplementation during sepsis or pneumonia. However, the possibility of decreasing the incidence of viral diseases in a population using dietary supplements of vitamin C and D is not supported by the present published peer reviewed literature. This is in accordance with previous evidence, which concluded that vitamin administration at high doses does not contribute to reducing the severity and progression of COVID-19 [49,94,95]. Among other things, the basal state of vitamin C probably influences the response to its administration. As recently highlighted, most patients who were enrolled in the clinical studies suffered from hypovitaminosis, and such hypovitaminosic patients are more likely to respond to its therapeutic supplementation [49,94,96]. We were unable to identify studies which investigated the efficacy of vitamin C and D supplementation in the prevention of COVID-19 in healthy patients. In this context, the effects of vitamin C and D application are not fully generalisable. While waiting to develop a targeted, safe and effective therapy, it is important to investigate individual predisposition and proper disease management [97]. Available data on the use of nutraceuticals in COVID-19 are inconsistent. Irrespective of COVID-19 infection, vitamins have beneficial properties with practically no side effects. Prevention of malnutrition by providing adequate amounts of macronutrients to maintain energy needs is highly recommended [98]. Integration with micronutrients is equally important to prevent viral infections: low levels of vitamins have been associated with adverse clinical outcomes [99]. Given the good safety profile, low cost, and the potential for rapid increase in their production, the administration of vitamins C and D to patients with infectious diseases may be reasonable. However, there is a lack of evidence-based guidelines which recommend vitamin C and D supplementation in patients with COVID-19, and results from high quality randomised controlled trials (RCTs) are inconsistent. Current investigations so far are mostly observational, and include a relatively small sample size which can lead to biased results. Large-scale multicenter studies are therefore needed. Vitamins participate in a multitude of biochemical pathways which may affect the susceptibility, severity and progression of COVID-19. Higher serum concentrations of 25(OH)D contribute to maintaining intact the epithelial layers, reducing virus replication, modulating pro-inflammatory cytokine and promoting the concentration of free angiotensin-converting enzyme-2 (ACE-2). These effects of vitamin D may explain the positive results obtained in some studies. More research is needed to evaluate the mechanisms by which Vitamin D may reduce the risk of COVID-19. Vitamin C shows relevant mechanisms of action for severe respiratory infections, including antioxidant, anti-inflammatory, antithrombotic and immunomodulatory functions. However, whether low concentrations of either vitamin C or vitamin D were a causative reason or an unrelated collateral effect related to COVID-19 susceptibility, severity and progression remains unclear. Whether exogenous replacement for higher serum levels of vitamins C or D would result in better prevention or better treatment outcomes is debated, and relevant evidence is missing. The results from larger RCTs currently would provide more definitive evidence. Optimization of intervention protocols in future trials, for example, an early and prolonged administration, is justified to ascertain their effectiveness. Concluding, the current available evidence is inconsistent and not exhaustive; therefore, vitamins C and D in COVID-19 patients should be cautiously administered under continuous monitoring.
The hypothesis that vitamin D status may affect the risk of COVID-19 is mainly based on observational studies [100,101,102,103,104,105,106,107,108,109,110,111,112,113,114]. We were unable to identify RCTs which investigated the incidence of COVID-19 in patients underoing vitamin D supplementation. Most studies which have identified inverse correlations between COVID-19 severity and risk of death are retrospective with limied numbers of COVID-19 patients. To date, the United States Observational Study is the largest observational study, reporting data on 191,779 patients with values of vitamin D tested in the previous 12 months [115]. The study reported COVID-19 positivity rates vs vitamin D concentration [115]. The finding that the COVID-19 positivity rate in the United States varied from 6.5% for vitamin D concentrations between 40 and 50 ng/mL, to 11.3% for values of 20 ng/mL, may result from the effect of vitamin D in reducing virus survival and replication by induction of cathelicidin and defensins, as well as by increasing free ACE-2 concentrations, thus preventing COVID-19 from entering cells through the ACE-2 receptor [116]. Regression fit to all data indicates that COVID-19 positivity is 40% lower for 25(OH)D values above 50 ng/mL (Institute of Medicine recommended value [117,118]) compared to values of 20 ng/mL. The higher rates in the northern states were explained by a genetic variation of the original Chinese form of the amino acid D614A of the Spike protein, to the mutated European form D614G [119]. The variation of the Spike amino acid is caused by a nucleotide mutation from A to G in position 23,403 of the Wuhan reference strain. The D614G form has higher transmission capabilities, and was introduced to New York by people returning from Europe. Such genetic alteration possibly explains some of the high COVID-19 positivity rates in these areas. Regarding ethnic differences, social determinants predisposing to COVID-19, such as lower income, reduced education and employment, as well as higher rates of comorbidities might explain why African Americans have higher rates of COVID-19 [120]. These factors may help explain why blacks and Hispanics have COVID-19 positivity rates 7% and 4% higher, respectively, than whites for the same vitamin D (30 ng/mL). However, the positive spread rate of COVID-19 was higher for blacks and Hispanics with 20 ng/mL than for whites with the same value (18%, 16% and 9%, respectively) than for blacks and Hispanics with about 60 ng/mL (11%, 9% and 5%, respectively), suggesting that low vitamin D status plays a role in increasing the rate of COVID-19. A potential limitation of Vitamin D studies is some scientific evidence that acute inflammatory disease lowers the concentration of 25(OH)D [121,122,123,124,125]. Another important factor which might be relevant in COVID-19 infection severity and progression is the interaction of vitamin D and its receptor (vitamin D receptor, VDR), as vitamin D is an important immunomodulator of both innate and adaptive immune responses [126,127]. Some previous investigations concluded that vitamin D supplementation might be effective to modulate COVID-19 infection at the early and at the hyperinflammatory stages [77,102,128]. Despite these positive results, the efficacy of Vitamin D application in patients with COVID-19 still remains controversial, and future studies are required [129]. A phase 3 RCT, the CORONAVIT study is currently ongoing (NCT04579640). In this study the authors determined whether population-level implementation of a test-and-treat approach to correction of sub-optimal vitamin D status influences the risk of acute respiratory infection or COVID-19 disease. In adult sub-optimal vitamin D status, vitamin D implementation has no impact on the risk of acute respiratory infection or COVID-19 disease.
Regarding vitamin C, many observational studies indicated a low state of vitamin C in critically ill patients with COVID-19 [130,131]. Currently, several RCTs are evaluating intravenous administration of vitamin C monotherapy [132,133,134,135]. Given the pharmacokinetics of vitamin C and the increased requirement during pulmonary infections, oral vitamin C might not be as effective as intravenous administration [136], significantly reducing levels of IL-6 by the first week [87]. Coagulopathy and development of microthrombi represent further common complications of COVID-19 [63], which probably are important components of lung problems [137]. Early vitamin C injections prevent microthrombi formation and blockage of capillaries [138]. Indeed, previous studies have also shown that the level of D-dimer in COVID-19 patients decreased if intravenous vitamin C was administered [139]. Another possible complication of COVID-19 is the extracellular neutrophil traps, which may predispose to the coagulopathy related to COVID-19 [140,141]. In sepsis models, administration of vitamin C may decrease the extracellular neutrophil trap formation [142]. Neutrophil-derived oxidative stress is thought to induce tissue damage in COVID-19 [143,144]. Patients with respiratory infection and sepsis demonstrated a considerable elevation of the oxidative stress markers compared to other critical patients [145,146]. In these patients, administration of vitamin C stabilized markers of oxidative stress, improving the survivorship [56,147]. Moreover, the administration of vitamin C in critical patients might have shortened the mechanical ventilation and the length the intensive care stay [148,149]. The above findings may be particularly important in countries with limited capacity of ICUs beds and more generally in contexts with limited resources, such as low-middle-income countries [150]. Most of the top 10 countries with the highest number of cases for COVID-19 have low-medium income [151], a known risk factor for hypovitaminosis C [152].
5. Conclusions
According to the main findings of the present study, our hypothesis that the administration of vitamins C and D in COVID-19 patients impacts positively disease susceptibility, severity and progression was not supported by the current evidence. While waiting to develop a targeted, safe and effective therapy, it is important to investigate individual predisposition and proper disease management. Available data on the use of nutraceuticals in COVID-19 are inconsistent. However, there is a lack of evidence-based guidelines which recommend vitamin C and D supplementation in patients with COVID-19, and results from high quality randomised controlled trials (RCTs) are inconsistent. Current investigations so far are mostly observational, and include a relatively small sample size, which can lead to biased results. Large-scale multicentre studies are therefore needed.
Author Contributions
Conceptualization, writing, revision and final approval, F.M.; revision and final approval, J.E.; revision and final approval, F.O.; supervision and final approval, F.H.; supervision and final approval, R.V.; writing, revision, and final approval, N.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Umakanthan, S.; Sahu, P.; Ranade, A.V.; Bukelo, M.M.; Rao, J.S.; Lf, A.-M.; Dahal, S.; Kumar, H.; Kv, D. Origin, transmission, diagnosis and management of coronavirus disease 2019 (COVID-19). Postgrad. Med. J. 2020, 96, 753–758. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Weber, C.D.; Pappalardo, G.; Schenker, H.; Hofmann, U.K.; Eschweiler, J.; Hildebrand, F. Orthopaedic, trauma surgery, and Covid-2019 pandemic: Clinical panorama and future prospective in Europe. Eur. J. Trauma Emerg. Surg. 2022. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Shi, L.; Wang, Y.; Zhang, J.; Huang, L.; Zhang, C.; Liu, S.; Zhao, P.; Liu, H.; Zhu, L.; et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020, 8, 420–422. [Google Scholar] [CrossRef]
- Xiong, S.; Liu, L.; Lin, F.; Shi, J.; Han, L.; Liu, H.; He, L.; Jiang, Q.; Wang, Z.; Fu, W.; et al. Clinical characteristics of 116 hospitalized patients with COVID-19 in Wuhan, China: A single-centered, retrospective, observational study. BMC Infect. Dis. 2020, 20, 787. [Google Scholar] [CrossRef]
- Bugeja, M.; Mariani, J.; Dowling, J.; Stringaro, G.; Portelli, J.L.; Sant, K.; Casaletto, J. Musculoskeletal steroid injections during the COVID-19 pandemic. J. Orthop. 2021, 26, 103–106. [Google Scholar] [CrossRef]
- Cai, H. Sex difference and smoking predisposition in patients with COVID-19. Lancet Respir. Med. 2020, 8, e20. [Google Scholar] [CrossRef]
- Yang, J.; Zheng, Y.; Gou, X.; Pu, K.; Chen, Z.; Guo, Q.; Ji, R.; Wang, H.; Wang, Y.; Zhou, Y. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: A systematic review and meta-analysis. Int. J. Infect. Dis. 2020, 94, 91–95. [Google Scholar] [CrossRef]
- Khan, M.A.; Khan, N.; Mustagir, G.; Rana, J.; Islam, S.; Kabir, I. Effects of underlying morbidities on the occurrence of deaths in COVID-19 patients: A systematic review and meta-analysis. J. Glob. Health 2020, 10, 020503. [Google Scholar] [CrossRef]
- Zhou, Y.; Yang, Q.; Chi, J.; Dong, B.; Lv, W.; Shen, L.; Wang, Y. Comorbidities and the risk of severe or fatal outcomes associated with coronavirus disease 2019: A systematic review and meta-analysis. Int. J. Infect. Dis. 2020, 99, 47–56. [Google Scholar] [CrossRef]
- Jain, V.; Yuan, J.-M. Predictive symptoms and comorbidities for severe COVID-19 and intensive care unit admission: A systematic review and meta-analysis. Int. J. Public Health 2020, 65, 533–546. [Google Scholar] [CrossRef]
- Wang, K.C.; Xiao, R.; Cheung, Z.B.; Barbera, J.P.; Forsh, D.A. Early mortality after hip fracture surgery in COVID-19 patients: A systematic review and meta-analysis. J. Orthop. 2020, 22, 584–591. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Ticinesi, A.; Nouvenne, A.; Folesani, G.; Prati, B.; Morelli, I.; Guida, L.; Lauretani, F.; Maggio, M.; Meschi, T. An investigation of multimorbidity measures as risk factors for pneumonia in elderly frail patients admitted to hospital. Eur. J. Intern. Med. 2015, 28, 102–106. [Google Scholar] [CrossRef] [PubMed]
- Cilloniz, C.; Polverino, E.; Ewig, S.; Aliberti, S.; Gabarrús, A.; Menéndez, R.; Mensa, J.; Blasi, F.; Torres, A. Impact of Age and Comorbidity on Cause and Outcome in Community-Acquired Pneumonia. Chest 2013, 144, 999–1007. [Google Scholar] [CrossRef] [PubMed]
- Ladha, K.S.; Zhao, K.; Quraishi, S.A.; Kurth, T.; Eikermann, M.; Kaafarani, H.M.; Klein, E.N.; Seethala, R.; Lee, J. The Deyo-Charlson and Elixhauser-van Walraven Comorbidity Indices as predictors of mortality in critically ill patients. BMJ Open 2015, 5, e008990. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.J.; Dong, X.; Cao, Y.Y.; Yuan, Y.D.; Yang, Y.B.; Yan, Y.Q.; Akdis, C.A.; Gao, Y.D. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy 2020, 75, 1730–1741. [Google Scholar] [CrossRef]
- Liu, W.; Tao, Z.-W.; Wang, L.; Yuan, M.-L.; Liu, K.; Zhou, L.; Wei, S.; Deng, Y.; Liu, J.; Liu, H.-G.; et al. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin. Med. J. 2020, 133, 1032–1038. [Google Scholar] [CrossRef]
- Duc, S.; Rainfray, M.; Soubeyran, P.-L.; Fonck, M.; Blanc, J.F.; Ceccaldi, J.; Cany, L.; Brouste, V.; Mathoulin-Pélissier, S. Predictive factors of depressive symptoms of elderly patients with cancer receiving first-line chemotherapy. Psychooncology 2016, 26, 15–21. [Google Scholar] [CrossRef]
- Ho, T.-S.; Wang, S.-M.; Liu, C.-C. Historical Review of Pandemic Influenza A in Taiwan, 2009. Pediatr. Neonatol. 2010, 51, 83–88. [Google Scholar] [CrossRef][Green Version]
- Wu, C.-T.; Hsia, S.-H.; Huang, J.-L. Influenza B-associated rhabdomyolysis in Taiwanese children. Acta Paediatr. 2009, 99, 1701–1704. [Google Scholar] [CrossRef]
- Ji, H.-L.; Zhao, R.; Matalon, S.; Matthay, M.A. Elevated Plasmin(ogen) as a Common Risk Factor for COVID-19 Susceptibility. Physiol. Rev. 2020, 100, 1065–1075. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.-H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280.e8. [Google Scholar] [CrossRef] [PubMed]
- McKee, D.L.; Sternberg, A.; Stange, U.; Laufer, S.; Naujokat, C. Candidate drugs against SARS-CoV-2 and COVID-19. Pharmacol. Res. 2020, 157, 104859. [Google Scholar] [CrossRef] [PubMed]
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.-L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. [Google Scholar] [CrossRef]
- Hu, B.; Huang, S.; Yin, L. The cytokine storm and COVID-19. J. Med. Virol. 2020, 93, 250–256. [Google Scholar] [CrossRef]
- Agrawal, D.; Yin, K. Vitamin D and inflammatory diseases. J. Inflamm. Res. 2014, 7, 69–87. [Google Scholar] [CrossRef]
- Panfili, F.M.; Roversi, M.; D’Argenio, P.; Rossi, P.; Cappa, M.; Fintini, D. Possible role of vitamin D in Covid-19 infection in pediatric population. J. Endocrinol. Investig. 2020, 44, 27–35. [Google Scholar] [CrossRef]
- Carlberg, C. Vitamin D Signaling in the Context of Innate Immunity: Focus on Human Monocytes. Front. Immunol. 2019, 10, 2211. [Google Scholar] [CrossRef]
- Manson, J.E.; Cook, N.R.; Lee, I.M.; Christen, W.; Bassuk, S.S.; Mora, S.; Gibson, H.; Gordon, D.; Copeland, T.; D’Agostino, D.; et al. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. N. Engl. J. Med. 2019, 380, 33–44. [Google Scholar] [CrossRef]
- Grant, W.B.; Al Anouti, F.; Moukayed, M. Targeted 25-hydroxyvitamin D concentration measurements and vitamin D3 supplementation can have important patient and public health benefits. Eur. J. Clin. Nutr. 2020, 74, 366–376. [Google Scholar] [CrossRef]
- Pittas, A.G.; Dawson-Hughes, B.; Sheehan, P.; Ware, J.H.; Knowler, W.C.; Aroda, V.R.; Brodsky, I.; Ceglia, L.; Chadha, C.; Chatterjee, R.; et al. Vitamin D Supplementation and Prevention of Type 2 Diabetes. N. Engl. J. Med. 2019, 381, 520–530. [Google Scholar] [CrossRef] [PubMed]
- Martineau, A.R.; Jolliffe, D.A.; Greenberg, L.; Aloia, J.F.; Bergman, P.; Dubnov-Raz, G.; Esposito, S.; Ganmaa, D.; Ginde, A.A.; Goodall, E.C.; et al. Vitamin D supplementation to prevent acute respiratory infections: Individual participant data meta-analysis. Health Technol. Assess. 2019, 23, 356. [Google Scholar] [CrossRef] [PubMed]
- Hayes, C.E.; Ntambi, J.M. Multiple Sclerosis: Lipids, Lymphocytes, and Vitamin D. Immunometabolism 2020, 2. [Google Scholar] [CrossRef]
- WHO. COVID-19 Dashboard. Available online: https://covid19.who.int (accessed on 17 March 2022).
- Mercola, J.; Grant, W.B.; Wagner, C.L. Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity. Nutrients 2020, 12, 3361. [Google Scholar] [CrossRef]
- Mitri, J.; Muraru, M.D.; Pittas, A.G. Vitamin D and type 2 diabetes: A systematic review. Eur. J. Clin. Nutr. 2011, 65, 1005–1015. [Google Scholar] [CrossRef]
- Kroll, M.H.; Bi, C.; Garber, C.C.; Kaufman, H.W.; Liu, D.; Caston-Balderrama, A.; Zhang, K.; Clarke, N.; Xie, M.; Reitz, R.E.; et al. Temporal Relationship between Vitamin D Status and Parathyroid Hormone in the United States. PLoS ONE 2015, 10, e0118108. [Google Scholar] [CrossRef]
- Yancy, C.W. COVID-19 and African Americans. JAMA 2020, 323, 1891–1892. [Google Scholar] [CrossRef]
- Yehia, B.R.; Winegar, A.; Fogel, R.; Fakih, M.; Ottenbacher, A.; Jesser, C.; Bufalino, A.; Huang, R.-H.; Cacchione, J. Association of Race with Mortality Among Patients Hospitalized with Coronavirus Disease 2019 (COVID-19) at 92 US Hospitals. JAMA Netw. Open 2020, 3, e2018039. [Google Scholar] [CrossRef]
- Ginde, A.A.; Liu, M.C.; Camargo, C.A., Jr. Demographic Differences and Trends of Vitamin D Insufficiency in the US Population, 1988–2004. Arch. Intern. Med. 2009, 169, 626–632. [Google Scholar] [CrossRef]
- Caricchio, R.; Gallucci, M.; Dass, C.; Zhang, X.; Gallucci, S.; Fleece, D.; Bromberg, M.; Criner, G.J. Preliminary predictive criteria for COVID-19 cytokine storm. Ann. Rheum. Dis. 2020, 80, 88–95. [Google Scholar] [CrossRef]
- Qin, C.; Zhou, L.; Hu, Z.; Zhang, S.; Yang, S.; Tao, Y.; Xie, C.; Ma, K.; Shang, K.; Wang, W.; et al. Dysregulation of Immune Response in Patients With Coronavirus 2019 (COVID-19) in Wuhan, China. Clin. Infect. Dis. 2020, 71, 762–768. [Google Scholar] [CrossRef] [PubMed]
- Zdrenghea, M.T.; Makrinioti, H.; Bagacean, C.; Bush, A.; Johnston, S.; Stanciu, L.A. Vitamin D modulation of innate immune responses to respiratory viral infections. Rev. Med. Virol. 2016, 27, e1909. [Google Scholar] [CrossRef] [PubMed]
- Telcian, A.G.; Zdrenghea, M.T.; Edwards, M.R.; Laza-Stanca, V.; Mallia, P.; Johnston, S.L.; Stanciu, L.A. Vitamin D increases the antiviral activity of bronchial epithelial cells in vitro. Antivir. Res. 2017, 137, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Cannell, J.J.; Vieth, R.; Umhau, J.C.; Holick, M.F.; Grant, W.B.; Madronich, S.; Garland, C.F.; Giovannucci, E. Epidemic influenza and vitamin D. Epidemiol. Infect. 2006, 134, 1129–1140. [Google Scholar] [CrossRef]
- Chowdhury, R.; Taneja, S.; Bhandari, N.; Sinha, B.; Upadhyay, R.P.; Bhan, M.K.; Strand, T. Vitamin-D deficiency predicts infections in young north Indian children: A secondary data analysis. PLoS ONE 2017, 12, e0170509. [Google Scholar] [CrossRef]
- Arihiro, S.; Nakashima, A.; Matsuoka, M.; Suto, S.; Uchiyama, K.; Kato, T.; Mitobe, J.; Komoike, N.; Itagaki, M.; Miyakawa, Y.; et al. Randomized Trial of Vitamin D Supplementation to Prevent Seasonal Influenza and Upper Respiratory Infection in Patients with Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2019, 25, 1088–1095. [Google Scholar] [CrossRef]
- Grant, W.B.; Lahore, H.; McDonnell, S.L.; Baggerly, C.A.; French, C.B.; Aliano, J.L.; Bhattoa, H.P. Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients 2020, 12, 988. [Google Scholar] [CrossRef]
- Carr, A.C.; Rowe, S. The Emerging Role of Vitamin C in the Prevention and Treatment of COVID-19. Nutrients 2020, 12, 3286. [Google Scholar] [CrossRef]
- Schorah, C.J.; Downing, C.; Piripitsi, A.; Gallivan, L.; Al-Hazaa, A.H.; Sanderson, M.J.; Bodenham, A. Total vitamin C, ascorbic acid, and dehydroascorbic acid concentrations in plasma of critically ill patients. Am. J. Clin. Nutr. 1996, 63, 760–765. [Google Scholar] [CrossRef]
- Galley, H.F.; Davies, M.J.; Webster, N.R. Ascorbyl radical formation in patients with sepsis: Effect of ascorbate loading. Free Radic. Biol. Med. 1996, 20, 139–143. [Google Scholar] [CrossRef]
- Borrelli, E.; Roux-Lombard, P.; Grau, G.E.; Girardin, E.; Ricou, B.; Dayer, J.; Suter, P.M. Plasma concentrations of cytokines, their soluble receptors, and antioxidant vitamins can predict the development of multiple organ failure in patients at risk. Crit. Care Med. 1996, 24, 392–397. [Google Scholar] [CrossRef]
- Long, C.; Maull, K.; Krishnan, R.; Laws, H.; Geiger, J.; Borghesi, L.; Franks, W.; Lawson, T.; Sauberlich, H. Ascorbic acid dynamics in the seriously ill and injured. J. Surg. Res. 2003, 109, 144–148. [Google Scholar] [CrossRef]
- de Grooth, H.-J.; Manubulu-Choo, W.-P.; Zandvliet, A.S.; de Man, A.M.E.S.; Girbes, A.R.; Swart, E.L.; van Straaten, H.M.O. Vitamin C Pharmacokinetics in Critically Ill Patients. Chest 2018, 153, 1368–1377. [Google Scholar] [CrossRef] [PubMed]
- Fowler, A.A., III; Syed, A.A.; Knowlson, S.; Sculthorpe, R.; Farthing, D.; Dewilde, C.; Farthing, C.A.; Larus, T.L.; Martin, E.; Brophy, D.F.; et al. Phase I safety trial of intravenous ascorbic acid in patients with severe sepsis. J. Transl. Med. 2014, 12, 32. [Google Scholar] [CrossRef] [PubMed]
- Fowler, A.A., 3rd; Truwit, J.D.; Hite, R.D.; Morris, P.E.; Dewilde, C.; Priday, A.; Fisher, B.; Thacker, L.R., 2nd; Natarajan, R.; Brophy, D.F.; et al. Effect of Vitamin C Infusion on Organ Failure and Biomarkers of Inflammation and Vascular Injury in Patients With Sepsis and Severe Acute Respiratory Failure. JAMA 2019, 322, 1261–1270. [Google Scholar] [CrossRef]
- Hunt, C.; Chakravorty, N.K.; Annan, G.; Habibzadeh, N.; Schorah, C.J. The clinical effects of vitamin C supplementation in elderly hospitalised patients with acute respiratory infections. Int. J. Vitam. Nutr. Res. 1994, 64, 212–219. [Google Scholar]
- Mochalkin, N.I. Ascorbic acid in the complex therapy of acute pneumonia. Voen. -Meditsinskii Zhurnal 1970, 9, 17–21. [Google Scholar]
- Hemilä, H.; Chalker, E. Reanalysis of the Effect of Vitamin C on Mortality in the CITRIS-ALI Trial: Important Findings Dismissed in the Trial Report. Front. Med. 2020, 7, 590853. [Google Scholar] [CrossRef]
- Kashiouris, M.G.; L’Heureux, M.; Cable, C.A.; Fisher, B.J.; Leichtle, S.W.; Fowler, A.A. The Emerging Role of Vitamin C as a Treatment for Sepsis. Nutrients 2020, 12, 292. [Google Scholar] [CrossRef]
- Carr, A.C.; Rosengrave, P.C.; Bayer, S.; Chambers, S.; Mehrtens, J.; Shaw, G.M. Hypovitaminosis C and vitamin C deficiency in critically ill patients despite recommended enteral and parenteral intakes. Crit. Care 2017, 21, 300. [Google Scholar] [CrossRef]
- Holford, P.; Carr, A.; Jovic, T.; Ali, S.; Whitaker, I.; Marik, P.; Smith, A.D. Vitamin C—An Adjunctive Therapy for Respiratory Infection, Sepsis and COVID-19. Nutrients 2020, 12, 3760. [Google Scholar] [CrossRef] [PubMed]
- Wiersinga, W.J.; Rhodes, A.; Cheng, A.C.; Peacock, S.J.; Prescott, H.C. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA 2020, 324, 782–793. [Google Scholar] [CrossRef] [PubMed]
- Blanco-Melo, D.; Nilsson-Payant, B.E.; Liu, W.-C.; Uhl, S.; Hoagland, D.; Møller, R.; Jordan, T.X.; Oishi, K.; Panis, M.; Sachs, D.; et al. Imbalanced Host Response to SARS-CoV-2 Drives Development of COVID-19. Cell 2020, 181, 1036–1045.e9. [Google Scholar] [CrossRef]
- Zhang, Q.; Bastard, P.; Liu, Z.; Le Pen, J.; Moncada-Velez, M.; Chen, J.; Ogishi, M.; Sabli, I.K.D.; Hodeib, S.; Korol, C.; et al. Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science 2020, 370, eabd4570. [Google Scholar] [CrossRef]
- Bastard, P.; Rosen, L.B.; Zhang, Q.; Michailidis, E.; Hoffmann, H.-H.; Zhang, Y.; Dorgham, K.; Philippot, Q.; Rosain, J.; Béziat, V.; et al. Autoantibodies against type I IFNs in patients with life-threatening COVID-19. Science 2020, 370, eabd4585. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Kim, H.; Bae, S.; Choi, J.; Lim, S.Y.; Lee, N.; Kong, J.M.; Hwang, Y.-I.; Kang, J.S.; Lee, W.J. Vitamin C Is an Essential Factor on the Anti-viral Immune Responses through the Production of Interferon-α/β at the Initial Stage of Influenza A Virus (H3N2) Infection. Immune Netw. 2013, 13, 70–74. [Google Scholar] [CrossRef]
- Geber, W.F.; Lefkowitz, S.S.; Hung, C.Y. Effect of Ascorbic Acid, Sodium Salicylate, and Caffeine on the Serum Interferon Level in Response to Viral Infection. Pharmacology 1975, 13, 228–233. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Howick, J.C.I.; Glasziou, P.; Greenhalgh, T.; Carl, H.; Liberati, A.; Moschetti, I.; Phillips, B.; Thornton, H.; Goddard, O.; Hodgkinson, M. The 2011 Oxford CEBM Levels of Evidence. Oxford Centre for Evidence-Based Medicine. 2011. Available online: https://wwwcebmnet/indexaspx?o=5653 (accessed on 17 March 2022).
- Alcala-Diaz, J.; Limia-Perez, L.; Gomez-Huelgas, R.; Martin-Escalante, M.; Cortes-Rodriguez, B.; Zambrana-Garcia, J.; Entrenas-Castillo, M.; Perez-Caballero, A.; López-Carmona, M.; Garcia-Alegria, J.; et al. Calcifediol Treatment and Hospital Mortality Due to COVID-19: A Cohort Study. Nutrients 2021, 13, 1760. [Google Scholar] [CrossRef]
- Annweiler, G.; Corvaisier, M.; Gautier, J.; Dubée, V.; Legrand, E.; Sacco, G.; Annweiler, C. Vitamin D Supplementation Associated to Better Survival in Hospitalized Frail Elderly COVID-19 Patients: The GERIA-COVID Quasi-Experimental Study. Nutrients 2020, 12, 3377. [Google Scholar] [CrossRef]
- Annweiler, C.; Hanotte, B.; de L’Eprevier, C.G.; Sabatier, J.-M.; Lafaie, L.; Célarier, T. Vitamin D and survival in COVID-19 patients: A quasi-experimental study. J. Steroid Biochem. Mol. Biol. 2020, 204, 105771. [Google Scholar] [CrossRef] [PubMed]
- Cangiano, B.; Fatti, L.M.; Danesi, L.; Gazzano, G.; Croci, M.; Vitale, G.; Gilardini, L.; Bonadonna, S.; Chiodini, I.; Caparello, C.F.; et al. Mortality in an Italian nursing home during COVID-19 pandemic: Correlation with gender, age, ADL, vitamin D supplementation, and limitations of the diagnostic tests. Aging 2020, 12, 24522–24534. [Google Scholar] [CrossRef] [PubMed]
- Lakkireddy, M.; Gadiga, S.G.; Malathi, R.D. Impact of daily high dose oral vitamin D therapy on the inflammatory markers in patients with COVID 19 disease. Sci. Rep. 2021, 11, 10641. [Google Scholar] [CrossRef] [PubMed]
- Elamir, Y.M.; Amir, H.; Lim, S.; Rana, Y.P.; Lopez, C.G.; Feliciano, N.V.; Omar, A.; Grist, W.P.; Via, M.A. A randomized pilot study using calcitriol in hospitalized COVID-19 patients. Bone 2021, 154, 116175. [Google Scholar] [CrossRef]
- Entrenas Castillo, M.E.; Entrenas Costa, L.M.E.; Vaquero Barrios, J.M.V.; Alcalá Díaz, J.F.A.; López Miranda, J.L.; Bouillon, R.; Quesada Gomez, J.M.Q. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study. J. Steroid Biochem. Mol. Biol. 2020, 203, 105751. [Google Scholar] [CrossRef]
- Arroyo-Díaz, J.A.; Julve, J.; Vlacho, B.; Corcoy, R.; Ponte, P.; Román, E.; Navas-Méndez, E.; Llauradó, G.; Franch-Nadal, J.; Domingo, P.; et al. Previous Vitamin D Supplementation and Morbidity and Mortality Outcomes in People Hospitalised for COVID19: A Cross-Sectional Study. Front. Public Health 2021, 9, 758347. [Google Scholar] [CrossRef]
- Güven, M.; Gültekin, H. The effect of high-dose parenteral vitamin D3 on COVID-19-related inhospital mortality in critical COVID-19 patients during intensive care unit admission: An observational cohort study. Eur. J. Clin. Nutr. 2021, 75, 1383–1388. [Google Scholar] [CrossRef]
- Hernández, J.L.; Nan, D.; Fernandez-Ayala, M.; García-Unzueta, M.; Hernández-Hernández, M.A.; López-Hoyos, M.; Muñoz-Cacho, P.; Olmos, J.M.; Gutiérrez-Cuadra, M.; Ruiz-Cubillán, J.J.; et al. Vitamin D Status in Hospitalized Patients with SARS-CoV-2 Infection. J. Clin. Endocrinol. Metab. 2021, 106, e1343–e1353. [Google Scholar] [CrossRef]
- Jevalikar, G.; Mithal, A.; Singh, A.; Sharma, R.; Farooqui, K.J.; Mahendru, S.; Dewan, A.; Budhiraja, S. Lack of association of baseline 25-hydroxyvitamin D levels with disease severity and mortality in Indian patients hospitalized for COVID-19. Sci. Rep. 2021, 11, 1–8. [Google Scholar] [CrossRef]
- Annweiler, C.; Beaudenon, M.; Gautier, J.; Gonsard, J.; Boucher, S.; Chapelet, G.; Darsonval, A.; Fougere, B.; Guerin, O.; Houvet, M.; et al. High-dose versus standard-dose vitamin D supplementation in older adults with COVID-19 (COVIT-TRIAL): A multicenter, open-label, randomized controlled superiority trial. PLoS Med. 2022, 19, e1003999. [Google Scholar] [CrossRef]
- Cereda, E.; Bogliolo, L.; Lobascio, F.; Barichella, M.; Zecchinelli, A.L.; Pezzoli, G.; Caccialanza, R. Vitamin D supplementation and outcomes in coronavirus disease 2019 (COVID-19) patients from the outbreak area of Lombardy, Italy. Nutrition 2020, 82, 111055. [Google Scholar] [CrossRef] [PubMed]
- Murai, I.H.; Fernandes, A.L.; Sales, L.P.; Pinto, A.J.; Goessler, K.F.; Duran, C.S.C.; Silva, C.B.R.; Franco, A.S.; Macedo, M.B.; Dalmolin, H.H.H.; et al. Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients With Moderate to Severe COVID-19. JAMA: J. Am. Med Assoc. 2021, 325, 1053–1060. [Google Scholar] [CrossRef] [PubMed]
- Gao, D.; Xu, M.; Wang, G.; Lv, J.; Ma, X.; Guo, Y.; Zhang, D.; Yang, H.; Jiang, W.; Deng, F.; et al. The efficiency and safety of high-dose vitamin C in patients with COVID-19: A retrospective cohort study. Aging 2021, 13, 7020–7034. [Google Scholar] [CrossRef] [PubMed]
- Al Sulaiman, K.; Aljuhani, O.; Bin Saleh, K.; Badreldin, H.A.; Al Harthi, A.; Alenazi, M.; Alharbi, A.; Algarni, R.; Al Harbi, S.; Alhammad, A.M.; et al. Ascorbic acid as an adjunctive therapy in critically ill patients with COVID-19: A propensity score matched study. Sci. Rep. 2021, 11, 17648. [Google Scholar] [CrossRef]
- Zhang, J.; Rao, X.; Li, Y.; Zhu, Y.; Liu, F.; Guo, G.; Luo, G.; Meng, Z.; De Backer, D.; Xiang, H.; et al. Pilot trial of high-dose vitamin C in critically ill COVID-19 patients. Ann. Intensiv. Care 2021, 11, 5. [Google Scholar] [CrossRef]
- JamaliMoghadamSiahkali, S.; Zarezade, B.; Koolaji, S.; SeyedAlinaghi, S.; Zendehdel, A.; Tabarestani, M.; Moghadam, E.S.; Abbasian, L.; Manshadi, S.A.D.; Salehi, M.; et al. Safety and effectiveness of high-dose vitamin C in patients with COVID-19: A randomized open-label clinical trial. Eur. J. Med. Res. 2021, 26, 20. [Google Scholar] [CrossRef]
- Kumari, P.; Dembra, S.; Dembra, P.; Bhawna, F.; Gul, A.; Ali, B.; Sohail, H.; Kumar, B.; Memon, M.K.; Rizwan, A. The Role of Vitamin C as Adjuvant Therapy in COVID-19. Cureus 2020, 12, e11779. [Google Scholar] [CrossRef]
- Li, M.; Ching, T.H.; Hipple, C.; Lopez, R.; Sahibzada, A.; Rahman, H. Use of Intravenous Vitamin C in Critically Ill Patients With COVID-19 Infection. J. Pharm. Pract. 2021. [Google Scholar] [CrossRef]
- Suna, K.; Melahat, U.; Murat, Y.; Figen, O.E.; Ayperi, O. Effect of high-dose intravenous vitamin C on prognosis in patients with SARS-CoV-2 pneumonia. Med. Clin. 2021, 158, 356–360. [Google Scholar] [CrossRef]
- Thomas, S.; Patel, D.; Bittel, B.; Wolski, K.; Wang, Q.; Kumar, A.; Il’Giovine, Z.J.; Mehra, R.; McWilliams, C.; Nissen, S.E.; et al. Effect of High-Dose Zinc and Ascorbic Acid Supplementation vs Usual Care on Symptom Length and Reduction Among Ambulatory Patients With SARS-CoV-2 Infection. JAMA Netw. Open 2021, 4, e210369. [Google Scholar] [CrossRef]
- Zheng, S.; Chen, Q.; Jiang, H.; Guo, C.; Luo, J.; Li, S.; Wang, H.; Li, H.; Zheng, X.; Weng, Z. No significant benefit of moderate-dose vitamin C on severe COVID-19 cases. Open Med. 2020, 16, 1403–1414. [Google Scholar] [CrossRef] [PubMed]
- Gruber-Bzura, B.M. High-Dose Vitamin C Supplementation as a Legitimate Anti-SARS-CoV-2 Prophylaxis in Healthy Subjects—Yes or No? Nutrients 2022, 14, 979. [Google Scholar] [CrossRef] [PubMed]
- Cerullo, G.; Negro, M.; Parimbelli, M.; Pecoraro, M.; Perna, S.; Liguori, G.; Rondanelli, M.; Cena, H.; D’Antona, G. The Long History of Vitamin C: From Prevention of the Common Cold to Potential Aid in the Treatment of COVID-19. Front. Immunol. 2020, 11, 574029. [Google Scholar] [CrossRef]
- Carr, A.C. Micronutrient status of COVID-19 patients: A critical consideration. Crit. Care 2020, 24, 349. [Google Scholar] [CrossRef]
- Migliorini, F.; Torsiello, E.; Spiezia, F.; Oliva, F.; Tingart, M.; Maffulli, N. Association between HLA genotypes and COVID-19 susceptibility, severity and progression: A comprehensive review of the literature. Eur. J. Med Res. 2021, 26, 84. [Google Scholar] [CrossRef] [PubMed]
- Barazzoni, R.; Bischoff, S.C.; Breda, J.; Wickramasinghe, K.; Krznaric, Z.; Nitzan, D.; Pirlich, M.; Singer, P. ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. Clin. Nutr. 2020, 39, 1631–1638. [Google Scholar] [CrossRef] [PubMed]
- Semba, R.D.; Tang, A.M. Micronutrients and the pathogenesis of human immunodeficiency virus infection. Br. J. Nutr. 1999, 81, 181–189. [Google Scholar] [CrossRef]
- Hastie, C.E.; Mackay, D.F.; Ho, F.; Celis-Morales, C.A.; Katikireddi, S.V.; Niedzwiedz, C.L.; Jani, B.D.; Welsh, P.; Mair, F.S.; Gray, S.R.; et al. Corrigendum to “Vitamin D concentrations and COVID-19 infection in UK Biobank” Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1315–1316. [Google Scholar] [CrossRef]
- D’Avolio, A.; Avataneo, V.; Manca, A.; Cusato, J.; De Nicolò, A.; Lucchini, R.; Keller, F.; Cantù, M. 25-Hydroxyvitamin D Concentrations Are Lower in Patients with Positive PCR for SARS-CoV-2. Nutrients 2020, 12, 1359. [Google Scholar] [CrossRef]
- Panagiotou, G.; Tee, S.A.; Ihsan, Y.; Athar, W.; Marchitelli, G.; Kelly, D.; Boot, C.S.; Stock, N.; Macfarlane, J.; Martineau, A.R.; et al. Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalised with COVID-19 are associated with greater disease severity: Results of a local audit of practice. Clin. Endocrinol. 2020, 93, 508–511. [Google Scholar] [CrossRef]
- Carpagnano, G.E.; Di Lecce, V.; Quaranta, V.N.; Zito, A.; Buonamico, E.; Capozza, E.; Palumbo, A.; Di Gioia, G.; Valerio, V.N.; Resta, O. Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19. J. Endocrinol. Investig. 2020, 44, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Im, J.H.; Je, Y.S.; Baek, J.; Chung, M.-H.; Kwon, H.Y.; Lee, J.-S. Nutritional status of patients with COVID-19. Int. J. Infect. Dis. 2020, 100, 390–393. [Google Scholar] [CrossRef] [PubMed]
- Signes-Costa, J.; Núñez-Gil, I.J.; Soriano, J.B.; Arroyo-Espliguero, R.; Eid, C.M.; Romero, R.; Uribarri, A.; Fernández-Rozas, I.; Aguado, M.G.; Becerra-Muñoz, V.M.; et al. Prevalence and 30-Day Mortality in Hospitalized Patients with Covid-19 and Prior Lung Diseases. Arch. De Bronconeumol. 2020, 57, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Baktash, V.; Hosack, T.; Patel, N.; Shah, S.; Kandiah, P.; Van De Abbeele, K.; Mandal, A.K.J.; Missouris, C.G. Vitamin D status and outcomes for hospitalised older patients with COVID-19. Postgrad. Med. J. 2020. [Google Scholar] [CrossRef]
- Hastie, C.E.; Pell, J.P.; Sattar, N. Vitamin D and COVID-19 infection and mortality in UK Biobank. Eur. J. Nutr. 2020, 60, 545–548. [Google Scholar] [CrossRef]
- Radujkovic, A.; Hippchen, T.; Tiwari-Heckler, S.; Dreher, S.; Boxberger, M.; Merle, U. Vitamin D Deficiency and Outcome of COVID-19 Patients. Nutrients 2020, 12, 2757. [Google Scholar] [CrossRef]
- Valcour, A.; Blocki, F.; Hawkins, D.M.; Rao, S.D. Effects of Age and Serum 25-OH-Vitamin D on Serum Parathyroid Hormone Levels. J. Clin. Endocrinol. Metab. 2012, 97, 3989–3995. [Google Scholar] [CrossRef]
- Pizzini, A.; Aichner, M.; Sahanic, S.; Böhm, A.; Egger, A.; Hoermann, G.; Kurz, K.; Widmann, G.; Bellmann-Weiler, R.; Weiss, G.; et al. Impact of Vitamin D Deficiency on COVID-19—A Prospective Analysis from the CovILD Registry. Nutrients 2020, 12, 2775. [Google Scholar] [CrossRef]
- Macaya, F.; Espejo Paeres, C.; Valls, A.; Fernandez-Ortiz, A.; Gonzalez Del Castillo, J.; Martin-Sanchez, F.J.; Runkle, I.; Rubio Herrera, M.A. Interaction between age and vitamin D deficiency in severe COVID-19 infection. Nutr. Hosp. 2020, 37, 1039–1042. [Google Scholar] [CrossRef]
- Ye, K.; Tang, F.; Liao, X.; Shaw, B.A.; Deng, M.; Huang, G.; Qin, Z.; Peng, X.; Xiao, H.; Chen, C.; et al. Does Serum Vitamin D Level Affect COVID-19 Infection and Its Severity?—A Case-Control Study. J. Am. Coll. Nutr. 2020. [Google Scholar] [CrossRef]
- Merzon, E.; Tworowski, D.; Gorohovski, A.; Vinker, S.; Cohen, A.G.; Green, I.; Frenkel-Morgenstern, M. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: An Israeli population-based study. FEBS J. 2020, 287, 3693–3702. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, D.O.; Best, T.J.; Zhang, H.; Vokes, T.; Arora, V.; Solway, J. Association of Vitamin D Status and Other Clinical Characteristics With COVID-19 Test Results. JAMA Netw. Open 2020, 3, e2019722. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, H.W.; Niles, J.K.; Kroll, M.H.; Bi, C.; Holick, M.F. SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels. PLoS ONE 2020, 15, e0239252. [Google Scholar] [CrossRef] [PubMed]
- Mahdavi, A.M. A brief review of interplay between vitamin D and angiotensin-converting enzyme 2: Implications for a potential treatment for COVID-19. Rev. Med. Virol. 2020, 30, e2119. [Google Scholar] [CrossRef] [PubMed]
- Ross, A.C.; Manson, J.E.; Abrams, S.; Aloia, J.F.; Brannon, P.M.; Clinton, S.K.; Durazo-Arvizu, R.A.; Gallagher, J.C.; Gallo, R.; Jones, G.; et al. The 2011 Dietary Reference Intakes for Calcium and Vitamin D: What Dietetics Practitioners Need to Know. J. Am. Diet. Assoc. 2011, 111, 524–527. [Google Scholar] [CrossRef] [PubMed]
- Ross, A.C.; Manson, J.E.; Abrams, S.A.; Aloia, J.F.; Brannon, P.M.; Clinton, S.K.; Durazo-Arvizu, R.A.; Gallagher, J.C.; Gallo, R.L.; Jones, G.; et al. The 2011 Report on Dietary Reference Intakes for Calcium and Vitamin D from the Institute of Medicine: What Clinicians Need to Know. J. Clin. Endocrinol. Metab. 2011, 96, 53–58. [Google Scholar] [CrossRef]
- Korber, B.; Fischer, W.M.; Gnanakaran, S.; Yoon, H.; Theiler, J.; Abfalterer, W.; Hengartner, N.; Giorgi, E.E.; Bhattacharya, T.; Foley, B.; et al. Tracking Changes in SARS-CoV-2 Spike: Evidence that D614G Increases Infectivity of the COVID-19 Virus. Cell 2020, 182, 812–827.e19. [Google Scholar] [CrossRef]
- Strickland, O.L.; Powell-Young, Y.; Reyes-Miranda, C.; Alzaghari, O.; Giger, J.N. African-Americans Have a Higher Propensity for Death from COVID-19: Rationale and Causation. JNBNA 2020, 31, 1–12. [Google Scholar]
- Silva, M.C.; Furlanetto, T.W. Does serum 25-hydroxyvitamin D decrease during acute-phase response? A systematic review. Nutr. Res. 2015, 35, 91–96. [Google Scholar] [CrossRef]
- Krishnan, A.; Ochola, J.; Mundy, J.; Jones, M.; Kruger, P.; Duncan, E.; Venkatesh, B. Acute fluid shifts influence the assessment of serum vitamin D status in critically ill patients. Crit. Care 2010, 14, R216. [Google Scholar] [CrossRef]
- Reid, D.; Toole, B.J.; Knox, S.; Talwar, D.; Harten, J.; O’Reilly, D.S.J.; Blackwell, S.; Kinsella, J.; McMillan, D.C.; Wallace, A.M.; et al. The relation between acute changes in the systemic inflammatory response and plasma 25-hydroxyvitamin D concentrations after elective knee arthroplasty. Am. J. Clin. Nutr. 2011, 93, 1006–1011. [Google Scholar] [CrossRef] [PubMed]
- Waldron, J.L.; Ashby, H.L.; Cornes, M.P.; Bechervaise, J.; Razavi, C.; Thomas, O.L.; Chugh, S.; Deshpande, S.; Ford, C.; Gama, R. Vitamin D: A negative acute phase reactant. J. Clin. Pathol. 2013, 66, 620–622. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, A.V.; Trump, D.L.; Johnson, C.S.; Feldman, D. The Role of Vitamin D in Cancer Prevention and Treatment. Endocrinol. Metab. Clin. N. Am. 2010, 39, 401–418. [Google Scholar] [CrossRef] [PubMed]
- Martens, P.-J.; Gysemans, C.; Verstuyf, A.; Mathieu, C. Vitamin D’s Effect on Immune Function. Nutrients 2020, 12, 1248. [Google Scholar] [CrossRef]
- Sassi, F.; Tamone, C.; D’Amelio, P. Vitamin D: Nutrient, Hormone, and Immunomodulator. Nutrients 2018, 10, 1656. [Google Scholar] [CrossRef] [PubMed]
- Ohaegbulam, K.C.; Swalih, M.; Patel, P.; Smith, M.A.; Perrin, R. Vitamin D Supplementation in COVID-19 Patients: A Clinical Case Series. Am. J. Ther. 2020, 27, e485–e490. [Google Scholar] [CrossRef]
- Malaguarnera, L. Vitamin D3 as Potential Treatment Adjuncts for COVID-19. Nutrients 2020, 12, 3512. [Google Scholar] [CrossRef]
- Arvinte, C.; Singh, M.; Marik, P.E. Serum Levels of Vitamin C and Vitamin D in a Cohort of Critically Ill COVID-19 Patients of a North American Community Hospital Intensive Care Unit in May 2020: A Pilot Study. Med. Drug Discov. 2020, 8, 100064. [Google Scholar] [CrossRef]
- Chiscano-Camón, L.; Ruiz-Rodriguez, J.C.; Ruiz-Sanmartin, A.; Roca, O.; Ferrer, R. Vitamin C levels in patients with SARS-CoV-2-associated acute respiratory distress syndrome. Crit. Care 2020, 24, 522. [Google Scholar] [CrossRef]
- Liu, F.; Zhu, Y.; Zhang, J.; Li, Y.; Peng, Z. Intravenous high-dose vitamin C for the treatment of severe COVID-19: Study protocol for a multicentre randomised controlled trial. BMJ Open 2020, 10, e039519. [Google Scholar] [CrossRef]
- Masse, M.H.; Menard, J.; Sprague, S.; Battista, M.C.; Cook, D.J.; Guyatt, G.H.; Heyland, D.K.; Kanji, S.; Pinto, R.; Day, A.G.; et al. Lessening Organ dysfunction with VITamin C (LOVIT): Protocol for a randomized controlled trial. Trials 2020, 21, 42. [Google Scholar] [CrossRef] [PubMed]
- Carr, A.C. A new clinical trial to test high-dose vitamin C in patients with COVID-19. Crit. Care 2020, 24, 133. [Google Scholar] [CrossRef]
- Khan, H.M.W.; Parikh, N.; Megala, S.M.; Predeteanu, G.S. Unusual Early Recovery of a Critical COVID-19 Patient After Administration of Intravenous Vitamin C. Am. J. Case Rep. 2020, 21, e925521. [Google Scholar] [CrossRef]
- Lykkesfeldt, J. On the effect of vitamin C intake on human health: How to (mis)interprete the clinical evidence. Redox Biol. 2020, 34, 101532. [Google Scholar] [CrossRef] [PubMed]
- José, R.J.; Williams, A.; Manuel, A.; Brown, J.S.; Chambers, R.C. Targeting coagulation activation in severe COVID-19 pneumonia: Lessons from bacterial pneumonia and sepsis. Eur. Respir. Rev. 2020, 29. [Google Scholar] [CrossRef] [PubMed]
- Tyml, K. Vitamin C and Microvascular Dysfunction in Systemic Inflammation. Antioxidants 2017, 6, 49. [Google Scholar] [CrossRef] [PubMed]
- Hiedra, R.; Lo, K.B.; Elbashabsheh, M.; Gul, F.; Wright, R.M.; Albano, J.; Azmaiparashvili, Z.; Aponte, G.P. The use of IV vitamin C for patients with COVID-19: A case series. Expert Rev. Anti-Infect. Ther. 2020, 18, 1259–1261. [Google Scholar] [CrossRef]
- Middleton, E.A.; He, X.-Y.; Denorme, F.; Campbell, R.A.; Ng, D.; Salvatore, S.P.; Mostyka, M.; Baxter-Stoltzfus, A.; Borczuk, A.C.; Loda, M.; et al. Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome. Blood 2020, 136, 1169–1179. [Google Scholar] [CrossRef]
- Skendros, P.; Mitsios, A.; Chrysanthopoulou, A.; Mastellos, D.C.; Metallidis, S.; Rafailidis, P.; Ntinopoulou, M.; Sertaridou, E.; Tsironidou, V.; Tsigalou, C.; et al. Complement and tissue factor–enriched neutrophil extracellular traps are key drivers in COVID-19 immunothrombosis. J. Clin. Investig. 2020, 130, 6151–6157. [Google Scholar] [CrossRef]
- Mohammed, B.M.; Fisher, B.J.; Kraskauskas, D.; Farkas, D.; Brophy, D.F.; Fowler, A.A.; Natarajan, R. Vitamin C: A Novel Regulator of Neutrophil Extracellular Trap Formation. Nutrients 2013, 5, 3131–3150. [Google Scholar] [CrossRef]
- Schönrich, G.; Raftery, M.J.; Samstag, Y. Devilishly radical NETwork in COVID-19: Oxidative stress, neutrophil extracellular traps (NETs), and T cell suppression. Adv. Biol. Regul. 2020, 77, 100741. [Google Scholar] [CrossRef] [PubMed]
- LaForge, M.; Elbim, C.; Frère, C.; Hémadi, M.; Massaad, C.; Nuss, P.; Benoliel, J.-J.; Becker, C. Tissue damage from neutrophil-induced oxidative stress in COVID-19. Nat. Rev. Immunol. 2020, 20, 515–516. [Google Scholar] [CrossRef] [PubMed]
- Carr, A.C.; Spencer, E.; Mackle, D.; Hunt, A.; Judd, H.; Mehrtens, J.; Parker, K.; Stockwell, Z.; Gale, C.; Beaumont, M.; et al. The effect of conservative oxygen therapy on systemic biomarkers of oxidative stress in critically ill patients. Free Radic. Biol. Med. 2020, 160, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Carr, A.C.; Spencer, E.; Dixon, L.; Chambers, S.T. Patients with Community Acquired Pneumonia Exhibit Depleted Vitamin C Status and Elevated Oxidative Stress. Nutrients 2020, 12, 1318. [Google Scholar] [CrossRef]
- Galley, H.F.; Howdle, P.D.; Walker, B.E.; Webster, N.R. The Effects of Intravenous Antioxidants in Patients With Septic Shock. Free Radic. Biol. Med. 1997, 23, 768–774. [Google Scholar] [CrossRef]
- Hemilä, H.; Chalker, E. Vitamin C may reduce the duration of mechanical ventilation in critically ill patients: A meta-regression analysis. J. Intensiv Care 2020, 8, 15. [Google Scholar] [CrossRef]
- Hemilä, H.; Chalker, E. Vitamin C Can Shorten the Length of Stay in the ICU: A Meta-Analysis. Nutrients 2019, 11, 708. [Google Scholar] [CrossRef]
- Siow, W.T.; Liew, M.F.; Shrestha, B.R.; Muchtar, F.; See, K.C. Managing COVID-19 in resource-limited settings: Critical care considerations. Crit. Care 2020, 24, 167. [Google Scholar] [CrossRef]
- Carr, A.C.; Rowe, S. Factors Affecting Vitamin C Status and Prevalence of Deficiency: A Global Health Perspective. Nutrients 2020, 12, 1963. [Google Scholar] [CrossRef]
- Rowe, S.; Carr, A.C. Global Vitamin C Status and Prevalence of Deficiency: A Cause for Concern? Nutrients 2020, 12, 2008. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).