Anxiety and Depression in Women with Polycystic Ovary Syndrome
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Group
- Increased serum concentration of androgens (hyperandrogenemia) or the presence of clinical signs related to androgen excess (hyperandrogenism);
- Oligo- or anovulation;
- Ultrasonographic-feature characteristics of polycystic ovaries.
2.2. Hospital Anxiety and Depression Scale (HADS)
2.3. Ego-Resiliency Scale
2.4. Coping Orientation to Problems Experiences Questionnaire (Mini-COPE)
- Active coping, which encompasses 3 strategies: Active coping, Planning, Positive reinterpretation;
- Seeking support, which encompasses 2 strategies: Seeking emotional support, Seeking instrumental support;
- Helplessness, which encompasses 3 strategies: Psychoactive substance use, Restraint, Self-blame;
- Avoidant coping, which encompasses 3 strategies: Dealing with something else, Denial, Venting.
2.5. Statistical Methods
- Pearson’s chi-square test to compare the socio-demographic characteristics between the PCOS group and the control group, and the severity of anxiety and depression symptoms (measured as none, mild, moderate, or severe) between the PCOS group and the control group;
- Student’s t-test to compare ego-resiliency, the frequency of using stress-coping strategies, the severity of anxiety and depression symptoms (in scores) between the PCOS group and the control group, the severity of anxiety and depression within two levels of education, place of residence (urban and rural), single or married status, and presence of children;
- F test analysis of variance to compare ego-resiliency, and the severity of anxiety and depression (in scores) between three age groups, four types of employment, and four BMI groups.
3. Results
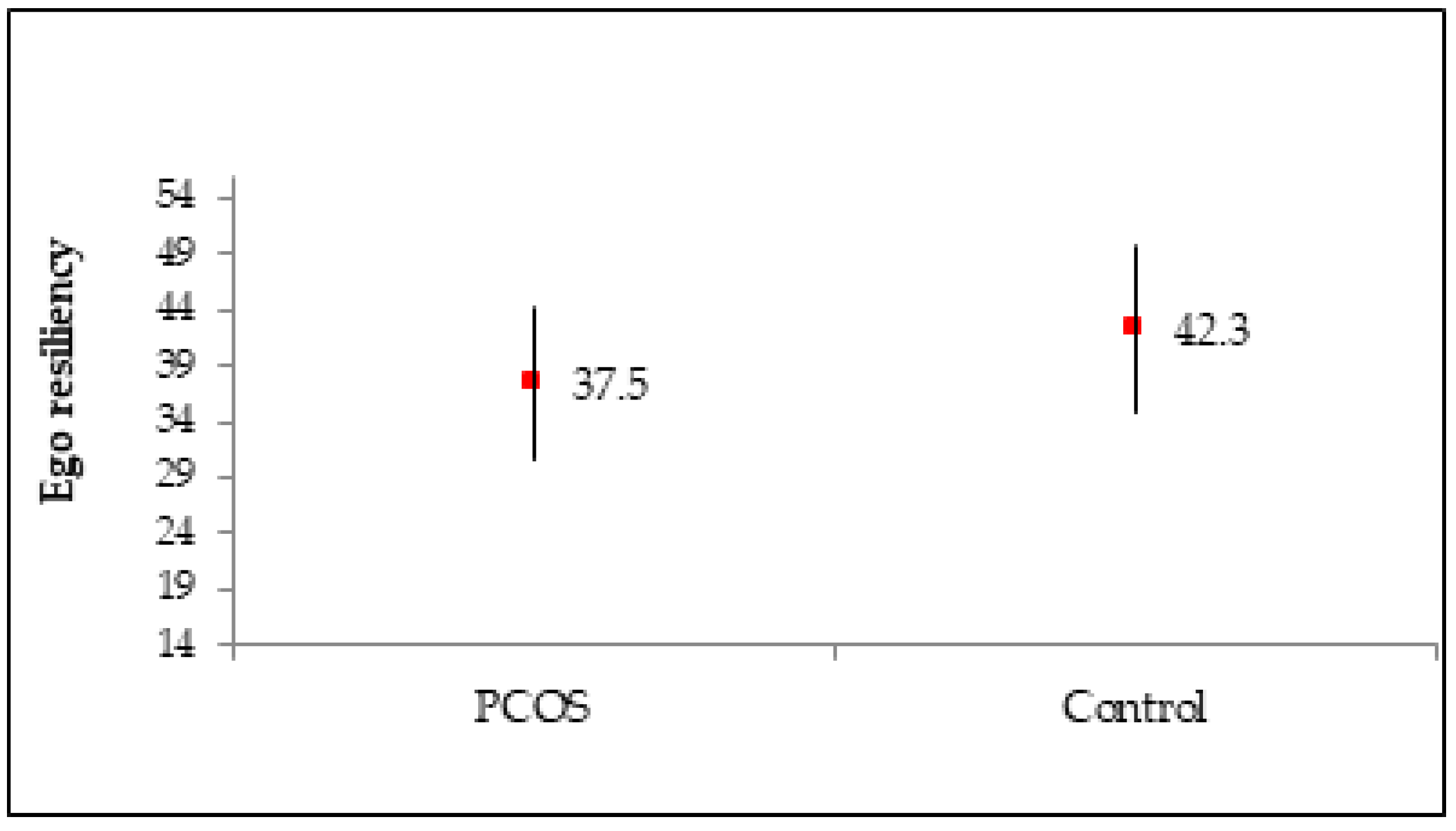
- the higher their ego-resiliency (r = −0.295, p < 0.001 and r = −0.499, p < 0.001, respectively);
- the more often they used some active strategies (Active coping, Planning, Positive reinterpretation, Seeking emotional support, and Humor) to cope with distress (r < 0, p < 0.05);
- the less often they used some passive strategies (Self-blame, Dealing with something else, Denial, and Venting) to cope with distress (r > 0, p < 0.05).
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nidhi, R.; Padmalatha, V.; Nagarathna, R.; Amritanshu, R. Prevalence of Polycystic Ovarian Syndrome in Indian Adolescents. J. Pediatric Adolesc. Gynecol. 2011, 24, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Escobar-Morreale, H.F. Polycystic ovary syndrome: Definition, aetiology, diagnosis and treatment. Nat. Rev. Endocrinol. 2018, 14, 270–284. [Google Scholar] [CrossRef] [PubMed]
- The Amsterdam ESHRE/ASRM-Sponsored 3rd PCOS Consensus Workshop Group. Consensus on women’s health aspects of polycystic ovary syndrome (PCOS). Hum. Reprod. 2012, 27, 14–24. [Google Scholar] [CrossRef] [PubMed]
- Brutocao, C.; Zaiem, F.; Alsawas, M.; Morrow, A.S.; Murad, M.H.; Javed, A. Psychiatric disorders in women with polycystic ovary syndrome: A systematic review and meta-analysis. Endocrine 2018, 62, 318–325. [Google Scholar] [CrossRef]
- Fatemeh, B.; Shahideh, J.S.; Negin, M. Health related quality of life and psychological parameters in different polycystic ovary syndrome phenotypes: A comparative cross-sectional study. J. Ovarian Res. 2021, 14, 57. [Google Scholar] [CrossRef]
- Ali, A.T. Polycystic ovary syndrome and metabolic syndrome. Ceska Gynekol. 2015, 80, 279–289. [Google Scholar]
- Roos, N.; Kieler, H.; Sahlin, L.; Ekman-Ordeberg, G.; Falconer, H.; Stephansson, O. Risk of adverse pregnancy outcomes in women with polycystic ovary syndrome: Population based cohort study. BMJ 2011, 343, d6309. [Google Scholar] [CrossRef] [Green Version]
- Farrell, K.; Antoni, M.H. Insulin resistance, obesity, inflammation, and depression in polycystic ovary syndrome: Biobehavioral mechanisms and interventions. Fertil. Steril. 2010, 94, 1565–1574. [Google Scholar] [CrossRef] [Green Version]
- Gholinezhad, M.; Golsorkhtabaramiri, M.; Esmaeilzadeh, S.; Ghanbarpour, A. Insulin resistance and adverse metabolic profile in overweight/obese and normal weight of young women with polycystic ovary syndrome. Casp. J. Intern. Med. 2018, 9, 260–267. [Google Scholar]
- Legro, R.S.; Arslanian, S.A.; Ehrmann, D.A.; Hoeger, K.M.; Murad, M.H.; Pasquali, R.; Welt, C.K. Diagnosis and Treatment of Polycystic Ovary Syndrome: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2013, 98, 4565–4592. [Google Scholar] [CrossRef] [Green Version]
- Conway, C.M. Editorial: “Old lamps for new”. Br. J. Anaesth. 1975, 47, 811–812. [Google Scholar] [PubMed]
- Papalou, O.; Diamanti-Kandarakis, E. The role of stress in PCOS. Expert Rev. Endocrinol. Metab. 2017, 12, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Livadas, S.; Chaskou, S.; Kandaraki, A.A.; Skourletos, G.; Economou, F.; Christou, M.; Boutzios, G.; Karachalios, A.; Zerva, A.; Xyrafis, X.; et al. Anxiety is associated with hormonal and metabolic profile in women with polycystic ovarian syndrome: Anxiety and hormonal/metabolic profile in PCOS. Clin. Endocrinol. 2011, 75, 698–703. [Google Scholar] [CrossRef] [PubMed]
- Quinn, M.; Shinkai, K.; Pasch, L.; Kuzmich, L.; Cedars, M.; Huddleston, H. Prevalence of androgenic alopecia in patients with polycystic ovary syndrome and characterization of associated clinical and biochemical features. Fertil. Steril. 2014, 101, 1129–1134. [Google Scholar] [CrossRef]
- Borghi, L.; Leone, D.; Vegni, E.; Galiano, V.; Lepadatu, C.; Sulpizio, P.; Garzia, E. Psychological distress, anger and quality of life in polycystic ovary syndrome: Associations with biochemical, phenotypical and socio-demographic factors. J. Psychosom. Obstet. Gynecol. 2018, 39, 128–137. [Google Scholar] [CrossRef]
- Benson, S.; Hahn, S.; Tan, S.; Janssen, O.E.; Schedlowski, M.; Elsenbruch, S. Maladaptive Coping with Illness in Women with Polycystic Ovary Syndrome. J. Obstet. Gynecol. Neonatal Nurs. 2010, 39, 37–45. [Google Scholar] [CrossRef]
- Karrer-Voegeli, S.; Rey, F.; Reymond, M.J.; Meuwly, J.Y.; Gaillard, R.C.; Gomez, F. Androgen Dependence of Hirsutism, Acne, and Alopecia in Women: Retrospective Analysis of 228 Patients Investigated for Hyperandrogenism. Medicine 2009, 88, 32–45. [Google Scholar] [CrossRef]
- Blay, S.L.; Aguiar, J.; Passos, I.C. Polycystic ovary syndrome and mental disorders: A systematic review and exploratory meta-analysis. Neuropsychiatr. Dis. Treat. 2016, 12, 2895–2903. [Google Scholar] [CrossRef] [Green Version]
- Barry, J.A.; Kuczmierczyk, A.R.; Hardiman, P.J. Anxiety and depression in polycystic ovary syndrome: A systematic review and meta-analysis. Hum. Reprod. 2011, 26, 2442–2451. [Google Scholar] [CrossRef] [Green Version]
- Cooney, L.G.; Lee, I.; Sammel, M.D.; Dokras, A. High prevalence of moderate and severe depressive and anxiety symptoms in polycystic ovary syndrome: A systematic review and meta-analysis. Hum. Reprod. 2017, 32, 1075–1091. [Google Scholar] [CrossRef] [Green Version]
- Teede, H.; Gibson-Helm, M.; Norman, R.J.; Boyle, J. Polycystic Ovary Syndrome: Perceptions and Attitudes of Women and Primary Health Care Physicians on Features of PCOS and Renaming the Syndrome. J. Clin. Endocrinol. Metab. 2014, 99, E107–E111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berni, T.R.; Morgan, C.L.; Berni, E.R.; Rees, D.A. Polycystic Ovary Syndrome Is Associated with Adverse Mental Health and Neurodevelopmental Outcomes. J. Clin. Endocrinol. Metab. 2018, 103, 2116–2125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, R.; Luo, M.; Li, J.; Peng, Y.; Wang, Y.; Liu, B.; Liu, G.; Wang, Y.; Lin, S.; Chen, R. Symptoms of anxiety and depression among Chinese women transitioning through menopause: Findings from a prospective community-based cohort study. Fertil. Steril. 2019, 112, 1160–1171. [Google Scholar] [CrossRef]
- Jedel, E.; Gustafson, D.; Waern, M.; Sverrisdottir, Y.B.; Landén, M.; Janson, P.O.; Labrief, F.; Ohlssong, C.; Stener-Victorindh, E. Sex steroids, insulin sensitivity and sympathetic nerve activity in relation to affective symptoms in women with polycystic ovary syndrome. Psychoneuroendocrinology 2011, 36, 1470–1479. [Google Scholar] [CrossRef] [PubMed]
- Stener-Victorin, E.; Manti, M.; Fornes, R.; Risal, S.; Lu, H.; Benrick, A. Origins and Impact of Psychological Traits in Polycystic Ovary Syndrome. Med. Sci. 2019, 7, 86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dokras, A.; Stener-Victorin, E.; Yildiz, B.O.; Li, R.; Ottey, S.; Shah, D.; Epperson, N.; Teede, H.M.B.B.S. Androgen Excess-Polycystic Ovary Syndrome Society: Position statement on depression, anxiety, quality of life, and eating disorders in polycystic ovary syndrome. Fertil. Steril. 2018, 109, 888–899. [Google Scholar] [CrossRef]
- De Ridder, D.; Schreurs, K. Developing interventions for chronically ill patients. Clin. Psychol. Rev. 2001, 21, 205–240. [Google Scholar] [CrossRef]
- Lahey, B.B. Public health significance of neuroticism. Am. Psychol. 2009, 64, 241–256. [Google Scholar] [CrossRef] [Green Version]
- Damone, A.L.; Joham, A.E.; Loxton, D.; Earnest, A.; Teede, H.J.; Moran, L.J. Depression, anxiety and perceived stress in women with and without PCOS: A community-based study. Psychol. Med. 2019, 49, 1510–1520. [Google Scholar] [CrossRef]
- Light, R.S.; Chilcot, J.; McBride, E. Psychological Distress in Women Living with Polycystic Ovary Syndrome: The Role of Illness Perceptions. Women’s Health Issues 2021, 31, 177–184. [Google Scholar] [CrossRef]
- Kumarapeli, V.; Seneviratne, R.; Wijeyaratne, C. Health-related quality of life and psychological distress in polycystic ovary syndrome: A hidden facet in South Asian women: HRQoL and psychological distress in South Asian women with PCOS. BJOG An. Int. J. Obstet. Gynaecol. 2011, 118, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Simon, W. Motivational factors and the psychotherapeutic change. Psychiatr. Pol. 2008, 42, 335–352. [Google Scholar] [PubMed]
- Benson, S.; Hahn, S.; Tan, S.; Mann, K.; Janssen, O.E.; Schedlowski, M.; Elsenbruch, S. Prevalence and implications of anxiety in polycystic ovary syndrome: Results of an internet-based survey in Germany. Hum. Reprod. 2009, 24, 1446–1451. [Google Scholar] [CrossRef] [PubMed]
- Emeksiz, H.C.; Bideci, A.; Nalbantoğlu, B.; Nalbantoğlu, A.; Çelik, C.; Yulaf, Y.; Çamurdan, M.O.; Cinaz, P. Anxiety and depression states of adolescents with polycystic ovary syndrome. Turk. J. Med. Sci 2018, 48, 531–536. [Google Scholar]
- Hahn, S.; Janssen, O.E.; Tan, S.; Pleger, K.; Mann, K.; Schedlowski, M.; Kimmig, R.; Benson, S.; Balamitsa, E.; Elsenbruch, S. Clinical and psychological correlates of quality-of-life in polycystic ovary syndrome. Eur. J. Endocrinol. 2005, 153, 853–860. [Google Scholar] [CrossRef] [Green Version]
- Abdollahi, L.; Mirghafourvand, M.; Babapour, J.K.; Mohammadi, M. Effectiveness of cognitive-behavioral therapy (CBT) in improving the quality of life and psychological fatigue in women with polycystic ovarian syndrome: A randomized controlled clinical trial. J. Psychosom. Obstet. Gynecol. 2019, 40, 283–293. [Google Scholar] [CrossRef]
- Ogińska–Bulik, N.; Zadworna-Cieślak, M. Rola prężności psychicznej w radzeniu sobie ze stresem związanym z egzaminem maturalnym. Przegląd Badań Eduk. 2015, 2, 7. [Google Scholar] [CrossRef]
- Folkman, S.; Lazarus, R.S.; Dunkel-Schetter, C.; DeLongis, A.; Gruen, R.J. Dynamics of a stressful encounter: Cognitive appraisal, coping, and encounter outcomes. J. Personal. Soc. Psychol. 1986, 50, 992–1003. [Google Scholar] [CrossRef]
- Folkman, S.; Greer, S. Promoting psychological well-being in the face of serious illness: When theory, research and practice inform each other. Psycho-Oncology 2000, 9, 11–19. [Google Scholar] [CrossRef]
- Folkman, S.; Lazarus, R.S. The relationship between coping and emotion: Implications for theory and research. Soc. Sci. Med. 1988, 26, 309–317. [Google Scholar] [CrossRef]
- Lechner, L.; Bolman, C.; van Dalen, A. Definite involuntary childlessness: Associations between coping, social support and psychological distress. Hum. Reprod. 2007, 22, 288–294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sigmon, S.T.; Whitcomb-Smith, S.R.; Rohan, K.J.; Kendrew, J.J. The role of anxiety level, coping styles, and cycle phase in menstrual distress. J. Anxiety Disord. 2004, 18, 177–191. [Google Scholar] [CrossRef]
- Carron, R.; Kooienga, S.; Boyle, D.K.; Alvero, R. Coping in Women with Polycystic Ovary Syndrome: Implications for Practitioners. J. Nurse Pract. 2017, 13, 700–707. [Google Scholar] [CrossRef]
- Basirat, Z.; Faramarzi, M.; Chehrazi, M.; Amiri, M.; Ghofrani, F.; Tajalli, Z. Differences between infertile women with and without PCOS in terms of anxiety, coping styles, personality traits, and social adjustment: A case–control study. Arch. Gynecol. Obstet. 2020, 301, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Beiraghdar, M.; Mehr, A.; Kolahi, L.; Asemi, N.; Mirzaei, M.; Adibi, N. The relationship between quality of life and coping strategies in polycystic ovary syndrome patients. Adv. Biomed. Res. 2015, 4, 168. [Google Scholar] [CrossRef]
- Kwon, T. Social stigma, ego-resilience, and depressive symptoms in adolescent school dropouts. J. Adolesc. 2020, 85, 153–163. [Google Scholar] [CrossRef]
- Ziarko, M.; Mojs, E.; Sikorska, D.; Samborski, W. Coping and Life Satisfaction: Mediating Role of Ego-Resiliency in Patients with Rheumatoid Arthritis. Med. Princ. Pract. 2020, 29, 160–165. [Google Scholar] [CrossRef]
- Taylor, Z.E.; Jones, B.L. Cultural Contributors to Ego-Resiliency and Associations with Depressive Problems in Midwestern Latino Youth. J. Res. Adolesc. 2020, 30, 349–361. [Google Scholar] [CrossRef]
- The Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil. Steril. 2004, 81, 19–25. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [Green Version]
- Mihalca, A.M.; Pilecka, W. The factorial structure and validity of the Hospital Anxiety and Depression Scale (HADS) in Polish adolescents. Psychiatr. Pol. 2015, 49, 1071–1088. [Google Scholar] [CrossRef]
- Block, J.; Kremen, A.M. IQ and Ego-Resiliency: Conceptual and empirical connections and separateness. J. Personal. Soc. Psychol. 1996, 70, 349–361. [Google Scholar] [CrossRef]
- Kaczmarek, Ł. Kwestionariusz Sprężystości Psychicznej—Polska adaptacja Ego Resiliency Scale. Czas. Psychol. 2011, 17, 263–265. [Google Scholar]
- Carver, C.; Scheier, M.; Weintraub, J. Assessing coping strategies: A theoretically based approach. J. Personal. Soc. Psychol. 1989, 56, 267–283. [Google Scholar] [CrossRef]
- Juczyński, Z.; Ogińska-Bulik, N. Narzędzia pomiaru stresu i radzenia sobie ze stresem. PTP Warszawa 2009. [Google Scholar]
- Alur-Gupta, S.; Lee, I.; Chemerinski, A.; Liu, C.; Lipson, J.; Allison, K.; Gallop, R.; Dokras, A. Racial differences in anxiety, depression, and quality of life in women with polycystic ovary syndrome. F S Rep. 2021, 2, 230–237. [Google Scholar]
- Yin, X.; Ji, Y.; Chan, C.L.W.; Chan, C.H.Y. The mental health of women with polycystic ovary syndrome: A systematic review and meta-analysis. Arch. Womens Ment. Health 2021, 24, 11–27. [Google Scholar] [CrossRef]
- Almeshari, W.K.; Alsubaie, A.K.; Alanazi, R.I.; Almalki, Y.A.; Masud, N.; Mahmoud, S.H. Depressive and Anxiety Symptom Assessment in Adults with Polycystic Ovarian Syndrome. Depress. Res. Treat. 2021, 2021, 6652133. [Google Scholar] [CrossRef]
- Alur-Gupta, S.; Chemerinski, A.; Liu, C.; Lipson, J.; Allison, K.; Sammel, M.D.; Dokras, A. Body-image distress is increased in women with polycystic ovary syndrome and mediates depression and anxiety. Fertil. Steril. 2019, 112, 930–938.e1. [Google Scholar] [CrossRef]
- Kogure, G.S.; Ribeiro, V.B.; Lopes, I.P.; Furtado, C.L.M.; Kodato, S.; Silva de Sá, M.F.; Ferriania, R.A.; da Silva Lara, L.A.; dos Reis, R.M. Body image and its relationships with sexual functioning, anxiety, and depression in women with polycystic ovary syndrome. J. Affect. Disord. 2019, 253, 385–393. [Google Scholar] [CrossRef]
- Biringer, E.; Howard, L.M.; Kessler, U.; Stewart, R.; Mykletun, A. Is infertility really associated with higher levels of mental distress in the female population? Results from the North-Trøndelag Health Study and the Medical Birth Registry of Norway. J. Psychosom. Obstet. Gynecol. 2015, 36, 38–45. [Google Scholar] [CrossRef] [Green Version]
- Gameiro, S.; van den Belt-Dusebout, A.W.; Smeenk, J.M.J.; Braat, D.D.M.; van Leeuwen, F.E.; Verhaak, C.M. Women’s adjustment trajectories during IVF and impact on mental health 11–17 years later. Hum. Reprod. 2016, 31, 1788–1798. [Google Scholar] [CrossRef] [Green Version]
- Verma, A.; van Ameijden, E.; Birt, C.; Bocsan, I. Why investigate urban health indicators? Eur. J. Public Health. 2017, 27, 1–3. [Google Scholar] [CrossRef] [Green Version]
- Giardinelli, L.; Innocenti, A.; Benni, L.; Stefanini, M.C.; Lino, G.; Lunardi, C.; Svelto, V.; Afshar, S.; Bovani, R.; Castellini, G.; et al. Depression and anxiety in perinatal period: Prevalence and risk factors in an Italian sample. Arch. Womens Ment. Health 2012, 15, 21–30. [Google Scholar] [CrossRef]
- Rahiminejad, M.E.; Moaddab, A.; Rabiee, S.; Esna-Ashari, F.; Borzouei, S.; Hosseini, S.M. The relationship between clinicobiochemical markers and depression in women with polycystic ovary syndrome. Iran. J. Reprod. Med. 2014, 12, 811–816. [Google Scholar]
- Himelein, M.J.; Thatcher, S.S. Depression and body image among women with polycystic ovary syndrome. J. Health Psychol. 2006, 11, 613–625. [Google Scholar] [CrossRef]
- Lin, H.; Liu, M.; Zhong, D.; Ng, E.H.Y.; Liu, J.; Li, J.; Shi, Y.; Zhang, C.; Wen, X.H.; Mai, Z.F.; et al. The Prevalence and Factors Associated With Anxiety-Like and Depression-Like Behaviors in Women With Polycystic Ovary Syndrome. Front. Psychiatry 2021, 12, 709674. [Google Scholar] [CrossRef]
- Ilska, M.; Przybyła-Basista, H. The role of partner support, ego-resiliency, prenatal attitudes towards maternity and pregnancy in psychological well-being of women in high-risk and low-risk pregnancy. Psychol. Health Med. 2020, 25, 630–638. [Google Scholar] [CrossRef]
- Özenli, Y.; Haydardedeoglu, B.; Micozkadıoğlu, I.; Şimşek, E.; Kılıçdağ, E.; Bağış, T. Anxiety, depression and ways of coping skills in women with polycystic ovary syndrome: A controlled study. J Turk. Ger. Gynecol. Assoc. 2008, 29, 190–193. [Google Scholar]
- Simon, S.; Keitel, M.; Bigony, C.; Park-Taylor, J. Psychological distress in women with polycystic ovary syndrome: The role of attachment and coping. Psychol. Health Med. 2021, 26, 735–744. [Google Scholar] [CrossRef]
- Kennedy, P.; Duff, J.; Evans, M.; Beedie, A. Coping effectiveness training reduces depression and anxiety following traumatic spinal cord injuries. Br. J. Clin. Psychol. 2003, 42, 41–52. [Google Scholar] [CrossRef]
- Chesney, M.A.; Chambers, D.B.; Taylor, J.M.; Johnson, L.M.; Folkman, S. Coping Effectiveness Training for Men Living With HIV: Results From a Randomized Clinical Trial Testing a Group-Based Intervention. Psychosom. Med. 2003, 65, 1038–1046. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Variable | Category | PCOS (N = 230) | Control (N = 199) | p |
|---|---|---|---|---|
| Age groups | 20–25 | 86 (37.39) | 75 (37.69) | 0.949 |
| 26–30 | 102 (44.35) | 90 (45.23) | ||
| 31–40 | 42 (18.26) | 34 (17.09) | ||
| Level of education | secondary | 73 (31.74) | 77 (38.69) | 0.132 |
| tertiary | 157 (68.26) | 122 (61.31) | ||
| Place of residence | urban | 166 (72.17) | 145 (72.86) | 0.873 |
| rural | 64 (27.83) | 54 (27.14) | ||
| Type of employment | student | 48 (20.87) | 48 (24.12) | 0.094 |
| manual job | 46 (20.00) | 36 (18.09) | ||
| non-manual job | 124 (53.91) | 93 (46.73) | ||
| unemployed | 12 (5.22) | 22 (11.06) | ||
| Socioeconomic status | very bad or bad | 4 (1.74) | 0 (0.00) | <0.001 |
| medium | 59 (25.65) | 51 (25.63) | ||
| good | 143 (62.17) | 93 (46.73) | ||
| very good | 24 (10.43) | 55 (27.64) | ||
| Marital status | single | 162 (70.43) | 146 (73.37) | 0.501 |
| married | 68 (29.57) | 53 (26.63) | ||
| Have children | no | 180 (78.26) | 148 (74.37) | 0.344 |
| yes | 50 (21.74) | 51 (25.63) | ||
| BMI | underweight | 6 (2.61) | 15 (7.54) | <0.001 |
| normal weight | 108 (46.96) | 149 (74.87) | ||
| overweight | 59 (25.65) | 30 (15.08) | ||
| obese | 57 (24.78) | 5 (2.51) |
| Factor | Strategy | PCOS (N = 230) | Control (N = 199) | p | |
|---|---|---|---|---|---|
| Active strategies | Active coping | Active coping | 1.6 ± 0.7 | 1.8 ± 0.6 | 0.001 |
| Planning | 1.8 ± 0.6 | 2.0 ± 0.6 | <0.001 | ||
| Positive reinterpretation | 1.1 ± 0.7 | 1.0 ± 0.7 | 0.183 | ||
| Seeking support | Seeking emotional support | 1.8 ± 0.7 | 1.8 ± 0.6 | 0.605 | |
| Seeking instrumental support | 1.7 ± 0.6 | 1.5 ± 0.7 | 0.001 | ||
| Religion | 1.4 ± 0.7 | 1.8 ± 0.8 | <0.001 | ||
| Acceptance | 1.5 ± 0.6 | 1.3 ± 0.6 | 0.001 | ||
| Humor | 0.7 ± 0.5 | 0.8 ± 0.6 | 0.051 | ||
| Passive strategies | Helplessness | Psychoactive substance use | 1.1 ± 0.6 | 0.7 ± 0.6 | <0.001 |
| Restraint | 1.6 ± 0.5 | 1.3 ± 0.5 | <0.001 | ||
| Self-blame | 1.9 ± 0.6 | 1.7 ± 0.6 | 0.002 | ||
| Avoidant coping | Dealing with something else | 1.9 ± 0.7 | 1.7 ± 0.6 | 0.001 | |
| Denial | 1.3 ± 0.6 | 1.2 ± 0.5 | 0.347 | ||
| Venting | 1.5 ± 0.7 | 1.3 ± 0.6 | 0.002 |
| Factor | Strategy | HADS-A | HADS-D | ||||
|---|---|---|---|---|---|---|---|
| r | p | r | p | ||||
| Ego resiliency | −0.295 | <0.001 | −0.499 | <0.001 | |||
| Active strategies | Active coping | Active coping | −0.403 | <0.001 | −0.247 | <0.001 | |
| Planning | −0.140 | 0.034 | −0.179 | 0.006 | |||
| Positive reinterpretation | −0.471 | <0.001 | −0.506 | <0.001 | |||
| Seeking support | Seeking emotional support | −0.209 | 0.001 | −0.266 | <0.001 | ||
| Seeking instrumental support | −0.018 | 0.784 | −0.063 | 0.339 | |||
| Religion | −0.080 | 0.226 | +0.180 | 0.006 | |||
| Acceptance | −0.028 | 0.672 | −0.039 | 0.558 | |||
| Humor | −0.220 | 0.001 | −0.183 | 0.005 | |||
| Passive strategies | Helplessness | Psychoactive substance use | −0.045 | 0.495 | −0.007 | 0.916 | |
| Restraint | 0.010 | 0.882 | −0.020 | 0.769 | |||
| Self−blame | +0.160 | 0.015 | +0.163 | 0.013 | |||
| Avoidant coping | Dealing with something else | +0.157 | 0.017 | +0.244 | <0.001 | ||
| Denial | +0.225 | 0.001 | +0.137 | 0.039 | |||
| Venting | +0.133 | 0.043 | +0.187 | 0.005 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dybciak, P.; Humeniuk, E.; Raczkiewicz, D.; Krakowiak, J.; Wdowiak, A.; Bojar, I. Anxiety and Depression in Women with Polycystic Ovary Syndrome. Medicina 2022, 58, 942. https://doi.org/10.3390/medicina58070942
Dybciak P, Humeniuk E, Raczkiewicz D, Krakowiak J, Wdowiak A, Bojar I. Anxiety and Depression in Women with Polycystic Ovary Syndrome. Medicina. 2022; 58(7):942. https://doi.org/10.3390/medicina58070942
Chicago/Turabian StyleDybciak, Paweł, Ewa Humeniuk, Dorota Raczkiewicz, Jan Krakowiak, Artur Wdowiak, and Iwona Bojar. 2022. "Anxiety and Depression in Women with Polycystic Ovary Syndrome" Medicina 58, no. 7: 942. https://doi.org/10.3390/medicina58070942
APA StyleDybciak, P., Humeniuk, E., Raczkiewicz, D., Krakowiak, J., Wdowiak, A., & Bojar, I. (2022). Anxiety and Depression in Women with Polycystic Ovary Syndrome. Medicina, 58(7), 942. https://doi.org/10.3390/medicina58070942








