Scar-Free Laparoscopy in BRCA-Mutated Women
Abstract
:1. Introduction
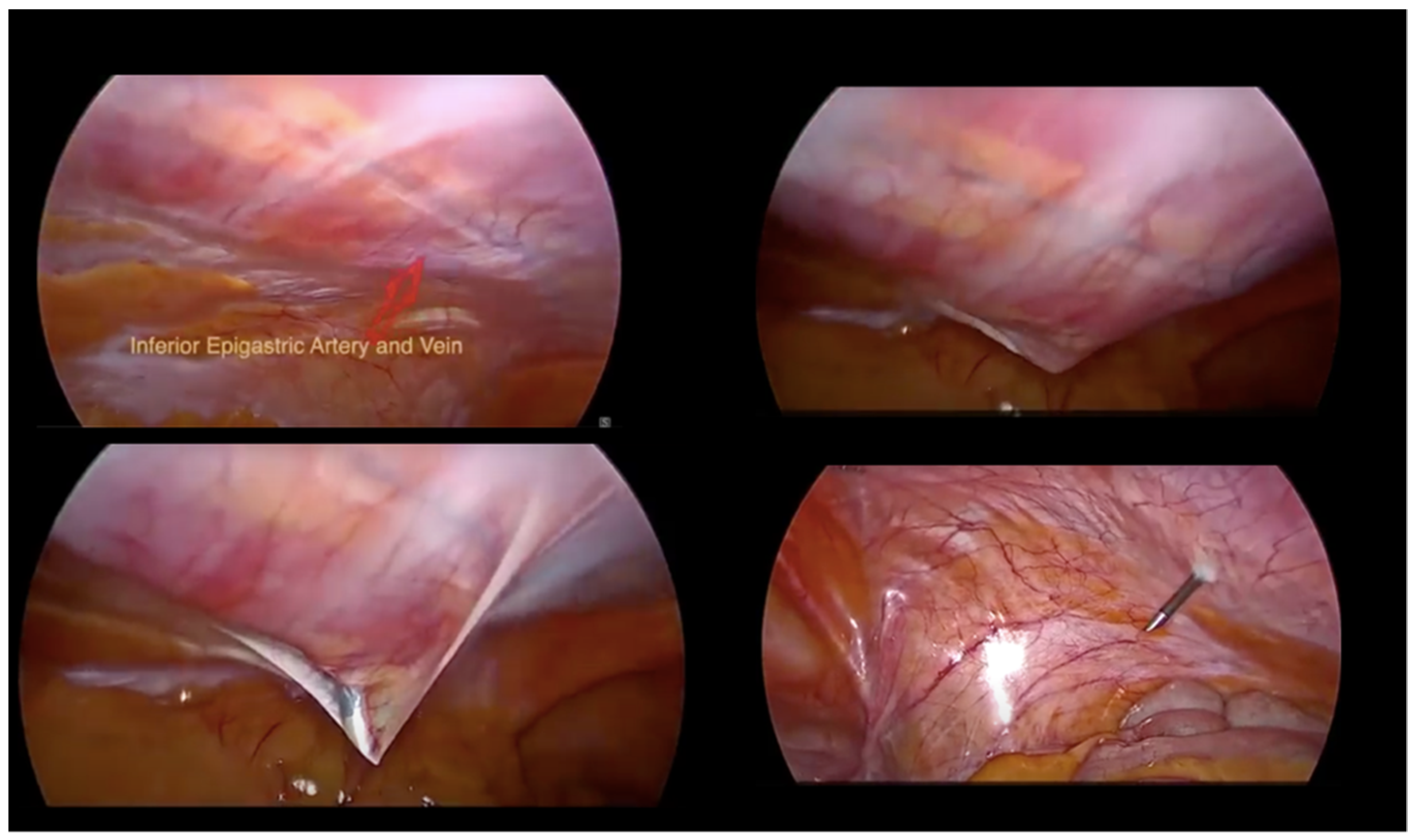
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kuchenbaecker, K.B.; Hopper, J.L.; Barnes, D.R.; Phillips, K.-A.; Mooij, T.M.; Roos-Blom, M.-J.; Jervis, S.; van Leeuwen, F.E.; Milne, R.L.; Andrieu, A.N.; et al. Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. JAMA 2017, 317, 2402–2416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Genetic/FamilialHigh-Risk Assessment: Breast, Ovarian, and Pancreatic Version 1.2022—11 August 2021. NCCN.org. Available online: https://www.nccn.org/professionals/physician_gls/pdf/genetics_bop.pdf (accessed on 24 November 2021).
- Metcalfe, K.A.; Price, M.A.; Mansfield, C.; Hallett, D.C.; Lindeman, G.J.; Fairchild, A.; Posner, J.; Friedman, S.; Snyder, C.; Kathleen Cunningham Foundation Consortium for Research into Familial Breast Cancer; et al. Predictors of long-term cancer-related distress among female BRCA1 and BRCA2 mutation carriers without a cancer diagnosis: An international analysis. Br. J. Cancer 2020, 123, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Dowdy, S.C.; Stefanek, M.; Hartmann, L.C. Surgical risk reduction: Prophylactic salpingo-oophorectomy and prophylactic mastectomy. Am. J. Obstet. Gynecol. 2004, 191, 1113–1123. [Google Scholar] [CrossRef] [PubMed]
- Pinsky, P.F.; Yu, K.; Kramer, B.S.; Black, A.; Buys, S.S.; Partridge, E.; Gohagan, J.; Berg, C.D.; Prorok, P.C. Extended mortality results for ovarian cancer screening in the PLCO trial with median 15years follow-up. Gynecol. Oncol. 2016, 143, 270–275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Powell, C.B.; Alabaster, A.; Le, A.; Stoller, N.; Armstrong, M.A.; Raine-Bennett, T. Sexual function, menopausal symptoms, depression and cancer worry in women with BRCA mutations. Psychooncology 2020, 29, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Siddaiah-Subramanya, M.; Tiang, K.W.; Nyandowe, M. A new era of minimally invasive surgery: Progress and development of major technical innovations in general surgery over the last decade. Surg. J. 2017, 3, e163–e166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lima, D.L.; Carvalho, G.L.; Cordeiro, R.N. Twenty years of mini-laparoscopy in Brazil: What we have learned so far. J. Minim. Access Surg. 2021, 17, 271–273. [Google Scholar] [CrossRef] [PubMed]
- Alexandre, M.; Black, J.; Whicker, M.; Minkin, M.J.; Ratner, E. The management of sexuality, intimacy, and menopause symptoms (SIMS) after prophylactic bilateral salpingo-oophorectomy: How to maintain sexual health in “previvors”. Maturitas 2017, 105, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Domchek, S.M.; Friebel, T.M.; Singer, C.F.; Evans, D.G.; Lynch, H.T.; Isaacs, C.; Garber, J.E.; Neuhausen, S.L.; Matloff, E.; Eeles, R.; et al. Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA 2010, 304, 967–975. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D'Alonzo, M.; Piva, E.; Pecchio, S.; Liberale, V.; Modaffari, P.; Ponzone, R.; Biglia, N. Satisfaction and Impact on Quality of Life of Clinical and Instrumental Surveillance and Prophylactic Surgery in BRCA-mutation Carriers. Clin. Breast Cancer 2018, 18, e1361–e1366. [Google Scholar] [CrossRef] [PubMed]
- Romano, F.; Legge, F.; Scambia, G.; Guido, M. Nerve-Sparing Laparoscopic Colposacropexy Using a Percutaneous Surgical System: A Case Report. J. Minim. Invasive Gynecol. 2017, 24, 536–537. [Google Scholar] [CrossRef] [PubMed]
- Rossitto, C.; Cianci, S.; Alletti, S.G.; Perrone, E.; Pizzacalla, S.; Scambia, G. Laparoscopic, minilaparoscopic, single-port and percutaneous hysterectomy: Comparison of perioperative outcomes of minimally invasive approaches in gynecologic surgery. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 216, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Ghezzi, F.; Uccella, S.; Casarin, J.; Cromi, A. Microlaparoscopic bilateral adnexectomy: A 3-mm umbilical port and a pair of 2-mm ancillary trocars served as conduits. Am. J. Obstet. Gynecol. 2014, 210, 279e1. [Google Scholar] [CrossRef] [PubMed]
- Fanfani, F.; Fagotti, A.; Rossitto, C.; Gagliardi, M.L.; Ercoli, A.; Gallotta, V.; Alletti, S.G.; Monterossi, G.; Turco, L.C.; Scambia, G. Laparoscopic, minilaparoscopic and single-port hysterectomy: Perioperative outcomes. Surg. Endosc. 2012, 26, 3592–3596. [Google Scholar] [CrossRef] [PubMed]
- Fanfani, F.; Fagotti, A.; Gagliardi, M.L.; Monterossi, G.; Rossitto, C.; Costantini, B.; Alletti, S.G.; Vizzielli, G.; Ercoli, A.; Scambia, G. Minilaparoscopic versus single-port total hysterectomy: A randomized trial. J. Minim. Invasive Gynecol. 2013, 20, 192–197. [Google Scholar] [CrossRef] [PubMed]
- Gueli Alletti, S.; Perrone, E.; Cretì, A.; Cianci, S.; Uccella, S.; Fedele, C.; Fanfani, F.; Palmieri, S.; Fagotti, A.; Scambia, G.; et al. Feasibility and perioperative outcomes of percutaneous-assisted laparoscopic hysterectomy: A multicentric Italian experience. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 245, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Ghezzi, F.; Fanfani, F.; Malzoni, M.; Uccella, S.; Fagotti, A.; Cosentino, F.; Cromi, A.; Scambia, G. Minilaparoscopic radical hysterectomy for cervical cancer: Multi-institutional experience in comparison with conventional laparoscopy. Eur. J. Surg. Oncol. 2013, 39, 1094–1100. [Google Scholar] [CrossRef] [PubMed]
- Misirlioglu, S.; Giray, B.; Vatansever, D.; Arslan, T.; Urman, B.; Taskiran, C. Mini-plus percutaneous setting in total laparoscopic hysterectomy. Minim. Invasive Ther. Allied Technol. 2020, 31, 284–290. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Restaino, S.; Finelli, A.; Pellecchia, G.; Biasioli, A.; Mauro, J.; Ronsini, C.; Martina, M.d.; Arcieri, M.; Della Corte, L.; Sorrentino, F.; et al. Scar-Free Laparoscopy in BRCA-Mutated Women. Medicina 2022, 58, 943. https://doi.org/10.3390/medicina58070943
Restaino S, Finelli A, Pellecchia G, Biasioli A, Mauro J, Ronsini C, Martina Md, Arcieri M, Della Corte L, Sorrentino F, et al. Scar-Free Laparoscopy in BRCA-Mutated Women. Medicina. 2022; 58(7):943. https://doi.org/10.3390/medicina58070943
Chicago/Turabian StyleRestaino, Stefano, Angelo Finelli, Giulia Pellecchia, Anna Biasioli, Jessica Mauro, Carlo Ronsini, Monica della Martina, Martina Arcieri, Luigi Della Corte, Felice Sorrentino, and et al. 2022. "Scar-Free Laparoscopy in BRCA-Mutated Women" Medicina 58, no. 7: 943. https://doi.org/10.3390/medicina58070943
APA StyleRestaino, S., Finelli, A., Pellecchia, G., Biasioli, A., Mauro, J., Ronsini, C., Martina, M. d., Arcieri, M., Della Corte, L., Sorrentino, F., Driul, L., & Vizzielli, G. (2022). Scar-Free Laparoscopy in BRCA-Mutated Women. Medicina, 58(7), 943. https://doi.org/10.3390/medicina58070943










