The Impact of Three-Dimensional Printer Technology on the Accuracy of Dental Implant Models
Abstract
:1. Introduction
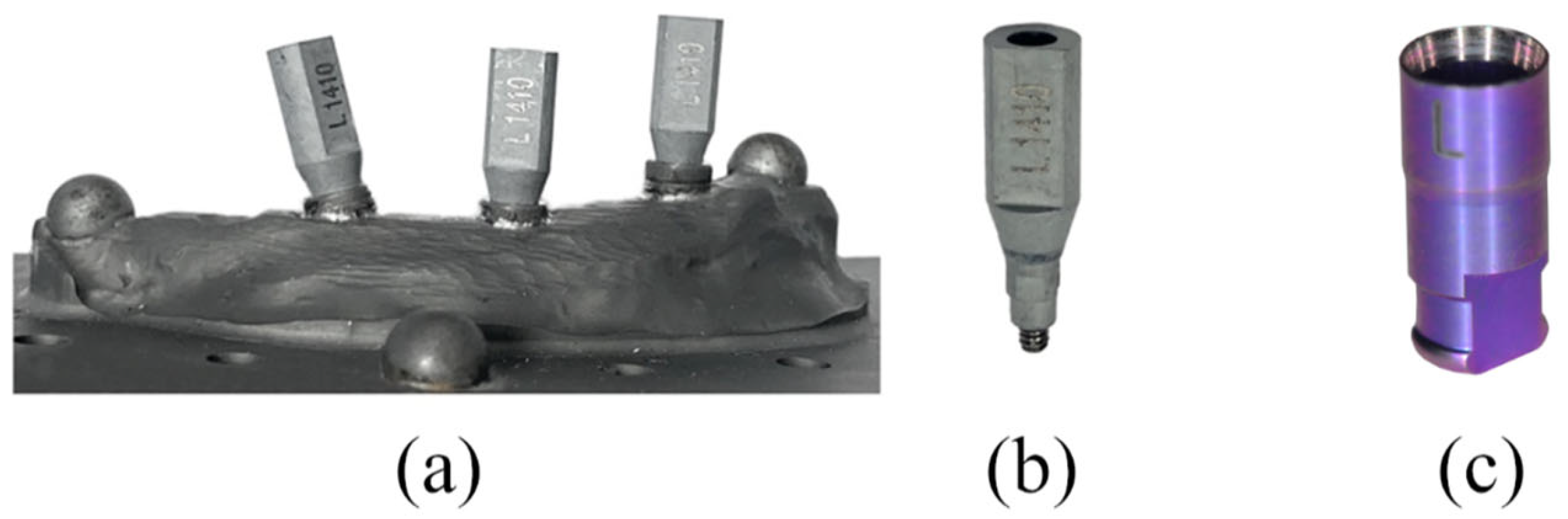
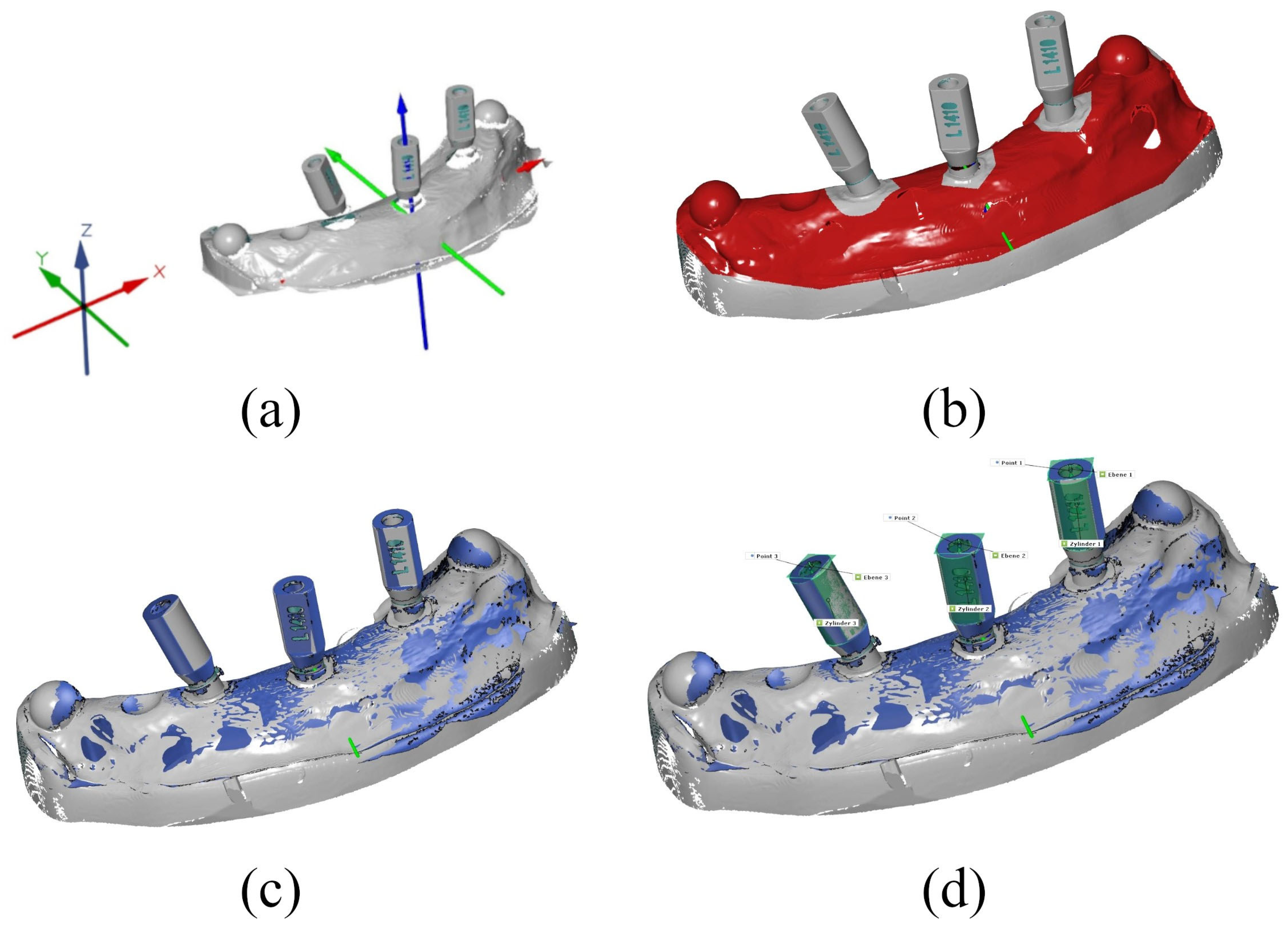
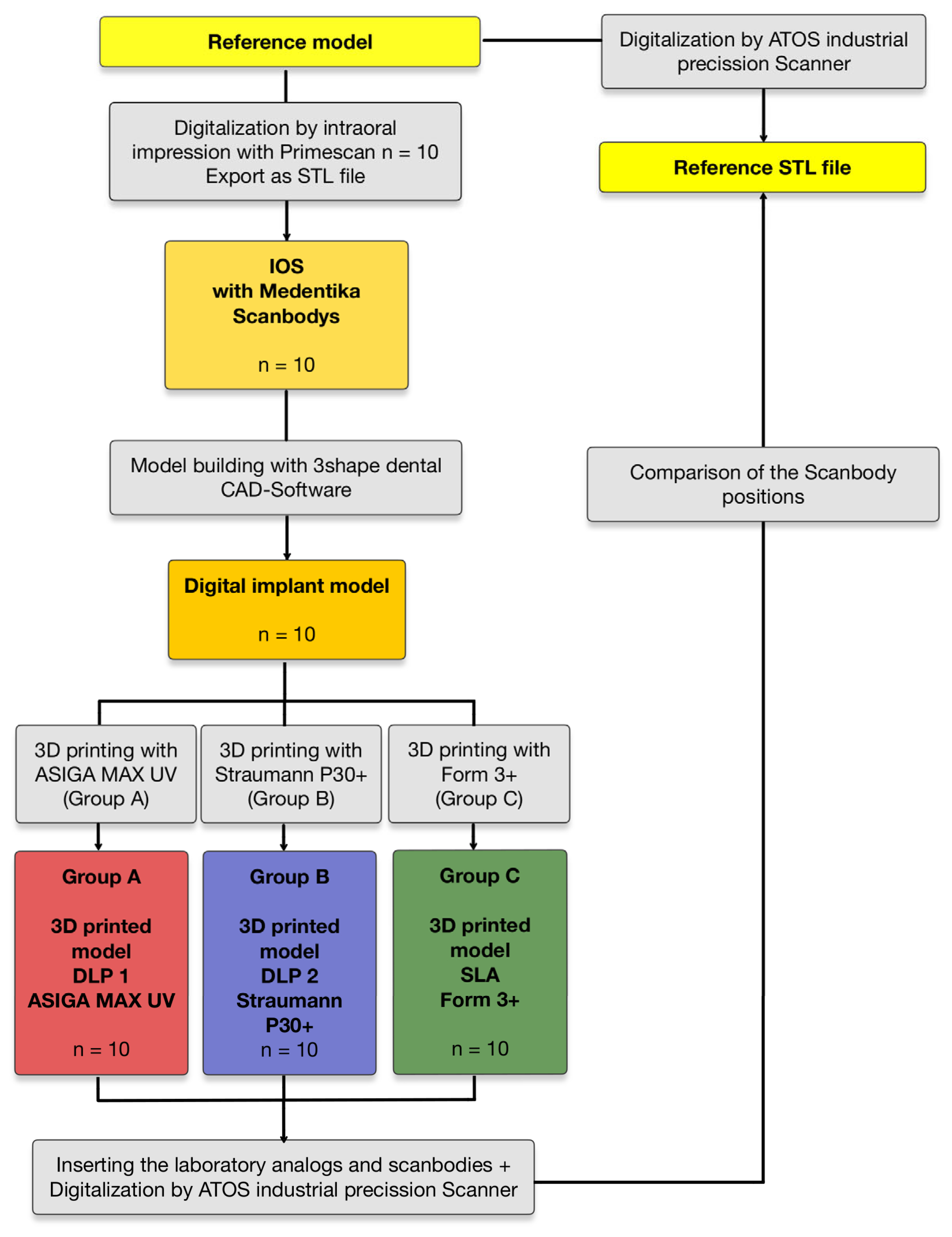
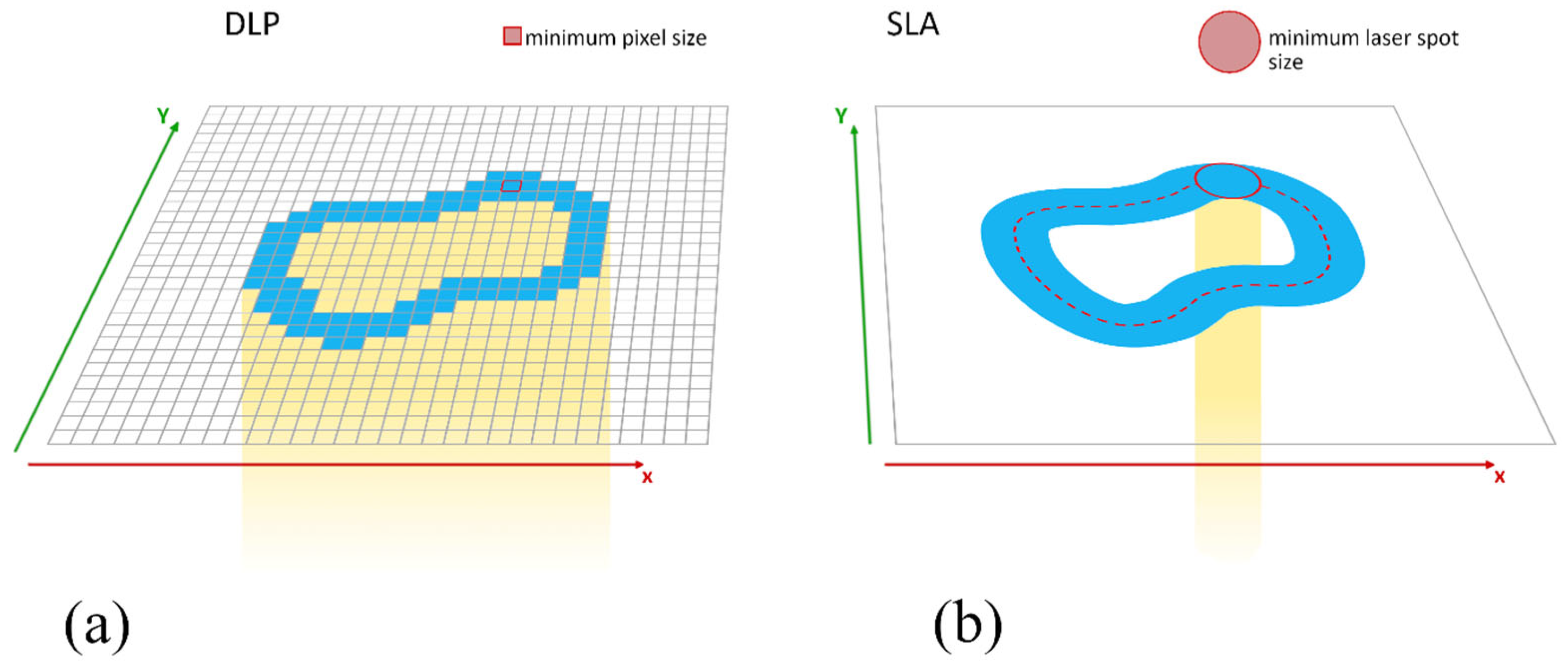
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
- The technology of the printer used has a significant influence on the accuracy of 3D-printed implant models (p < 0.001).
- The two DLP printers examined show mostly higher trueness, (0.07 ± 0.02 mm) and (0.12 ± 0.13 mm), respectively, than the SLA printer examined (0.26 ± 0.17 mm).
- The DLP printer P30 shows very good reproducibility in its results and can be recommended for the fabrication of implant models.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Buser, D.; Sennerby, L.; De Bruyn, H. Modern implant dentistry based on osseointegration: 50 years of progress, current trends and open questions. Periodontology 2000 2017, 73, 7–21. [Google Scholar] [CrossRef] [PubMed]
- Hebel, K.; Gajjar, R.; Hofstede, T. Single-tooth replacement: Bridge vs. implant-supported restoration. J. Can. Dent. Assoc. 2000, 66, 435–438. [Google Scholar]
- Lee, D.J.; Saponaro, P.C. Management of Edentulous Patients. Dent. Clin. N. Am. 2019, 63, 249–261. [Google Scholar]
- Sailer, I.; Karasan, D.; Todorovic, A.; Ligoutsikou, M.; Pjetursson, B.E. Prosthetic failures in dental implant therapy. Periodontology 2000 2022, 88, 130–144. [Google Scholar] [CrossRef] [PubMed]
- Papaspyridakos, P.; Chen, C.J.; Gallucci, G.O.; Doukoudakis, A.; Weber, H.P.; Chronopoulos, V. Accuracy of implant impressions for partially and completely edentulous patients: A systematic review. Int. J. Oral Maxillofac. Implants 2014, 29, 836–845. [Google Scholar]
- Matta, R.E.; Adler, W.; Wichmann, M.; Heckmann, S.M. Accuracy of impression scanning compared with stone casts of implant impressions. J. Prosthet. Dent. 2017, 117, 507–512. [Google Scholar] [CrossRef]
- De Angelis, P.; Manicone, P.F.; De Angelis, S.; Grippaudo, C.; Gasparini, G.; Liguori, M.G.; Camodeca, F.; Piccirillo, G.B.; Desantis, V.; D’Amato, G.; et al. Patient and Operator Centered Outcomes in Implant Dentistry: Comparison between Fully Digital and Conventional Workflow for Single Crown and Three-Unit Fixed-Bridge. Materials 2020, 13, 2781. [Google Scholar] [CrossRef]
- Siqueira, R.; Galli, M.; Chen, Z.; Mendonça, G.; Meirelles, L.; Wang, H.L.; Chan, H.L. Intraoral scanning reduces procedure time and improves patient comfort in fixed prosthodontics and implant dentistry: A systematic review. Clin. Oral. Investig. 2021, 25, 6517–6531. [Google Scholar]
- Richert, R.; Goujat, A.; Venet, L.; Viguie, G.; Viennot, S.; Robinson, P.; Farges, J.C.; Fages, M.; Ducret, M. Intraoral Scanner Technologies: A Review to Make a Successful Impression. J. Healthc. Eng. 2017, 2017, 8427595. [Google Scholar]
- Marques, S.; Ribeiro, P.; Falcão, C.; Lemos, B.F.; Ríos-Carrasco, B.; Ríos-Santos, J.V.; Herrero-Climent, M. Digital Impressions in Implant Dentistry: A Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 1020. [Google Scholar] [CrossRef]
- Andriessen, F.S.; Rijkens, D.R.; van der Meer, W.J.; Wismeijer, D.W. Applicability and accuracy of an intraoral scanner for scanning multiple implants in edentulous mandibles: A pilot study. J. Prosthet. Dent. 2014, 111, 186–194. [Google Scholar] [PubMed]
- Kihara, H.; Hatakeyama, W.; Komine, F.; Takafuji, K.; Takahashi, T.; Yokota, J.; Oriso, K.; Kondo, H. Accuracy and practicality of intraoral scanner in dentistry: A literature review. J. Prosthodont. Res. 2020, 64, 109–113. [Google Scholar] [PubMed]
- Kernen, F.R.; Recca, M.; Vach, K.; Nahles, S.; Nelson, K.; Flügge, T.V. In vitro scanning accuracy using different aids for multiple implants in the edentulous arch. Clin. Oral. Implants Res. 2022, 33, 1010–1020. [Google Scholar] [CrossRef] [PubMed]
- Graf, T.; Güth, J.F.; Diegritz, C.; Liebermann, A.; Schweiger, J.; Schubert, O. Efficiency of occlusal and interproximal adjustments in CAD-CAM manufactured single implant crowns—Cast-free vs. 3D printed cast-based. J. Adv. Prosthodont. 2021, 13, 351–360. [Google Scholar]
- Buda, M.; Bratos, M.; Sorensen, J.A. Accuracy of 3-dimensional computer-aided manufactured single-tooth implant definitive casts. J. Prosthet. Dent. 2018, 120, 913–918. [Google Scholar]
- Mata-Mata, S.J.; Donmez, M.B.; Meirelles, L.; Johnston, W.M.; Yilmaz, B. Influence of digital implant analog design on the positional trueness of an analog in additively manufactured models: An in-vitro study. Clin. Implant Dent. Relat. Res. 2022, 24, 821–830. [Google Scholar]
- Rungrojwittayakul, O.; Kan, J.Y.; Shiozaki, K.; Swamidass, R.S.; Goodacre, B.J.; Goodacre, C.J.; Lozada, J.L. Accuracy of 3D Printed Models Created by Two Technologies of Printers with Different Designs of Model Base. J. Prosthodont. 2020, 29, 124–128. [Google Scholar]
- Alshawaf, B.; Weber, H.P.; Finkelman, M.; El Rafie, K.; Kudara, Y.; Papaspyridakos, P. Accuracy of printed casts generated from digital implant impressions versus stone casts from conventional implant impressions: A comparative in vitro study. Clin. Oral. Implants Res. 2018, 29, 835–842. [Google Scholar]
- Revilla-León, M.; Özcan, M. Additive Manufacturing Technologies Used for Processing Polymers: Current Status and Potential Application in Prosthetic Dentistry. J. Prosthodont. 2019, 28, 146–158. [Google Scholar]
- Schweiger, J.; Edelhoff, D.; Güth, J.-F. 3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing. J. Clin. Med. 2021, 10, 2010. [Google Scholar] [CrossRef]
- Jockusch, J.; Özcan, M. Additive manufacturing of dental polymers: An overview on processes, materials and applications. Dent. Mater. J. 2020, 39, 345–354. [Google Scholar] [PubMed]
- van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [PubMed]
- Jeong, Y.G.; Lee, W.S.; Lee, K.B. Accuracy evaluation of dental models manufactured by CAD/CAM milling method and 3D printing method. J. Adv. Prosthodont. 2018, 10, 245–251. [Google Scholar] [PubMed]
- Revilla-León, M.; Gonzalez-Martín, Ó.; Pérez López, J.; Sánchez-Rubio, J.L.; Özcan, M. Position Accuracy of Implant Analogs on 3D Printed Polymer versus Conventional Dental Stone Casts Measured Using a Coordinate Measuring Machine. J. Prosthodont. 2018, 27, 560–567. [Google Scholar]
- Ide, Y.; Nayar, S.; Logan, H.; Gallagher, B.; Wolfaardt, J. The effect of the angle of acuteness of additive manufactured models and the direction of printing on the dimensional fidelity: Clinical implications. Odontology 2017, 105, 108–115. [Google Scholar]
- Puebla, K.; Arcaute, K.; Quintana, R.; Wicker, R.B. Effects of environmental conditions, aging, and build orientations on the mechanical properties of ASTM type I specimens manufactured via stereolithography. Rapid Prototyp. J. 2012, 18, 374–388. [Google Scholar]
- Demirel, M.; Diken Türksayar, A.A.; Donmez, M.B.; Yilmaz, B. Effect of 3D printing technology and print orientation on the trueness of additively manufactured definitive casts with different tooth preparations. J. Dent. 2024, 148, 105244. [Google Scholar] [CrossRef]
- Le, V.; Keßler, A.; Folwaczny, M. Influence of DLP and SLA printer technology on the accuracy of surgical guides for implant dentistry in free-end situations. Int. J. Comput. Dent. 2023, 26, 217–226. [Google Scholar]
- Caussin, E.; Moussally, C.; Le Goff, S.; Fasham, T.; Troizier-Cheyne, M.; Tapie, L.; Dursun, E.; Attal, J.P.; François, P. Vat Photopolymerization 3D Printing in Dentistry: A Comprehensive Review of Actual Popular Technologies. Materials 2024, 17, 950. [Google Scholar] [CrossRef]
- Kropfeld, J.; Berger, L.; Adler, W.; Schulz, K.L.; Motel, C.; Wichmann, M.; Matta, R.E. Impact of Scanbody Geometry and CAD Software on Determining 3D Implant Position. Dent. J. 2024, 12, 94. [Google Scholar] [CrossRef]
- Jin, G.; Shin, S.H.; Shim, J.S.; Lee, K.W.; Kim, J.E. Accuracy of 3D printed models and implant-analog positions according to the implant-analog-holder offset, inner structure, and printing layer thickness: An in-vitro study. J. Dent. 2022, 125, 104268. [Google Scholar] [CrossRef] [PubMed]
- Matta, R.E.; Bergauer, B.; Adler, W.; Wichmann, M.; Nickenig, H.J. The impact of the fabrication method on the three-dimensional accuracy of an implant surgery template. J. Cranio-Maxillofac. Surg. 2017, 45, 804–808. [Google Scholar] [CrossRef] [PubMed]
- Motel, C.; Kirchner, E.; Adler, W.; Wichmann, M.; Matta, R.E. Impact of Different Scan Bodies and Scan Strategies on the Accuracy of Digital Implant Impressions Assessed with an Intraoral Scanner: An In Vitro Study. J. Prosthodont. 2020, 29, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, N.; Osman, R.; Wismeijer, D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J. Prosthet. Dent. 2016, 115, 760–767. [Google Scholar] [CrossRef]
- Park, G.S.; Kim, S.K.; Heo, S.J.; Koak, J.Y.; Seo, D.G. Effects of Printing Parameters on the Fit of Implant-Supported 3D Printing Resin Prosthetics. Materials 2019, 12, 2533. [Google Scholar] [CrossRef]
- Kirby, S.; Pesun, I.; Nowakowski, A.; França, R. Effect of Different Post-Curing Methods on the Degree of Conversion of 3D-Printed Resin for Models in Dentistry. Polymers 2024, 16, 549. [Google Scholar] [CrossRef]
- Chen, Y.; Li, H.; Zhai, Z.; Nakano, T.; Ishigaki, S. Impact of internal design on the accuracy of 3-dimensionally printed casts fabricated by stereolithography and digital light processing technology. J. Prosthet. Dent. 2023, 130, 381.e1–381.e7. [Google Scholar] [CrossRef]
- Etemad-Shahidi, Y.; Qallandar, O.B.; Evenden, J.; Alifui-Segbaya, F.; Ahmed, K.E. Accuracy of 3-Dimensionally Printed Full-Arch Dental Models: A Systematic Review. J. Clin. Med. 2020, 9, 3357. [Google Scholar] [CrossRef]



| Resin 1 IMPRIMO® LC Model Beige (DLP—ASIGA MAX UV) | Resin 2 PRO RESIN, MODEL X (DLP—Straumann P30) | Resin 3 Formlabs Dental Model Resin (SLA—Form 3+) | |
|---|---|---|---|
| composition | alkoxylated bisphenol-A dimethacrylate, phosphine oxide, stabilizers, dyes, and pigments | UDMA, diacrylate, acrylic resin, phosphine oxide | bismethacrylate, methacrylate monomers, ethyl phenylphosphinate |
| layer height | 50 µm | 50 µm | 50 µm |
| build angle | 0° | 0° | 0° |
| mean printing time | 37 min 32 s | 45 min 12 s | 1 h 50 min 8 s |
| printing temperature | 30.0 °C | 35.0 °C | 35.0 °C |
| wavelength | 385 nm | 385 nm | 405 nm |
| light intensity | 11.7 | no available information | 250 mW Laser |
| Group | Mean | SD | Min | Max | ||
|---|---|---|---|---|---|---|
| Group A | ASIGA MAX UV | dXYZ | 0.12 mm | 0.13 mm | 0.03 mm | 0.79 mm |
| DLP 1 | x | 0.06 mm | 0.05 mm | 0.00 mm | 0.21 mm | |
| y | 0.05 mm | 0.03 mm | 0.01 mm | 0.11 mm | ||
| z | 0.06 mm | 0.14 mm | 0.01 mm | 0.78 mm | ||
| Group B | Straumann P30+ | dXYZ | 0.07 mm | 0.02 mm | 0.03 mm | 0.10 mm |
| DLP 2 | x | 0.03 mm | 0.02 mm | 0.00 mm | 0.07 mm | |
| y | 0.04 mm | 0.02 mm | 0.00 mm | 0.08 mm | ||
| z | 0.03 mm | 0.01 mm | 0.00 mm | 0.05 mm | ||
| Group C | Form 3+ | dXYZ | 0.26 mm | 0.17 mm | 0.09 mm | 0.93 mm |
| SLA | x | 0.05 mm | 0.05 mm | 0.00 mm | 0.18 mm | |
| y | 0.17 mm | 0.06 mm | 0.08 mm | 0.37 mm | ||
| z | 0.14 mm | 0.20 mm | 0.01 mm | 0.91 mm |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strunz, A.; Berger, L.; Seidel, A.; Ries, J.; Adler, W.; Wichmann, M.; Matta, R.E. The Impact of Three-Dimensional Printer Technology on the Accuracy of Dental Implant Models. Materials 2025, 18, 1902. https://doi.org/10.3390/ma18091902
Strunz A, Berger L, Seidel A, Ries J, Adler W, Wichmann M, Matta RE. The Impact of Three-Dimensional Printer Technology on the Accuracy of Dental Implant Models. Materials. 2025; 18(9):1902. https://doi.org/10.3390/ma18091902
Chicago/Turabian StyleStrunz, Alexander, Lara Berger, Anna Seidel, Johannes Ries, Werner Adler, Manfred Wichmann, and Ragai Edward Matta. 2025. "The Impact of Three-Dimensional Printer Technology on the Accuracy of Dental Implant Models" Materials 18, no. 9: 1902. https://doi.org/10.3390/ma18091902
APA StyleStrunz, A., Berger, L., Seidel, A., Ries, J., Adler, W., Wichmann, M., & Matta, R. E. (2025). The Impact of Three-Dimensional Printer Technology on the Accuracy of Dental Implant Models. Materials, 18(9), 1902. https://doi.org/10.3390/ma18091902






