Contribution of Food, Energy, Macronutrients and Fiber Consumption Patterns to Obesity and Other Non-Communicable Disease Risks in the Indonesian Population
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Subjects
2.3. Data Collection and Measurements
2.4. Data Analysis
3. Results
3.1. Sociodemographic Characteristics of Participants
3.2. Consumption Patterns
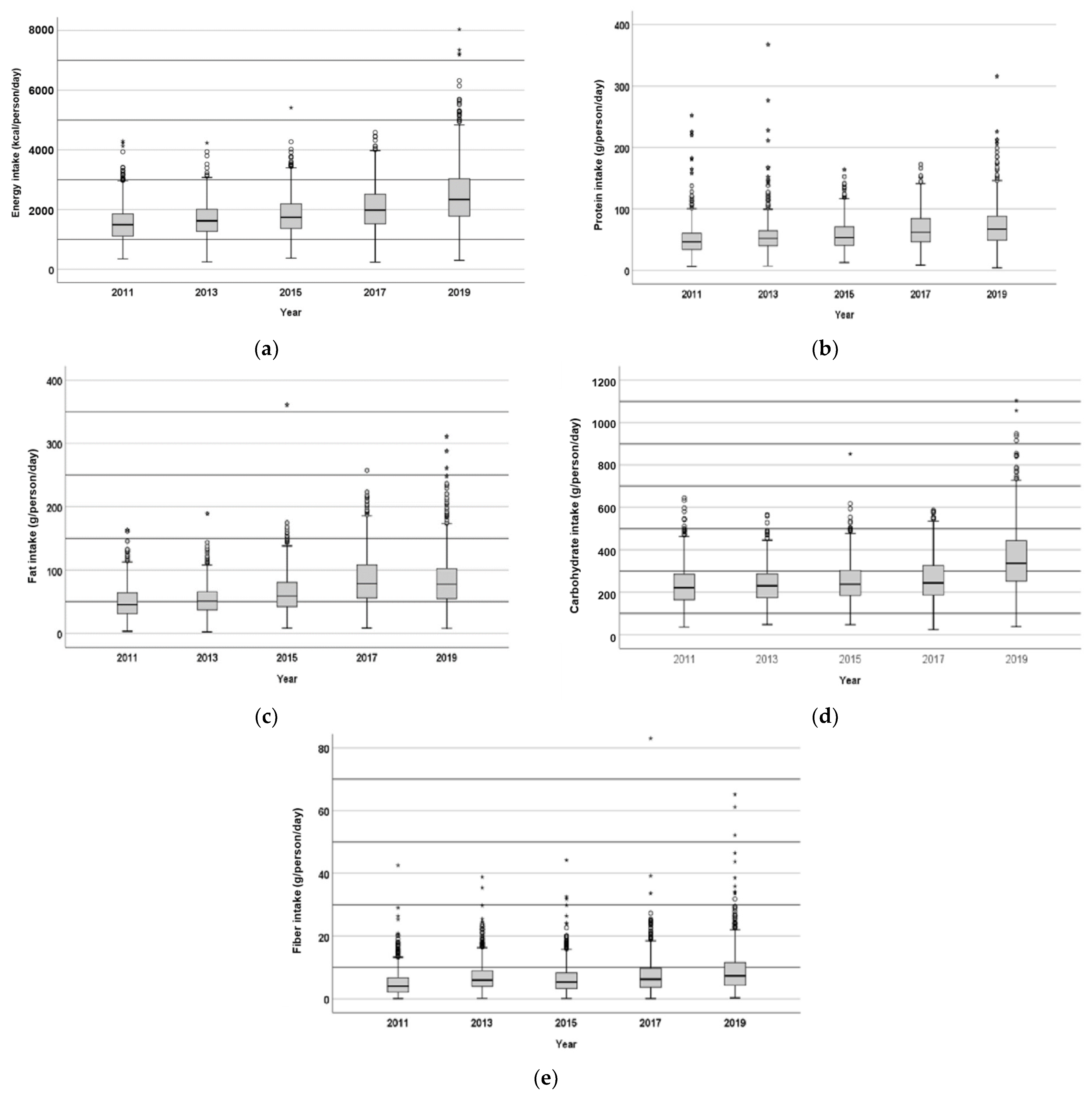
3.3. Energy, Macronutrients and Fiber Intake
3.4. Contribution of Food Groups to Nutrient Intake
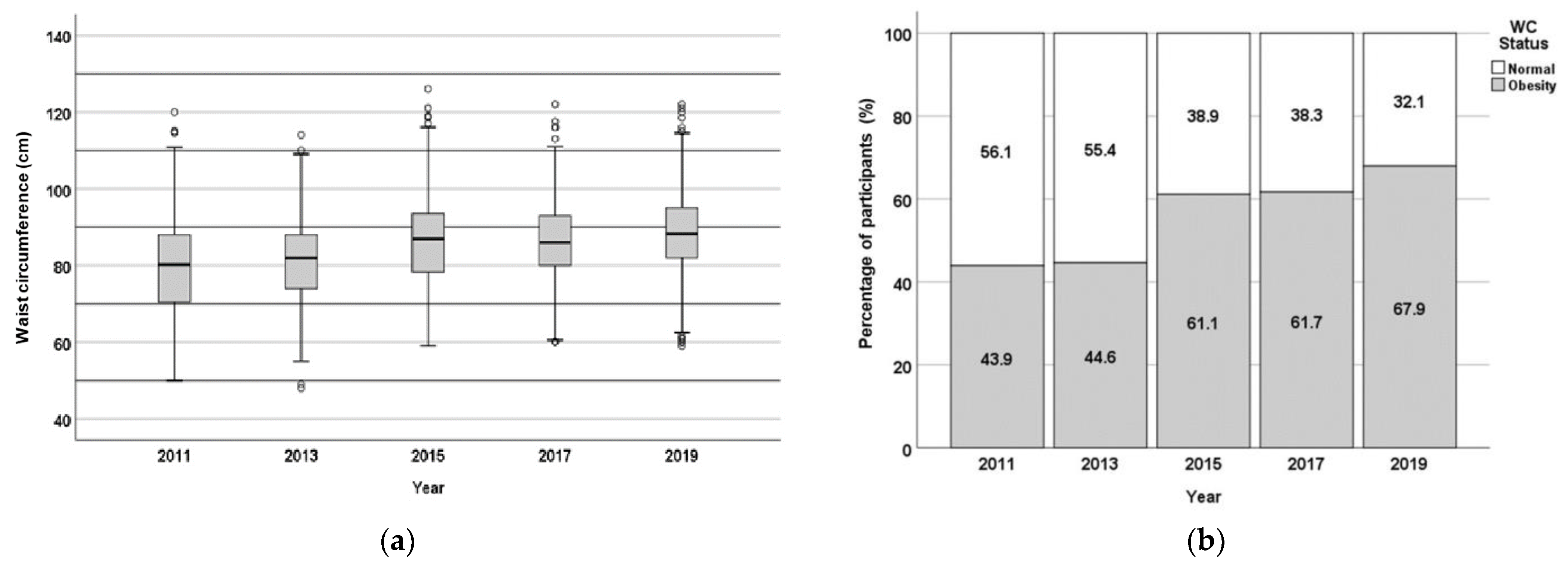
3.5. Obesity as an Early Indication of Non-Communicable Diseases
3.6. Observation of Biomedical Parameters of Non-Communicable Diseases
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mohajan, D.; Mohajan, H.K. Obesity and Its Related Diseases: A New Escalating Alarming in Global Health. J. Innov. Med Res. 2023, 2, 12–23. [Google Scholar] [CrossRef]
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 14 March 2025).
- Gołacki, J.; Matyjaszek-Matuszek, B. Obesity—Standards, Trends and Advances. Adv. Med. Sci. 2024, 69, 208–215. [Google Scholar] [CrossRef]
- Kaptoge, S.; Pennells, L.; De Bacquer, D.; Cooney, M.T.; Kavousi, M.; Stevens, G.; Riley, L.M.; Savin, S.; Khan, T.; Altay, S.; et al. World Health Organization Cardiovascular Disease Risk Charts: Revised Models to Estimate Risk in 21 Global Regions. Lancet Glob. Health 2019, 7, e1332–e1345. [Google Scholar] [CrossRef] [PubMed]
- Damasceno, A. Noncommunicable Disease. In Heart of Africa: Clinical Profile of an Evolving Burden of Heart Disease in Africa; Stewart, S.S., Sliwa, K., Mocumbi, A., Damasceno, A., Ntsekhe., M., Eds.; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2016; pp. 155–157. ISBN 9781118336960. [Google Scholar]
- Kelly, B.; Silveira, S.; Moreira, T.; Oliveira, S.; Andrade, A.; Hermana, H.; Hermsdorff, M.; Oliveira, C.D.; Rosa, B.; Castro, C. Dietary Pattern and Macronutrients Profile on the Variation of Inflammatory Biomarkers: Scientific Update. Cardiol. Res. Pract. 2018, 2018, 4762575. [Google Scholar] [CrossRef]
- Bestari, F.F.; Andarwulan, N.; Palupi, E. Synthesis of Effect Sizes on Dose Response from Ultra-Processed Food Consumption against Various Noncommunicable Diseases. Foods 2023, 12, 4457. [Google Scholar] [CrossRef]
- Crovetto, M.; Sepúlveda, M.J. Relationship between Dietary Energy Intake, Nutritional Status and Cardiovascular Risk in Adults from the Communes of Quellón and Chonchi, Chiloé, Chile. J. Prev. Med. Hyg. 2022, 63, 435–441. [Google Scholar] [CrossRef]
- Pereira, M.; Valado, A. Dietary Fiber in Preventing Non-Communicable Diseases: Predicting Prevented Deaths and Economic Impact through the Use of Algae as a Fiber Source. Recent Prog. Nutr. 2024, 4, 1–11. [Google Scholar] [CrossRef]
- Health Development Policy Agency. Indonesia Health Survey 2023 in Numbers; Health Development Policy Agency: Jakarta, Indonesia, 2024. [Google Scholar]
- Harbuwono, D.S.; Pramono, L.A.; Yunir, E.; Subekti, I. Obesity and Central Obesity in Indonesia: Evidence from a National Health Survey. Med. J. Indones. 2018, 27, 114–120. [Google Scholar] [CrossRef]
- Ministry of Health Republic Indonesia. Hasil Utama Riset Kesehatan Dasar (Key Results of Basic Health Research). 2018. Available online: https://layanandata.kemkes.go.id/katalog-data/riskesdas/ketersediaan-data/riskesdas-2018 (accessed on 14 March 2025).
- Ardiana, M.; Harsoyo, P.M.; Hermawan, H.O.; Sufiyah, I.M.; Firmanda, D.R.; Desita, S.R.; Paramitha, A.D.; Hariftyani, A.S.; Shabrina, F.A.; Triastuti, F. Higher Cardiovascular Risks and Atherogenic Index of Plasma Found in Police Officers of Developing Country in Surabaya, East Java, Indonesia. Clin. Epidemiol. Glob. Health 2022, 17, 101132. [Google Scholar] [CrossRef]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef]
- Lipoeto, N.I.; Wattanapenpaiboon, N.; Malik, A.; Wahlqvist, M.L. The Nutrition Transition in West Sumatra, Indonesia. Asia Pac. J. Clin. Nutr. 2004, 13, 312–316. [Google Scholar] [PubMed]
- Pengpid, S.; Peltzer, K. The Prevalence of Underweight, Overweight/Obesity and Their Related Lifestyle Factors in Indonesia, 2014–2015. AIMS Public Health 2017, 4, 633–649. [Google Scholar] [CrossRef] [PubMed]
- Mahiroh, H.; Astutik, E.; Pratama, R.A. The Association of Body Mass Index, Physical Activity and Hypertension in Indonesia. Jurnal Ners 2019, 14, 16–22. [Google Scholar] [CrossRef]
- Peltzer, K.; Pengpid, S. The Prevalence and Social Determinants of Hypertension among Adults in Indonesia: A Cross-Sectional Population-Based National Survey. Int. J. Hypertens. 2018, 2018, 5610725. [Google Scholar] [CrossRef]
- Anyanwu, O.A.; Folta, S.C.; Zhang, F.F.; Chui, K.; Chomitz, V.R.; Kartasurya, M.I.; Naumova, E.N. A Cross-Sectional Assessment of Dietary Patterns and Their Relationship to Hypertension and Obesity in Indonesia. Curr. Dev. Nutr. 2022, 6, nzac091. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Standard STEPS Instrument. Available online: https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/steps/instrument (accessed on 28 March 2025).
- World Health Organization. Regional Office for the Western Pacific. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment; Health Communications Australia: Sydney, Australia, 2000; Available online: https://iris.who.int/handle/10665/206936 (accessed on 14 March 2025).
- American Diabetes Association Professional Practice Committee. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2022. Diabetes Care 2022, 45, 17–38. [Google Scholar] [CrossRef]
- National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Circulation 2002, 106, 3143–3421. [Google Scholar] [CrossRef]
- Chen, Q.J.; Lai, H.M.; Chen, B.D.; Li, X.M.; Zhai, H.; He, C.H.; Pan, S.; Luo, J.Y.; Gao, J.; Liu, F.; et al. Appropriate LDL-C-to-HDL-C Ratio Cutoffs for Categorization of Cardiovascular Disease Risk Factors among Uygur Adults in Xinjiang, China. Int. J. Environ. Res. Public Health 2016, 13, 235. [Google Scholar] [CrossRef]
- Institute of Nutrition, Mahidol University. ASEAN Food Composition Database ASEANFOODS Regional Centre and INFOODS Regional Database Centre; Institute of Nutrition, Mahidol University: Nakhon Pathom, Thailand, 2014; ISBN 9746644807. [Google Scholar]
- Direktorat Jenderal Kesehatan Masyarakat. Tabel Komposisi Pangan Indonesia 2017; Kementerian Kesehatan RI: Jakarta, Indonesia, 2018; Available online: https://repository.stikespersadanabire.ac.id/assets/upload/files/docs_1634523137.pdf (accessed on 14 March 2025).
- NutriSurvey. Available online: https://nutrisurvey.de/nbs.htm (accessed on 14 March 2025).
- Trumbo, P.; Schlicker, S.; Yates, A.A.; Poos, M. Food and Nutrition Board of the Institute of Medicine, The National Academies. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J. Am. Diet. Assoc. 2002, 102, 1621–1630. [Google Scholar] [CrossRef]
- Khatib, O.M.N. (Ed.) Guidelines for the Prevention, Management and Care of Diabetes Mellitus; (EMRO Technical Publications Series No. 32); World Health Organization Regional Office for the Eastern Mediterranean: Cairo, Egypt, 2006. [Google Scholar]
- Peraturan Badan Pangan Nasional Nomor 11 Tahun 2023 Tentang Pola Pangan Harapan. Available online: https://peraturan.bpk.go.id/Details/307661/peraturan-bapanas-no-11-tahun-2023 (accessed on 14 March 2025).
- Fridman, D.; Makaryus, A.N.; Makaryus, J.N.; Bhanvadia, A.; Erion Qaja, A.M.; McFarlaneQaj, S.I. Diabetes and Coronary Artery Disease—Pathophysiologic Insights and Therapeutic Implications. Intech 2016, 11, 247–260. [Google Scholar] [CrossRef]
- Koch, W.; Karim, M.R.; Marzec, Z.; Miyataka, H.; Himeno, S.; Asakawa, Y. Dietary Intake of Metals by the Young Adult Population of Eastern Poland: Results from a Market Basket Study. J. Trace Elem. Med. Biol. 2016, 35, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Zähringer, J.; Beyerbach, J.; Werner, S.W.; Heseker, H.; Koletzko, B.; Meerpohl, J.J. Total Dietary Fat Intake, Fat Quality, and Health Outcomes: A Scoping Review of Systematic Reviews of Prospective Studies. Ann. Nutr. Metab. 2021, 77, 4–15. [Google Scholar] [CrossRef]
- Khanam, Z.; Shankar, H.; Mishra, C. Macro-Nutrient Intake of Reproductive Age Group Women: Findings of a Community Based Study from Rural Varanasi. Int. J. Community Med. Public Health 2016, 3, 566–575. [Google Scholar] [CrossRef]
- Zhao, Y.; Araki, T. Evaluation of Disparities in Adults’ Macronutrient Intake Status: Results from the China Health and Nutrition 2011 Survey. Nutrients 2021, 13, 3044. [Google Scholar] [CrossRef]
- González-Torres, S.; González-Silva, N.; Pérez-Reyes, Á.; Anaya-Esparza, L.M.; Sánchez-Enríquez, S.; Vargas-Becerra, P.N.; Villagrán, Z.; García-García, M.R. Food Consumption and Metabolic Risks in Young University Students. Int. J. Environ. Res. Public Health 2022, 19, 449. [Google Scholar] [CrossRef]
- Carlsen, H.; Pajari, A.M. Dietary Fiber—A Scoping Review for Nordic Nutrition Recommendations 2023. Food Nutr. Res. 2023, 67, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Baladina, N.; Toiba, H.; Hanani, N.; Suhartini, S.; Widarjono, A. Do Income Levels Affect the Food Consumption Pattern of Households? Evidence from Indonesia. AEFR 2024, 14, 695–711. [Google Scholar] [CrossRef]
- Anindita, R.; Khoiriyah, N.; Sa’Diyah, A.A. Food Consumption Pattern Far Away from Home as a Source of Household Food Protein in Indonesia. IOP Conf. Ser. Earth Environ. Sci. 2022, 1107, 012118. [Google Scholar] [CrossRef]
- Khusun, H.; Februhartanty, J.; Anggraini, R.; Mognard, E.; Alem, Y.; Noor, M.I.; Karim, N.; Laporte, C.; Poulain, J.P.; Monsivais, P.; et al. Animal and Plant Protein Food Sources in Indonesia Differ Across Socio-Demographic Groups: Socio-Cultural Research in Protein Transition in Indonesia and Malaysia. Front. Nutr. 2022, 9, 762459. [Google Scholar] [CrossRef]
- Burke, S.J.; Gibney, M.J.; Dwyer, N.A.O.; Mccarthy, S.N. The Influence of Cereal and Dairy Consumption on the Irish Diet: Implications for Developing Food-Based Dietary Guidelines. Public Health Nutr. 2005, 8, 227–237. [Google Scholar] [CrossRef]
- Auestad, N.; Hurley, J.S.; Fulgoni, V.L.; Schweitzer, C.M. Contribution of Food Groups to Energy and Nutrient Intakes in Five Developed Countries. Nutrients 2015, 7, 4593–4618. [Google Scholar] [CrossRef] [PubMed]
- Laskowski, W.; Górska-Warsewicz, H.; Rejman, K.; Czeczotko, M.; Zwolińska, J. How Important Are Cereals and Cereal Products in the Average Polish Diet? Nutrients 2019, 11, 679. [Google Scholar] [CrossRef] [PubMed]
- Prihatini, S.; Jahari, A.B. Kontribusi Golongan Bahan Makanan Terhadap Konsumsi Energi Dan Protein Rumah Tangga Di Indonesia. Puslitbang Gizi Dan Makanan 2010, 33, 30–41. [Google Scholar]
- Isaura, E.R.; Chen, Y.C.; Yang, S.H. Pathways from Food Consumption Score to Cardiovascular Disease: A Seven-Year Follow-up Study of Indonesian Adults. Int. J. Environ. Res. Public Health 2018, 15, 1567. [Google Scholar] [CrossRef]
- Willems, A.E.M.; Sura-De Jong, M.; Van Beek, A.P.; Nederhof, E.; Van Dijk, G. Effects of Macronutrient Intake in Obesity: A Meta-Analysis of Low-Carbohydrate and Low-Fat Diets on Markers of the Metabolic Syndrome. Nutr. Rev. 2021, 79, 429–444. [Google Scholar] [CrossRef]
- Almaraz, R.S.; Fuentes, M.M.; Milla, S.P.; Plaza, B.L.; Bermejo López, L.M.; Candela, C.G. Indicaciones de Diferentes Tipos de Fibra En Distintas Patologías. Nutr. Hosp. 2015, 31, 2372–2383. [Google Scholar] [CrossRef]
- Karimi, E.; Yarizadeh, H.; Setayesh, L.; Sajjadi, S.F.; Ghodoosi, N.; Khorraminezhad, L.; Mirzaei, K. High Carbohydrate Intakes May Predict More Inflammatory Status than High Fat Intakes in Pre-Menopause Women with Overweight or Obesity: A Cross-Sectional Study. BMC Res. Notes 2021, 14, 279. [Google Scholar] [CrossRef]
- Friedman, M.I.; Sørensen, T.I.A.; Taubes, G.; Lund, J.; Ludwig, D.S. Trapped Fat: Obesity Pathogenesis as an Intrinsic Disorder in Metabolic Fuel Partitioning. Obes. Rev. 2024, 25, e13795. [Google Scholar] [CrossRef]
- Ghanemi, A.; Yoshioka, M.; St-Amand, J. Broken Energy Homeostasis and Obesity Pathogenesis: The Surrounding Concepts. J. Clin. Med. 2018, 7, 453. [Google Scholar] [CrossRef]
- Fatade, Y.A.; Dave, E.K.; Vatsa, N.; Crumbs, T.; Calhoun, A.; Sharma, A.; Shufelt, C.L.; Mehta, P.K. Obesity and Diabetes in Heart Disease in Women. Metab Target Organ Damage M&TOD 2024, 4, 22. [Google Scholar] [CrossRef]
- Yang, K.; Yang, Y.; Xie, Y.; Mao, Y.; Li, X.; Guo, Q. Impact of Macronutrient Composition in Nutrition Shakes on Postprandial Glycemic Response, Appetite, and Food Intake. Food Hydrocoll. 2023, 141, 108685. [Google Scholar] [CrossRef]
- Hasan Entezari, M.; Salehi, M.; Rafieian-Kopaei, M.; Kafeshani, M. Fat and Carbohydrate Proportions Influence on the Insulin Resistance; a Systematic Review and Meta-Analysis on Controlled Clinical Trials. J. Prev. Epidemiol. 2017, 2, e02. [Google Scholar]
- Ailshul, M.D. Energy Balance and Obesity in Man. Nutr. Today 1975, 10, 29–30. [Google Scholar] [CrossRef]
- Temesgen, M.; Ratta, N. Adverse Effect of Fat Intake on Insulin Sensitivity and Associated Risk of Non-Communicable Diseases (NCD): A Review. Adv. Life Sci. Technol. 2015, 29, 23–40. [Google Scholar]
- McKenzie, M.R.; Illingworth, S. Should a Low Carbohydrate Diet Be Recommended for Diabetes Management? Proc. Nutr. Soc. 2017, 76, 91027. [Google Scholar] [CrossRef]
- Wikarek, T.; Kocełak, P.; Owczarek, A.J.; Chudek, J.; Olszanecka-Glinianowicz, M. Effect of Dietary Macronutrients on Postprandial Glucagon and Insulin Release in Obese and Normal-Weight Women. Int. J. Endocrinol. 2020, 2020, 4603682. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Ruirui, G.; Li, X.; Wang, F.; Wu, Z.; Liu, Y.; Dong, Y.; Li, B. The Association between Multiple Trajectories of Macronutrient Intake and the Risk of New-Onset Diabetes in Chinese Adults. J. Diabetes 2024, 16, e13555. [Google Scholar] [CrossRef]
- El-Alameey, I.R.; Aljohani, R.N.; Allhebi, S.A.; Alahmadi, H.A.; Alsakrani, R.K. Macronutrient Intake and Association with the Risk Factors of Diabetic Complications among People with Type 2 Diabetes. Maced. J. Med. Sci. 2024, 12, 73–82. [Google Scholar] [CrossRef]
- Chan, Q.; Stamler, J.; Oude Griep, L.M.; Daviglus, M.L.; Van Horn, L.; Elliott, P. An Update on Nutrients and Blood Pressure Summary of INTERMAP Study Findings. J. Atheroscler. Thromb. 2016, 23, 276–289. [Google Scholar] [CrossRef]
- Oh, H.Y.; Kim, M.K.; Lee, M.; Kim, Y.O. Macronutrient Composition and Sodium Intake of Diet Are Associated with Risk of Metabolic Syndrome and Hypertension in Korean Women. PLoS ONE 2013, 8, e78088. [Google Scholar] [CrossRef]
- Miller, V.; Mente, A.; Dehghan, M.; Rangarajan, S.; Zhang, X.; Swaminathan, S.; Dagenais, G.; Gupta, R.; Mohan, V.; Lear, S.; et al. Fruit, Vegetable, and Legume Intake, and Cardiovascular Disease and Deaths in 18 Countries (PURE): A Prospective Cohort Study. Lancet 2017, 390, 2037–2049. [Google Scholar] [CrossRef] [PubMed]
- Farhadnejad, H.; Mokhtari, E.; Teymoori, F.; Jahromi, M.K.; Saber, N.; Ahmadirad, H.; Norouzzadeh, M.; Mirmiran, P.; Azizi, F. Macronutrients Quality Indices and Risk of Metabolic Syndrome and Its Components in Iranian Adults. BMC Cardiovasc. Disord. 2024, 24, 126. [Google Scholar] [CrossRef]
- Lee, S.W.; Kim, H.C.; Nam, C.; Lee, H.Y.; Ahn, S.V.; Oh, Y.A.; Suh, I. Age-Differential Association between Serum Uric Acid and Incident Hypertension. Hypertens. Res. 2019, 42, 428–437. [Google Scholar] [CrossRef]
- Ren, X.; Yang, X.; Jiang, H.; Han, T.; Sun, C. The Association of Energy and Macronutrient Intake at Dinner vs Breakfast with the Incidence of Type 2 Diabetes Mellitus in a Cohort Study: The China Health and Nutrition Survey, 1997–2011. J. Diabetes 2021, 13, 882–892. [Google Scholar] [CrossRef] [PubMed]
- Koemel, N.A.; Senior, A.M.; Laouali, N.; Celermajer, D.S.; Grech, A.; Parker, H.M.; Simpson, S.J.; Raubenheimer, D.; Gill, T.P.; Skilton, M.R. Associations between Dietary Macronutrient Composition and Cardiometabolic Health: Data from NHANES 1999–2014. Eur. J. Nutr. 2025, 64, 68. [Google Scholar] [CrossRef] [PubMed]
- Mirmiran, P.; Hosseini-Esfahani, F.; Esfandiar, Z.; Hosseinpour-Niazi, S.; Azizi, F. Associations between Dietary Antioxidant Intakes and Cardiovascular Disease. Sci. Rep. 2022, 12, 1504. [Google Scholar] [CrossRef]
- Budhathoki, S.; Sawada, N.; Iwasaki, M.; Yamaji, T.; Goto, A.; Kotemori, A.; Ishihara, J.; Takachi, R.; Charvat, H.; Mizoue, T.; et al. Association of Animal and Plant Protein Intake with All-Cause and Cause-Specific Mortality in a Japanese Cohort. JAMA Intern. Med. 2019, 179, 1509–1518. [Google Scholar] [CrossRef]
- Nilsson, L.M.; Winkvist, A.; Eliasson, M.; Jansson, J.H.; Hallmans, G.; Johansson, I.; Lindahl, B.; Lenner, P.; Van Guelpen, B. Low-Carbohydrate, High-Protein Score and Mortality in a Northern Swedish Population-Based Cohort. Eur. J. Clin. Nutr. 2012, 66, 694–700. [Google Scholar] [CrossRef]
- Li, X.; Yu, J.; Wen, L.; Li, Q.; Yan, J.; Tian, J.; Tong, C.; Tong, Q.; Qi, H.; Saffery, R.; et al. Vitamin D Status in Women with Dichorionic Twin Pregnancies and Their Neonates: A Pilot Study in China. BMC Pregnancy Childbirth 2021, 21, 279. [Google Scholar] [CrossRef]
- Braun, K.; Guasch-Ferré, M.L.; Malik, V.; Alessa, H.; Willett, W.; Hu, F.B.; Voortman, T.; Bhupathiraju, S. Carbohydrate Quantity and Quality and Risk of Type 2 Diabetes: Results from Three Large Prospective US Cohorts. Curr. Dev. Nutr. 2020, 4, 1380. [Google Scholar] [CrossRef]


| Food Groups | 2011 | 2013 | 2015 | 2017 | 2019 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean ± SD (g) | n | Mean ± SD (g) | n | Mean ± SD (g) | n | Mean ± SD (g) | n | Mean ± SD (g) | |
| Cereals and cereal products | 867 | 259.61 a ± 111.36 | 865 | 241.47 b ± 91.97 | 866 | 259.11 c ± 104.41 | 867 | 255.41 c ± 113.86 | 866 | 234.84 d ± 132.06 |
| Starchy roots and tubers and products | 389 | 16.33 a ± 31.95 | 298 | 16.51 b ± 37.33 | 526 | 24.66 a ± 45.26 | 543 | 34.03 c ± 52.13 | 598 | 43.37 c ± 65.82 |
| Legumes, nuts and seeds, and products | 690 | 76.02 a ± 76.60 | 743 | 67.39 b ± 58.18 | 756 | 83.79 c ± 78.71 | 751 | 94.14 d ± 84.36 | 737 | 83.29 e ± 78.10 |
| Vegetables and products | 742 | 48.13 a ± 42.46 | 726 | 48.72 b ± 47.29 | 747 | 49.71 c ± 46.19 | 773 | 68.08 d ± 58.81 | 782 | 61.15 e ± 52.77 |
| Fruits and products | 420 | 73.19 a ± 107.21 | 436 | 50.56 b ± 77.21 | 370 | 55.29 c ± 96.13 | 482 | 85.88 a ± 121.56 | 477 | 82.39 b ± 122.16 |
| Meat and products | 505 | 42.56 a ± 51.89 | 541 | 36.44 b ± 43.76 | 525 | 50.36 c ± 74.85 | 579 | 63.75 d ± 69.21 | 644 | 71.68 e ± 76.41 |
| Finfish, shellfish, other aquatic animals and products | 464 | 25.34 a ± 36.44 | 465 | 27.30 b ± 37.33 | 491 | 32.15 c ± 55.48 | 430 | 26.23 d ± 42.85 | 388 | 22.43 e ± 41.31 |
| Eggs and products | 470 | 29.93 a ± 40.70 | 594 | 36.10 b ± 40.18 | 464 | 30.82 c ± 41.65 | 516 | 35.73 d ± 44.30 | 577 | 37.22 e ± 45.99 |
| Milk and products | 145 | 6.27 a ± 26.69 | 74 | 3.57 b ± 20.08 | 101 | 6.78 c ± 37.11 | 325 | 10.83 d ± 46.95 | 384 | 13.13 e ± 43.59 |
| Fats and oils | 862 | 41.71 a ± 38.74 | 858 | 37.05 b ± 40.28 | 862 | 55.04 c ± 48.67 | 861 | 71.05 d ± 55.84 | 862 | 78.62 e ± 71.68 |
| Sugars, syrup and confectionery | 641 | 19.55 a ± 18.10 | 506 | 17.19 b ± 33.06 | 658 | 21.95 b ± 22.95 | 691 | 25.61 bc ± 27.09 | 722 | 34.19 c ± 26.48 |
| Spices and condiments | 859 | 11.43 a ± 10.33 | 850 | 12.58 b ± 13.81 | 864 | 15.12 c ± 17.78 | 866 | 19.66 a ± 21.50 | 860 | 13.47 d ± 15.05 |
| Alcoholic beverages | - | - | - | - | 1 | 0.21 a ± 6.28 | 2 | 0.27 b ± 7.65 | 4 | 1.51 c ± 43.47 |
| Nonalcoholic beverages | 735 | 205.70 a ± 231.26 | 788 | 421.15 b ± 357.41 | 791 | 426.35 c ± 369.04 | 802 | 442.09 d ± 347.95 | 794 | 471.06 e ± 411.44 |
| Fast foods | 1 | 0.12 a ± 3.40 | 2 | 0.10 b ± 2.17 | 2 | 0.23 c ± 4.80 | 3 | 0.33 d ± 7.79 | 5 | 0.76 e ± 10.46 |
| Mixed food dishes | 301 | 17.01 a ± 33.70 | 477 | 31.47 b ± 45.63 | 274 | 12.21 c ± 28.57 | 358 | 17.94 d ± 31.81 | 372 | 19.72 e ± 43.89 |
| Miscellaneous | - | - | - | - | - | - | - | - | 3 | 0.00 a ± 0.08 |
| Traditional herbs and supplements | 6 | 0.01 a ± 0.11 | 14 | 0.30 b ± 4.05 | 10 | 0.04 c ± 0.70 | 25 | 0.33 d ± 3.52 | 27 | 0.27 e ± 4.87 |
| Total | 872.92 | 1047.90 | 1123.82 | 1251.34 | 1 69.11 e | |||||
| Drinking water | 853 | 984.97 a ± 537.14 | 831 | 1005.10 a ± 598.61 | 853 | 1229.13 c ± 630.26 | 855 | 1297.88 d ± 657.42 | 855 | 1413.01 e ± 749.08 |
| Total with drinking water | 1857.89 | 2052.99 | 2352.94 | 2549.22 | 2682.12 | |||||
| Food Groups | Energy Contribution | Protein Contribution | Fat Contribution | Carbohydrate Contribution | Fiber Contribution | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| kcal/Day | % | g/Day | % | g/Day | % | g/Day | % | g/Day | % | |
| Cereals and products | 868.43 ± 389.20 | 47.71 ± 13.75 | 20.96 ± 9.50 | 37.20 ± 13.98 | 5.04 ± 3.40 | 9.21 ± 8.11 | 176.63 ± 79.96 | 71.57 ± 14.42 | 1.70 ± 2.08 | 28.03 ± 22.83 |
| Starchy roots, tubers and products | 33.75 ± 81.15 | 1.78 ± 3.97 | 0.34 ± 0.69 | 0.63 ± 1.79 | 0.40 ± 2.24 | 0.57 ± 2.62 | 7.24 ± 16.57 | 2.92 ± 6.16 | 0.23 ± 0.71 | 3.82 ± 9.50 |
| Legumes, nuts and seeds, and products | 125.60 ± 127.12 | 6.81 ± 6.11 | 10.75 ± 10.14 | 18.02 ± 14.86 | 7.06 ± 8.20 | 10.56 ± 10.23 | 7.22 ± 8.50 | 3.06 ± 3.49 | 1.04 ± 1.23 | 17.82 ± 17.70 |
| Vegetables and products | 16.28 ± 16.35 | 0.92 ± 0.94 | 0.99 ± 1.11 | 1.76 ± 2.10 | 0.26 ± 0.37 | 0.44 ± 0.65 | 3.05 ± 3.12 | 1.31 ± 1.37 | 1.17 ± 1.59 | 18.54 ± 17.17 |
| Fruits and products | 48.84 ± 74.86 | 2.66 ± 3.99 | 0.58 ± 0.91 | 1.05 ± 1.75 | 1.08 ± 4.27 | 1.53 ± 5.47 | 11.86 ± 18.06 | 4.79 ± 7.02 | 1.43 ± 2.64 | 17.67 ± 22.97 |
| Meat and products | 150.13 ± 191.12 | 7.79 ± 9.04 | 11.51 ± 15.12 | 16.94 ± 18.14 | 11.03 ± 14.73 | 14.88 ± 16.75 | 0.92 ± 3.14 | 0.38 ± 1.33 | 0.01 ± 0.14 | 0.21 ± 2.27 |
| Finfish, shellfish, other aquatic animals and products | 34.66 ± 58.00 | 1.97 ± 3.09 | 5.89 ± 10.23 | 9.56 ± 13.07 | 0.81 ± 2.03 | 1.43 ± 3.26 | 0.78 ± 2.06 | 0.33 ± 0.88 | 0.00 ± 0.00 | 0.00 ± 0.07 |
| Eggs and products | 56.38 ± 71.16 | 3.12 ± 4.04 | 4.06 ± 5.24 | 7.11 ± 9.33 | 3.63 ± 4.69 | 5.75 ± 7.83 | 1.47 ± 5.86 | 0.63 ± 2.25 | 0.01 ± 0.06 | 0.26 ± 1.40 |
| Milk and products | 17.49 ± 51.44 | 0.93 ± 2.70 | 1.11 ± 3.06 | 1.8 ± 4.70 | 0.69 ± 2.64 | 1.01 ± 3.89 | 1.71 ± 4.83 | 0.73 ± 2.12 | 0.00 ± 0.00 | 0.00 ± 0.00 |
| Fats and oils | 321.26 ± 237.12 | 16.78 ± 8.16 | 0.50 ± 0.96 | 0.82 ± 1.59 | 35.43 ± 26.32 | 50.69 ± 17.46 | 1.82 ± 3.57 | 0.73 ± 1.44 | 0.34 ± 0.67 | 5.29 ± 10.01 |
| Sugars, syrup and confectionery | 85.28 ± 97.58 | 4.76 ± 5.15 | 0.29 ± 1.30 | 0.49 ± 2.10 | 0.40 ± 1.68 | 0.65 ± 2.76 | 19.43 ± 21.11 | 8.04 ± 8.15 | 0.07 ± 0.55 | 0.78 ± 5.05 |
| Spices and condiments | 8.05 ± 13.29 | 0.44 ± 0.66 | 0.60 ± 2.01 | 0.96 ± 1.82 | 0.10 ± 0.25 | 0.16 ± 0.41 | 1.18 ± 1.72 | 0.52 ± 0.83 | 0.11 ± 0.34 | 2.06 ± 5.14 |
| Alcoholic beverages | 0.80 ± 34.03 | 0.01 ± 0.52 | 0.00 ± 0.13 | 0.00 ± 0.09 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.03 ± 1.28 | 0.01 ± 0.23 | 0.00 ± 0.00 | 0.00 ± 0.00 |
| Nonalcoholic beverages | 27.55 ± 68.20 | 1.52 ± 3.63 | 0.73 ± 3.42 | 1.22 ± 3.46 | 0.12 ± 0.56 | 0.24 ± 1.31 | 4.62 ± 12.88 | 1.92 ± 5.12 | 0.19 ± 1.25 | 2.42 ± 8.56 |
| Fast foods | 0.87 ± 18.17 | 0.05 ± 1.09 | 0.07 ± 1.58 | 0.09 ± 1.89 | 0.05 ± 1.21 | 0.08 ± 1.71 | 0.02 ± 0.57 | 0.01 ± 0.34 | 0.00 ± 0.04 | 0.02 ± 0.77 |
| Mixed food dishes | 48.98 ± 88.27 | 2.78 ± 5.03 | 1.30 ± 2.48 | 2.33 ± 4.51 | 1.67 ± 3.34 | 2.78 ± 5.68 | 7.23 ± 13.51 | 3.10 ± 5.77 | 0.17 ± 0.48 | 3.07 ± 8.09 |
| Miscellaneous | - | - | - | - | - | - | - | - | - | - |
| Traditional herbs and supplements | 0.01 ± 0.87 | 0.001 ± 0.09 | 0.001 ± 0.06 | 0.002 ± 0.14 | - | - | 0.003 ± 0.18 | 0.01 ± 0.36 | - | - |
| Drinking water | - | - | - | - | - | - | - | - | - | - |
| Total | 1844.36 | 100.30 | 59.68 | 99.99 | 67.77 | 99.98 | 245.20 | 100.05 | 6.49 | 100.00 |
| Parameters | Year | ||||
|---|---|---|---|---|---|
| 2011 | 2013 | 2015 | 2017 | 2019 | |
| Fasting blood glucose (mg/dL) | 92.04 ± 25.91 | 85.80 ± 24.25 | 95.73 ± 30.29 | 105.02 ± 44.80 | 105.88 ± 38.90 |
| Blood glucose 2-h postprandial (mg/dL) | 126.05 ± 53.66 | 123.23 ± 45.87 | 136.34 ± 55.04 | 144.39 ± 68.04 | 138.48 ± 63.25 |
| Total cholesterol (mg/dL) | 195.70 ± 34.81 | 200.23 ± 35.15 | 196.47 ± 35.78 | 199.13 ± 36.73 | 204.82 ± 38.54 |
| Triglycerides (mg/dL) | 106.96 ± 62.79 | 117.25 ± 71.05 | 116.73 ± 68.08 | 122.59 ± 78.52 | 128.60 ± 87.40 |
| LDL cholesterol (mg/dL) | 126.49 ± 30.49 | 128.09 ± 31.75 | 128.03 ± 32.65 | 123.64 ± 31.59 | 128.27 ± 33.54 |
| HDL cholesterol (mg/dL) | 51.37 ± 11.46 | 52.14 ± 12.35 | 52.89 ± 11.25 | 51.80 ± 12.35 | 48.86 ± 11.89 |
| LDL-C/HDL-C ratio | 2.58 ± 0.82 | 2.56 ± 0.82 | 2.52 ± 0.81 | 2.50 ± 0.82 | 2.75 ± 0.93 |
| Blood pressure, systolic (mmHg) | 129.79 ± 23.78 | 127.29 ± 22.29 | 127.80 ± 21.42 | 104.83 ± 29.54 | 128.01 ± 20.09 |
| Blood pressure, diastolic (mmHg) | 81.34 ± 13.24 | 80.76 ± 12.72 | 80.34 ± 12.05 | 83.97 ± 12.15 | 81.00 ± 11.08 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Retiaty, F.; Andarwulan, N.; Palupi, N.S.; Ernawati, F.; Kazimierczak, R.; Średnicka-Tober, D. Contribution of Food, Energy, Macronutrients and Fiber Consumption Patterns to Obesity and Other Non-Communicable Disease Risks in the Indonesian Population. Nutrients 2025, 17, 1459. https://doi.org/10.3390/nu17091459
Retiaty F, Andarwulan N, Palupi NS, Ernawati F, Kazimierczak R, Średnicka-Tober D. Contribution of Food, Energy, Macronutrients and Fiber Consumption Patterns to Obesity and Other Non-Communicable Disease Risks in the Indonesian Population. Nutrients. 2025; 17(9):1459. https://doi.org/10.3390/nu17091459
Chicago/Turabian StyleRetiaty, Fifi, Nuri Andarwulan, Nurheni Sri Palupi, Fitrah Ernawati, Renata Kazimierczak, and Dominika Średnicka-Tober. 2025. "Contribution of Food, Energy, Macronutrients and Fiber Consumption Patterns to Obesity and Other Non-Communicable Disease Risks in the Indonesian Population" Nutrients 17, no. 9: 1459. https://doi.org/10.3390/nu17091459
APA StyleRetiaty, F., Andarwulan, N., Palupi, N. S., Ernawati, F., Kazimierczak, R., & Średnicka-Tober, D. (2025). Contribution of Food, Energy, Macronutrients and Fiber Consumption Patterns to Obesity and Other Non-Communicable Disease Risks in the Indonesian Population. Nutrients, 17(9), 1459. https://doi.org/10.3390/nu17091459







