Multiregional Sequencing of IDH-WT Glioblastoma Reveals High Genetic Heterogeneity and a Dynamic Evolutionary History
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. GB Patients
2.2. Sample Collection
2.3. Sample Processing
2.4. Multi-Region Whole-Exome Sequence (WES) Analysis
2.5. Bioinformatic Analysis and Data Interpretation
3. Results
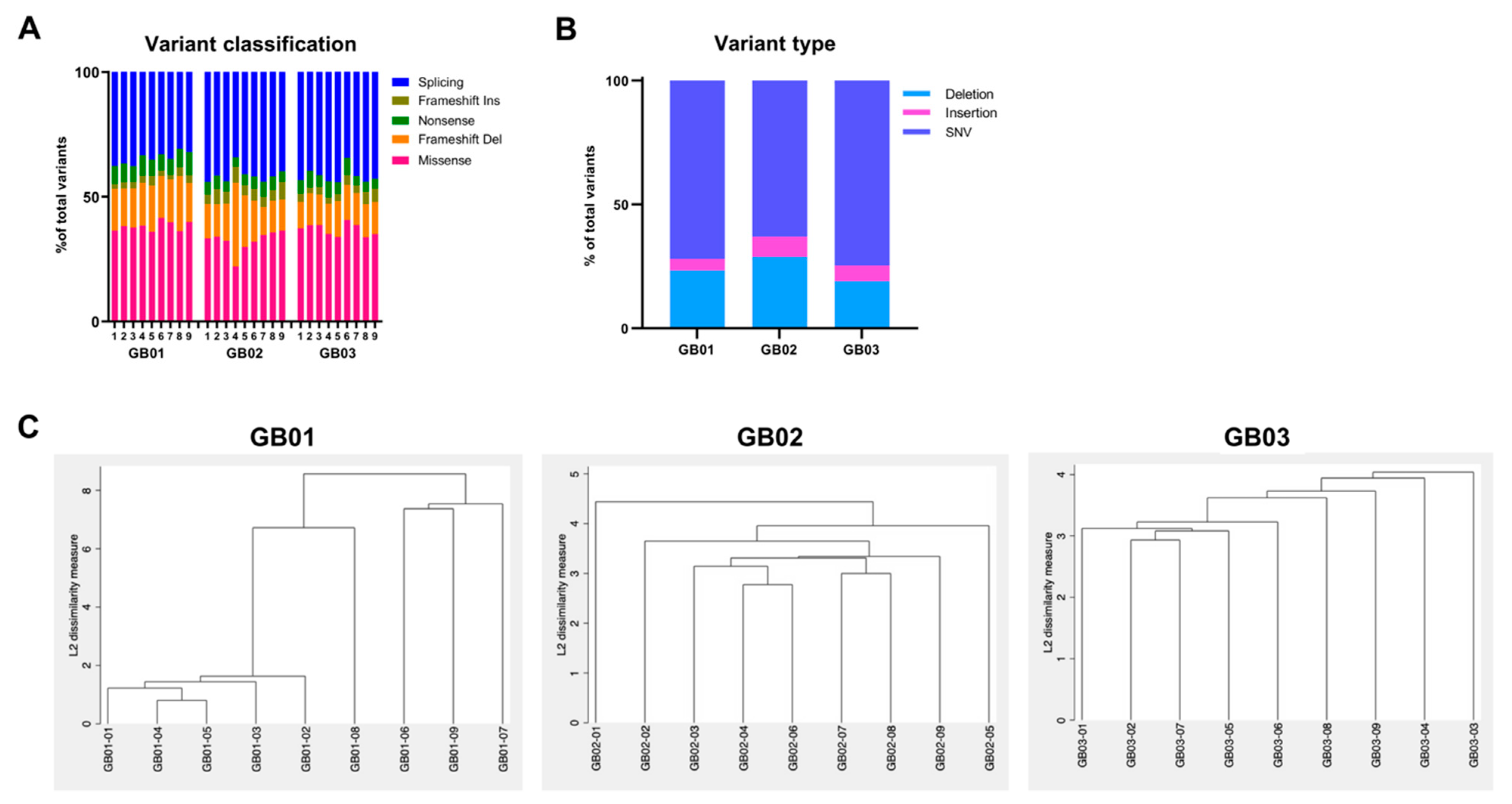
3.1. Whole-Exome Sequencing
3.2. Copy Number Variation Analysis
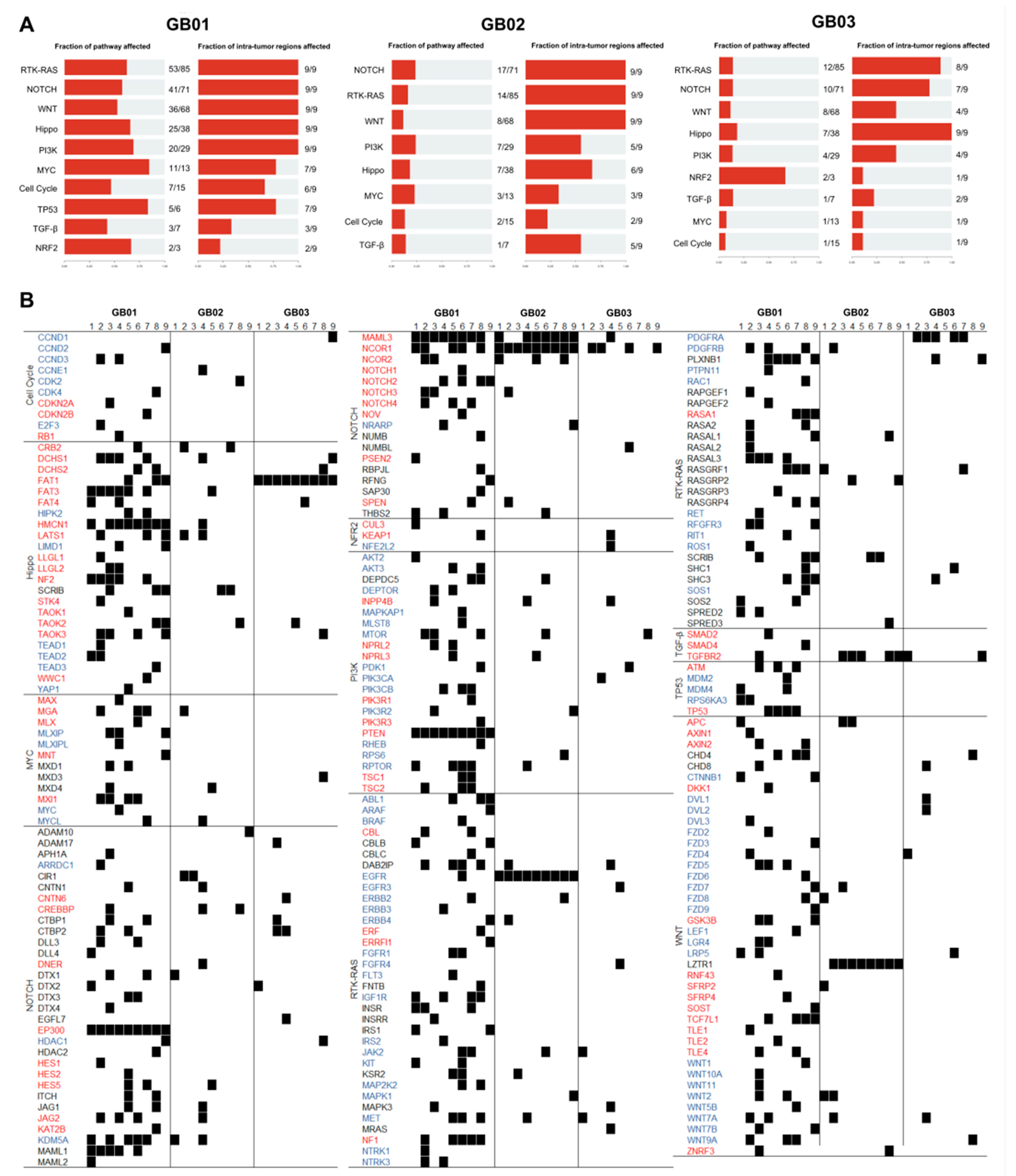
3.3. Mutational Landscape
3.4. Somatic Mutations
3.5. Rare Variants
3.6. Phylogenetic and Clonal Evolution
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CNV | Copy number variation |
| GB | Glioblastoma |
| GCS | Global score |
| MAF | Minor allele frequency |
| PTI | Phylogenetic tree inference |
| SNV | Single-nucleotide variant |
| VAF | Variant allele frequency |
| WES | Whole-Exome Sequencing |
References
- Gallaher, J.A.; Massey, S.C.; Hawkins-Daarud, A.; Noticewala, S.S.; Rockne, R.C.; Johnston, S.K.; Gonzalez-Cuyar, L.; Juliano, J.; Gil, O.; Swanson, K.R.; et al. From cells to tissue: How cell scale heterogeneity impacts glioblastoma growth and treatment response. PLoS Comput. Biol. 2020, 16, e1007672. [Google Scholar] [CrossRef]
- Mahlokozera, T.; Vellimana, A.K.; Li, T.; Mao, D.D.; Zohny, Z.S.; Kim, D.H.; Tran, D.D.; Marcus, D.S.; Fouke, S.J.; Campian, J.L.; et al. Biological and therapeutic implications of multisector sequencing in newly diagnosed glioblastoma. Neuro Oncol. 2018, 20, 472–483. [Google Scholar] [CrossRef]
- Sottoriva, A.; Spiteri, I.; Piccirillo, S.G.M.; Touloumis, A.; Collins, V.P.; Marioni, J.C.; Curtis, C.; Watts, C.; Tavaré, S. Intratumor heterogeneity in human glioblastoma reflects cancer evolutionary dynamics. Proc. Natl. Acad. Sci. USA 2013, 110, 4009–4014. [Google Scholar] [CrossRef] [PubMed]
- Stupp, R.; Mason, W.P.; van den Bent, M.J.; Weller, M.; Fisher, B.; Taphoorn, M.J.B.; Belanger, K.; Brandes, A.A.; Marosi, C.; Bogdahn, U.; et al. Radiotherapy plus Concomitant and Adjuvant Temozolomide for Glioblastoma. N. Engl. J. Med. 2005, 352, 987–996. [Google Scholar] [CrossRef] [PubMed]
- Weller, M.; van den Bent, M.; Tonn, J.C.; Stupp, R.; Preusser, M.; Cohen-Jonathan-Moyal, E.; Henriksson, R.; Le Rhun, E.; Balana, C.; Chinot, O.; et al. European Association for Neuro-Oncology (EANO) guideline on the diagnosis and treatment of adult astrocytic and oligodendroglial gliomas. Lancet Oncol. 2017, 18, e315–e329. [Google Scholar] [CrossRef]
- Thakkar, J.P.; Dolecek, T.A.; Horbinski, C.; Ostrom, Q.T.; Lightner, D.D.; Barnholtz-Sloan, J.S.; Villano, J.L. Epidemiologic and Molecular Prognostic Review of Glioblastoma. Cancer Epidemiol. Biomark. Prev. 2014, 23, 1985–1996. [Google Scholar] [CrossRef]
- Hanif, F.; Muzaffar, K.; Perveen, K.; Malhi, S.M.; Simjee, S.U. Glioblastoma Multiforme: A Review of its Epidemiology and Pathogenesis through Clinical Presentation and Treatment. Asian Pac. J. Cancer Prev. 2017, 18, 3–9. [Google Scholar]
- Louis, D.N.; Perry, A.; Reifenberger, G.; von Deimling, A.; Figarella-Branger, D.; Cavenee, W.K.; Ohgaki, H.; Wiestler, O.D.; Kleihues, P.; Ellison, D.W. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: A summary. Acta Neuropathol. 2016, 131, 803–820. [Google Scholar] [CrossRef]
- Parsons, D.W.; Jones, S.; Zhang, X.; Lin, J.C.-H.; Leary, R.J.; Angenendt, P.; Mankoo, P.; Carter, H.; Siu, I.-M.; Gallia, G.L.; et al. An Integrated Genomic Analysis of Human Glioblastoma Multiforme. Science 2008, 321, 1807–1812. [Google Scholar] [CrossRef]
- Civita, P.; Franceschi, S.; Aretini, P.; Ortenzi, V.; Menicagli, M.; Lessi, F.; Pasqualetti, F.; Naccarato, A.G.; Mazzanti, C.M. Laser Capture Microdissection and RNA-Seq Analysis: High Sensitivity Approaches to Explain Histopathological Heterogeneity in Human Glioblastoma FFPE Archived Tissues. Front. Oncol. 2019, 9, 482. [Google Scholar] [CrossRef] [PubMed]
- Brastianos, P.K.; Nayyar, N.; Rosebrock, D.; Leshchiner, I.; Gill, C.M.; Livitz, D.; Bertalan, M.S.; D’Andrea, M.; Hoang, K.; Aquilanti, E.; et al. Resolving the phylogenetic origin of glioblastoma via multifocal genomic analysis of pre-treatment and treatment-resistant autopsy specimens. NPJ Precis. Oncol. 2017, 1, 33. [Google Scholar] [CrossRef]
- Franceschi, S.; Lessi, F.; Aretini, P.; Ortenzi, V.; Scatena, C.; Menicagli, M.; La Ferla, M.; Civita, P.; Zavaglia, K.; Scopelliti, C.; et al. Cancer astrocytes have a more conserved molecular status in long recurrence free survival (RFS) IDH1 wild-type glioblastoma patients: New emerging cancer players. Oncotarget 2018, 9, 24014–24027. [Google Scholar] [CrossRef] [PubMed]
- Parker, N.R.; Hudson, A.L.; Khong, P.; Parkinson, J.F.; Dwight, T.; Ikin, R.J.; Zhu, Y.; Cheng, Z.J.; Vafaee, F.; Chen, J.; et al. Intratumoral heterogeneity identified at the epigenetic, genetic and transcriptional level in glioblastoma. Sci. Rep. 2016, 6, 22477. [Google Scholar] [CrossRef] [PubMed]
- Gerlinger, M.; Rowan, A.J.; Horswell, S.; Larkin, J.; Endesfelder, D.; Gronroos, E.; Martinez, P.; Matthews, N.; Stewart, A.; Tarpey, P.; et al. Intratumor Heterogeneity and Branched Evolution Revealed by Multiregion Sequencing. N. Engl. J. Med. 2012, 366, 883–892. [Google Scholar] [CrossRef]
- Kumar, A.; Boyle, E.A.; Tokita, M.; Mikheev, A.M.; Sanger, M.C.; Girard, E.; Silber, J.R.; Gonzalez-Cuyar, L.F.; Hiatt, J.B.; Adey, A.; et al. Deep sequencing of multiple regions of glial tumors reveals spatial heterogeneity for mutations in clinically relevant genes. Genome Biol. 2014, 15, 530. [Google Scholar] [CrossRef] [PubMed]
- Wingett, S.W.; Andrews, S. FastQ Screen: A tool for multi-genome mapping and quality control. F1000Research 2018, 7, 1338. [Google Scholar] [CrossRef]
- Li, H. Aligning sequence reads, clone sequences and assembly contigs with BWA-MEM. arXiv 2013, arXiv:1303.3997. [Google Scholar]
- McKenna, A.; Hanna, M.; Banks, E.; Sivachenko, A.; Cibulskis, K.; Kernytsky, A.; Garimella, K.; Altshuler, D.; Gabriel, S.B.; Daly, M.J.; et al. The Genome Analysis Toolkit: A MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 2010, 20, 1297–1303. [Google Scholar] [CrossRef]
- Benjamin, D.; Sato, T.; Cibulskis, K.; Getz, G.; Stewart, C.; Lichtenstein, L. Calling Somatic SNVs and Indels with Mutect2. bioRxiv 2019, 861054. [Google Scholar] [CrossRef]
- Karczewski, K.J.; Francioli, L.C.; Tiao, G.; Cummings, B.B.; Alfoeldi, J.; Wang, Q.S.; Collins, R.L.; Laricchia, K.M.; Ganna, A.; Birnbaum, D.P.; et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature 2020, 581, 434–443. [Google Scholar] [CrossRef]
- Mayakonda, A.; Koeffler, H.P. Maftools: Efficient analysis, visualization and summarization of MAF files from large-scale cohort based cancer studies. bioRxiv 2016, 052662. [Google Scholar] [CrossRef]
- Talevich, E.; Shain, A.H.; Botton, T.; Bastian, B.C. CNVkit: Genome-Wide Copy Number Detection and Visualization from Targeted DNA Sequencing. PLoS Comput. Biol. 2016, 12, e1004873. [Google Scholar] [CrossRef] [PubMed]
- Franch-Expósito, S.; Bassaganyas, L.; Vila-Casadesús, M.; Hernández-Illán, E.; Esteban-Fabró, R.; Díaz-Gay, M.; Lozano, J.J.; Castells, A.; Llovet, J.M.; Castellvi-Bel, S.; et al. CNApp, a tool for the quantification of copy number alterations and integrative analysis revealing clinical implications. eLife 2020, 9, e50267. [Google Scholar] [CrossRef] [PubMed]
- Colaprico, A.; Silva, T.C.; Olsen, C.; Garofano, L.; Cava, C.; Garolini, D.; Sabedot, T.S.; Malta, T.M.; Pagnotta, S.M.; Castiglioni, I.; et al. TCGAbiolinks: An R/Bioconductor package for integrative analysis of TCGA data. Nucleic Acids Res. 2016, 44, e71. [Google Scholar] [CrossRef] [PubMed]
- Liaw, A.; Wiener, M. Classification and Regression with randomForest. R News 2002, 2, 18–22. [Google Scholar]
- Phillips, H.S.; Kharbanda, S.; Chen, R.; Forrest, W.F.; Soriano, R.H.; Wu, T.D.; Misra, A.; Nigro, J.M.; Colman, H.; Soroceanu, L.; et al. Molecular subclasses of high-grade glioma predict prognosis, delineate a pattern of disease progression, and resemble stages in neurogenesis. Cancer Cell 2006, 9, 157–173. [Google Scholar] [CrossRef]
- Verhaak, R.G.; Hoadley, K.A.; Purdom, E.; Wang, V.; Qi, Y.; Wilkerson, M.D.; Miller, C.R.; Ding, L.; Golub, T.; Mesirov, J.P.; et al. Integrated Genomic Analysis Identifies Clinically Relevant Subtypes of Glioblastoma Characterized by Abnormalities in PDGFRA, IDH1, EGFR, and NF1. Cancer Cell 2010, 17, 98–110. [Google Scholar] [CrossRef]
- Kopanos, C.; Tsiolkas, V.; Kouris, A.E.; Chapple, C.; Aguilera, M.A.; Meyer, R.; Massouras, A. VarSome: The human genomic variant search engine. Bioinformatics 2019, 35, 1978–1980. [Google Scholar] [CrossRef]
- Richards, S.; Aziz, N.; Bale, S.; Bick, D.; Das, S.; Gastier-Foster, J.; Grody, W.W.; Hegde, M.; Lyon, E.; Spector, E.; et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 2015, 17, 405–423. [Google Scholar] [CrossRef]
- Sanchez-Vega, F.; Mina, M.; Armenia, J.; Chatila, W.K.; Luna, A.; La, K.C.; Dimitriadoy, S.; Liu, D.L.; Kantheti, H.S.; Saghafinia, S.; et al. Oncogenic Signaling Pathways in The Cancer Genome Atlas. Cell 2018, 173, 321–337.e10. [Google Scholar] [CrossRef]
- Wu, P.; Hou, L.; Zhang, Y.; Zhang, L. Phylogenetic Tree Inference: A Top-Down Approach to Track Tumor Evolution. Front. Genet. 2020, 10, 1371. [Google Scholar] [CrossRef]
- Brancato, V.; Nuzzo, S.; Tramontano, L.; Condorelli, G.; Salvatore, M.; Cavaliere, C. Predicting Survival in Glioblastoma Patients Using Diffusion MR Imaging Metrics—A Systematic Review. Cancers 2020, 12, 2858. [Google Scholar] [CrossRef]
- Poon, M.T.C.; Sudlow, C.L.M.; Figueroa, J.D.; Brennan, P.M. Longer-term (≥2 years) survival in patients with glioblastoma in population-based studies pre- and post-2005: A systematic review and meta-analysis. Sci. Rep. 2020, 10, 1–10. [Google Scholar] [CrossRef]
- Brennan, C.W.; Verhaak, R.G.W.; McKenna, A.; Campos, B.; Noushmehr, H.; Salama, S.R.; Zheng, S.; Chakravarty, D.; Sanborn, J.Z.; Berman, S.H.; et al. The Somatic Genomic Landscape of Glioblastoma. Cell 2013, 155, 462–477. [Google Scholar] [CrossRef]
- Jacob, F.; Salinas, R.D.; Zhang, D.Y.; Nguyen, P.T.; Schnoll, J.G.; Wong, S.Z.H.; Thokala, R.; Sheikh, S.; Saxena, D.; Prokop, S.; et al. A Patient-Derived Glioblastoma Organoid Model and Biobank Recapitulates Inter- and Intra-tumoral Heterogeneity. Cell 2020, 180, 188–204.e22. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Lee, I.-H.; Cho, H.J.; Park, C.-K.; Jung, Y.-S.; Kim, Y.; Nam, S.H.; Kim, B.S.; Johnson, M.D.; Kong, D.-S.; et al. Spatiotemporal Evolution of the Primary Glioblastoma Genome. Cancer Cell 2015, 28, 318–328. [Google Scholar] [CrossRef]
- Nørøxe, D.S.; Yde, C.W.; Østrup, O.; Michaelsen, S.R.; Schmidt, A.Y.; Kinalis, S.; Torp, M.H.; Skjøth-Rasmussen, J.; Brennum, J.; Hamerlik, P.; et al. Genomic profiling of newly diagnosed glioblastoma patients and its potential for clinical utility—A prospective, translational study. Mol. Oncol. 2020, 14, 2727–2743. [Google Scholar] [CrossRef] [PubMed]
- Noushmehr, H.; Weisenberger, D.J.; Diefes, K.; Phillips, H.S.; Pujara, K.; Berman, B.P.; Pan, F.; Pelloski, C.E.; Sulman, E.P.; Bhat, K.P.; et al. Identification of a CpG Island Methylator Phenotype that Defines a Distinct Subgroup of Glioma. Cancer Cell 2010, 17, 510–522. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.P.; Tirosh, I.; Trombetta, J.J.; Shalek, A.K.; Gillespie, S.M.; Wakimoto, H.; Cahill, D.P.; Nahed, B.V.; Curry, W.T.; Martuza, R.L.; et al. Single-cell RNA-seq highlights intratumoral heterogeneity in primary glioblastoma. Science 2014, 344, 1396–1401. [Google Scholar] [CrossRef] [PubMed]
- Zheng, S.; Fu, J.; Vegesna, R.; Mao, Y.; Heathcock, L.E.; Torres-Garcia, W.; Ezhilarasan, R.; Wang, S.; McKenna, A.; Chin, L.; et al. A survey of intragenic breakpoints in glioblastoma identifies a distinct subset associated with poor survival. Genes Dev. 2013, 27, 1462–1472. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Zheng, S.; Amini, S.S.; Virk, S.M.; Mikkelsen, T.; Brat, D.J.; Grimsby, J.; Sougnez, C.; Muller, F.; Hu, J.; et al. Whole-genome and multisector exome sequencing of primary and post-treatment glioblastoma reveals patterns of tumor evolution. Genome Res. 2015, 25, 316–327. [Google Scholar] [CrossRef]
- Lee, J.-K.; Wang, J.; Sa, J.K.; Ladewig, E.; Lee, H.-O.; Lee, I.-H.; Kang, H.J.; Rosenbloom, D.S.; Camara, P.G.; Liu, Z.; et al. Spatiotemporal genomic architecture informs precision oncology in glioblastoma. Nat. Genet. 2017, 49, 594–599. [Google Scholar] [CrossRef]
- Spiteri, I.; Caravagna, G.; Cresswell, G.; Vatsiou, A.; Nichol, D.; Acar, A.; Ermini, L.; Chkhaidze, K.; Werner, B.; Mair, R.; et al. Evolutionary dynamics of residual disease in human glioblastoma. Ann. Oncol. 2019, 30, 456–463. [Google Scholar] [CrossRef]
- Mirchia, K.; Sathe, A.A.; Walker, J.M.; Fudym, Y.; Galbraith, K.; Viapiano, M.S.; Corona, R.J.; Snuderl, M.; Xing, C.; Hatanpaa, K.J.; et al. Total copy number variation as a prognostic factor in adult astrocytoma subtypes. Acta Neuropathol. Commun. 2019, 7, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Pisapia, D.J. The Updated World Health Organization Glioma Classification: Cellular and Molecular Origins of Adult Infiltrating Gliomas. Arch. Pathol. Lab. Med. 2017, 141, 1633–1645. [Google Scholar] [CrossRef] [PubMed]
- Cohen, A.; Sato, M.; Aldape, K.; Mason, C.C.; Alfaro-Munoz, K.; Heathcock, L.; South, S.T.; Abegglen, L.M.; Schiffman, J.D.; Colman, H. DNA copy number analysis of Grade II–III and Grade IV gliomas reveals differences in molecular ontogeny including chromothripsis associated with IDH mutation status. Acta Neuropathol. Commun. 2015, 3, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Lassman, A.B.; Roberts-Rapp, L.A.; Sokolova, I.; Song, M.; Pestova, E.; Kular, R.; Mullen, C.; Zha, Z.; Lu, X.; Gomez, E.; et al. Comparison of Biomarker Assays for EGFR: Implications for Precision Medicine in Patients with Glioblastoma. Clin. Cancer Res. 2019, 25, 3259–3265. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; Diaz, A.K.; Paugh, B.S.; Rankin, S.L.; Ju, B.; Li, Y.; Zhu, X.; Qu, C.; Chen, X.; Zhang, J.; et al. The genomic landscape of diffuse intrinsic pontine glioma and pediatric non-brainstem high-grade glioma. Nat. Genet. 2014, 46, 444–450. [Google Scholar] [CrossRef]
- Fan, Q.W.; Weiss, W.A. Targeting the RTK-PI3K-mTOR axis in malignant glioma: Overcoming resistance. Curr. Top. Microbiol. Immunol. 2010, 347, 279–296. [Google Scholar] [CrossRef]
- Li, X.; Wu, C.; Chen, N.; Gu, H.; Yen, A.; Cao, L.; Wang, E.; Wang, L. PI3K/Akt/mTOR signaling pathway and targeted therapy for glioblastoma. Oncotarget 2016, 7, 33440–33450. [Google Scholar] [CrossRef]
- Lorusso, P.M. Inhibition of the PI3K/AKT/mTOR Pathway in Solid Tumors. J. Clin. Oncol. 2016, 34, 3803–3815. [Google Scholar] [CrossRef] [PubMed]
- Cheng, F.; Guo, D. MET in glioma: Signaling pathways and targeted therapies. J. Exp. Clin. Cancer Res. 2019, 38, 1–13. [Google Scholar] [CrossRef]
- Stechishin, O.D.; Luchman, H.A.; Ruan, Y.; Blough, M.D.; Nguyen, S.A.; Kelly, J.J.; Cairncross, J.G.; Weiss, S. On-target JAK2/STAT3 inhibition slows disease progression in orthotopic xenografts of human glioblastoma brain tumor stem cells. Neuro Oncol. 2012, 15, 198–207. [Google Scholar] [CrossRef] [PubMed]
- Bazzoni, R.; Bentivegna, A. Role of Notch Signaling Pathway in Glioblastoma Multiforme Pathogenesis. Cancers 2019, 11, 292. [Google Scholar] [CrossRef] [PubMed]
- Gersey, Z.; Osiason, A.D.; Bloom, L.; Shah, S.; Thompson, J.W.; Bregy, A.; Agarwal, N.; Komotar, R.J. Therapeutic Targeting of the Notch Pathway in Glioblastoma Multiforme. World Neurosurg. 2019, 131, 252–263.e2. [Google Scholar] [CrossRef]
- Liang, J.; Meng, Q.; Zhao, W.; Tong, P.; Li, P.; Zhao, Y.; Zhao, X.; Li, H. An expression based REST signature predicts patient survival and therapeutic response for glioblastoma multiforme. Sci. Rep. 2016, 6, 34556. [Google Scholar] [CrossRef]
- Pisapia, D.J.; Ohara, K.; Bareja, R.; Wilkes, D.C.; Hissong, E.; Croyle, J.A.; Kim, J.-H.; Saab, J.; Macdonald, T.Y.; Beg, S.; et al. Fusions involving BCOR and CREBBP are rare events in infiltrating glioma. Acta Neuropathol. Commun. 2020, 8, 80. [Google Scholar] [CrossRef]
- Meyer, S.N.; Scuoppo, C.; Vlasevska, S.; Bal, E.; Holmes, A.B.; Holloman, M.; Garcia-Ibanez, L.; Nataraj, S.; Duval, R.; Vantrimpont, T.; et al. Unique and Shared Epigenetic Programs of the CREBBP and EP300 Acetyltransferases in Germinal Center B Cells Reveal Targetable Dependencies in Lymphoma. Immunity 2019, 51, 535–547.e9. [Google Scholar] [CrossRef]
- Ring, A.; Kaur, P.; Lang, J.E. EP300 knockdown reduces cancer stem cell phenotype, tumor growth and metastasis in triple negative breast cancer. BMC Cancer 2020, 20, 1–14. [Google Scholar] [CrossRef]
- Wang, H.; Li, F.; Liu, N.; Liu, X.; Yang, X.; Guo, Y.; Bei, J.; Zeng, Y.; Shao, J. Prognostic implications of a molecular classifier derived from whole-exome sequencing in nasopharyngeal carcinoma. Cancer Med. 2019, 8, 2705–2716. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Geng, D.; Gao, J.; Qi, Y.; Shi, Y.; Wang, Y.; Jiang, Y.; Zhang, Y.; Fu, J.; Dong, Y.; et al. Expression and significance of Hippo/YAP signaling in glioma progression. Tumor Biol. 2016, 37, 15665–15676. [Google Scholar] [CrossRef]
- Masliantsev, K.; Karayan-Tapon, L.; Guichet, P.-O. Hippo Signaling Pathway in Gliomas. Cells 2021, 10, 184. [Google Scholar] [CrossRef] [PubMed]
- Morris, L.G.; Kaufman, A.M.; Gong, Y.; Ramaswami, D.; Walsh, L.A.; Turcan, Ş.; Eng, S.; Kannan, K.; Zou, Y.; Peng, L.; et al. Recurrent somatic mutation of FAT1 in multiple human cancers leads to aberrant Wnt activation. Nat. Genet. 2013, 45, 253–261. [Google Scholar] [CrossRef]
- Laginestra, M.A.; Cascione, L.; Motta, G.; Fuligni, F.; Agostinelli, C.; Rossi, M.; Sapienza, M.R.; Righi, S.; Broccoli, A.; Indio, V.; et al. Whole exome sequencing reveals mutations in FAT1 tumor suppressor gene clinically impacting on peripheral T-cell lymphoma not otherwise specified. Mod. Pathol. 2019, 33, 179–187. [Google Scholar] [CrossRef]
- Dikshit, B.; Irshad, K.; Madan, E.; Aggarwal, N.; Sarkar, C.K.; Chandra, P.S.; Gupta, D.; Chattopadhyay, P.K.; Sinha, S.; Chosdol, K. FAT1 acts as an upstream regulator of oncogenic and inflammatory pathways, via PDCD4, in glioma cells. Oncogene 2013, 32, 3798–3808. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Xia, Q.; Liu, L.; Li, S.; Dong, L. Current Opinion on Molecular Characterization for GBM Classification in Guiding Clinical Diagnosis, Prognosis, and Therapy. Front. Mol. Biosci. 2020, 7, 241. [Google Scholar] [CrossRef] [PubMed]
- Meacham, C.E.; Morrison, S.J. Tumour heterogeneity and cancer cell plasticity. Nat. Cell Biol. 2013, 501, 328–337. [Google Scholar] [CrossRef]
- Bonavia, R.; Inda, M.-D.-M.; Cavenee, W.K.; Furnari, F.B. Heterogeneity Maintenance in Glioblastoma: A Social Network. Cancer Res. 2011, 71, 4055–4060. [Google Scholar] [CrossRef]
- Wels, J.; Kaplan, R.N.; Rafii, S.; Lyden, D. Migratory neighbors and distant invaders: Tumor-associated niche cells. Genes Dev. 2008, 22, 559–574. [Google Scholar] [CrossRef]
- Hambardzumyan, D.; Bergers, G. Glioblastoma: Defining Tumor Niches. Trends Cancer 2015, 1, 252–265. [Google Scholar] [CrossRef]
- Leite, D.M.; Zvar Baskovic, B.; Civita, P.; Neto, C.; Gumbleton, M.; Pilkington, G.J. A human co-culture cell model incorporating microglia supports glioblastoma growth and migration, and confers resistance to cytotoxics. FASEB J. 2020. [Google Scholar] [CrossRef] [PubMed]
- Filippova, N.; Nabors, L.B. Elavl1 role in cell fusion and tunneling membrane nanotube formations with implication to treat glioma heterogeneity. Cancers 2020, 12, 3069. [Google Scholar] [CrossRef] [PubMed]




| Tumor | Sex | Age | MGMT | Region | Therapy | RFS | OS |
|---|---|---|---|---|---|---|---|
| GB01 | F | 55 | 8% | Left peritrigonal area | TMZ concurrent with RT followed by adjuvant TMZ | 13 months | 20 months |
| GB02 | F | 74 | 56% | Right parietal lobe | RT | nd | nd (>6 months) |
| GB03 | F | 58 | <7% | Right frontal-temporal-parietal area | TMZ concurrent with RT followed by adjuvant TMZ | 16 months | 20 months |
| Gene | Variant | Tumor (Regions) | Genotype | Type | Cosmic | Described in CNS | VARSOME |
|---|---|---|---|---|---|---|---|
| APC | Gln163Lys | GB01-04 | het | Missense | Likely Pathogenic | ||
| ATM | Ser421Ter | GB01 (01, 02, 03, 04, 06, 07), GB02 (03, 07, 08) | het | Nonsense | COSM4165637 | Pathogenic | |
| ATR | Glu359Ter | GB02–05 | het | Nonsense | Pathogenic | ||
| Arg1951Ter | GB03–06 | het | Nonsense | COSM6933109 | Pathogenic | ||
| Gln264Ter | GB01–03 | het | Nonsense | Pathogenic | |||
| Trp2094Ter | GB01–04 | het | Nonsense | Pathogenic | |||
| BRAF | Arg271Ser | GB02–09 | het | Missense | Likely Pathogenic | ||
| Glu375Ter | GB01 (05) | het | Nonsense | COSM5702658 | Pathogenic | ||
| EGFR | Arg108Lys | GB02 (all) | het | Missense | COSM21683 | Y | Likely Pathogenic |
| Thr273Pro | GB02–02 | het | Missense | Likely Pathogenic | |||
| ERBB3 | Lys695ArgfsTer15 | GB01–04 | het | Frameshift | Pathogenic | ||
| Leu12Ter | GB01–01 | het | Nonsense | Pathogenic | |||
| c.2840-2A > G | GB01–02 | het | Splice Site | Pathogenic | |||
| KMT2D | Gln3370SerfsTer22 | GB03–03 | het | Frameshift | Pathogenic | ||
| Arg2830Ter | GB01–07 | het | Nonsense | COSM220674 | Y | Pathogenic | |
| MET | Thr230ArgfsTer33 | GB01–05 | het | Frameshift | Pathogenic | ||
| Asp449HisfsTer4 | GB01–08 | het | Frameshift | Pathogenic | |||
| MSH6 | Ala1302GlufsTer25 | GB01–09 | het | Frameshift | Pathogenic | ||
| Phe115LeufsTer34 | GB01–09 | het | Frameshift | Pathogenic | |||
| Phe1088SerfsTer2 | GB01–09, GB02 (05, 06), GB03 (08) | het | Frameshift | Pathogenic | |||
| MYC | Thr73Pro | GB01–01 | het | Missense | Likely Pathogenic | ||
| NOTCH1 | Val1229LeufsTer216 | GB01–03 | het | Frameshift | Pathogenic | ||
| His2275ProfsTer20 | GB01–08 | het | Frameshift | Pathogenic | |||
| Met2237CysfsTer11 | GB03–02 | het | Frameshift | Pathogenic | |||
| c.1556-2A > C | GB02 (02, 05) | het | Splice Site | Pathogenic | |||
| c.4587-2A > C | GB03 (08) | het | Splice Site | Pathogenic | |||
| Gly1339AlafsTer106 | GB03–06 | het | Splice Site | Pathogenic | |||
| PIK3CA | Ser1003Leu | GB01–01 | het | Missense | COSM5700983 | Likely Pathogenic | |
| Leu649Ile | GB01–03 | het | Missense | Likely Pathogenic | |||
| Ile391Lys | GB01–08 | het | Missense | Likely Pathogenic | |||
| Phe667Cys | GB02–01 | het | Missense | Likely Pathogenic | |||
| Cys838Trp | GB03–05 | het | Missense | Likely Pathogenic | |||
| Met1043Ile | GB03 (all) | het | Missense | COSM773 | Pathogenic | ||
| c.1540-1G > T | GB03–02 | het | Splice Site | Pathogenic | |||
| PTEN | Asp52Asn | GB01 (all) | het | Missense | COSM5059 | Likely Pathogenic | |
| Trp274Cys | GB02–06 | het | Missense | Likely Pathogenic | |||
| His272Gln | GB02–07 | het | Missense | Pathogenic | |||
| c.1027-2delA | GB01–07 | het | Splice Site | Pathogenic | |||
| RB1 | Leu337TrpfsTer12 | GB01–04 | het | Frameshift | Pathogenic | ||
| Leu683Pro | GB01–01 | het | Missense | Likely Pathogenic | |||
| Leu448Ile | GB01–02 | het | Missense | Likely Pathogenic | |||
| Leu400Met | GB01–04 | het | Missense | Likely Pathogenic | |||
| His483Asn | GB01–05 | het | Missense | Likely Pathogenic | |||
| Ile711Leu | GB02–07 | het | Missense | Likely Pathogenic | |||
| Glu465Ter | GB01–05 | het | Nonsense | COSM6936008 | Pathogenic | ||
| Tyr446Ter | GB02–02 | het | Nonsense | Pathogenic | |||
| Ser474Ile | GB01 (01–07) GB02 (03, 04, 08, 09) | het | Splice Site | COSM4807851 | Pathogenic | ||
| c.1421 + 1G > T | GB01 (02, 03, 05), GB02 (03) | het | Splice Site | Pathogenic | |||
| SF3B1 | Tyr623His | GB01–01 | het | Missense | Likely Pathogenic | ||
| Ile704Met | GB03–03 | het | Missense | Likely Pathogenic | |||
| Glu62Ter | GB03–03 | het | Nonsense | Pathogenic | |||
| Gln1252His | GB02–03 | het | Splice Site | Likely Pathogenic | |||
| Gln1252Ter | GB01–09 | het | Splice Site | Pathogenic | |||
| SOX2 | Arg57AlafsTer46 | GB01–08 | het | Frameshift | Pathogenic | ||
| Ala94Asp | GB01–08 | het | Missense | Likely Pathogenic | |||
| TERT | Ile1046Ter | GB01–09 | het | Frameshift | Pathogenic | ||
| c.2582 + 2T > G | GB02–08 | het | Splice Site | Pathogenic | |||
| TP53 | Tyr103Ser | GB02–09 | het | Missense | Likely Pathogenic | ||
| Gln144Ter | GB01–01 | het | Nonsense | Pathogenic |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Franceschi, S.; Civita, P.; Pasqualetti, F.; Lessi, F.; Modena, M.; Barachini, S.; Morelli, M.; Santonocito, O.; Vannozzi, R.; Pilkington, G.J.; et al. Multiregional Sequencing of IDH-WT Glioblastoma Reveals High Genetic Heterogeneity and a Dynamic Evolutionary History. Cancers 2021, 13, 2044. https://doi.org/10.3390/cancers13092044
Franceschi S, Civita P, Pasqualetti F, Lessi F, Modena M, Barachini S, Morelli M, Santonocito O, Vannozzi R, Pilkington GJ, et al. Multiregional Sequencing of IDH-WT Glioblastoma Reveals High Genetic Heterogeneity and a Dynamic Evolutionary History. Cancers. 2021; 13(9):2044. https://doi.org/10.3390/cancers13092044
Chicago/Turabian StyleFranceschi, Sara, Prospero Civita, Francesco Pasqualetti, Francesca Lessi, Martina Modena, Serena Barachini, Mariangela Morelli, Orazio Santonocito, Riccardo Vannozzi, Geoffrey J. Pilkington, and et al. 2021. "Multiregional Sequencing of IDH-WT Glioblastoma Reveals High Genetic Heterogeneity and a Dynamic Evolutionary History" Cancers 13, no. 9: 2044. https://doi.org/10.3390/cancers13092044
APA StyleFranceschi, S., Civita, P., Pasqualetti, F., Lessi, F., Modena, M., Barachini, S., Morelli, M., Santonocito, O., Vannozzi, R., Pilkington, G. J., Ortenzi, V., Naccarato, A. G., Aretini, P., & Mazzanti, C. M. (2021). Multiregional Sequencing of IDH-WT Glioblastoma Reveals High Genetic Heterogeneity and a Dynamic Evolutionary History. Cancers, 13(9), 2044. https://doi.org/10.3390/cancers13092044











