Safety and Efficacy of Salvage Neck Dissection Following Carbon-ion Radiotherapy with Chemotherapy for a Patient with Mucosal Malignant Melanoma of Head and Neck
Abstract
:1. Introduction
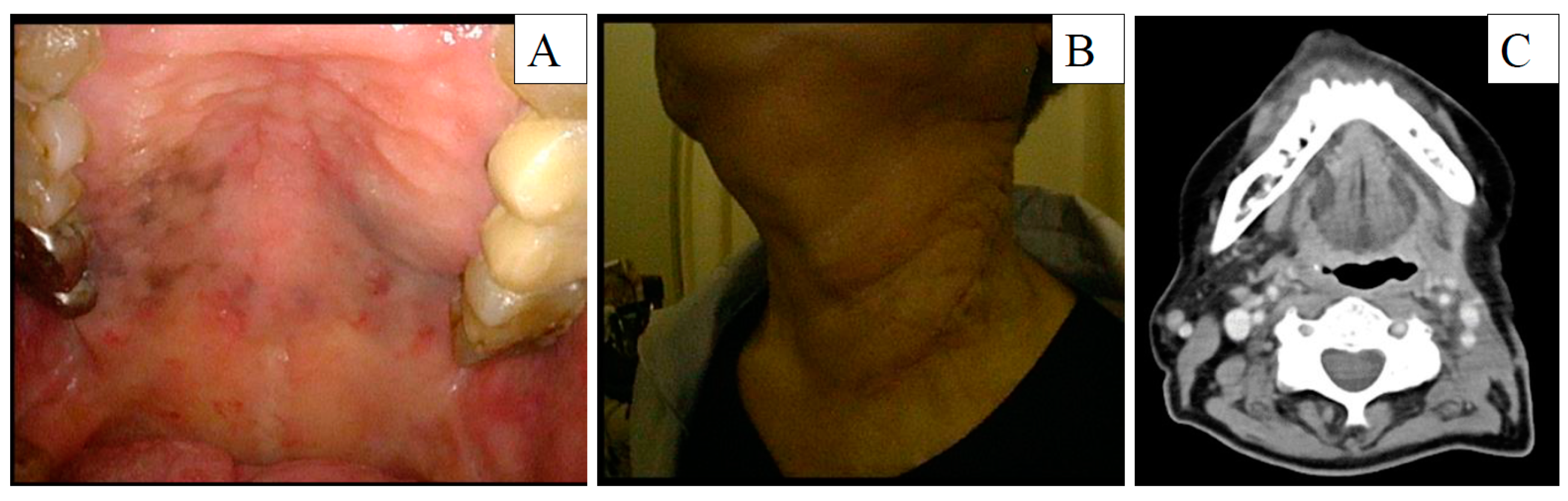
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Green:, B.; Elhamshary, A.; Gomez, R.; Rahimi, S.; Brennan, P.A. An update on the current management of head and neck mucosal melanoma. J. Oral Pathol. Med. 2017, 46, 475–479. [Google Scholar] [CrossRef] [PubMed]
- López, F.; Rodrigo, J.P.; Cardesa, A.; Triantafyllou, A.; Devaney, K.O.; Mendenhall, W.M.; Haigentz, M., Jr.; Strojan, P.; Pellitteri, P.K.; Bradford, C.R.; et al. Update on primary head and neck mucosal melanoma. Head Neck 2016, 38, 147–155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zenda, S.; Akimoto, T.; Mizumoto, M.; Hayashi, R.; Arahira, S.; Okumura, T.; Sakurai, H. Phase II study of proton beam therapy as a nonsurgical approach for mucosal melanoma of the nasal cavity or para-nasal sinuses. Radiother. Oncol. 2016, 118, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Ikawa, H.; Koto, M.; Demizu, Y.; Saitoh, J.I.; Suefuji, H.; Okimoto, T.; Ohno, T.; Shioyama, Y.; Takagi, R.; Hayashi, K.; et al. Multicenter study of carbon-ion radiation therapy for nonsquamous cell carcinomas of the oral cavity. Cancer Med. 2019, 8, 4547–4554. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, Y.; Saikawa, M. Update on the classification and nomenclature system for neck dissection: Revisions proposed by the Japan Neck Dissection Study Group. Int. J. Clin. Oncol. 2010, 15, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.; Takano, G.; Hanai, N.; Nishikawa, D.; Koide, Y.; Beppu, S.; Hasegawa, Y. Primary tumor size predicts distant metastasis of mucosal malignant melanoma in head and neck. Anticancer Res. 2018, 38, 6485–6490. [Google Scholar] [CrossRef] [PubMed]
- Ohtaki, Y.; Shimizu, K.; Saitoh, J.I.; Kamiyoshihara, M.; Mogi, A.; Nakazawa, S.; Ohno, T.; Shirabe, K. Is salvage surgery for patients with lung cancer after carbon ion radiotherapy easy or difficult? Interact. Cardiovasc. Thorac. Surg. 2019, 28, 953–956. [Google Scholar] [CrossRef] [PubMed]
- Mizobuchi, T.; Yamamoto, N.; Nakajima, M.; Baba, M.; Miyoshi, K.; Nakayama, H.; Watanabe, S.; Katoh, R.; Kohno, T.; Kamiyoshihara, M.; et al. Salvage surgery for local recurrence after carbon ion radiotherapy for patients with lung cancer. Eur. J. Cardiothorac. Surg. 2016, 49, 1503–1509. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naganawa, K.; Koto, M.; Takagi, R.; Hasegawa, A.; Ikawa, H.; Shimozato, K.; Kamada, T.; Okamoto, Y. Organizing Committee for the Working Group for Head-and-Neck Cancer. Long-term outcomes after carbon-ion radiotherapy for oral mucosal malignant melanoma. J. Radiat. Res. 2017, 58, 517–522. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kohyama, K.; Yamada, K.; Sugiura, H.; Hyodo, I.; Ozawa, T.; Hasegawa, Y.; Kato, H.; Kamei, Y. Salvage surgery and microsurgical reconstruction for recurrence of skull base osteosarcoma after carbon ion radiotherapy. Nagoya J. Med. Sci. 2015, 77, 667–673. [Google Scholar] [PubMed]




© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suzuki, H.; Sasaki, E.; Motai, R.; Goto, S.; Nishikawa, D.; Beppu, S.; Terada, H.; Sawabe, M.; Hanai, N. Safety and Efficacy of Salvage Neck Dissection Following Carbon-ion Radiotherapy with Chemotherapy for a Patient with Mucosal Malignant Melanoma of Head and Neck. Diagnostics 2020, 10, 82. https://doi.org/10.3390/diagnostics10020082
Suzuki H, Sasaki E, Motai R, Goto S, Nishikawa D, Beppu S, Terada H, Sawabe M, Hanai N. Safety and Efficacy of Salvage Neck Dissection Following Carbon-ion Radiotherapy with Chemotherapy for a Patient with Mucosal Malignant Melanoma of Head and Neck. Diagnostics. 2020; 10(2):82. https://doi.org/10.3390/diagnostics10020082
Chicago/Turabian StyleSuzuki, Hidenori, Eiichi Sasaki, Risa Motai, Seiya Goto, Daisuke Nishikawa, Shintaro Beppu, Hoshino Terada, Michi Sawabe, and Nobuhiro Hanai. 2020. "Safety and Efficacy of Salvage Neck Dissection Following Carbon-ion Radiotherapy with Chemotherapy for a Patient with Mucosal Malignant Melanoma of Head and Neck" Diagnostics 10, no. 2: 82. https://doi.org/10.3390/diagnostics10020082



