Comparative Analysis of Examination Methods for Periapical Lesion Diagnostics: Assessing Cone-Beam Computer Tomography, Ultrasound, and Periapical Radiography
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Inclusion and Exclusion Criteria
2.3. Examination
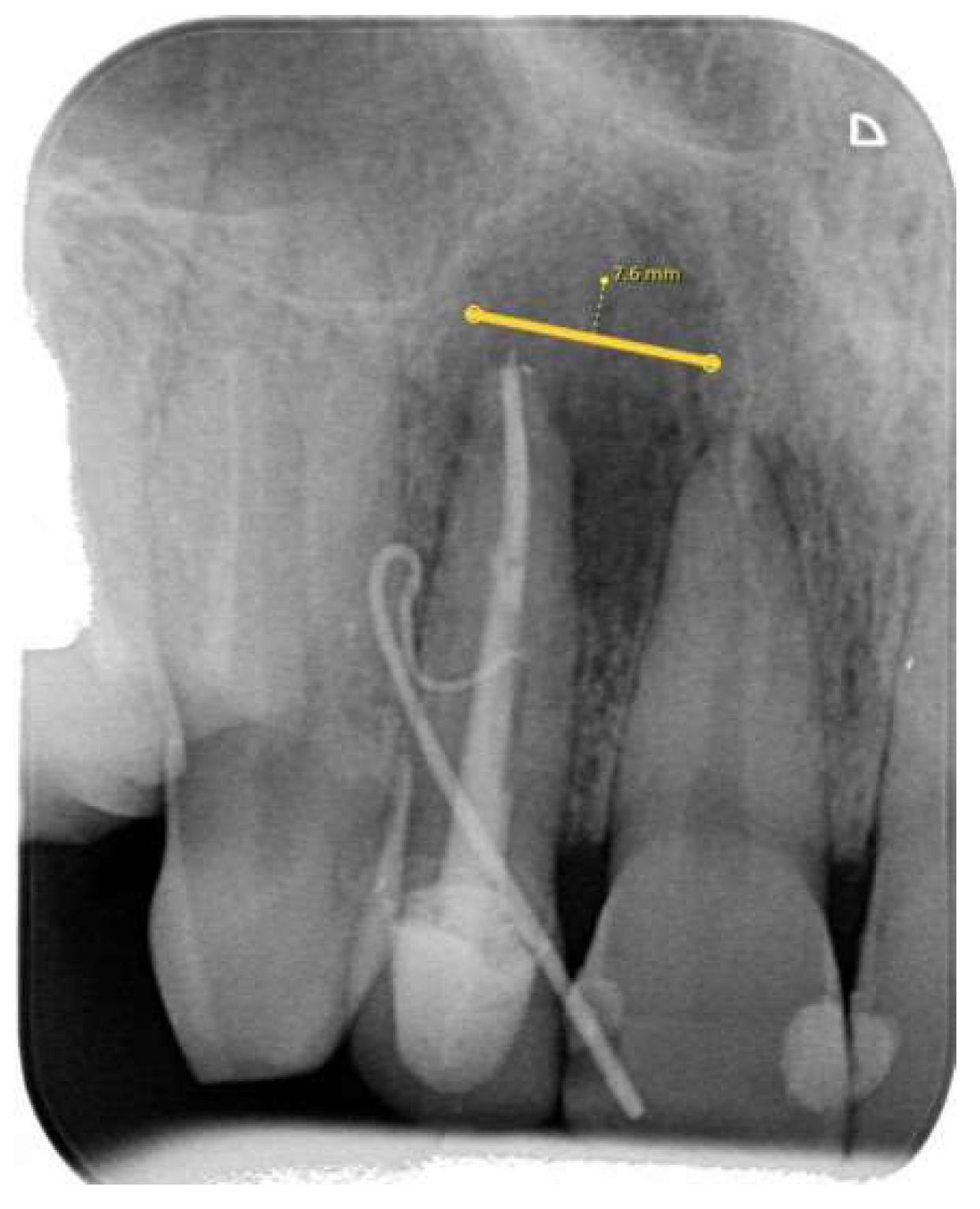
2.3.1. Periapical (PA) Radiography Examination and Evaluation
- Category 1: no discernible periapical lesion was identified;
- Category 2: a periapical lesion was possibly present, however, the distinction was not unequivocal;
- Category 3: a periapical lesion was definitively observed.
2.3.2. Cone-Beam Computer Tomography (CBCT) Radiographic Examination and Evaluation
2.3.3. Ultrasound Examination and Evaluation
2.4. Statistical Analysis
3. Results
3.1. Comparison of Examination Methods
3.2. Observers’ Agreement: Assessing Periapical Lesions through Qualitative and Quantitative Evaluation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Karamifar, K.; Tondari, A.; Saghiri, M.A. Endodontic Periapical Lesion: An Overview on the Etiology, Diagnosis and Current Treatment Modalities. Eur. Endod. J. 2020, 5, 54–67. [Google Scholar] [CrossRef] [PubMed]
- Reit, C.; Petersson, K.; Molven, O.P.K.M.O.; Reit, C. Textbook of Endodontology. In Diagnosis of Pulpal and Periradicular Disease, 1st ed.; Blackwell Publishing Ltd.: Oxford, UK, 2003. [Google Scholar]
- Weber, A.L. Imaging of the paranasal sinuses and oromaxillofacial region imaging of cysts and odontogenic tumors of the jaw. Definition and classification. Radiol. Clin. N. Am. 1993, 31, 101–120. [Google Scholar] [CrossRef] [PubMed]
- Shah, N. Recent advances in imaging technologies in dentistry. World J. Radiol. 2014, 6, 794. [Google Scholar] [CrossRef] [PubMed]
- Musu, D.; Rossi-Fedele, G.; Campisi, G.; Cotti, E. Ultrasonography in the diagnosis of bone lesions of the jaws: A systematic review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 122, e19–e29. [Google Scholar] [CrossRef]
- Special Committee to Revise the Joint AAE/AAOMR Position Statement on use of CBCT in Endodontics. AAE and AAOMR Joint Position Statement: Use of Cone Beam Computed Tomography in Endodontics 2015 Update. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 120, 508–512. [Google Scholar] [CrossRef] [PubMed]
- Chugal, N.; Assad, H.; Markovic, D.; Mallya, S.M. Applying the American Association of Endodontists and American Academy of Oral and Maxillofacial Radiology guidelines for cone-beam computed tomography prescription: Impact on endodontic clinical decisions. J. Am. Dent. Assoc. 2024, 155, 48–58. [Google Scholar] [CrossRef]
- American Association of Endodontists. The Impact of Cone Beam Computer Tomography in Endodontics: A New Era in Diagnosis and Treatment Planning; American Association of Endodontists: Chicago, IL, USA, 2018. [Google Scholar]
- Natkin, R.J.; Oswald, L.; Seattle, W. The relationship of lesion size to diagnosis, incidence, and treatment of periapical cysts and granulomas. Oral Surg. Oral Med. Oral Pathol. 1984, 57, 82–94. [Google Scholar] [CrossRef]
- Valizadeh, S.; Tavakkoli, M.A.; Vasigh, H.K.; Azizi, Z.; Zarrabian, T. Evaluation of Cone Beam Computed Tomography (CBCT) System: Comparison with Intraoral Periapical Radiography in Proximal Caries Detection. J. Dent. Res. Dent. Clin. Dent. Prospect. 2012, 6, 1–5. [Google Scholar] [CrossRef]
- De Vos, W.; Casselman, J.; Swennen, G.R.J. Cone-beam computerized tomography (CBCT) imaging of the oral and maxillofacial region: A systematic review of the literature. Int. J. Oral Maxillofac. Surg. 2009, 38, 609–625. [Google Scholar] [CrossRef]
- Signorelli, L.; Patcas, R.; Peltomäki, T.; Schätzle, M. Radiation dose of cone-beam computed tomography compared to conventional radiographs in orthodontics. J. Orofac. Orthop. 2016, 77, 9–15. [Google Scholar] [CrossRef]
- Li, G. Patient radiation dose and protection from cone-beam computed tomography. Imaging Sci. Dent. 2013, 43, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Simon, J.H.; Sedghizadeh, P.; Soliman, O.N.; Chapman, T.; Enciso, R. Evaluation of the reliability and accuracy of using cone-beam computed tomography for diagnosing periapical cysts from granulomas. J. Endod. 2013, 39, 1485–1490. [Google Scholar] [CrossRef] [PubMed]
- Theodorakou, C.; Walker, A.; Horner, K.; Pauwels, R.; Bogaerts, R.; Jacobs, R. Estimation of paediatric organ and effective doses from dental cone beam CT using anthropomorphic phantoms. Br. J. Radiol. 2012, 85, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Stokes, K.; Thieme, R.; Jennings, E.; Sholapurkar, A. Cone beam computed tomography in dentistry: Practitioner awareness and attitudes. A scoping review. Aust. Dent. J. 2021, 66, 234–245. [Google Scholar] [CrossRef]
- Kruse, C.; Spin-Neto, R.; Wenzel, A.; Kirkevang, L.L. Cone beam computed tomography and periapical lesions: A systematic review analysing studies on diagnostic efficacy by a hierarchical model. Int. Endod. J. 2015, 48, 815–828. [Google Scholar] [CrossRef]
- Lizio, G.; Salizzoni, E.; Coe, M.; Gatto, M.R.; Asioli, S.; Balbi, T.; Pelliccioni, G.A. Differential diagnosis between a granuloma and radicular cyst: Effectiveness of magnetic resonance imaging. Int. Endod. J. 2018, 51, 1077–1087. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, R.E.; Heiland, M.; Bartel-Friedrich, S. Potentials of ultrasound in the diagnosis of midfacial fractures*. Clin. Oral Investig. 2003, 7, 226–229. [Google Scholar] [CrossRef]
- Cotti, E.; Campisi, G. Advanced radiographic techniques for the detection of lesions in bone. Endod. Top. 2004, 7, 52–72. [Google Scholar] [CrossRef]
- Arslan, Z.B.; Demir, H.; Yıldız, D.B.; Yaşar, F. Diagnostic accuracy of panoramic radiography and ultrasonography in detecting periapical lesions using periapical radiography as a gold standard. Dentomaxillofacial Radiol. 2020, 49, 20190290. [Google Scholar] [CrossRef]
- Jia, W.; Jing, H.; Xia, G.; Angang, D.; Wei, Z.; Pengfei, Z.; Shujun, R.; Mengying, M.; Zhengwei, H.; Shensheng, G. Utility of Ultrasonography for Diagnosing and Differentiating Periapical Granuloma from Radicular Cyst. Acad. Radiol. 2023, 30, 2329–2339. [Google Scholar] [CrossRef]
- Abdelsalam, T.A.; Amer, M.E.; Mahrous, A.; Abdelkader, M. Evaluation of oral and maxillofacial swellings using ultrasonographic features. Imaging Sci. Dent. 2019, 49, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Juerchott, A.; Pfefferle, T.; Flechtenmacher, C.; Mente, J.; Bendszus, M.; Heiland, S.; Hilgenfeld, T. Differentiation of periapical granulomas and cysts by using dental MRI: A pilot study. Int. J. Oral Sci. 2018, 10, 17. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Langland, O.E.; Langlais, R.P. Early pioneers of oral and maxiofacial radiology. Oral Surg. Med. Oral Pathol. Oral Radiol. Endod. 1995, 80, 496–511. [Google Scholar] [CrossRef] [PubMed]
- Masthoff, M.; Gerwing, M.; Masthoff, M.; Timme, M.; Kleinheinz, J.; Berninger, M.; Heindel, W.; Wildgruber, M.; Schülke, C. Dental Imaging-A basic guide for the radiologist. RoFo Fortschritte Auf Dem Geb. Rontgenstrahlen Bildgeb. Verfahr. 2019, 191, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Dawood, A.; Whaites, E.; Ford, T.P. New dimensions in endodontic imaging: Part 1. Conventional and alternative radiographic systems. Int. Endod. J. 2009, 42, 447–462. [Google Scholar] [CrossRef] [PubMed]
- Mozzo, P. A new volumetric CT machine for dental imaging based on the cone-beam technique: Preliminary results. Eur. Radiol. 1998, 8, 1558–1564. [Google Scholar] [CrossRef] [PubMed]
- Aboudara, C.A.; Hatcher, D.; Nielsen, I.L.; Miller, A. A three-dimensional evaluation of the upper airway in adolescents. Orthod. Craniofac. Res. 2003, 6 (Suppl. 1), 173–175. [Google Scholar] [CrossRef] [PubMed]
- Wanderley, V.A.; Leite, A.F.; de Faria Vasconcelos, K.; Pauwels, R.; Mueller-Garcia, F.; Becker, K.; Oliveira, M.L.; Jacobs, R. Impact of metal artefacts on subjective perception of image quality of 13 CBCT devices. Clin. Oral Investig. 2022, 26, 4457–4466. [Google Scholar] [CrossRef]
- Chan, F.; Brown, L.F.; Parashos, P. CBCT in contemporary endodontics. Aust. Dent. J. 2023, 68, S39–S55. [Google Scholar] [CrossRef]
- Preston, D.L.; Cullings, H.; Suyama, A.; Funamoto, S.; Nishi, N.; Soda, M.; Mabuchi, K.; Kodama, K.; Kasagi, F.; Shore, R.E. Solid Cancer Incidence in Atomic Bomb Survivors Exposed In Utero or as Young Children. J. Natl. Cancer Inst. 2008, 100, 428–436. [Google Scholar] [CrossRef]
- Zielinski, J.M.; Ashmore, P.J.; Band, P.R.; Jiang, H.; Shilnikova, N.S.; Tait, V.K.; Krewski, D. Low dose ionizing radiation exposure and cardiovascular disease mortality: Cohort study based on Canadian national dose registry of radiation workers. Int. J. Occup. Med. Environ. Health 2009, 22, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Hall, E.J.; Brenner, D.J. Cancer risks from diagnostic radiology. Br. J. Radiol. 2008, 81, 362–378. [Google Scholar] [CrossRef] [PubMed]
- Brenner, D.J.; Doll, R.; Goodhead, D.T.; Hall, E.J.; Land, C.E.; Little, J.B.; Lubin, J.H.; Preston, D.L.; Preston, R.J.; Puskin, J.S.; et al. Cancer Risks Attributable to Low Doses of Ionizing Radiation: Assessing What We Really Know. 2003. Available online: www.pnas.orgcgidoi10.1073pnas.2235592100 (accessed on 10 November 2003).
- Cotti, E.; Campisi, G.; Ambu, R.; Dettori, C. Ultrasound real-time imaging in the differential diagnosis of periapical lesions. Int. Endod. J. 2003, 36, 556–563. [Google Scholar] [CrossRef]
- Cotti, E.; Campisi, G.; Garau, V.; Puddu, G. A new technique for the study of periapical bone lesions: Ultrasound real time imaging. Int. Endod. J. 2002, 35, 148–152. [Google Scholar] [CrossRef] [PubMed]
- Raghav, N.; Reddy, S.S.; Giridhar, A.G.; Murthy, S.; Devi, B.Y.; Santana, N.; Rakesh, N.; Kaushik, A. Comparison of the efficacy of conventional radiography, digital radiography, and ultrasound in diagnosing periapical lesions. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2010, 110, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, T.L.D.; Costa, A.L.F.; Tucunduva, M.J.A.; Tucunduva-Neto, R.R.; Shinohara, E.H.; de Freitas, C.F. Ultrasound evaluation of intra-osseous cavity: A preliminary study in pig mandibles. J. Oral Biol. Craniofac. Res. 2016, 6, S14–S17. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.; Jacobs, R.; Levring Jäghagen, E.; Lindh, C.; Baksi, G.; Schulze, D.; Schulze, R. Basic training requirements for the use of dental CBCT by dentists: A position paper prepared by the European Academy of Dento Maxillo Facial Radiology. Dentomaxillofacial Radiol. 2014, 43, 20130291. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Brown, J.; Semper, M.; Abella, F.; Mannocci, F. European Society of Endodontology position statement: Use of cone beam computed tomography in Endodontics. Int. Endod. J. 2019, 52, 1675–1678. [Google Scholar] [CrossRef]
- Protection Radiation No 172. Cone Beam CT for Dental and Maxillofacial Radiology (Evidence-Based Guidelines). Available online: www.sedentexct.eu (accessed on 12 March 2012).
- Avcı, F.; Etöz, M.; Üstün, Y.; Arslan, T. Evaluation of ultrasonography as a diagnostic tool in the management of periapical cysts and granulomas: A clinical study. Imaging Sci. Dent. 2022, 52, 209. [Google Scholar] [CrossRef]






| Incisors N (%) | Canines N (%) | Premolars N (%) | Total N (%) | |
|---|---|---|---|---|
| Mandibular | 6 (14%) | 0 (0%) | 1 (2%) | 7 (16%) |
| Maxillary | 29 (68%) | 4 (9%) | 3 (7%) | 36 (84%) |
| Total | 35 (82%) | 4 (9%) | 4 (9%) | 43 (100%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karkle, A.; Slaidina, A.; Zolovs, M.; Vaskevica, A.; Meistere, D.; Bokvalde, Z.; Neimane, L. Comparative Analysis of Examination Methods for Periapical Lesion Diagnostics: Assessing Cone-Beam Computer Tomography, Ultrasound, and Periapical Radiography. Diagnostics 2024, 14, 766. https://doi.org/10.3390/diagnostics14070766
Karkle A, Slaidina A, Zolovs M, Vaskevica A, Meistere D, Bokvalde Z, Neimane L. Comparative Analysis of Examination Methods for Periapical Lesion Diagnostics: Assessing Cone-Beam Computer Tomography, Ultrasound, and Periapical Radiography. Diagnostics. 2024; 14(7):766. https://doi.org/10.3390/diagnostics14070766
Chicago/Turabian StyleKarkle, Aleksandra, Anda Slaidina, Maksims Zolovs, Anete Vaskevica, Dita Meistere, Zanda Bokvalde, and Laura Neimane. 2024. "Comparative Analysis of Examination Methods for Periapical Lesion Diagnostics: Assessing Cone-Beam Computer Tomography, Ultrasound, and Periapical Radiography" Diagnostics 14, no. 7: 766. https://doi.org/10.3390/diagnostics14070766
APA StyleKarkle, A., Slaidina, A., Zolovs, M., Vaskevica, A., Meistere, D., Bokvalde, Z., & Neimane, L. (2024). Comparative Analysis of Examination Methods for Periapical Lesion Diagnostics: Assessing Cone-Beam Computer Tomography, Ultrasound, and Periapical Radiography. Diagnostics, 14(7), 766. https://doi.org/10.3390/diagnostics14070766





