Piper nigrum Fruit Extract as an Antibiotic Resistance Reversal Agent in MDR Bacteria
Abstract
:1. Introduction
2. Materials and Methods
2.1. Plant Material and Herbarium Number
2.2. Plant Extract Preparation
2.2.1. Cleaning of Plant Material
2.2.2. Extraction and Fractionation
2.2.3. Bacterial Strain
2.3. Antibiotic Susceptibility Test (AST)
2.4. Antibiotic Resistance Reversal Activity
3. Results
3.1. Antibiotic Susceptibility
3.2. Antibiotic Resistance Reversal of S. aureus by P. nigrum Extracts
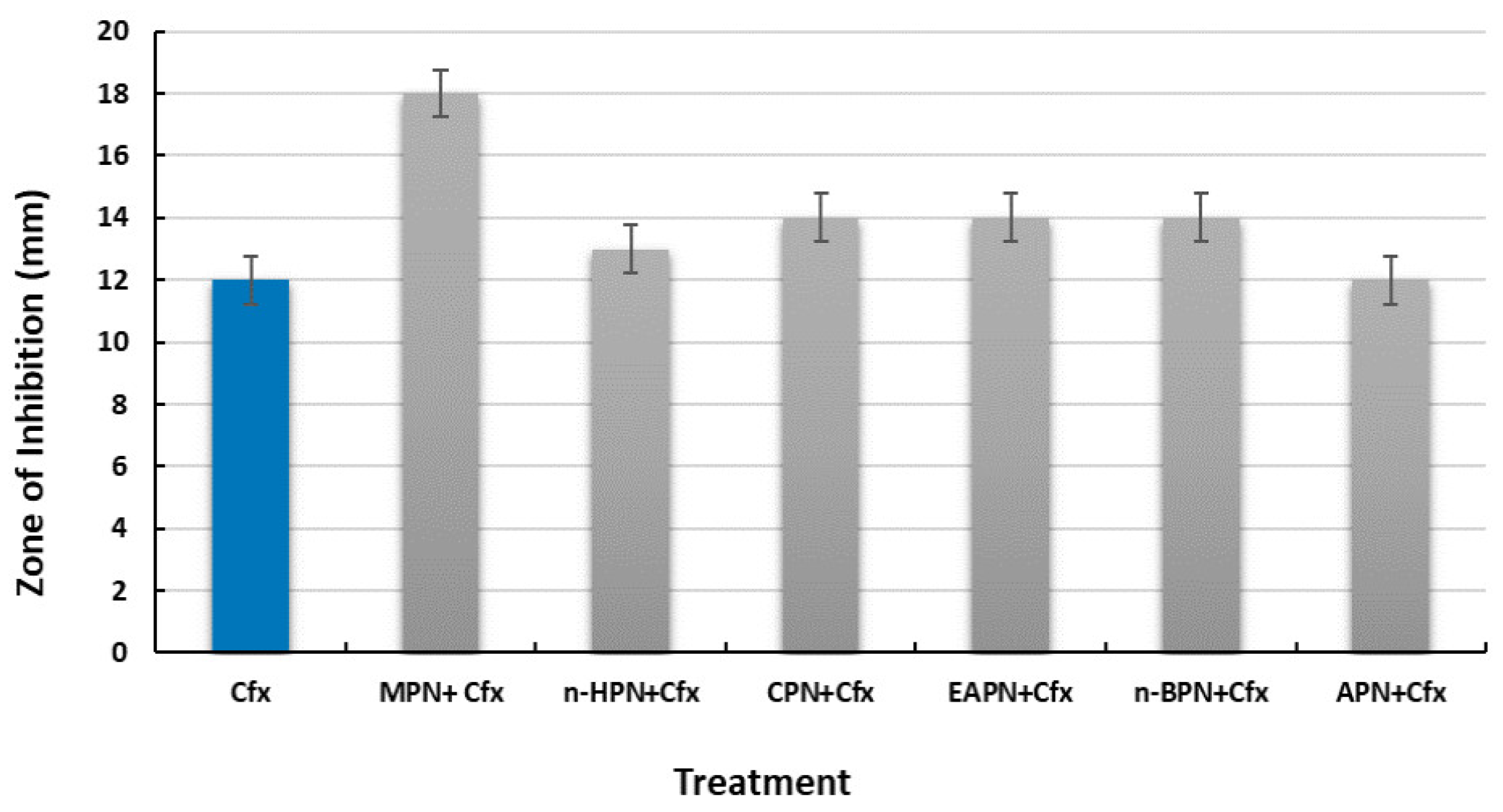
3.2.1. Cefoxitin
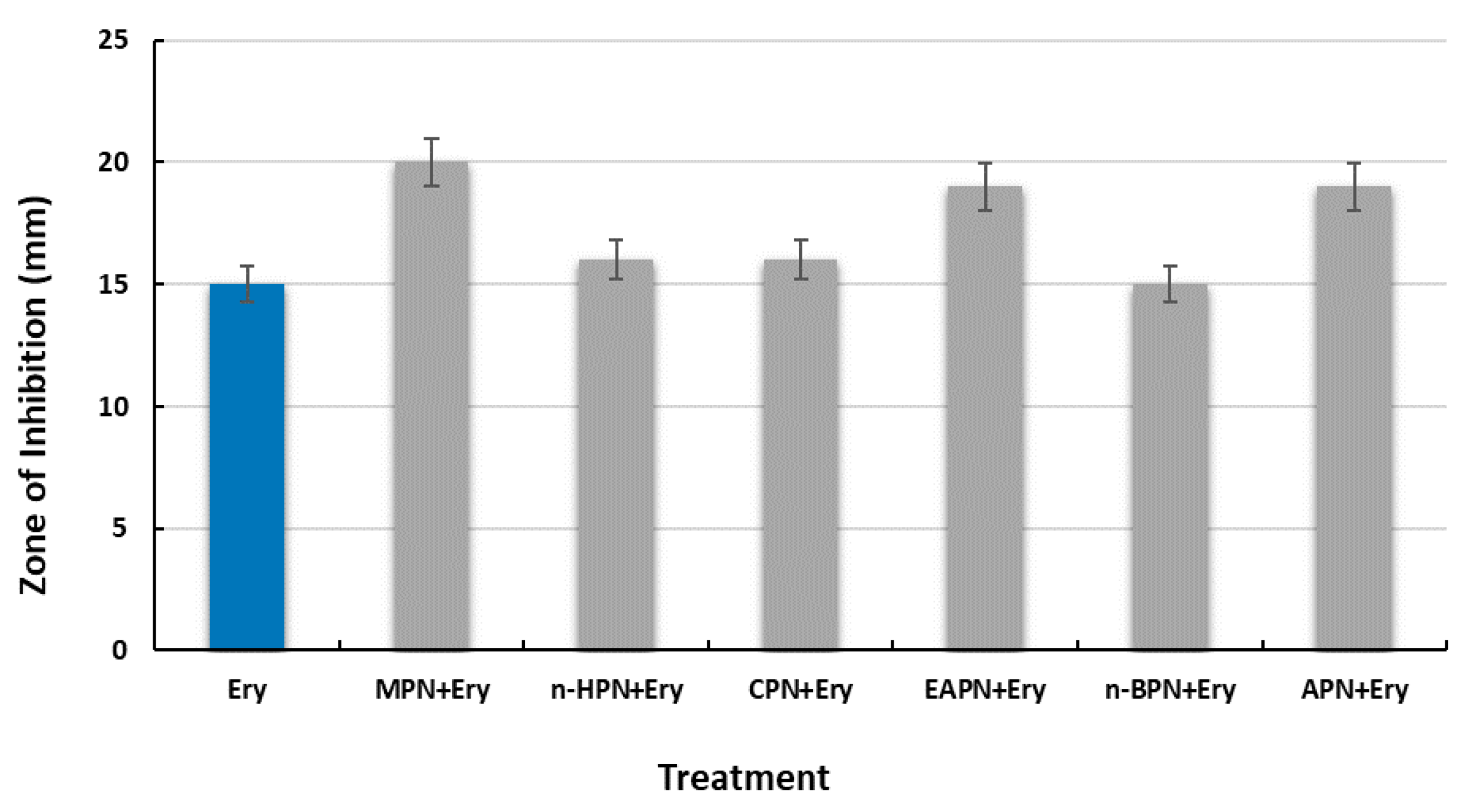
3.2.2. Erythromycin
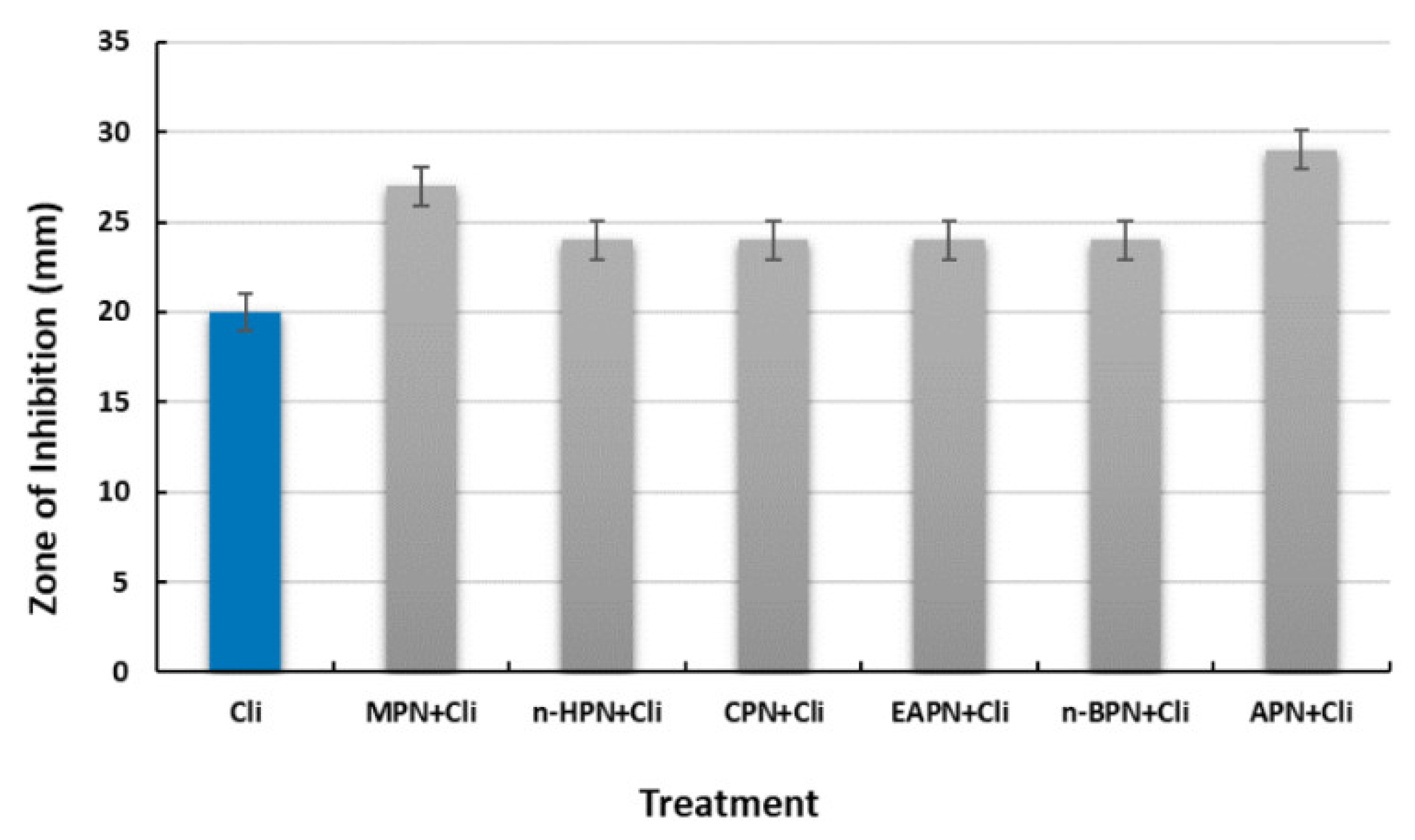
3.2.3. Clindamycin
3.2.4. Levofloxacin
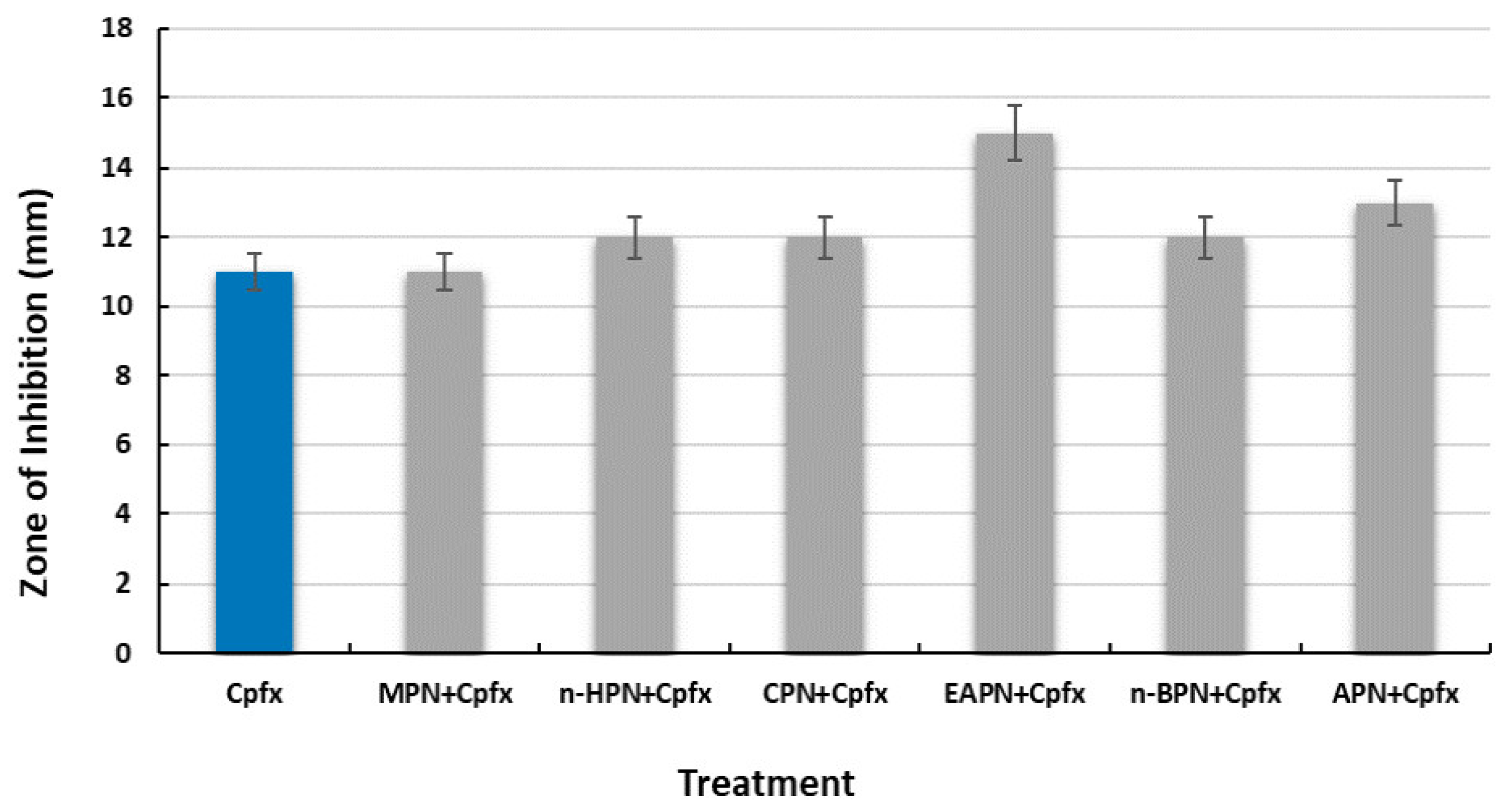
3.2.5. Ciprofloxacin
3.2.6. Amikacin
3.2.7. Gentamicin
3.3. Antibiotic Resistance Reversal of S. typhi by P. nigrum Extracts
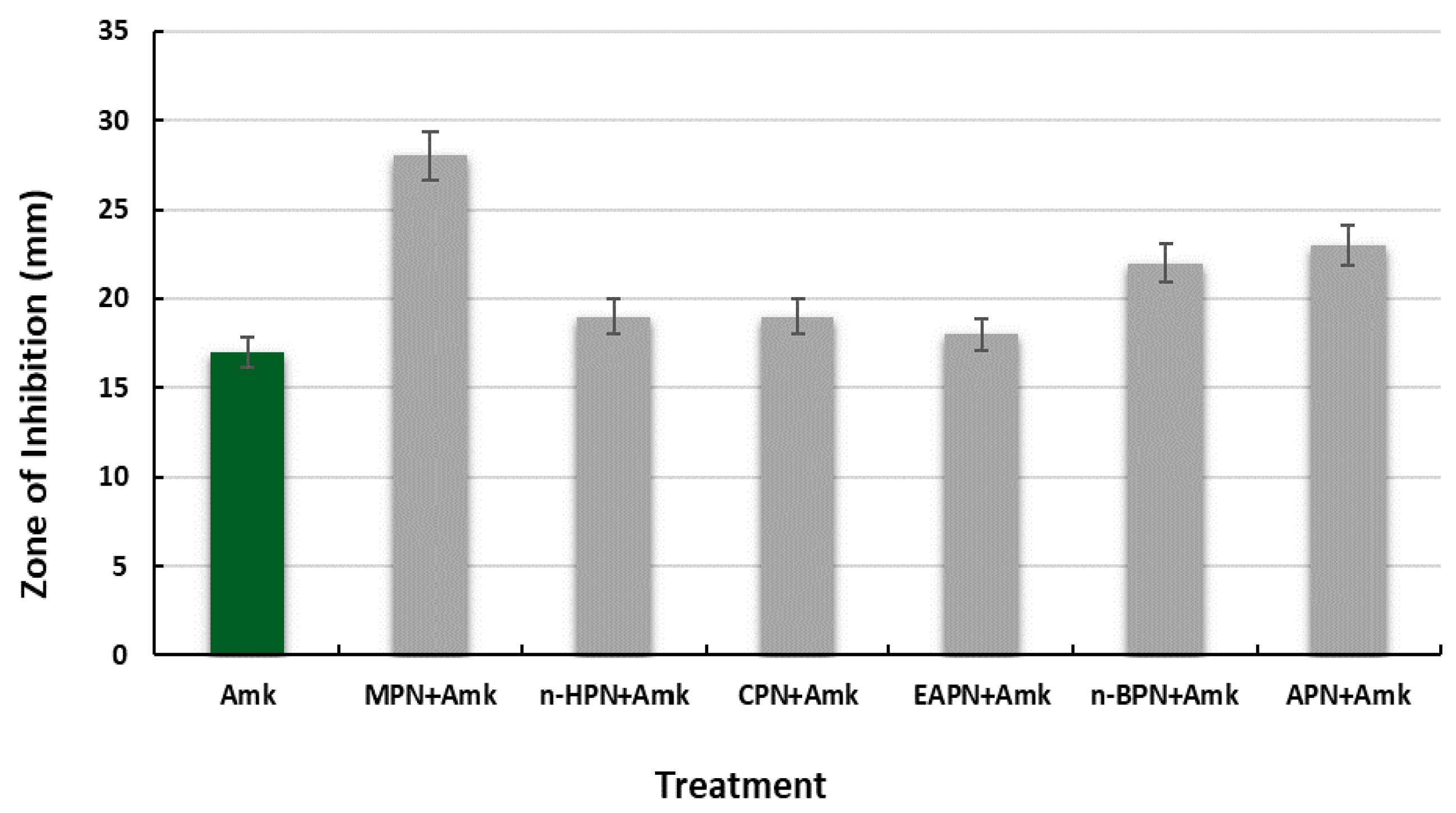
3.3.1. Amikacin
3.3.2. Gentamicin
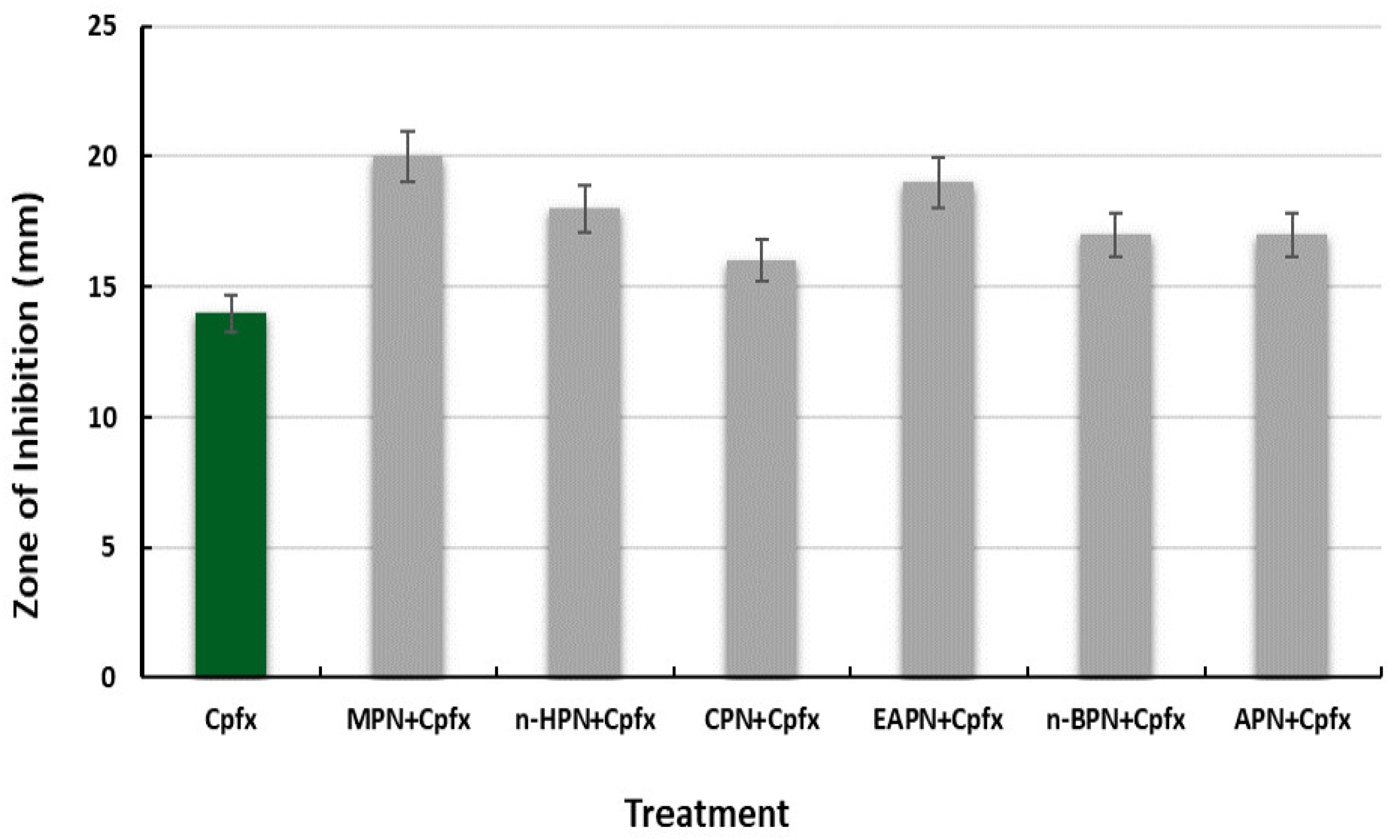
3.3.3. Ciprofloxacin
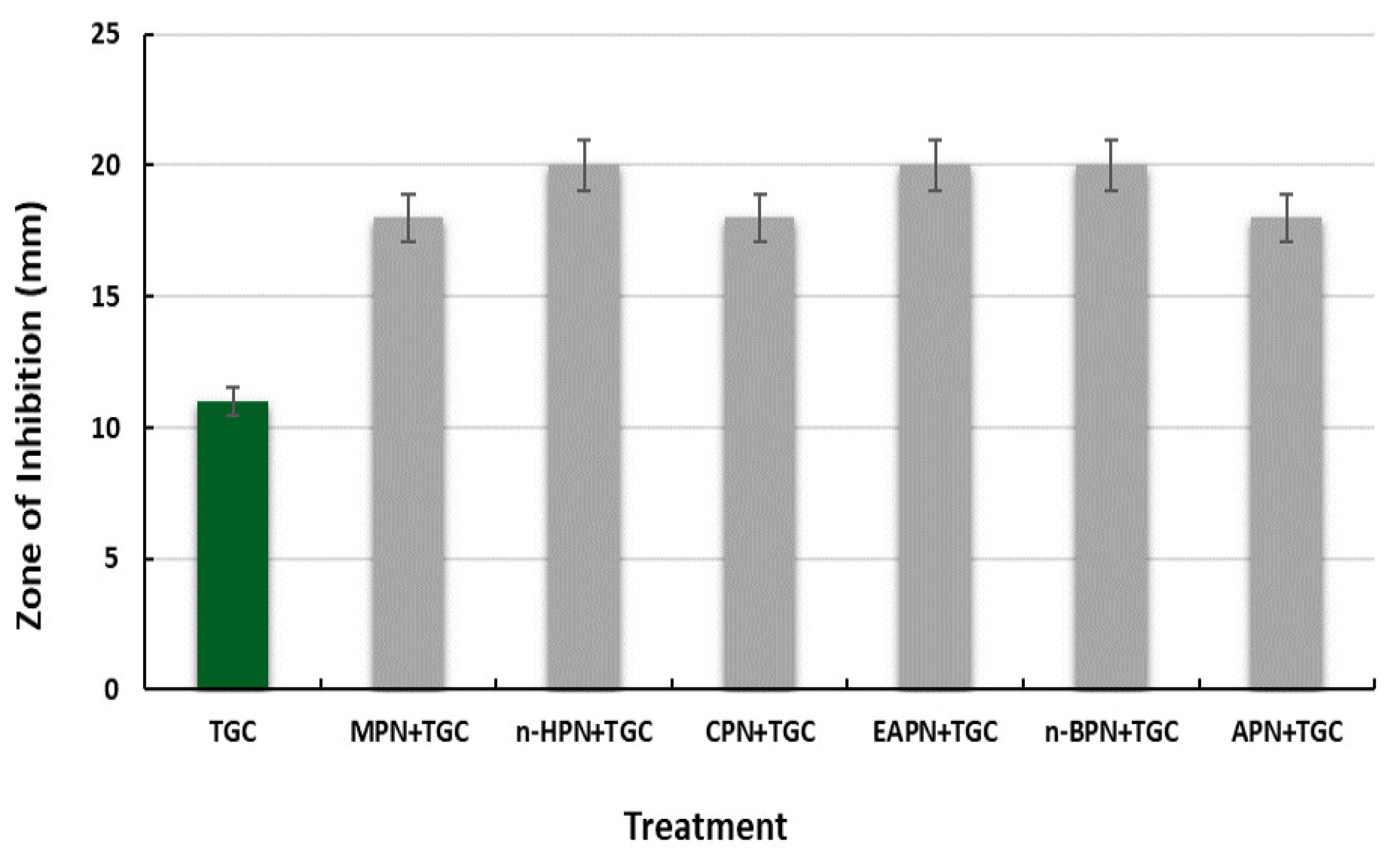
3.3.4. Tigecycline
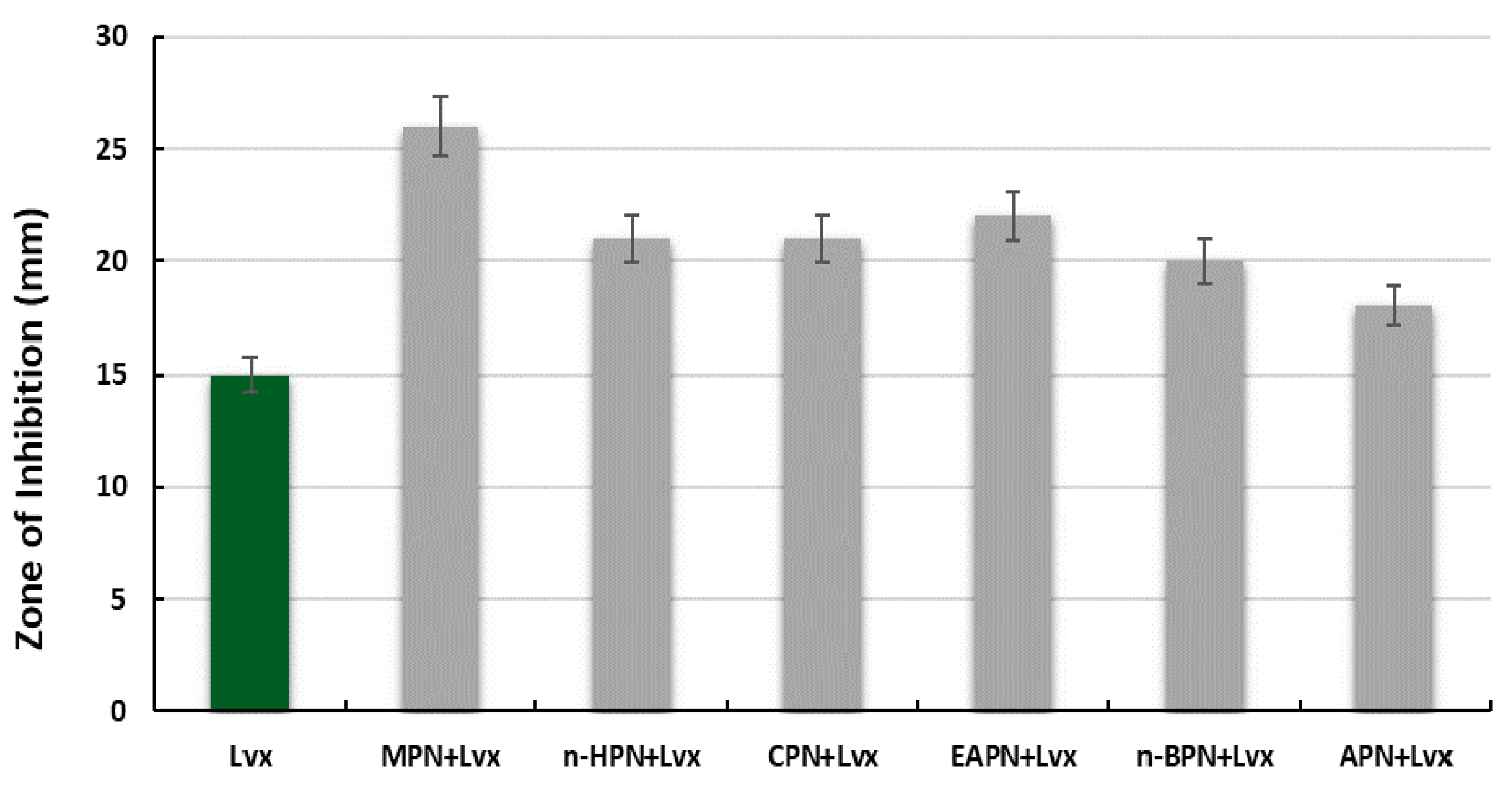
3.3.5. Levofloxacin
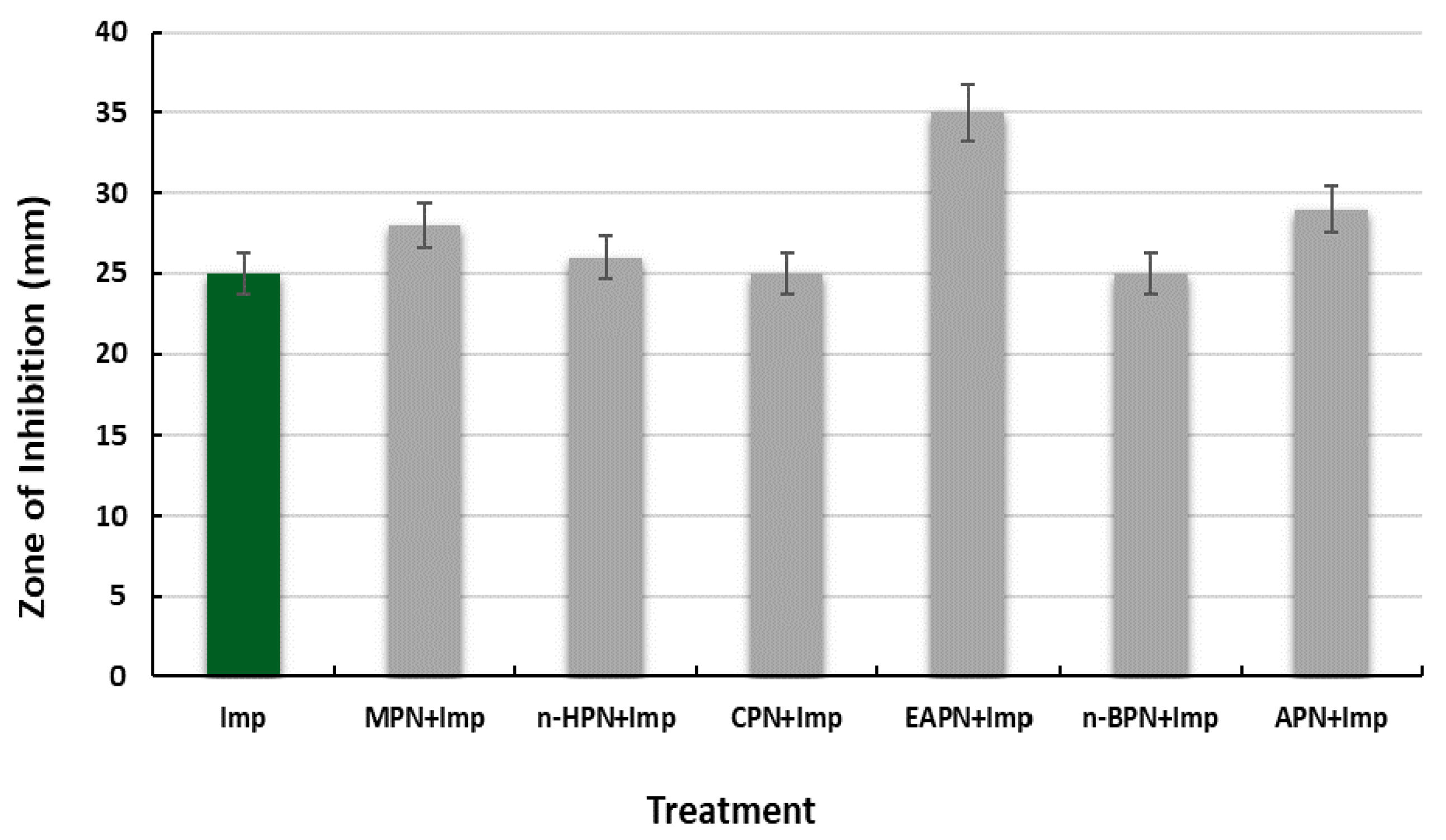
3.3.6. Imipenem
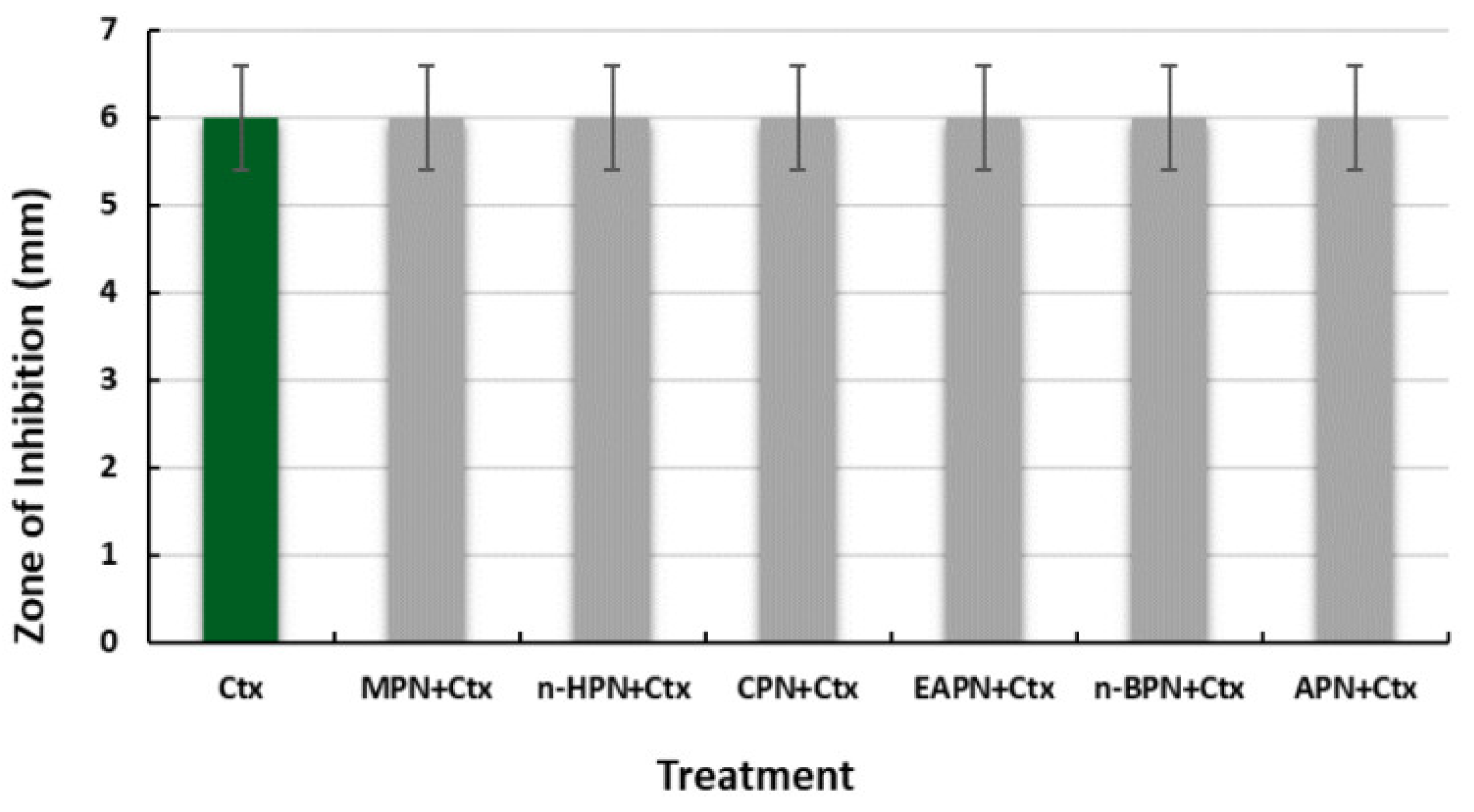
3.3.7. Cefotaxime
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Solanki, P.; Sultana, Y.; Singh, S. Traditional Medicine: Exploring Their Potential in Overcoming Multi-Drug Resistance. In Strategies to Overcome Superbug Invasions: Emerging Research and Opportunities; Chopra, D.S., Kaul, A., Eds.; IGI Global: Hershey, PA, USA, 2021; pp. 118–129. [Google Scholar] [CrossRef]
- Spengler, G.; Kincses, A.; Gajdács, M.; Amaral, L. New Roads Leading to Old Destinations: Efflux Pumps as Targets to Reverse Multidrug Resistance in Bacteria. Molecules 2017, 22, 468. [Google Scholar] [CrossRef] [Green Version]
- Piddock, L.J. Multidrug-resistance efflux pumps—Not just for resistance. Nat. Rev. Microbiol. 2006, 4, 629–636. [Google Scholar] [CrossRef]
- Baym, M.; Stone, L.K.; Kishony, R. Multidrug evolutionary strategies to reverse antibiotic resistance. Science 2016, 351, aad3292. [Google Scholar] [CrossRef] [Green Version]
- Su, T.; Qiu, Y.; Hua, X.; Ye, B.; Luo, H.; Liu, D.; Qu, P.; Qiu, Z. Novel Opportunity to Reverse Antibiotic Resistance: To Explore Traditional Chinese Medicine With Potential Activity against Antibiotics-Resistance Bacteria. Front. Microbiol. 2020, 11, 610070. [Google Scholar] [CrossRef]
- Levy, S.B.; Marshall, B. Antibacterial resistance worldwide: Causes, challenges and responses. Nat. Med. 2004, 10, S122–S129. [Google Scholar] [CrossRef]
- Asma, S.T.; Imre, K.; Morar, A.; Imre, M.; Acaroz, U.; Shah, S.R.A.; Hussain, S.Z.; Arslan-Acaroz, D.; Istanbullugil, F.R.; Madani, K.; et al. Natural strategies as potential weapons against bacterial biofilms. Life 2022, 12, 1618. [Google Scholar] [CrossRef]
- Venter, H. Reversing resistance to counter antimicrobial resistance in the World Health Organisation’s critical priority of most dangerous pathogens. Biosci. Rep. 2019, 29, BSR20180474. [Google Scholar] [CrossRef] [Green Version]
- Kumar, V.; Shriram, V.; Mulla, J. Antibiotic resistance reversal of multiple drug resistant bacteria using Piper longum fruit extract. J. Appl. Pharm. Sci. 2013, 3, 112–116. [Google Scholar] [CrossRef]
- Nitha, B.; Remashree, A.B.; Balachandran, I. Antibacterial activity of some selected indian medicinal plants. IJPSR 2012, 3, 2038–2042. [Google Scholar] [CrossRef]
- Raga, D.D.; Espiritu, R.A.; Shen, C.C.; Ragasa, C.Y. A bioactive sesquiterpene from Bixa orellana. J. Nat. Med. 2011, 65, 206–211. [Google Scholar] [CrossRef]
- Butler, M.; Buss, A.D. Natural products--the future scaffolds for novel antibiotics? Biochem Pharmacol. 2006, 71, 919–929. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; Kaushik, K. Medicinal, biological and pharmacological aspects of Plumbago zeylanica (Linn.). J. Pharmacogn. Phytochem. 2014, 3, 117–120. [Google Scholar]
- Sallam, K.I.; Abd-Elghany, S.M.; Imre, K.; Morar, A.; Herman, V.; Hussein, M.A.; Mahros, M.A. Ensuring safety and improving keeping quality of meatballs by addition of sesame oil and sesamol as natural antimicrobial and antioxidant agents. Food Microbiol. 2021, 99, 103834. [Google Scholar] [CrossRef] [PubMed]
- Stan (Tudora), C.; Cardei, P.; Muscalu, A.; Boiu-Sicuia, O.A.; Vladut, N.V.; Israel-Roming, F. Statistical analysis on the potential antifungal activity of some essential oils obtained from medicinal plants. AgroLife Sci. J. 2022, 11, 211–220. [Google Scholar]
- Shriram, V.; Jahagirdar, S.; Latha, C.; Kumar, V.; Dhakephalkar, P.; Rojatkar, S.; Shitole, M.G. Antibacterial & antiplasmid activities of Helicteres isora L. Indian J. Med. Res. 2010, 132, 94–99. [Google Scholar]
- Khder, A.K.; Muhammed, S.A. Potential of Aqueous and Alcohol Extracts of Quercus infectoria, Linusm usitatissium and Cinnamomum zeylanicium as Antimicrobials and Curing of Antibiotic Resistance in E. coli. Curr. Res. J. Biol. Sci. 2010, 2, 333–337. [Google Scholar]
- Reshmi, S.; Sathya, E.; Suganya Devi, P. Isolation of piperdine from Piper nigrum and its antiproliferative activity. J. Med. Plant Res. 2010, 4, 1535–1546. [Google Scholar] [CrossRef]
- Wang, D.; Zhang, L.; Huang, J.; Himabindu, K.; Tewari, D.; Horbańczuk, J.O.; Xu, S.; Chen, Z.; Atanasov, A.G. Cardiovascular protective effect of black pepper (Piper nigrum L.) and its major bioactive constituent piperine. Trends Food Sci. Technol. 2021, 117, 34–45. [Google Scholar] [CrossRef]
- Choudhury, R.P.; Choudhury, D.M.; Ningthoujam, S.S.; Das, D.; Nath, D.; Das Talukdar, A. Ethnomedicinal plants used by traditional healers of North Tripura district, Tripura, North East India. J. Ethnopharmacol. 2015, 26, 135–148. [Google Scholar] [CrossRef]
- Scott, I.; Jensen, H.; Philogène, B.J.R.; Arnason, J.T. A review of Piper spp. (Piperaceae) phytochemistry, insecticidal activity and mode of action. Phytochem. Rev. 2008, 7, 65–75. [Google Scholar] [CrossRef]
- Achenbach, H.; Fietz, W.; Worth, J. Constituents of tropical medicinal plants. IXX. GC/MS- investigations of the constituents of Piper amalago-30 new amides of the piperine-type. Planta Med. 1986, 52, 12–18. [Google Scholar] [CrossRef]
- Das, B.; Kashinatham, A.; Madhusudhan, P. One new and two rare alkamides from two samples of the fruits of Piper longum. Nat. Prod. Sci. 1998, 4, 23–25. [Google Scholar]
- Zhang, C.; Zhao, J.; Famous, E.; Pan, S.; Peng, X.; Tian, J. Antioxidant, hepatoprotective and antifungal activities of black pepper (Piper nigrum L.) essential oil. Food Chem. 2021, 346, 128845. [Google Scholar] [CrossRef] [PubMed]
- Qadri, H.; Shah, A.; Mudasir Ahmad, S.; Alshehri, B.; Almilaibary, A.; Ahmad Mir, M. Natural products and their semi-synthetic derivatives against antimicrobial-resistant human pathogenic bacteria and fungi. Saudi J. Biol. Sci. 2022, 29, 103376. [Google Scholar] [CrossRef]
- Ashokkumar, K.; Murugan, M.; Dhanya, M.K.; Pandian, A.; Warkentin, T.D. Phytochemistry and therapeutic potential of black pepper Piper nigrum (L.) essential oil and piperine: A review. Clin. Phytosci. 2021, 7, 52. [Google Scholar] [CrossRef]
- Mushtaq, A.; Anwar, R.; Ahmad, M. Lavandula stoechas (L) a very potent antioxidant attenuates dementia in scopolamine induced memory deficit mice. Front Pharmacol. 2018, 23, 1375. [Google Scholar] [CrossRef] [Green Version]
- Procop, W.; Church, D.L.; Hall, G.S.; Janda, W.M. Gram-Positive Cocci Part I: Staphylococci and Related Gram-Positive Cocci. In Color Atlas and Textbook of Diagnostic Microbiology, 7th ed.; Jones & Bartlett Publishers: Burlington, MA, USA, 2017; pp. 670–1105. [Google Scholar]
- Cusack, T.P.; Ashley, E.A.; Ling, C.L.; Rattanavong, S.; Roberts, T.; Turner, P.; Wangrangsimakul, T.; Dance, D.A.B. Impact of CLSI and EUCAST breakpoint discrepancies on reporting of antimicrobial susceptibility and AMR surveillance. Clin. Microbiol. Infect. 2019, 25, 910–911. [Google Scholar] [CrossRef] [Green Version]
- Humphries, R.M.; Hindler, J.A.; Shaffer, K.; Campeau, S.A. Evaluation of ciprofloxacin and levofloxacin disk diffusion and Etest using the 2019 Enterobacteriaceae CLSI breakpoints. J. Clin. Microbiol. 2019, 57, e01797-18. [Google Scholar] [CrossRef] [Green Version]
- Moore, D. Antibiotic Classification and Mechanism. 2015. Available online: http://www.orthobullets.com/basic-science/9059/antibioticclassification-and-mechanism (accessed on 31 July 2022).
- Nahak, G.; Sahu, R.K. Phytochemical evaluation and antioxidant activity of Piper cubeba and Piper nigrum. J. Appl. Pharm. Sci. 2011, 1, 153–157. [Google Scholar]
- Meghwal, M.; Goswami, T.K. Piper nigrum and piperine: An update. Phyther. Res. 2013, 27, 1121–1130. [Google Scholar] [CrossRef]
- Tegeos, G.; Stermitz, F.R.; Lomovskaya, O.; Lewis, K. Multidrug pump inhibitors uncover remarkable activity of plant antimicrobials. Antimicrob. Agents Chemother. 2002, 46, 3133–3141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reddy, S.V.; Srinivas, P.V.; Praveen, B.; Kishore, K.H.; Raju, B.C.; Murthy, U.S.; Rao, J.M. Antibacterial constituents from the berries of Piper nigrum. Phytomedicine 2004, 11, 697–700. [Google Scholar] [CrossRef] [PubMed]
- Lakhmi, V.V.; Padma, S.; Polasa, H. Elimination of multidrug-resistant plasmid in bacteria by plumbagin, a compound derived from a plant. Curr. Microbiol. 1987, 16, 159–161. [Google Scholar] [CrossRef]





| Antibiotics Tested (μg) | Zone of Inhibition for Test Strain (mm) | Zone of Inhibition According to CLSI (mm) [29,30] | ||
|---|---|---|---|---|
| Sensitive | Intermediate | Resistant | ||
| Cefoxitin (30) | 12 | ≥25 | - | ≤20 |
| Erythromycin (15) | 15 | ≥23 | 14–22 | ≤13 |
| Clindamycin (10) | 20 | ≥21 | 15–20 | ≤14 |
| Levofloxacin (5) | 14 | ≥19 | 16–18 | ≤15 |
| Ciprofloxacin (5) | 11 | ≥21 | 16–20 | ≤15 |
| Amikacin (30) | 14 | ≥17 | 13–14 | ≤12 |
| Gentamicin (10) | 15 | ≥15 | 13–14 | ≤12 |
| Antibiotics Tested (μg) | Zone of Inhibition for Test Strain (mm) | Zone of Inhibition According to CLSI (mm) [29,30] | ||
|---|---|---|---|---|
| Sensitive | Intermediate | Resistant | ||
| Ceftazidime (30) | 11 | ≥26 | 23–25 | ≤22 |
| Tigecycline (10) | 11 | ≥16 | - | ≤12 |
| Levofloxacin (5) | 15 | ≥19 | 14–16 | ≤13 |
| Ciprofloxacin (5) | 14 | ≥21 | 16–20 | ≤15 |
| Amikacin (30) | 17 | ≥17 | 13–14 | ≤12 |
| Gentamicin (10) | 16 | ≥15 | 13–14 | ≤12 |
| Imipenem (10) | 25 | ≥23 | 20–22 | ≤19 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Din, M.S.U.; Gohar, U.F.; Hameed, U.; Mukhtar, H.; Morar, A.; Herman, V.; Imre, K. Piper nigrum Fruit Extract as an Antibiotic Resistance Reversal Agent in MDR Bacteria. Appl. Sci. 2022, 12, 12542. https://doi.org/10.3390/app122412542
Din MSU, Gohar UF, Hameed U, Mukhtar H, Morar A, Herman V, Imre K. Piper nigrum Fruit Extract as an Antibiotic Resistance Reversal Agent in MDR Bacteria. Applied Sciences. 2022; 12(24):12542. https://doi.org/10.3390/app122412542
Chicago/Turabian StyleDin, Maryam Salah Ud, Umar Farooq Gohar, Uzma Hameed, Hamid Mukhtar, Adriana Morar, Viorel Herman, and Kálmán Imre. 2022. "Piper nigrum Fruit Extract as an Antibiotic Resistance Reversal Agent in MDR Bacteria" Applied Sciences 12, no. 24: 12542. https://doi.org/10.3390/app122412542
APA StyleDin, M. S. U., Gohar, U. F., Hameed, U., Mukhtar, H., Morar, A., Herman, V., & Imre, K. (2022). Piper nigrum Fruit Extract as an Antibiotic Resistance Reversal Agent in MDR Bacteria. Applied Sciences, 12(24), 12542. https://doi.org/10.3390/app122412542









