Assessment of Indigenous Plants Knowledge among Traditional Healers in Eastern Morocco: Quali-Quantitative Approach (Part I)
Abstract
1. Introduction
- -
- The fuqaha (singular: fqîh), tolba (singular: tâleb) or tobba (singular: tabîb), and the healers of all kinds (kuwway or cautery installer, hajjam or barber phlebotomist, jabbar or bonestter, mul ssnan or tooth puller, qabla or traditional birth attendant…)
- -
- The apothecaries who divide themselves into two very distinct guilds ‘aṭṭârin (singular: ‘aṭṭâr) and the ‘aššabin (singular: ‘aššab). ‘aṭṭârin represents what could be called the apothecary grocers, traders of spices, aromatics, and medicinal drugs expensive and imported from distant lands. The ‘aššabin are the herbalists proper or merchants of medicinal and aromatic plants whose range, more diverse, has a large number of medicinal and magical drugs (roots, dried plants, seeds, bark, minerals, animal products) or confections, crammed together with various ingredients used in magic.
2. Results and Discussions
2.1. Demographic Information of the THs and Professional Activity
2.1.1. Demographic Information of all Respondents
2.1.2. Description of the Professional Activity
2.1.3. The Nature of the Products Sold by the THs
2.1.4. Diagnosis of Diseases
2.1.5. Use of Traditional Medicine
2.1.6. Conservation and Transmission of Knowledge
2.2. Medicinal Plants of Eeastern Morocco, Use, Knowledge and Importance by THs
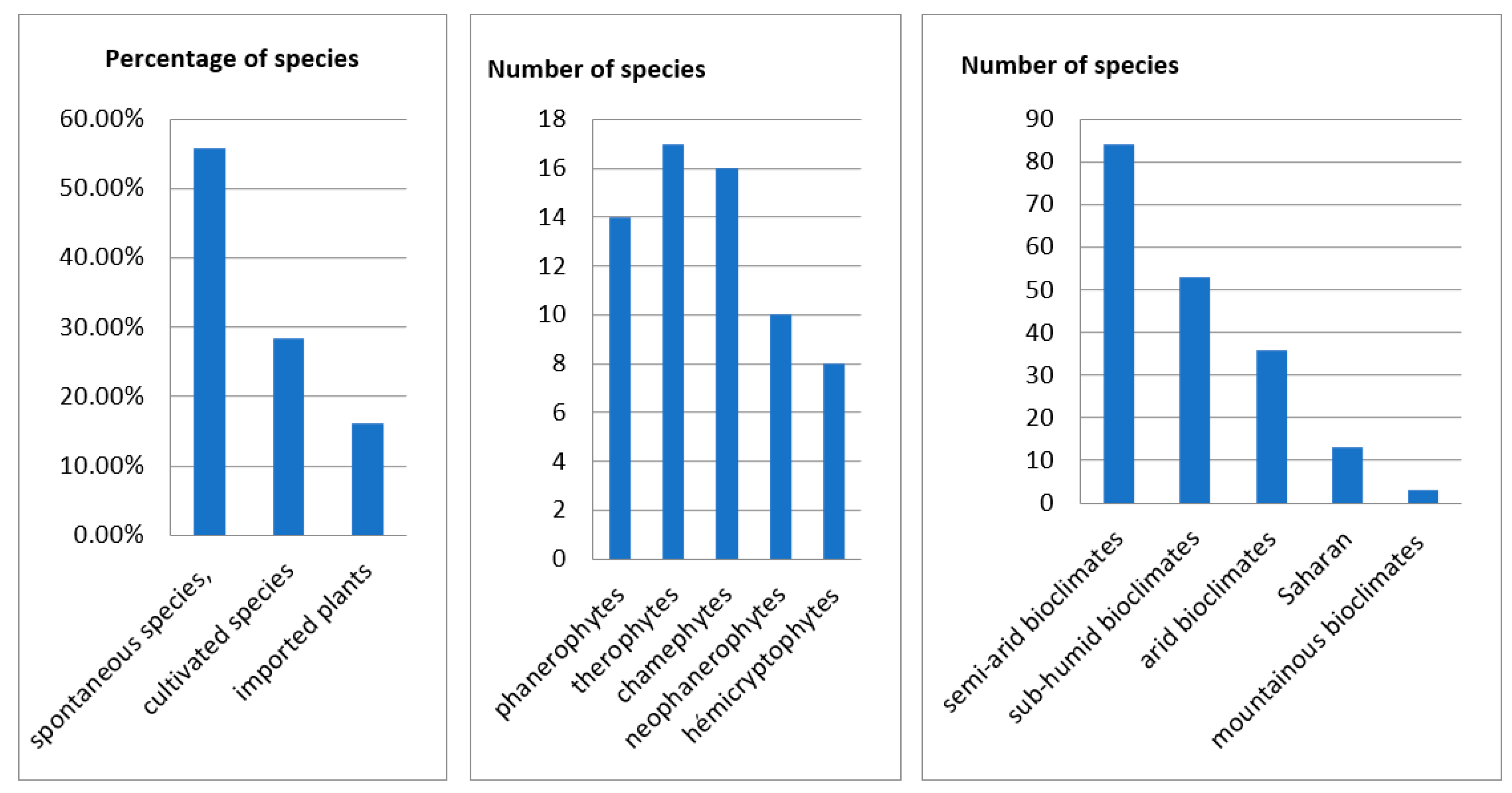
2.2.1. Cultural Wealth
2.2.2. Description of the Species
2.3. The Vernacular Names
2.4. Toxicity
2.5. Characteristics of Inventoried Recipes
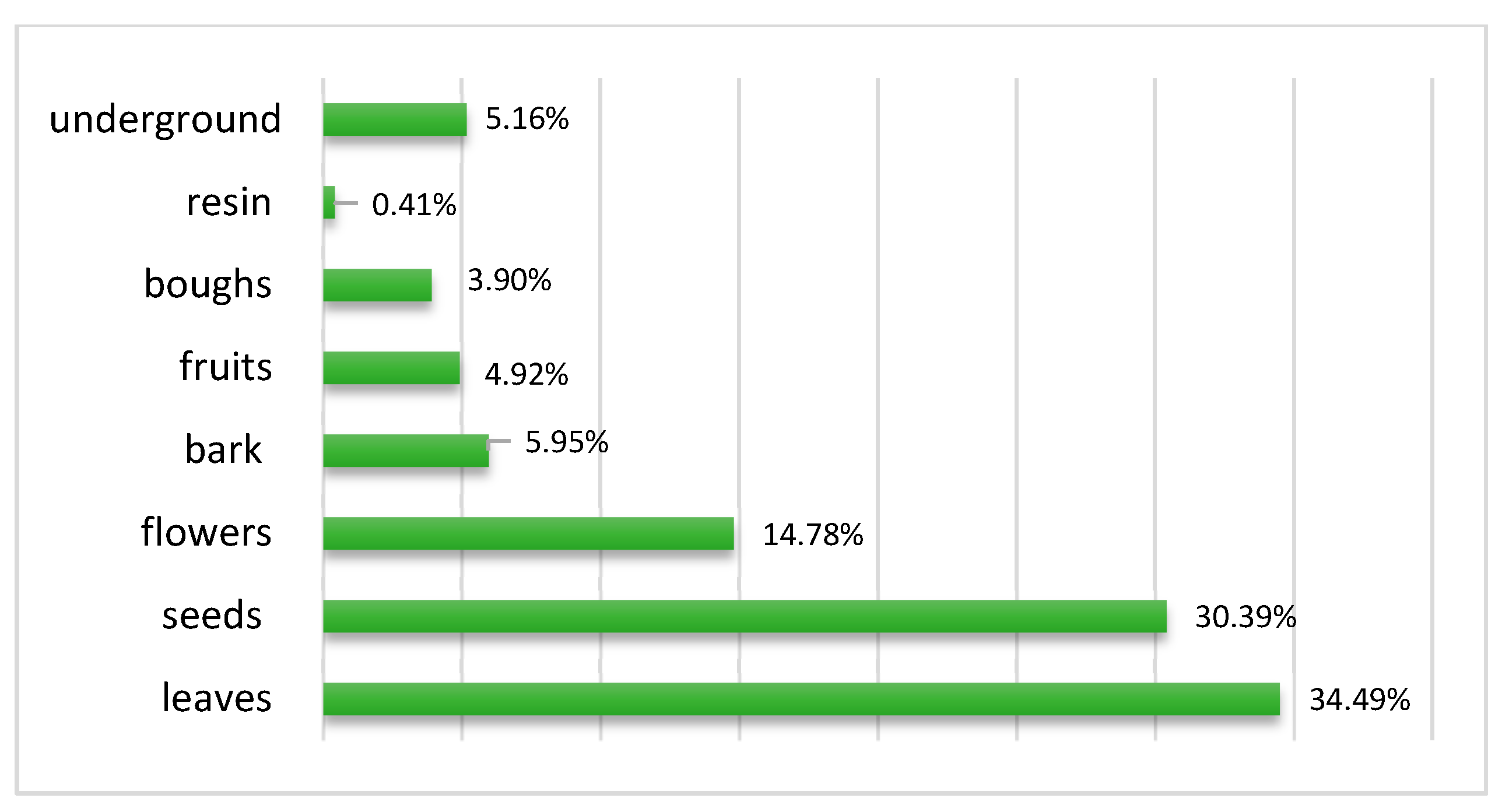
2.5.1. Parts of the Plants Used
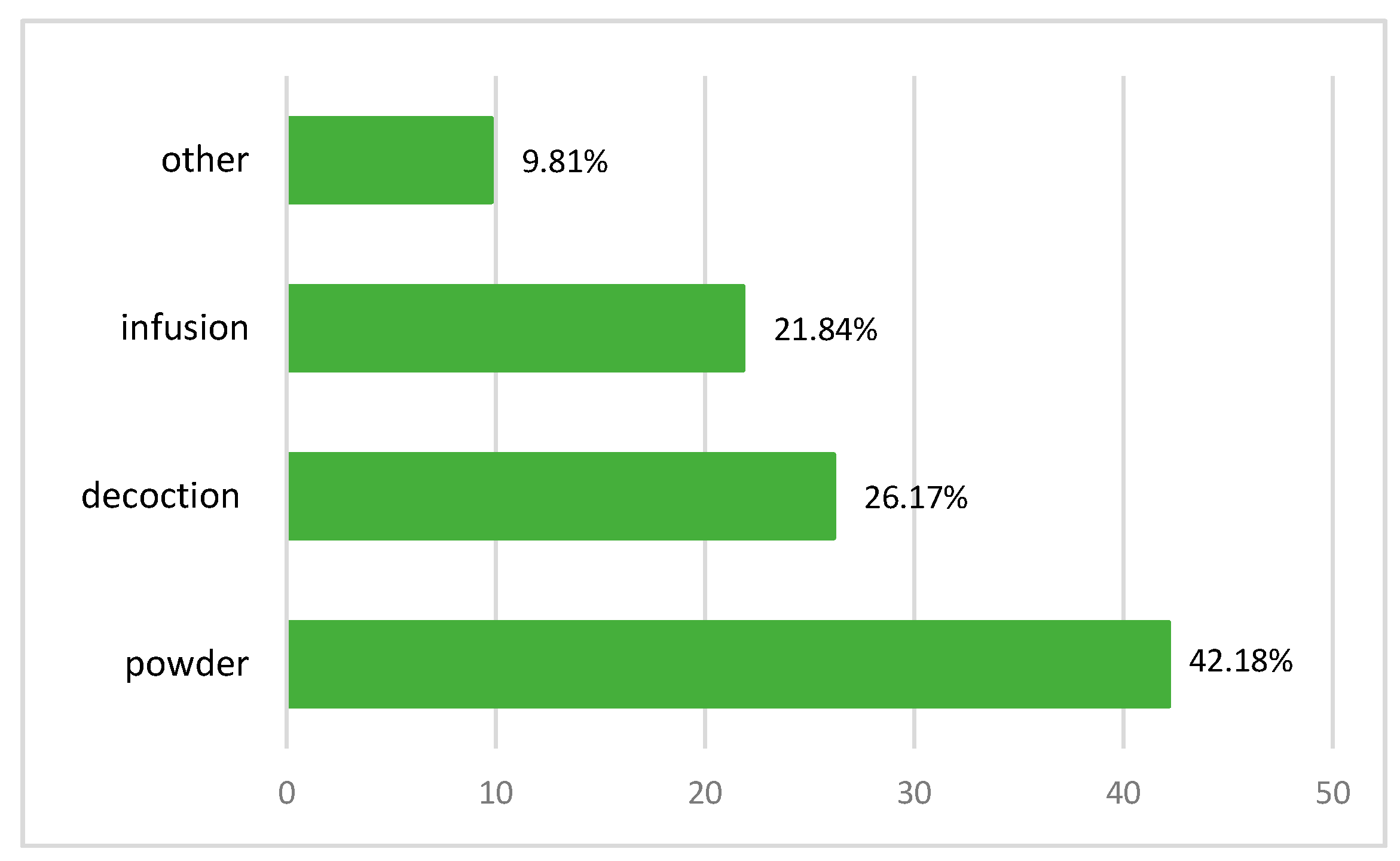
2.5.2. Recipe Preparation Techniques
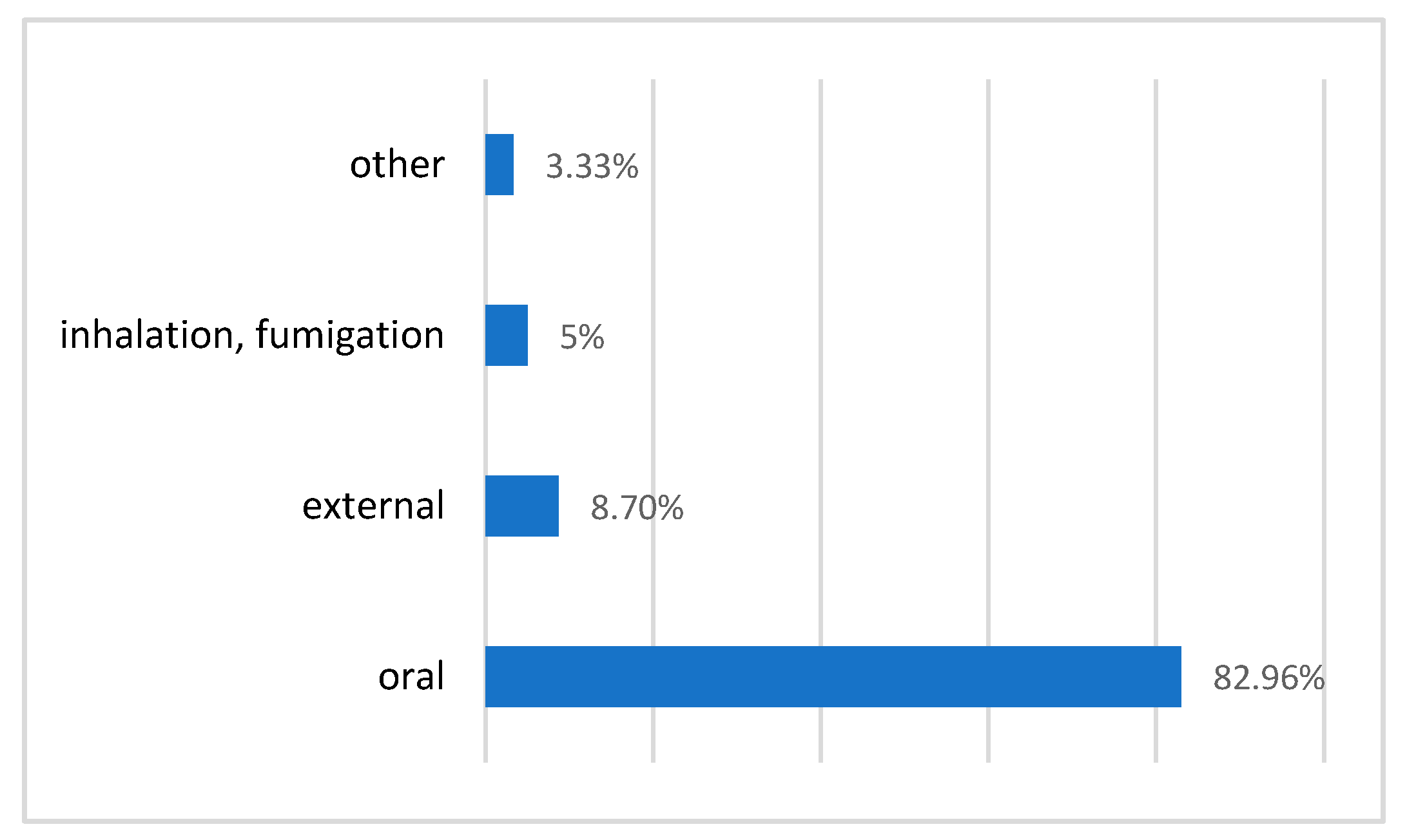
2.5.3. Routes for Administering Remedies
2.5.4. Association with Other Plants and/or Ingredients
2.5.5. The Duration of the Preparation
2.6. Diseases and Treatments
2.6.1. The Most Common Ailments
2.6.2. Diversity of Plants Used in the Treatment of diseases
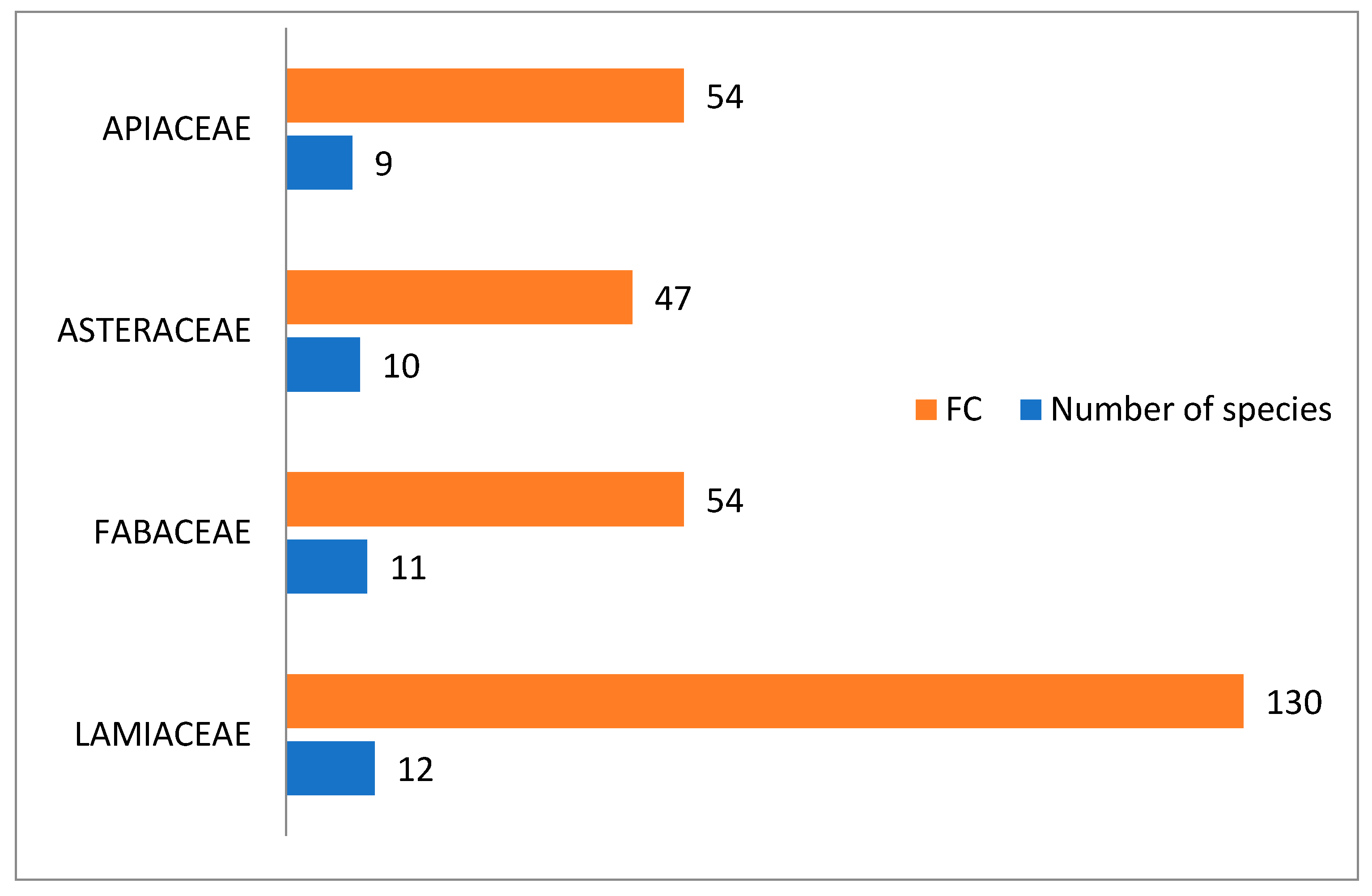
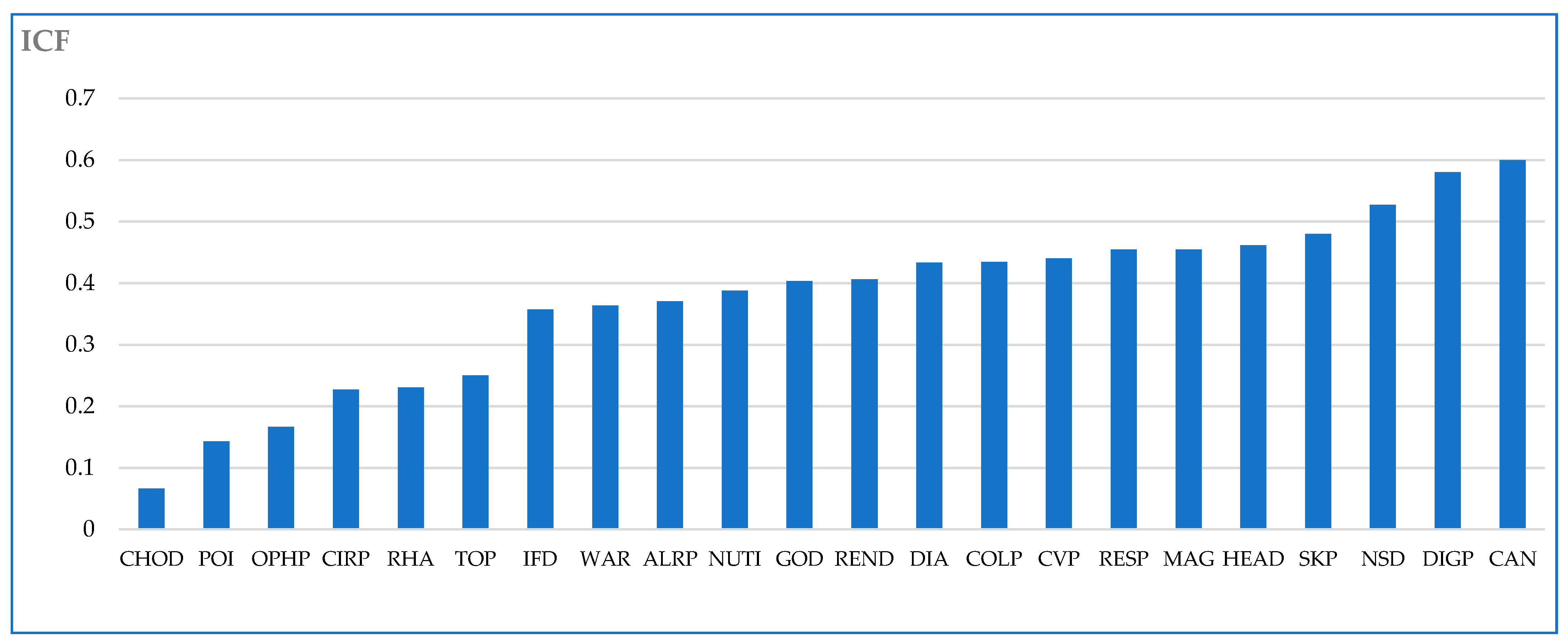
2.7. Informant Consensus Factor
2.8. The Most Important Species According to FC
3. Materials and Methods
3.1. Description of the Study Area
3.2. Ethnobotanical Survey
3.3. Floristic Identification and Taxonomic Validation
3.4. The Vernacular Names
3.5. Classification of Diseases
3.6. Data Analysis
3.6.1. Frequency Cited (FC)
3.6.2. Informant Consensus Factor for Each Ailment (ICF)
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Scientific Name | Biological Type | Ecology | Provenance | Bioclimatic Stages | Biogeographic Distribution | Toxicity in Literature [7,9] |
|---|---|---|---|---|---|---|
| Acacia gummifera Willd. | Ph | P E | plains and low mountains | A SAd | Ms AA HA Mam Man | |
| Aframomum melegueta (Roscoe) K. Schum. | I. | |||||
| Ajuga iva (L.) Schreb. | hem (TH) | P E | degraded forests and scrublands, uncultivated fields, rockeries, plains and mountains | A SAd SAf SH H | all of Morocco | is not toxic but in high doses causes cephalalgia |
| Allium sativum L. | C. | is not toxic but prolonged use on the skin can produce excoriations | ||||
| Aloysia citriodora Palau | C. | its prolonged use can cause gastric irritation | ||||
| Alpinia officinarum Hance) | I. | |||||
| Ammodaucus leucotrichus Coss. & Durieu | Th | p | desert sand, river gravel | S A | Ms AA? | is not toxic at low doses |
| Ammoides pusilla (Brot.) Breistr. | Th | P E | rocky and clayey slopes, plains and low mountains | A SAd SH | MA Mam Man Op Om LM R | is not toxic at low doses |
| Anabasis aretioides Coss. & Moq. ex Bunge | Ch | A | desert, steppes | S | Ms | at low doses, it is a little toxic |
| Anacyclus pyrethrum (L.) Link | Hém | P E | forest clearings, matorrals, pastures, (plains), low, middle and high mountain | Saf SH H HM | As AA HA MA Man Op Om R | toxic in high doses; it causes headache and sometimes even the loss of consciousness |
| Anastatica hierochuntica L. | Th | H P | steppes | S A | Ms As AA | |
| Apium graveolens L. | Th-b (Hém) | P E (A) | marshes and watersides of the plains, widely cultivated | A SAd SH | Ms Mam Man Op Om LM R | |
| Arbutus pavarii Pamp. | Ph (Nph) | A H | forests and matorrals, plains, low and middle Mountains | SAd SH H | AA HA MA Mam Man Om LM R | |
| Argania spinosa (L.) Skeels | Ph | P | plains and low mountains | S A SAd | Ms AA HA Mam LM | |
| Aristolochia fontanesii Boiss. & Reut. | G | P | fields, eras, matorrals, stony, clay or sandy soils, plains, low and medium. Mountains | SAd SH H | AA HA MA Mam Man Om LM R | Aristolochin causes renal irritation up to necrosis of the epitelial elements and paralisy of the limbs |
| Artemisia herba alba Asso | CH (Hém) | E A | steppes and rocky pastures | S A SAf | Ms AA HA MA Op Om LM R | toxic in high doses |
| Astracantha gummifera (Labill.) Podlech | ||||||
| Avena sativa L. | C. | is not toxic at low doses | ||||
| Berberis hispanica Boiss. & Reut. | Nph (Ph) | P E | forests and matorrals, cracks in mountain rocks | Saf SH H | As (rare) HA MA R | |
| Beta vulgaris L. | Th, Hém | P | maritime rocks, rubble, meadows, wasteland, plains, low and mid. Mountains | A SAd SH | all of Morocco except the Saharan regions | |
| Boswellia sacra Flueck. | I. | is not toxic at low doses | ||||
| Calamintha nepeta (L.) Savi | Ch | H P E | forests and matorrals, stony erms, rocks, plains and low mountains | SAd SH H | HA HM Man Om LM R | |
| Calendula arvensis (Vaill.) L. | Th | H P E | all of Morocco | |||
| Camellia sinensis (L.) Kuntze | I., C. | is not toxic | ||||
| Cannabis sativa L. | C. | very toxic; it causes anaphrodisia | ||||
| Capparis spinosa L. | Ch (Nph) | (H) P E | rocks, walls, rocky and clay slopes, plains and low mountains | S A Sad SH | spontaneous in Morocco | several substances which have been shown to be toxic |
| Capsicum annuum L. | C. | |||||
| Carlina gummifera (L.) Less. | Hém (G) | E A | Open matorrals, hermes, wasteland, plains and low mountains | A SAD SH | HA MA Mam Man Om LM R | roots are very toxic; the heat destroys its toxic power |
| Carum carvi L. | C. | is not toxic at low doses | ||||
| Cassia senna L. var. senna | I. | |||||
| Ceratonia siliqua L. | Ph | A H | plains and low mountains | SAD (SAF) SH | As AA HA MA Mam Man Op? Om LM R | fruit is not toxic |
| Chenopodium ambrosioides L. | Th | P E A | Naturalized in fresh uncultivated environments, ditches, hedges, sandy alluvium | A SAD SH | Ms HA Mam Man Op LM R | |
| Cinnamomum cassia (L.) J.Presl | I. | |||||
| Cistus populifolius L. | Nph | P | low mountain and plains matorrals | SH H | R | |
| Citrullus colocynthis (L.) Schrad. | G | E | S A SAd | Ms As AA Mam Man Op LM R | most of the time, toxic accidents occur during attempted abortions | |
| Citrus limon (L.) Burm. f. | ||||||
| Citrus salicifolia Raf. | ||||||
| Coriandrum sativum L. | C. | |||||
| Corrigiola telephiifolia Pourr. | Hém | P E | Stony and sandy land, plains and mountains | SAD SAF SH | AA HA MA Mam Man R | |
| Costus (ND) | ||||||
| Crataegums monogyna Jacq. | Nph (Ph) | H P | low and middle Mountains | SAd SAf SH H | all of Morocco except Ms et As | |
| Crocus sativus L. | C. | is not toxic at low doses | ||||
| Cuminum cyminum L. | C. | |||||
| Curcuma longa L. | I. | |||||
| Cydonia oblonga Mill. | C. | |||||
| Cynara cardunculus L. | G | P E | pastures and wasteland, especially in clay soils, plains and low mountains | A SAd SH | MA Mam Man Op Om LM R | |
| Daphne gnidium L. | CH | P | forests, matorrals, fields, eras, plains, low and mid. Mountains | SAd SH | all of Morocco except Ms. | berries are very poisonous |
| Datura stramonium L. | Th | P E A | crops, rubble and open areas, nitrophilic | S A SAd SH | all of Morocco | plant is very poisonous |
| Delphinium staphisagria L. | Hém | P | forests and cool matorals, plains and low mountains | SH H | western rif | in high doses it causes fatal poisoning |
| Dittrichia viscosa (L.) Greuter | Ch (Nph) | E A | open environments on sufficiently humid clay substrates, waterfronts, plains and low mountains | A SAd Saf SH H | no Saharan Morocco | is not toxic at low doses |
| Elettaria cardamomum (L.) Maton | I. | |||||
| Eruca vesicaria (L.) Cav. | Th | P € | SAd (SAF) | Mam Op? LM | ||
| Eucalyptus torquata Luehm. | I. | is not toxic at low doses | ||||
| Euphorbia falcata L. | Th | P E | eras, crops, fallows, plains, low (and middle) mountains | A SAd Saf SH H | all of Morocco except the Ms | the plants for internal use, causes gastroenteritis more or less severe |
| Euphorbia resinifera O. Berg | Nph (-s) | E | limestone bedrock, low and middle Mountains | A SAd SAf | AA HA MA Mam | in high doses the plant causes hematuria and death by asphyxiation. the plant and its fresh or dry latex are dangerous products |
| Ferula communis L. | G | P E | plains, low and middle Mountains | A SAD SAF SH H | all of Morocco | very toxic |
| Foeniculum vulgare Mill. | Ch (Hém; Tb-b) | P E | uncultivated fields, arid hillsides, ravines, rocks, plains and low mountains | A SAd SAf SH H | all of Morocco except the Ms | oil is very toxic |
| Fraxinus angustifolia Vahl | Ph | H P | low and middle Mountains | SAD SAF SH H | HA MA Mam Man Om LM R | is not toxic |
| Globularia alypum L. | Ch | P | forests and matorals, plains and low mountains | A SAD SAF SH (H) | all of Morocco | is not toxic; a high dose causes headache and a lowering of temperatur |
| Glycine max (L.) Merr. | is not toxic at low doses | |||||
| Glycyrrhiza glabra L. | C. | is not toxic at low doses | ||||
| Helianthus annuus L. | C. | |||||
| Herniaria hirsuta L. | Th | (H) P E | sandy fields, places uncultivated arid | SAd SH | Mam Man LM R | |
| Hibiscus sabdariffa L. | I. | |||||
| Hordeum vulgare L. | C. | is not toxic | ||||
| Hyoscyamus albus L. | Th | P E | rubble, crops, old walls | A SAD SAF SH H | AA HA MA Mam Man Op Om LM R | toxic in high dose |
| Hyoscyamus niger L. | Th | P E | crops, rubble, plains, low and middle Mountains | SAD SH H | HA MA Man LM? R | toxic in high dose |
| Illicium verum Hook.f. | ||||||
| Juglans regia L. | C. | is not toxic at low doses | ||||
| Juncus acutus L. | Hém (GR) | P E | hygrophilic and halophilic, sands and salty mud, edges of rivers and dayas, plains, low (and mid) mountains | S A SAD SAF SH H | Ms HA Mam Man Op LM R | is not toxic at low doses |
| Lagenaria siceraria (Molina) Standl. | C. | |||||
| Laurus nobilis L. | Ph | (H) P | ravines and rocks of forests and Matorrals, plains, and mountains up to 1800 m | SH H | MA R | |
| Lavandula dentata L. | CH Nph | P A | plains and low mountains | SAd SH | AA HA MA Mam Man LM OM R | |
| Lawsonia inermis L. | C. | is not toxic at low doses | ||||
| Lepidium sativum L. | C. | is not toxic | ||||
| Linum usitatissimum L. | Th | P E | Man Man LM R | seeds containing linamarin which on hydrolysis gives cyaanhydriden acid. A high dose is toxic | ||
| Lupinus albus L. | C. | |||||
| Malus pumila Mill. | C. | |||||
| Mandragora officinarum L. | G | P E | Matorrals, ermes, uneducated places, fields | SAd SH | Mam Man LM R | several accidents and even deaths have been reported |
| Matricaria chamomilla L. | Th | H P € | Harvests, fields, uncultivated, gardens | SAd SH | Man LM R | |
| Mentha pulegium L. | Hém | P E | humid places, plains, low mountains | SAd SH H | no saharien Morocco | is not toxic in high doses, it causes loss of consciousness and cardiac disorder |
| Mentha spicata L. | C. | is not toxic | ||||
| Myristica afragrans Houtt. | I. | toxic in medium doses | ||||
| Myrtus communis L. | Nph | P | plains, and low mountains | SAd SH | Man OM LM R | not very toxic but its essence can cause headache |
| Nerium oleander L. | Nph | P E | edges of wadis | S A Sad Saf SH H | all Morocco | very toxic |
| Nigella sativa L. | C. | high dose toxic | ||||
| Ocimum basilicum L. | C. | is not toxic at low doses | ||||
| Olea europaea L. | Ph | P | plains, and low mountains | A SAd SAf SH H | no saharien Morocco | is not toxic at low doses |
| Opuntia ficus-indica (L.) Mill. | Nph | P E | plains, low and middle Mountains | A Sad SH | HA MA Mam Man Om LM R | is not toxic, ingestion of a large number of fruits causes stubborn constipation and sometimes dangerous |
| Origanum compactum Benth. | Ch | E | forests, matorrals, fields, erms, rocks, plains and low mountains | A SAd SH | MA Mam Man R | Essence of origon in high doses causes paralysis pressured by excitations |
| Origanum majorana L. | C. | in high doses gasoline is stupefying and toxic for humans | ||||
| Panax ginseng C.A.Mey. | I. | |||||
| Papaver rhoeas L. | Th | P E | fields, harvests, wasteland, plains, low and middle mountains | A SAd SAf SH H | all of Morocco | |
| Papaver somniferum L. | Th | (H) P E | fields, uncultivated places, plains, low and mid. Mountains | S A SAD SAF SH | all of Morocco | |
| Peganum harmala L. | CH | P E | steps, uncultivated fields, rubble, plains and low mountains | S A SAd | all of Morocco | is not toxic at low doses |
| Phillyrea angustifolia L. | Ph | H P | clear forests and Matorals, plains, low and middle Mountains | SAd SH H | As? HA MA Man R | |
| Phoenix dactylifera L. | C. | P | Saharan and arid streams and oases | S A | Ms As AA HA Mam | is not toxic |
| Pimpinella anisum L. | C. | in high doses, it causes stupidity and convulsions | ||||
| Piper cubeba L. f. | I. | |||||
| Piper longum L. | I. | |||||
| Piper nigrum L. | I. | is not toxic at low doses | ||||
| Pistacia atlantica Desf. | Ph | P E | lains, low and middle mountains | A SAd SAf SH | all of Morocco | In low doses, the fruit is not toxic |
| Pistacia Ientiscus L. | Ph | P | plaines, basses (et moy.) montagnes | SAD SH H | As AA HA MA Mam Man Om LM R | is not toxic at low doses |
| Prunus dulcis (Mill.) D. A. Webb | Ph | H P | orests and rocks | SAd SH H | MA Mam Om R | |
| Punica granatum L. | C. | high dose bark is very toxic | ||||
| Quercus faginea Lam. | Ph | h | N.Afr. | |||
| Quercus suber L. | Ph | P E | plains, low and middle mountains | SH H | HA MA Man R | |
| Ricinus communis L. | seeds is very toxic | |||||
| Rosa centifolia L. | C. | |||||
| Rosmarinus officinalis L. | contains a toxic gasoline in high dose, it causes tomacal hemorrhage, albuminuria and steatosis of the liver | |||||
| Rubia peregrina L. | Ch (G) | P E | forests and matorals, low and middle plains Mountains | A SAd SAf SH H | HA MA Mam Man Om LM R | is not toxic at low dose |
| Ruta chalepensis L. | Ch | P E | clear forests, dry uncultivated hillsides, rocks, plains, low and middle mountains | A SAd SAf SH | HA? Mam Man Om R | is not toxic at low doses |
| Salvia officinalis L. | C. | |||||
| Sesamum indicum L. | C. | |||||
| Sorghum bicolor (L.) Moench | C. | |||||
| Syzygium aromaticum (L.) Merr. & L. M. Perry(3) | I. | I. | ||||
| Tamarindus indica L. | I. | |||||
| Telephium imperati L. | hém (ch) | P E | rocky erms and mountain rocks | SAf SH HM | As AA HA MA Man Op Om R | |
| Terminalia chebula Retz. | ||||||
| Tetraclinis articulata (Vahl) Mast. | Ph | E | plains, low (and middle) mountains | SAd (SH) | AA HA MA Mam Man Op Om LM R | is not toxic at low doses |
| Tetraena gaetula (Emb. & Maire) Beier & Thulin | Ch | P E | epandage argileux salés | Ms oriental | ||
| Thymelaea hirsuta (L.) Endl. | Nph | H P | steps, forest glades, rockeries | A SAd SAf SH | As AA occidental HA MA Mam Op Om LM? R? | |
| Thymus broussonetii Boiss. | Ch | P | clear forests and Matorrals, plains and low mountains | A SAd | HA Mam Man | |
| Tilia sylvestris Desf. | I. | |||||
| Trigonella foenum-graecum L. | C. | |||||
| Urtica dioïca L. | GR | P E | wet cultivated places, fresh ravines | A | Mam | a decoction administered internally may cause eczema and urine retention |
| Valeriana celtica L. | G | E | limestone and sand-limestone rocks, high mountains | SAf SH HM | MA north eastern | |
| Vicia faba L. | C. | |||||
| Viscum album L. | Ch (-p) | P E | wet forests | H | ||
| Vitis vinifera L. | C. | |||||
| Warionia saharae Benth. & Coss. | Nph | P E | substrate rocky, plains, low mountains | S A SAd | Ms As AA HA Mam | |
| Zea mays L. | C. | is not toxic at low doses | ||||
| Zingiber officinale Roscoe | I. | I. | is not toxic; in high doses it can cause amnesia | |||
| Ziziphus lotus (L.) Lam. | (Ph) Nph | P E | not forest areas, plains, low (and middle) mountains | S A SAd SAf SH | all of Morocco | fruit is not toxic in low doses |
References
- Elachouri, M.; Kharchoufa, L.; Fakchich, J.; Lorigooini, Z. Ancestral phytotherapeutic practices in Morocco: Regards on history, current state, regulatory and safety of commonly used herbal medicine. Arab. J. Chem. Environ. Res. 2021, 8, 133–149. [Google Scholar]
- Renaud, H.-C. Tuhfat Al-Ahbāb Glossaire de la Matière Médicale; Marocaine: Paris, France, 1934. [Google Scholar]
- Bellakhdar, J. La pharmacopée marocaine traditionnelle. In Médecine arabe Ancienne et Savoirs Populaires; Ibis Press: Paris, French, 1997. [Google Scholar]
- Claisse-Dauchy, R.; de Foucault, B. Médecine arabo-musulmane: Modes de transmission des savoirs au Maroc (régions de Meknès et Rabat-Salé). Des. Sources Du Savoir Aux Médicaments Du Futur. 2016, 321–326. [Google Scholar] [CrossRef]
- Bammou, M.; Daoudi, A.; Sellam, K.; El Rhaffari, L.; Ibijbijen, J.; Nassiri, L. Étude Ethnobotanique des Astéracées dans la Région Meknès-Tafilalet (Maroc)/[Ethnobotanical Survey of Asteraceae Family used in Meknes-Tafilalet Region (Morocco)]. Int. J. Innov. Appl. Stud. 2015, 13, 789–815. [Google Scholar]
- Addo-Fordjour, P.; Anning, A.K.; Atakora, E.A.; Agyei, P.S. Diversity and distribution of climbing plants in a semi-deciduous rain forest, KNUST Botanic Garden, Ghana. Int. J. Bot. 2008, 4, 186–195. [Google Scholar] [CrossRef]
- Benítez, G.; González-Tejero, M.R.; Molero-Mesa, J. Pharmaceutical ethnobotany in the western part of Granada province (southern Spain): Ethnopharmacological synthesis. J. Ethnopharmacol. 2010, 129, 87–105. [Google Scholar] [CrossRef]
- El Rhaffari, L.; Zaid, A. Pratique de la phytothérapie dans le sud-est du Maroc (Tafilalet). Un savoir empirique pour une pharmacopée rénovée. Des Sources Du Savoir Aux Médicaments Du Futur. 2001, 293–318. [Google Scholar] [CrossRef]
- Abouri, M.; El Mousadik, A.; Msanda, F.; Boubaker, H.; Saadi, B.; Khalil, C. An ethnobotanical survey of medicinal plants used in Terai forest of western Nepal. J. Ethnobiol. Ethnomed. 2012, 8, 99–123. [Google Scholar] [CrossRef]
- Saadi, B.; Msanda, F.; Boubaker, H. Contributions of folk medicine knowledge in South- western Morocco: The case of rural communities of Imouzzer Ida Outanane Region. Int. J. Med. Plant. Res. 2013, 2, 135–145. [Google Scholar]
- El-Hilaly, J.; Hmammouchi, M.; Lyoussi, B. Ethnobotanical studies and economic evaluation of medicinal plants in Taounate province (Northern Morocco). J. Ethnopharmacol. 2002, 86, 149–158. [Google Scholar] [CrossRef]
- Oualidi, J.E.L.; Khamar, H.; Fennane, M. Checklist des Endémiques et Spécimens Types de la Flore Vasculaire de l’Afrique du Nord. Doc. De L’Institut Sci. 2012, 25, 1–189. [Google Scholar]
- Fennane, M.; Ejdali, M. Aromatic and medicinal plants of Morocco: Richness, diversity and threats Plantes aromatiques et médicinales du Maroc: Richesse, diversité et menaces. Bull. L’institut Sci. Rabat. Sect. Sci. La Vie 2016, 38, 27–42. [Google Scholar] [CrossRef]
- Fakchich, J.; Elachouri, M. An overview on ethnobotanico-pharmacological studies carried out in Morocco, from 1991 to 2015: Systematic review (part 1). J. Ethnopharmacol. 2021, 267, 113200. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, A.; Jamila, F.; Mostafa, E. First insight on ethnobotanical appraisal of plants used traditionally as medicine by berber community (Amazigh-speaking), living in driouch province (north-eastern morocco). Ethnobot. Res. Appl. 2021, 22, 1–71. [Google Scholar] [CrossRef]
- Ziyyat, A.; Legssyer, A.; Mekhfi, H.; Dassouli, A.; Serhrouchni, M.; Benjelloun, W. Phytotherapy of hypertension and diabetes in oriental Morocco. J. Ethnopharmacol. 1997, 58, 45–54. [Google Scholar] [CrossRef]
- Lahsissene, H.; Aahouadi, K.; Tijane, M.; Hseini, S. Catalogue Des Plantes Medicinales Utilisées Dans La Région De Zaër (Maroc Occidental). Lejeunia. Rev. Bot. 2009, 186, 1–26. [Google Scholar]
- Bencheikh, N.; Elbouzidi, A.; Kharchoufa, L.; Ouassou, H.; Merrouni, I.A.; Mechchate, H.; Es-Safi, I.; Hano, C.; Addi, M.; Bouhrim, M.; et al. Inventory of medicinal plants used traditionally to manage kidney diseases in north-eastern Morocc: Ethnobotanical fieldwork and pharmacological evidence. Plants 2021, 10, 1966. [Google Scholar] [CrossRef]
- Ilyass, A.M.; Loubna, K.; Noureddine, B.; Mostafa, E. Ethnobotanical profile of medicinal plants used by people of North-eastern Morocco: Cross-cultural and historical approach (part I). Ethnobot. Res. Appl. 2021, 21, 1–45. [Google Scholar] [CrossRef]
- Charnot, A. La Toxicologie au Maroc, Mémoire de la Société des Sciences Naturelles du Maroc; Emile Larose: Paris, French, 1945; pp. 572–598. [Google Scholar]
- Bruneton, J. Plantes Toxiques: Vegetaux Dangereux Pour L’homme et Les Animaux; Tec: Paris, French, 1996. [Google Scholar]
- Kharchoufa, L.; Bouhrim, M.; Bencheikh, N.; Addi, M.; Hano, C.; Mechchate, H.; Elachouri, M. Potential toxicity of medicinal plants inventoried in northeastern Morocco: An ethnobotanical approach. Plants 2021, 10, 1108. [Google Scholar] [CrossRef]
- Benlamdini, N.; Elhafian, M.; Rochdi, A.; Zidane, L. Étude floristique et ethnobotanique de la flore médicinale du Haut Atlas oriental (Haute Moulouya). J. Appl. Biosci. 2014, 78, 6771. [Google Scholar] [CrossRef]
- Salhi, S.; Fadli, M.; Zidane, L.; Douira, A. Etudes floristique et ethnobotanique des plantes médicinales de la ville de Kénitra (Maroc) Souad. Mediterr. Bot. 2010, 31, 133–146. [Google Scholar] [CrossRef]
- Ghourri, M.; Zidane, L.; Houda, E.Y.; Rochdi, A.; Fadli, M.; Douira, A. Etude floristique et ethnobotanique des plantes médicinales de la ville d’El Ouatia (Maroc saharien). Kastamonu Univ. J. For. Fac. 2012, 12, 218–235. [Google Scholar] [CrossRef]
- Bouayyadi, L.; El Hafian, M.; Zidane, L. Étude floristique et ethnobotanique de la flore médicinale dans la région du Gharb, Maroc. J. Appl. Biosci. 2015, 93, 8770. [Google Scholar] [CrossRef]
- El Yahyaoui, O.; Ouaaziz, N.A.; Sammama, A.; Kerrouri, S.; Bouabid, B.; Lrhorfi, L.A.; Zidane, L.; Bengueddour, R. Etude ethnobotanique: Plantes médicinales commercialisées à la province de Laâyoune; identification et utilisation [Ethnobotanical Study: Medicinal plants commercialized in the province of Laayoune; identification and use]. Int. J. Innov. Appl. Stud. 2015, 12, 533. [Google Scholar]
- Zerkani, H.; Tagnaout, I.; Zair, T.; Meknes, Z. Ethnobotanical survey and inventory of medicinal flora in the rural municipalities of Ait Ishaq, Tighassaline, El-Hammam and Ageulmam azegza—Khenifra province, Morocco. J. Chem. Pharm. Res. 2015, 7, 611–627. [Google Scholar] [CrossRef]
- Poffenberger, M.; Singh, S. Forest management partnerships: Regenerating India’s forests. Unasylva 1992, 43, 46. [Google Scholar]
- Bitsindou, M. Enquête sur la Phytothérapie Traditionnelle à Kindamba et Odzala (Congo) et Analyse de Convergence D’usage des Plantes Médicinale en Afrique Centrale Mem; Doc Ined.; Université Libre de Bruxelles: Brussels, Belgium, 1986. [Google Scholar]
- Bigendako-Polygenis, M.J.; Lejoly, J. La pharmacopée traditionnelle au Burundi. Pesticides et médicaments en santé animale. Pres. Univ. Namur. 1990, 45, 425–442. [Google Scholar]
- Didi, O.E.H.M.; Hadj-Mahammed, M.; Zabeirou, H. Place Des Plantes Spontanees Dans La Medecine Traditionnelle De La Region De OUARGLA (Sahara Septentrional Est). Courr. Du Savoir 2003, 3, 47–51. [Google Scholar]
- Yapi, A. Inventaire des Plantes Médicinales de la Famille des Asteraceae des Marchés de la Commune d’Abobo (Abidjan, Côte d’Ivoire); Université Félix Houphouët-Boigny: Abidjan, Côte d’Ivoire, 2013. [Google Scholar]
- Jaiswal, Y.; Liang, Z.; Zhao, Z. Botanical Drugs in Ayurveda and Traditional Chinese Medicine; Elsevier: Amsterdam, The Netherlands, 2016; Volume 194, ISBN 1700018000. [Google Scholar]
- Ghourri, M.; Zidane, L.; Douira, A. Usage des plantes médicinales dans le traitement du Diabète Au Sahara marocain (Tan-Tan). Japs 2013, 17, 2388–2411. [Google Scholar]
- Messaoudi, M.; Filali, H.; Tazi, A.; Hakkou, F. Ethnobotannical surveys of healing medicinal plants traditionally used in the main Moroccan citiees. J. Pharmacogn. Phyther. Full 2015, 7, 164–182. [Google Scholar]
- Rhaffari, L.; Hammani, K.; Benlyas, M.; Zaid, A. Traitement de la leishmaniose cutanée par la phytothérapie au Tafilalet. Biol. Santé 2002, 1, 45–54. [Google Scholar]
- Benkhnigue, O.; Zidane, L.; Fadli, M.; Elyacoubi, H.; Rochdi, A.; Douira, A. Etude ethnobotanique des plantes médicinales dans la région de Mechraâ Bel Ksiri (Région du Gharb du Maroc). Acta Botánica Barcinonensia 2011, 53, 191–216. [Google Scholar]
- Zhao, Z.; Liang, Z.; Chan, K.; Lu, G.; Lee, E.L.M.; Chen, H.; Li, L. A unique issue in the standardization of Chinese materia medica: Processing. Planta Med. 2010, 76, 1975–1986. [Google Scholar] [CrossRef] [PubMed]
- Ouhaddou, H.; Boubaker, H.; Msanda, F.; El Mousadik, A. An ethnobotanical study of medicinal plants of the Agadir Ida Ou Tanane province (southwest Morocco). J. Appl. Biosci. 2015, 84, 7707. [Google Scholar] [CrossRef]
- El–Said, F.; Sofowora, E.A.; Malcolm, S.A.; Hofer, A. An investigation into the efficacy of Ocimum gratissimum as used in Nigerian native medicine. Planta Med. 1969, 17, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Fleurentin, J.; Pelt, J.M. Las plantas medicinales. Mundo Científico 1990, 105, 926–934. [Google Scholar]
- Bussmann, R.W.; Sharon, D. Traditional medicinal plant use in Northern Peru: Tracking two thousand years of healing culture. J. Ethnobiol. Ethnomedicine 2006, 2, 47. [Google Scholar] [CrossRef] [PubMed]
- Fakchich, J.; Elachouri, M. Ethnobotanical survey of medicinal plants used by people in Oriental Morocco to manage various ailments. J. Ethnopharmacol. 2014, 154, 76–87. [Google Scholar] [CrossRef]
- Briguiche, H.; Rochdi, A.; Zidane, L. The catalogue of medicinal plants used in the region of El Jadida. Int. J. Herb. Med. 2015, 2, 46–54. [Google Scholar]
- El Hafian, M.; Benlandini, N.; Elyacoubi, H.; Zidane, L.; Rochdi, A. Étude floristique et ethnobotanique des plantes médicinales utilisées au niveau de la préfecture d’Agadir-Ida-Outanane (Maroc). J. Appl. Biosci. 2014, 81, 7198. [Google Scholar] [CrossRef]
- Benkhnigue, O.; Akka, F.B.; Salhi, S.; Fadli, M.; Zidane, A.D.e.L. Catalogue des plantes médicinales utilisées dans le traitement du diabète dans la région d’Al. J. Anim. Plant Sci. 2014, 23, 3539–3568. [Google Scholar]
- Alami, Z.; Aynaou, H.; Alami, B.; Hdidou, Y.; Latrech, H. Herbal medicines use among diabetic patients in Oriental Morocco. J. Pharmacogn. Phyther. 2015, 7, 9–17. [Google Scholar] [CrossRef]
- Ait, A.; Said, H.; Derfoufi, S.; Sbai, I.; Benmoussa, A. Research Article Ethnopharmacological survey of traditional medicinal plants used for the treatment of infantile colic in Morocco. J. Chem. Pharm. Res. 2015, 7, 664–671. [Google Scholar]
- Ghourri, M.; Zidane, L.; Douira, A. La phytothérapie et les infections urinaires (La pyélonéphrite et la cystite) au Sahara Marocain. J. Anim. Plant. Sci. 2014, 20, 3171–3193. [Google Scholar]
- Bellakhdar, J. Repertory of standard herbal drugs in the Maroccan pharmacopoea. J. Ethnopharmacol. 1991, 35, 123–143. [Google Scholar] [CrossRef]
- El Hilah, F.; Ben Akka, F.; Dahmani, J.; Belahbib, N.; Zidane, L. Étude Ethnobotanique Des Plantes Médicinales Utilisées Dans Le Traitement Des Infections Du Système Respiratoire Dans Le Plateau Central Marocain. J. Anim. Plant Sci. 2015, 25, 3886–3897. [Google Scholar]
- Mikou, K.; Rachiq, S.; Oulidi, A.J.; Beniaich, G. Étude ethnobotanique des plantes médicinales et aromatiques utilisées dans la ville de Fès au MarocEthnobotanical survey of medicinal and aromatic plants used by the people of Fez in Morocco. Phytothérapie 2016, 14, 35–43. [Google Scholar] [CrossRef]
- Fadil, M.; Farah, A.; Haloui, T.; Rachiq, S. Étude ethnobotanique des plantes exploitées par les coopératives et les associations de la région Meknès-Tafilalet au Maroc. Phytotherapie 2015, 13, 19–30. [Google Scholar] [CrossRef]
- Daoudi, A.; Bammou, M.; Zarkani, S.; Slimani, I.; Ibijbijen, J.; Nassiri, L. Étude ethnobotanique de la flore médicinale dans la commune rurale d’Aguelmouss province de Khénifra (Maroc). Phytotherapie 2015, 14, 220–228. [Google Scholar] [CrossRef]
- Eddouks, M.; Maghrani, M.; Lemhadri, A.; Ouahidi, M.L.; Jouad, H. Ethnopharmacological survey of medicinal plants used for the treatment of diabetes mellitus, hypertension and cardiac diseases in the south-east region of Morocco (Tafilalet). J. Ethnopharmacol. 2002, 82, 97–103. [Google Scholar] [CrossRef]
- Merzouki, A.; Ed-derfoufi, F.; Molero Mesa, J. Contribution to the knowledge of Rifian traditional medicine. II: Folk medicine in Ksar Lakbir district (NW Morocco). Fitoterapia 2000, 71, 278–307. [Google Scholar] [CrossRef]
- Orch, H.; Douira, A. Étude ethnobotanique des plantes médicinales utilisées dans le traitement du diabète, et des maladies cardiaques dans la région d ’ Izarène (Nord du Maroc). J. Appl. Biosci. 2015, 86, 7940–7956. [Google Scholar] [CrossRef]
- Tahri, N.; Basti, A.E.L.; Zidane, L.; Rochdi, A.; Douira, A. Etude ethnobotanique des plantes medicinales dans La province de settat (Maroc). J. For. Fac. 2012, 12, 192–208. [Google Scholar]
- Hseini, S.; Kahouadji, A.; Lahssissene, H.; Tijane, M. Analyses floristique et ethnobotanique des plantes vasculaires médicinales utilisées dans la région de Rabat (Maroc occidental). Mediterr. Bot. 2007, 100, 93–100. [Google Scholar]
- Bensalem, S.; Soubhye, J.; Aldib, I.; Bournine, L.; Nguyen, A.T.; Vanhaeverbeek, M.; Rousseau, A.; Boudjeltia, K.Z.; Sarakbi, A.; Kauffmann, J.M.; et al. Inhibition of myeloperoxidase activity by the alkaloids of Peganum harmala L. (Zygophyllaceae). J. Ethnopharmacol. 2014, 154, 361–369. [Google Scholar] [CrossRef] [PubMed]
- Chebat, A.; Skalli, S.; Errihani, H.; Boulaâmane, L.; Mokrim, M.; Mahfoud, T.; Soulaymani, R.; Kahouadji, A. Étude de prévalence des effets indésirables liés à l’utilisation des plantes médicinales par les patients de l’Institut National d’Oncologie, Rabat. Phytotherapie 2014, 12, 25–32. [Google Scholar] [CrossRef]
- Kabbaj, F.Z.; Meddah, B.; Cherrah, Y.; El, M.; Faouzi, A. Ethnopharmacological profile of traditional plants used in Morocco by cancer patients as herbal therapeutics. Phytopharmacology 2012, 2, 243–256. [Google Scholar]
- El Abbouyi, P.A.; Filali-Ansari, N.; Khyari, P.S.; Loukili, H. Inventory of medicinal plants prescribed by traditional healers in El Jadida city and suburbs (Morocco). Int. J. Green Pharm. 2014, 8, 242–251. [Google Scholar] [CrossRef]
- Tahraoui, A.; El-Hilaly, J.; Israili, Z.H.; Lyoussi, B. Ethnopharmacological survey of plants used in the traditional treatment of hypertension and diabetes in south-eastern Morocco (Errachidia province). J. Ethnopharmacol. 2007, 110, 105–117. [Google Scholar] [CrossRef]
- Ouarghidi, A.; Martin, G.J.; Powell, B.; Esser, G.; Abbad, A. Botanical identification of medicinal roots collected and traded in Morocco and comparison to the existing literature. J. Ethnobiol. Ethnomed. 2013, 9, 1. [Google Scholar] [CrossRef]
- Zeggwagh, A.A.; Lahlou, Y.; Bousliman, Y. Enquete sur les aspects toxicologiques de la phytotherapie utilisee par un herboriste à Fes, Maroc. Pan Afr. Med. J. 2013, 14, 1–6. [Google Scholar] [CrossRef]
- EL Hassani, M.; Douiri, E.M.; Bammi, J.; Zidane, L.; Badoc, A.; Douira, A. Plantes médicinales de la Moyenne Moulouya (Nord-Est du Maroc). Ethnopharmacologia 2013, 50, 39. [Google Scholar]
- African Plants (Version 3.4.0). 2016. Available online: http://africanplantdatabase.ch (accessed on 15 February 2022).
- Plant List (Version 1.1. September 2013). Available online: http://www.theplantlist.org (accessed on 15 February 2022).
- Ennaji, M. Multilingualism, Cultural Identity, and Education in Morocco; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2005. [Google Scholar]
- Trotter, R.; Logan, M. Informant consensus: A new approach for identifying potentially effective medicinal plants. Plants Indig. Med. Diet. Routledge 2019, 91–112. [Google Scholar]
- Heinrich, M.; Ankli, A.; Frei, B.; Weimann, C.; Sticher, O. Medicinal plants in Mexico: Healers’ consensus and cultural importance. Soc. Sci. Med. 1998, 47, 1859–1871. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Sample | Characteristic | Sample | ||
|---|---|---|---|---|---|
| Number | Percentage (%) | Number | Percentage (%) | ||
| Age: | Education level: | ||||
| <30 years old | 8 | 26.7 | illiterate | 1 | 3.4 |
| >30 years old | 22 | 73.4 | primary | 12 | 40 |
| Place of birth: | secondary | 9 | 30 | ||
| Eeastern Morocco | 24 | 80 | university | 5 | 16.7 |
| Outside Eeastern Morococ | 6 | 20 | fqîh | 2 | 6.7 |
| Languages and dialectare spoken: | Integration: | ||||
| Only one language | 5 | 16.7 | yes | 3 | 10 |
| Two languages | 11 | 36.7 | Locally | 10 | 33.3 |
| Three languages | 6 | 20 | National | 2 | 6.7 |
| 4–5 languages | 6 | 20 | Regional | 7 | 23.3 |
| Living outside the region: | Owning a farm: | ||||
| yes | 6 | 20 | no | 20 | 66.7 |
| never | 16 | 53.4 | yes | 3 | 10 |
| Characteristic | Sample | Characteristic | Sample | Characteristic | Sample | |||
|---|---|---|---|---|---|---|---|---|
| Number | Percentage (%) | Number | Percentage (%) | Number | Percentage (%) | |||
| Description of the professional activity | Relationships with scientific institutes: | Use of traditional medicine | ||||||
| THs: | no | 28 | 93.4 | Treatment by plants: | ||||
| versatile herbalists | 25 | 83.4 | yes | 2 | 6.7 | no | 3 | 10 |
| practitioner | 4 | 13.4 | Organization of the field of medicinal plants: | yes | 25 | 83.3 | ||
| Exercise of the profession: | unorganized | 21 | 70 | treatment by drugs: | ||||
| only | 24 | 80 | organized | 5 | 16.7 | no | 10 | 33.3 |
| others profession | 4 | 13.4 | Nature of the products sold by THs | yes | 18 | 60 | ||
| Diploma: | Materials sold: | preference: | ||||||
| no | 24 | 80 | plants | 23 | 76.7 | |||
| yes | 4 | 13.4 | minerals | 8 | 26.7 | plants | 21 | 70 |
| References: | animals | 11 | 36.7 | drugs | 11 | 36.7 | ||
| no | 20 | 66.7 | magic | 1 | 3.4 | Conservation and transmission of knowledge | ||
| yes | 2 | 6.7 | products made from plants | 10 | 33.4 | transmission from father to son: | ||
| yes, Arabic | 8 | 26.7 | preparation of herbal remedies: | no | 18 | 60 | ||
| Travel to the patient: | no | 19 | 63.4 | yes | 10 | 33.4 | ||
| no | 16 | 53.3 | yes | 3 | 10 | succession: | ||
| yes | 6 | 20 | Where do products from plants sold in his herbalism’s shop come from: | no | 23 | 76.7 | ||
| Set the price: | They don’t sell these products | 6 | 20 | yes | 7 | 23.4 | ||
| no | 2 | 6.7 | others cities of Morocco or other countries | 10 | 33.4 | Do you train people? | ||
| yes | 21 | 70 | Plants sold: | more than 11 people | 1 | 3.4 | ||
| Pay by money: | purchased | 23 | 76.7 | no | 18 | 60 | ||
| no | 1 | 3.4 | harvest | 2 | 6.7 | yes | 9 | 30 |
| yes | 22 | 73.4 | Disease diagnosis | Toxicity | ||||
| no and yes | 1 | 3.4 | You are always in your herbalism? | |||||
| Duration of the experience: | no | 9 | 30 | no response | 4 | 13.4 | ||
| de 4 at 6 years | 5 | 16.7 | interrogation | 13 | 4 | yes | 26 | 86.7 |
| 6 at 10 years | 4 | 13.4 | bodily | 3 | 10 | Which replaces THs in case of absence: | ||
| 10 at 14 years | 6 | 20 | Gives treatment after diagnostics by a doctor: | anyone | 18 | 60 | ||
| 14 years and more | 12 | 40 | no | 12 | 40 | people related to the domain | 5 | 16.7 |
| yes | 9 | 30 | ||||||
| Scientific Name | Family | Voucher | Vernacular Names | Part Used (FC) | Preparation Used (FC) | Mode of Administration (FC) | Diseases | Toxicity According to THs (FC) | Other Data (FC) | Duration of Preparation Minutes (FC) | Added Products (FC) | Dosage (FC) | FC |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Acacia gummifera Willd. | FABACEAE | HUMPOM793 | arq ṭalḥ (عَرْقْ الطَّلْحْ)/ ‘arq ṭarḥ (عَرْقْ الطَّرْحْ)/ smaġ l-’arabî صْمَغْ الْعَرَبِي | seeds (1) | powder (1) | oral route (1) | ALRP (1) | honey (1) | 1 | ||||
| Aframomum melegueta (Roscoe) K. Schum. | ZINGIBERACEAE | HUMPOM873 | lġûza ṣṣaḥrâwiya (لْكُوزَ صَّحْرَاوِيَ) | seeds (3) | powder (3) | oral route (3) | WAR (2) COLP (1) NSD (1) | a small amount should be used because the plant is toxic (2) | aromatic (2) | mixture of plants (râs l-ḥanût) (1) soup or hen (djâj baldi) (1) | 4 | ||
| Ajuga iva (L.) Schreb. | LAMIACEAE | HUMPOM809 | الشَّنْدْكُورَ ššandġûra | leaves (3) | powder (2) decoction (1) | oral route (3) | DIGP (1) COLP (1) POI (1) | honey (1) milk or honey or water (1) | a spoon every morning before or after meals (1) | 3 | |||
| Allium sativum L. | AMARYLLIDACEAE | HUMPOM749 | tûm تُومْ | bulb (5) seeds (3) | powder (3) cooked (1) juice (3) salad (1) | oral route (7) drops in nose (1) | RESP (4) CVP (3) COLP (2) IFD (2) ALRP (1) DIGP (1) HEAD (1) | honey (2) oil (1) milk (1) Acacia gummifera; Lepidium sativum; Glycyrrhiza glabra; Juncus acutus; Linum usitatissimum; Mentha spicata; Origanum majorana; Matricaria chamomilla (1) | a small spoon every morning before the meal (1) | 14 | |||
| Aloysia citriodora Palau | VERBENACEAE | HUMPOM871 | مَالْوِيزَ mâlwîza | leaves (8) | decoction (4) infusion (4) | oral route (8) | NSD (5) DIGP (5) REND (1)) | 15 (2) 5 (1) | Camellia sinensis (1) | one glass per day in the evening (1) one glass before meals (1) | 11 | ||
| Alpinia officinarum Hance) | ZINGIBERACEAE | HUMPOM874 | l-ḵodanjal الْخُدَنْجَلْ/ḵolanjân خُلَنْجَانْ | rhizome (4) | decoction (3) powder (2) | oral route (5) | WAR (3) GOD (2) DIGP (1) COLP (1) IFD (1) RHA (1) | the patient must not have had cardiac and kidney problems and gall bladder (1) | honey or milk (1) soup or hen (djâj baldi) (1) Coffea arabica (1) | 9 | |||
| Ammodaucus leucotrichus Coss. & Durieu | APIACEAE | HUMPOM752 | l-kammûnṣṣûfî الْكَمُّونْ الصُّوفِي | seeds (6) leaves (1) | decoction (3) infusion (3) powder (1) | oral route (7) | DIGP (5) NSD (3) DIA (2) NUTI (1) CHOD (1) CIRP (1) COLP (1) CVP (1) | 15 (1) | Tilia sylvestris; Origanum majorana; Crataegus laciniata (1) | 15 | |||
| Ammoides pusilla (Brot.) Breistr | APIACEAE | HUMPOM753 | nnûnḵa النُّونْخَ | leaves (4) | decoction (1) decocted with lemon (1) infusion (1) powder (1) | oral route (3) inhalation (1) washing (1) | COLP (2) WAR (2) GOD (2) NSD (1) | 15 (1) | honey (1) milk (1) | before sleep (1) | 7 | ||
| Anabasis aretioides Coss. & Moq. ex Bunge | AMARANTHACEAE | HUMPOM746 | adġa’ أَدْكَعْ | NSD (1) | toxic (1) | 1 | |||||||
| Anacyclus pyrethrum (L.) Link | ASTERACEAE | HUMPOM765 | ‘aqar qarḥa (عَقَرْ قَرْحْ) tikanṭîst (تِكَنْتِيسْتْ) | rhizome (1) | decoction (1) powder (1) | oral route (2) | DIGP (1) WAR (1) GOD (1) | honey (1) | once a day in the evening (1) | 3 | |||
| Anastatica hierochuntica L. | BRASSICACEAE | HUMPOM775 | kaf maryam كَفْ مَرْيَمْ | branches (2) | powder (2) | external route (1) oral route (1) | GOD (2) NSD (1) | milk (1) | 3 | ||||
| Apium graveolens L. | APIACEAE | HUMPOM754 | lakrâfaṣ لَكْرَافَصْ | seeds (1) | powder (1) | oral route (1) | REND (1) | honey (1) | 1 | ||||
| Arbutus pavarii Pamp. | FABACEAE | HUMPOM794 | sâsnû سَاسْنُو | seeds (1) | decoction (1) | oral route (1) | NUTI (1) CIRP (1) CVP (1) | 3 | |||||
| Argania spinosa (L.) Skeels | SAPOTACEAE | HUMPOM860 | argân أَرْكَانْ | seeds (1) | oil (1) | external route (1) | SKP (1) | 1 | |||||
| Aristolochia fontanesii Boiss. & Reut. | ARISTOLOCHIACEAE | HUMPOM764 | بَرَّزْطَمْ barrazṭam | rhizome (6) | powder (6) | oral route (6) | CAN (5) CVP (1) DIGP (1) | the plant is very toxic, it can lead to death (1) toxic (1) very toxic for the kidneys (1) | the patient must not be diabetic (1) | honey or milk (1) honey (5) | for 40 days (1) once before meals for about an hour (1) | 7 | |
| Artemisia herba alba Asso | ASTERACEAE | HUMPOM766 | šîḥ شِيحْ | aerial part (2) | decoction (2) | oral route (2) | DIGP (2) | nervous people should not use it (1) | one glass per day (1) | 2 | |||
| Astracantha gummifera (Labill.) Podlech | FABACEAE | HUMPOM795 | lakṯîra لَكْثِيرَ | resin (2) | without preparation (1) | external route (1) oral route (1) | NUTI (1) SKP (1) | Camellia sinensis or milk or honey (1) | 2 | ||||
| Avena sativa L. | POACEAE | HUMPOM843 | zwân الزْوَانْ/ ššûfân الشُّوفَانْ/ l-ḵarṭâl الْخَرْطَالْ | CHOD (1) | 1 | ||||||||
| Berberis hispanica Boiss. & Reut. | BERBARIDACEAE | HUMPOM774 | aġrîs أَغْرِيسْ | roots (5) bark (3) fresh roots (1) | powder (7) infusion (2) infused powder (1) | oral route (9) pate (1) | CAN (6) DIA (4) DIGP (2) POI (2) NUTI (1) CHOD (1) SKP (1) CVP (1) | toxic (1) | 15 (2) | Aristolochia fontanesii (1) honey (5) | before meals for 40 days (1) morning and evening before meals for 40 days (1) a teaspoon morning and evening (1) | 17 | |
| Beta vulgaris L. | AMARANTHACEAE | HUMPOM747 | šmandar شْمَنْدَر/ sokkar nabâtî سُكَّرْ نَبَاتِي | tubercules (1) | powder (1) | oral route (1) | ALRP (1) | Ammodaucus leucotrichus; Tamarindus indica; Lepidium sativum; Linum usitatissimum; Glycyrrhiza glabra and honey (1) | 1 | ||||
| Boswellia sacra Flueck. | BURSERACEAE | HUMPOM778 | ṣalabân صَلَبَانْ/ ‘udṣṣalîb l-hor عُودْ الصَّلِيبْ الْحُرْ | burn (1) | inhalation (1) | MAG (1) | 1 | ||||||
| Calamintha nepeta (L.) Savi | LAMIACEAE | HUMPOM810 | nnabṭa النَّابْطَ/ l-mânta الْمَانْتَ | leaves (6) | decoction (5) infusion (1) | oral route (6) | COLP (5) DIGP (1) REND (1) | do not drink the preparation during the day (2) | 10 (2) | milk (1) | a drink in the evening (2) | 7 | |
| Calendula arvensis (Vaill.) L. | ASTERACEAE | HUMPOM767 | jjamra الجَّمْرَ | flowers (6) | infusion (5) powder (1) | oral route (5) massage (1) | CAN (3) SKP (1) DIGP (1) HEAD (1) | 15 (2) | Aristolochia fontanesii; Berberis hispanica (1) Origanum majorana; Salvia officinalis (1) | 5 | |||
| Camellia sinensis (L.) Kuntze | THEACEAE | HUMPOM867 | atây أَتَايْ | leaves (2) | decoction (1) infusion (1) | oral route (2) | NUTI (1) CAN (1) REND (1) | Crocus sativus L. | 3 | ||||
| Cannabis sativa L. | CANNABACEAE | HUMPOM780 | laḥšîš لَحْشِيشْ/ l-kîf الْكِيفْ | seeds (2) | powder (2) | external route (2) | SKP (2) | 2 | |||||
| Capparis spinosa L. | CAPPARACEAE | HUMPOM781 | l-kabbâr الْكَبَّارْ/ tâylâlût تَايْلَالُوتْ | fruit (2) seeds (1) | burn (2) powder (1) | oral route (2) inhalation (1) | DIGP (1) COLP (1) MAG (1) GOD (1) | honey (2) milk (1) | 4 | ||||
| Capsicum annuum L. | SOLANACEAE | HUMPOM862 | l-falfal laḥmar الفَلْفَلْ لَحْمَرْ/ labzar laḥmar لَبْزَارْ لَحْمَرْ/ l-ḥârra الْحَارَّ/ ssudâniya السُّودَانِيَ/ lqalyaṭa الْقَلْيَاطَ | seeds (2) | powder (2) | oral route (2) | NUTI (2) GOD (1) | honey (2) | 3 | ||||
| Carlina gummifera (L.) Less. | ASTERACEAE | HUMPOM768 | addâd أَدَّادْ | roots (1) | burn (1) | inhalation (1) | MAG (1) | toxic (1) | 1 | ||||
| Carum carvi L. | APIACEAE | HUMPOM755 | l-karwiya الْكَرْوِيَ/ ssanût السَّانُوتْ | seeds (3) leaves (1) | decoction (2) infusion (2) | oral route (4) | DIGP (4) COLP (2) | 15 (2) | honey (2) water (1) Aloysia citriodora; Cuminum cyminum; Foeniculum vulgare; Pimpinella anisum; Carum carvi (1) | once a day every evening (1) a teaspoon in a glass of water (1) | 6 | ||
| Cassia senna L. var. senna | FABACEAE | HUMPOM796 | sanâ سَنَا/ ssanâ السَّنَا | leaves (9) | decoction (5) infusion (3) powder (1) | oral route (9) | DIGP (7) NUTI (1) CIRP (1) | toxic (2) causes hypersensitivity and irritation (1) toxic causes diarrhea (2) toxic, it causes injury to intestines and stomach (1) | 15 (2) | honey (1) Origanum majorana; Thymelaea hirsuta; Laurus nobilis (1) | 15 leaves, three times a day (1) half a glass after meals (1) one glass before meals (1) one glass per day (1) | 9 | |
| Ceratonia siliqua L. | FABACEAE | HUMPOM797 | l-ḵarrûb الْخَرُّوبْ | fruit (5) | powder (5) | oral route (5) | DIGP (4) NUTI (2) GOD (1) | honey (4) | 7 | ||||
| Chenopodium ambrosioides L. | AMARANTHACEAE | HUMPOM748 | mḵînza مْخِينْزَ | leaves (3) aerial part (1) aerial part with leaves (1) | juice (3) decoction (2) | oral route (3) external route (2) dough on the head (1) | HEAD (4) IFD (2) DIGP (1) | toxic (1) | 5 (1) | rose water (1) rose water; Allium sativum (1) honey (1) juice with Citrus sinensis (1) | six leaves in a glass of water after meals (1) | 7 | |
| Cinnamomum cassia (L.) J.Presl | LAURACEAE | HUMPOM821 | l-qarfa الْقَرْفَ | bark (3) | powder (3) | oral route (3) | GOD (2) WAR (1) RHA (1) | the patient must not have cardiac or kidney problems (1) | honey (2) hot milk (1) soup (1) hen (djâj baldi) (1) | 4 | |||
| Cistus populifolius L. | CISTACEAE | HUMPOM785 | irgal إِرْكَلْ/ hirgal هِرْكَلْ | seeds (2) | powder (2) | oral route (2) | COLP (1) GOD (1) | 50 g grilled plant + 1.5 kg of honey (1) honey (1) | a spoon each morning (1) | 2 | |||
| Citrullus colocynthis (L.) Schrad. | CUCURBITACEAE | HUMPOM787 | laḥdaj لْحَدْجَ/ l-ḥanẓal الحَنْظَل/ḥandal حَنْدَلْ | fruit (1) | without preparation (1) | foot bath (1) | DIA (2) | 2 | |||||
| Citrus limon (L.) Burm. f. | RUTACEAE | HUMPOM856 | l-ḥâmaḍ الْحَامَضْ/ lîmûn لِيمُونْ/ llîm اللِّيمْ | fruit (1) | juice (1) | oral route (1) | COLP (1) | Crocus sativus (1) | 1 | ||||
| Citrus salicifolia Raf. | RUTACEAE | HUMPOM857 | waẓmî وَظْمِي | rhizome (1) | decoction (1) | oral route (1) | IFD (1) WAR (1) GOD (1) | toxic (1) | 3 | ||||
| Coriandrum sativum L. | APIACEAE | HUMPOM756 | l-qaṣbar (الْقَصْبَرْ) | seeds (4) | burn (2) powder (2) | inhalation (2) oral route (2) | MAG (2) DIGP (1) | toxic, it must be used for a short time (1) | honey (1) | 3 | |||
| Corrigiola telephiifolia Pourr. | MOLLUGINACEAE | HUMPOM827 | sarġîna (سَرْغِينَ) | rhizome (2) | burn (1) powder (1) | inhalation (1) external route (1) | SKP (1) MAG (1) | 2 | |||||
| Costus (ND) | ZINGIBERACEAE | HUMPOM875 | القِسْطْ الْبَحْرِي lqisṭ lbaḥrî | branches (3) | powder (3) | external route (2) oral route (1) | SKP (2) IFD (1) POI (1) RESP (1) | honey (2) | 150 g in 4 L of water (1) one spoon per glass of hot water twice a day (1) one spoon per glass of hot water and honey twice a day morning and evening (1) | 5 | |||
| Crataegums monogyna Jacq. | ROSACEAE | HUMPOM850 | admâm (أَدْمَامْ)/ zza’rûr (الزَّعْرُورْ) | leaves (7) | infusion (6) | oral route (6) | CVP (4) NSD (3) DIGP (2) CIRP (1) | it should not be used by pregnant women who have a thyroid gland (1) | 15 (3) | Tilia sylvestris; Origanum majorana; Matricaria chamomilla (1) | 10 | ||
| Crocus sativus L. | IRIDACEAE | HUMPOM806 | za’frân zzaġba زَعْفْرَانْ الزَّغْبَ/ za’frân lhûr زَعْفْرَانْ الْحُرْ/ za’frân šša’ra زَعْفْرَانْ الشَّعْرَ | petals (10) | infusion (6) powder (3) decoction (2) | oral route (10) | NUTI (3) CAN (2) COLP (2) REND (2) IFD (1) WAR (1) | aromatic, for cooking (2) | 15 (5) | honey (2) vinegar of Malus pumila or lemon (1) Camellia sinensis (1) vinegar of Malus pumila (1) lemon (1) Camellia sinensis (1) Rubia peregrina (1) mixture of plants (râs l-ḥanût) (1) | 11 | ||
| Cuminum cyminum L. | APIACEAE | HUMPOM757 | l-kammûn الْكَمُّونْ | seeds (1) | powder (1) | oral route (1) | DIGP (1) NSD (1) | 2 | |||||
| Curcuma longa L. | ZINGIBERACEAE | HUMPOM876 | l-ḵarqûm الْخَرْقُومْ/ l-karkam الْكَرْكَمْ/ l-’ûd laṣfar الْعُودْ لَصْفَرْ | branches bark (6) | powder (5) decoction (1) | oral route (6) | IFD (2) NUTI (1) DIGP (1) WAR (1) GOD (1) RHA (1) | condiment; coloring (1) | honey (3) soup orhen (djâj baldi) (1) hot water (1) | one glass three times a day (1) once in the morning before meals for a period of 10 to 15 days (1) | 7 | ||
| Cydonia oblonga Mill. | ROSACEAE | HUMPOM851 | ṣfarjal صْفَرْجَلْ | fruit (1) | juice (1) | oral route (1) | NSD (1) | milk (1) | 1 | ||||
| Cynara cardunculus L. | ASTERACEAE | HUMPOM769 | l-ḵoršaf الْخُرْشَفْ/ l-ḥak الْحَكْ | aerial part (1) | decoction (1) | oral route (1) | DIGP (1) | 1 | |||||
| Daphne gnidium L. | THYMELAEACEAE | HUMPOM868 | alazzâz أَلَزَّازْ | leaves (4) | powder (4) | external route (4) | SKP (4) | Lawsonia inermis (2) mixtur of plants (ḵalṭa) (1) | 4 | ||||
| Datura stramonium L. | SOLANACEAE | HUMPOM863 | šdaq jmal شْدَقْ جْمَلْ | MAG (1) | toxic acts on the central nervous system (1) | 1 | |||||||
| Delphinium staphisagria L. | RANUNCULACEAE | HUMPOM848 | ḥâbbat râs حَبَّةْ رَاسْ | powder (3) | external route (3) | SKP (3) | Lawsonia inermis (1) | 3 | |||||
| Dittrichia viscosa (L.) Greuter | ASTERACEAE | HUMPOM770 | maġramân مَكْرَمَانْ/ mayramân مَيْرَمَانْ | aerial part (2) | masticate (1) | oral route (2) | DIGP (1) RHA (1) | aromatic (2) | 2 | ||||
| Elettaria cardamomum (L.) Maton | ZINGIBERACEAE | HUMPOM877 | qa’ qollâ قَاعْ قُلَّا/ habḥân حَبْ هَانْ | seeds (1) | powder (1) | oral route (1) | WAR (1) GOD (1) | soup or hen (djâj baldi) (1) | 2 | ||||
| Eruca vesicaria (L.) Cav. | BRASSICACEAE | HUMPOM776 | jjarjîr الجَّرْجِيرْ | seeds (2) leaves (1) fresh leaves (1) | oil (3) infusion (1) | oral route (4) | CHOD (2) GOD (2) NUTI (1) | toxic, a small amount is used (1) toxic causes prostate pain (1) | 10 (1) | honey (1) | a spoon in a glass of water and a little honey three times a day (1) a spoon in a glass of water morning and evening (1) a spoon and two spoon of honey morning and evening (1) | 4 | |
| Eucalyptus torquata Luehm. | MYRTACEAE | HUMPOM829 | kâlîptûs كَالْيبْتُوسْ | leaves (2) | decoction (2) | massage (1) oral route (1) | ALRP (1) RESP (1) | 2 | |||||
| Euphorbia falcata L. | EUPHORBIACEAE | HUMPOM790 | ḥayât annofûs حَيَاةْ النُّفُوسْ | seeds (1) | powder (1) | oral route (1) | GOD (1) | honey (1) | 1 | ||||
| Euphorbia resinifera O. Berg | EUPHORBIACEAE | HUMPOM791 | takkâwt تَكَّاوْتْ/ tikkîwt تِكِّيوْتْ | powder (1) | external route (1) | SKP (1) | 1 | ||||||
| Ferula communis L. | APIACEAE | HUMPOM758 | l-fasûḵ الْفَاسُوخْ/ šajrat kalḵ شَجْرَةْ كَلْخْ/ l-bûbâl الْبُوبَالْ | seeds (1) | maceration (1) powder (1) | inhalation (1) oral route (1) | POI (1) | 1 | |||||
| Foeniculum vulgare Mill. | APIACEAE | HUMPOM759 | nnâfa’ النَّافَعْ/ l-basbâs الْبَسْبَاسْ | seeds (9) roots (1) | powder (6) decoction (4) infusion (1) | oral route (10) | DIGP (7) NUTI (2) REND (1) NSD (1) | confectionery (1) | 5 (1) | honey (3) meal (1) water (1) milk (1) | a spoon in the morning before the meal or in the evening after the meal (1) | 11 | |
| Fraxinus angustifolia Vahl | OLEACEAE | HUMPOM833 | tûzzâlat تُوزَّالَتْ/ lsânṭayr لْسَانْ طَيْرْ | seeds (3) | cooked (2) without preparation (1) powder (1) | oral route (2) to chew (1) | COLP (2) NUTI (1) WAR (1) GOD (1) | aromatic, for cooking (2) | meal (1) mixsture of plants (râs l-ḥanût) or meal (couscous) (1) soup (1) hen (djâj baldi) (1) | 5 | |||
| Globularia alypum L. | PLANTAGINACEAE | HUMPOM842 | ‘în larnab (عِينْ لَرْنَبْ) | leaves (1) | decoction (1) | oral route (1) | DIGP (1) | 1 | |||||
| Glycine max (L.) Merr. | FABACEAE | HUMPOM798 | ṣûjâ صُوجَا | seeds (4) | powder (4) | oral route (4) | NUTI (3) CHOD (1) | honey (2) Foeniculum vulgare, Linum usitatissimum, Pimpinella anisum, Carum carvi, pollen of Phoenix dactylifera (1) juice (1) drink (1) | three times a day (1) | 4 | |||
| Glycyrrhiza glabra L. | FABACEAE | HUMPOM799 | ‘arq ssûs عَرْقْ السُّوسْ | branches (4) | powder (3) decoction (1) | oral route (4) | ALRP (3) NUTI (1) DIGP (1) RESP (1) | for the patient must not have hypertension (1) | 5 (1) | honey (1) water (2) | two spoon in a glass of water for 40 days (1) three times a day (1) a spoon in a glass of water for 40 days (1) | 6 | |
| Helianthus annuus L. | ASTERACEAE | HUMPOM771 | ‘abbad š-šams عَبَّادْ الشَّمْسْ/ nowwâr š-šams نُوَّارْ الشَّمْسْ | seeds (1) petals (1) | powder (2) | oral route (2) | ALRP (1) CAN (1) | one to two scoops Three times a day (1) | 2 | ||||
| Herniaria hirsuta L. | CARYOPHYLLACEAE | HUMPOM783 | harrâst laḥjar هَرَّاسَةْ لَحْجَرْ/ fattâtat laḥjar فَتَّاتَةْ لَحْجَرْ | aerial part (3) leaves (1) flowering top (1) | decoction (5) | oral route (5) | REND (5) | toxic, long use causes irritation (1) | 15 (1) | Aristolochia fontanesii; Calendula arvensis; Berberis hispanica; Nigella sativa; Juncus acutus; Aloe succotrina; Citrullus colocynthis and honey (miel of darhmouss) (1) | two glasses three times a day (1) half a liter a day (1) one glass three times a day (1) | 5 | |
| Hibiscus sabdariffa L. | MALVACEAE | HUMPOM825 | karkadî كَرْكَدِي | flowers (6) leaves (2) | infusion (7) decoction (1) | oral route (8) | DIGP (3) CVP (3) ALRP (1) SKP (1) DIA (1) NSD (1) | 15 (4) | Vitis vinifera; Urtica dioïca; Olea europaea; Berberis hispanica (1) Salvia officinalis; Matricaria chamomilla; Origanum majorana (1) Matricaria chamomilla; Mentha spicata; Laurus nobilis; Thymelaea hirsuta (1) Salvia officinalis; Matricaria chamomilla; Mentha spicata; Rosmarinus officinalis; Myrtus communis (1) | a glass after meals (1) | 10 | ||
| Hordeum vulgare L. | POACEAE | HUMPOM844 | š’îr شْعِيرْ/ zra’ زْرَعْ/ ttalbîna التَّلْبِينَ | seeds (2) | decoction (1) powder (1) cooked powder (1) cooked (1) | oral route (3) | NUTI (2) CVP (2) NSD (2) DIGP (1) | honey (2) | 7 | ||||
| Hyoscyamus albus L. | SOLANACEAE | HUMPOM864 | bûnarjûf بُونَرُجُوفْ | burn (1) decoction (1) powder (1) | drops (1) inhalation (1) external route (1) | SKP (1) MAG (1) OPHP (1) | toxic (3) | 3 | |||||
| Hyoscyamus niger L. | SOLANACEAE | HUMPOM865 | sikrân سِكْرَانْ | burn (1) decoction (1) powder (1) | drops (1) inhalation (1) external route (1) | SKP (1) MAG (1) OPHP (1) | toxic (3) | 3 | |||||
| Illicium verum Hook.f. | SCHISANDRACEAE | HUMPOM861 | l-baḍyân الْبَضْيَانَ/ l-yansûn الْيَنْسُونْ/ rjîla الرْجِيلَ | fruit (8) | powder (5) cooked powder (2) decoction (1) | oral route (6) mouthwash (1) to chew (1) | TOP (2) WAR (2) GOD (2) ALRP (1) NUTI (1) CHOD (1) CIRP (1) CVP (1) POI (1) REND (1) | honey (2) soup (1) hen (djâj beldi) (1) meal (1) | 12 | ||||
| Juglans regia L. | JUGLANDACEAE | HUMPOM807 | l-ġarġâ’ الْكَرْكَاعْ/ swâk السْوَاكْ | bark (1) fruit (1) | decoction (1) powder (1) | oral route (2) | NUTI (1) TOP (1) DIGP (1) | honey (1) | 3 | ||||
| Juncus acutus L. | JUNCACEAE | HUMPOM808 | ṣmâr صْمَارْ | flowers (2) roots (1) | powder (2) decoction (1) | oral route (3) | ALRP (1) REND (1) | used as rugs for mosquets (1) | honey (2) | 2 | |||
| Lagenaria siceraria (Molina) Standl. | CUCURBITACEAE | HUMPOM788 | lgar’a slâwiya لْكَرْعَ سْلَاوِيَ | fruit bark (1) | burn (1) | inhalation (1) | HEAD (1) | 1 | |||||
| Laurus nobilis L. | LAMIACEAE | HUMPOM811 | warqat sidna mûsa وَرْقَةْ سِيدْنَا مُوسَى | leaves (3) | cooked (1) decoction (1) powder (1) | oral route (2) | DIGP (2) | aromatic (1) | meal (1) honey (1) | 2 | |||
| Lavandula dentata L. | LAMIACEAE | HUMPOM812 | ḵzamâ خْزَامَى | flowers (8) tip (4) leaves (3) | decoction (9) powder (3) infusion (1) | oral route (9) external route (4) inhalation (1) | GOD (5) SKP (4) COLP (2) WAR (2) REND (2) DIGP (1) NSD (1) | not used by people with cardiac problems (1) | aromatic (2) | Origanum compactum; Ammoides pusilla; Mentha pulegium (1) mixsture (ḵalṭa) (2) | two glasses, three times a day (1) one glass, after meals (1) one glass, three times a day (1) | 17 | |
| Lawsonia inermis L. | LYTHRACEAE | HUMPOM823 | l-ḥanna الْحَنَّ/ l-ḥannî الْحَنِّي | leaves (2) | powder (2) | external route (2) | SKP (2) | 2 | |||||
| Lepidium sativum L. | BRASSICACEAE | HUMPOM777 | ḥab ršâd حَبْ رْشَادْ/ l-ḥarf الْحَرْفْ | seeds (9) | powder (6) decoction (1) infusion (1) cooked powder (1) | oral route (7) direct a seed into the eye (1) gouttes (1) | NUTI (2) ALRP (2) OPHP (2) GOD (2) COLP (1) REND (1) | honey (5) meal (1) | 10 | ||||
| Linum usitatissimum L. | LINACEAE | HUMPOM822 | zarrî’t lakattan (زَرِّيعَةْ الْكَتَّانْ | seeds (7) | powder (5) decoction (2) | oral route (7) | ALRP (3) NUTI (2) DIGP (2) CHOD (1) OPHP (1) REND (1) | honey (4) milk (1) Eruca vesicaria; Nigella sativa and honey (1) Glycyrrhiza glabra (1) | 9 | ||||
| Lupinus albus L. | FABACEAE | HUMPOM800 | tarmas (تَرْمَسْ)/ l-fûl lmiṣrî (الْفُولْ الْمِصْرِي) | seeds (2) | powder (2) | oral route (2) | ALRP (1) DIA (1) DIGP (1) CVP (1) | camel fat (1) | we add half a glass to a glass of water and take it two or three times a day (1) | 4 | |||
| Malus pumila Mill. | ROSACEAE | HUMPOM852 | taffâḥ (تَفَّاحْ) | fruit (3) | vinegar (2) salad (1) | oral route (3) | NUTI (1) CHOD (1) COLP (1) | Crocus sativus (1) | before meals (1) a large spoon of warm water every morning (1) | 3 | |||
| Mandragora officinarum L. | SOLANACEAE | HUMPOM866 | bîḍ l-ġûl بِيضْ الْغُولْ/ aryâla أَرْيَالَ/ ‘ašbat aytâm عَشْبَةْ أَيْتَامْ | rhizome (1) | powder (1) | oral route (1) | CAN (1) WAR (1) GOD (1) | mixture of plants (râs l-ḥanût) (1) | 3 | ||||
| Matricaria chamomilla L. | ASTERACEAE | HUMPOM772 | bâbûnj بَابُونْجْ/ mânsâniya مَانْسَانِيَ | flowers (15) leaves (2) | infusion (10) decoction (6) powder (2) maceration (1) | oral route (14) drops (1) inhalation (1) external route (1) | DIGP (5) NSD (5) HEAD (4) NUTI (3) ALRP (3) SKP (2) RESP (2) CIRP (1) OPHP (1) | 15 (5) 5 (1) 20 (1) | honey (2) | three times a day (1) | 25 | ||
| Mentha pulegium L. | LAMIACEAE | HUMPOM813 | fliyyû فْلِيُّو | aerial part (3) | decoction (3) | oral route (3) | COLP (3) DIGP (1) | 4 | |||||
| Mentha spicata L. | LAMIACEAE | HUMPOM814 | na’nâ’ نَعْنَاعْ | leaves (7) | infusion (5) powder (1) vinegar (1) | oral route (7) washing (1) | NUTI (3) NSD (3) ALRP (2) GOD (2) DIGP (1) WAR (1) REND (1) | 15 (4) 16 (1) | mixture of plants (râs l-ḥanût) (1) honey (1) Salvia officinalis; Origanum majoran (1) | three times a day (4) | 13 | ||
| Myristica afragrans Houtt. | MYRISTICACEAE | HUMPOM828 | l-ġûza الْكُوزَ/ ġûzatṭṭîb كُوزَةْ الطِّيبْ/ ġûzat ššark كُوزَةْ الشَّرْكْ/ bsîbîsa | seeds (5) | powder (4) cooked powder (1) | oral route (5) | WAR (2) GOD (2) NUTI (1) DIGP (1) NSD (1) | aromatic, for cooking (1) | soup (2) hen (djâj beldi) (2) meal (2) mixture of plants (râs l-ḥanût) (1) | 7 | |||
| Myrtus communis L. | MYRTACEAE | HUMPOM830 | rîḥân رِيحَانْ | leaves (10) | decoction (7) infusion (2) powder (1) | oral route (7) external route (3) | DIGP (4) SKP (3) NUTI (1) CHOD (1) CIRP (1) DIA (1) POI (1) HEAD (1) | 15 (1) | Lawsonia inermis (1) mixture of plant (ḵalṭa) (1) | a glass in the morning before the meal (1) a glass in the morning before the meal or before sleep (1) | 13 | ||
| Nerium oleander L. | APOCYNACEAE | HUMPOM761 | ddafla الدَّفْلَ/ alîlî أَلِيلِي/ arîrî أَرِيرِي | branches (1) leafy branches (1) | burn (2) | inhalation (2) | TOP (1) HEAD (1) | 2 | |||||
| Nigella sativa L. | RANUNCULACEAE | HUMPOM847 | ssanûj السَّانُوجْ/ l-ḥabba sawda حَبَّ سَوْدَا/ḥabbat l-baraka حَبَّةْ الْبَرَكَ | seeds (8) | powder (7) cooked powder (1) | oral route (8) | COLP (2) RESP (2) CAN (1) DIA (1) DIGP (1) CVP (1) REND (1) GOD (1) RHA (1) NSD (1) | toxic (1) | honey (5) meal (1) | 12 | |||
| Ocimum basilicum L. | LAMIACEAE | HUMPOM815 | laḥbaq لَحْبَقْ | aerial part (1) | infusion (1) | oral route (1) | GOD (1) | 1 | |||||
| Olea europaea L. | OLEACEAE | HUMPOM834 | zaytûn زَيْتُونْ/ zabbûj زَبُّوجْ | fruit (1) | oil (1) | oral route (1) | DIGP (1) | 1 | |||||
| Opuntia ficus-indica (L.) Mill. | CACTACEAE | HUMPOM779 | l-handya الْهَنْدِيَ | flowers (3) | decoction (1) infusion (1) powder (1) | oral route (3) | REND (2) DIGP (1) | 15 (1) | honey (1) Rubia peregrina; Alpinia officinarum; Zea mays L.; Thymelaea hirsuta; Tetraena gaetula; Origanum majorana; Salvia officinalis; Matricaria chamomilla; Mentha spicata (1) | 3 | |||
| Origanum compactum Benth. | LAMIACEAE | HUMPOM816 | za’tar زَعْتَرْ | leaves (14) | decoction (9) infusion (3) powder (2) cooked powder (1) | oral route (13) massage (1) | DIGP (5) COLP (5) REND (3) GOD (3) WAR (2) NUTI (1) CHOD (1) CIRP (1) SKP (1) DIA (1) POI (1) RESP (1) NSD (1) | aromatic, for cooking (1) | 5 (2) 10 (2) 15 (2) | meal (1) honey (1) Matricaria chamomilla; Crataegus laciniata (1) salvia officinalis (1) Mentha spicata (1) | before sleep (2) after the meal (1) two glasses twice a day (1) once a day morning or evening (1) | 26 | |
| Origanum majorana L. | LAMIACEAE | HUMPOM817 | mardaddûš (مَرْدَدُّوشْ) | leaves (12) aerial part (1) | infusion (10) decoction (2) powder (1) | oral route (12) | DIGP (6) ALRP (3) NSD (3) CVP (2) CIRP (1) | aromatic, for cooking (1) | 15 (8) | three times a day (4) a glass after meals (1) a tea spoon (1) | 15 | ||
| Panax ginseng C.A.Mey. | ARALIACEAE | HUMPOM762 | ‘arq l-ḥayat عَرْقْ الْحَيَاةْ/ jînsîng (جِينْسِينْكْ) | roots (2) | powder (2) | oral route (2) | NUTI (2) GOD (1) | honey (2) pollens of Phoenix dactylifera (1) | 3 | ||||
| Papaver rhoeas L. | PAPAVERACEAE | HUMPOM836 | banna’mân بَنَّعْمَانْ | seeds (1) | powder (1) | oral route (1) | COLP (1) GOD (1) | honey (1) | 2 | ||||
| Papaver somniferum L. | PAPAVERACEAE | HUMPOM837 | ḵaršâša خَرْشَاشَ | seeds (2) | burn (1) powder (1) | fumigation (1) oral route (1) | NSD (2) | a small amount should be used (1) toxic (1) | meal (1) | 2 | |||
| Peganum harmala L. | NITRARIACEAE | HUMPOM832 | l-ḥarmal الْحَرْمَلْ | seeds (11) fresh seeds (1) | powder (5) decoction (3) burn (2) oil (1) | external route (5) inhalation (3) oral route (2) | SKP (6) MAG (3) COLP (2) RHA (2) CVP (2) DIA (1) WAR (1) GOD (1) NSD (1) HEAD (1) | toxic (1) toxic causes dizziness (1) | honey (1) water (1) mixture of plants (ḵalṭa) (1) | 250 g in 1.5 L of water in decoction until half of the water has evaporated, then add the honey (1) once a day in the morning for 40 (1) | 20 | ||
| Phillyrea angustifolia L. | OLEACEAE | HUMPOM835 | mlîlâs مْلِيلَسْ | leaves (3) branches (1) | decoction (3) | oral route (3) | IFD (3) | one liter per day three times per day before meals (1) | 3 | ||||
| Phoenix dactylifera L. | ARECACEAE | HUMPOM763 | tmar تْمَرْ/ naḵla نَخْلَ | pollens (3) | powder (3) | oral route (3) | NUTI (3) GOD (3) NSD (3) CIRP (2) WAR (2) | honey (1) Panax ginseng and honey (1) | one spoon in the morning (1) one spoon in the morning before meals (1) | 13 | |||
| Pimpinella anisum L. | APIACEAE | HUMPOM760 | ḥabbatḥlâwa حَبَّةْ حْلَاوَ/ l-yansûn اليَنْسُونْ | seeds (4) leaves (1) | decoction (2) infusion (2) powder (1) | oral route (5) | NSD (3) NUTI (2) CHOD (1) CIRP (1) DIA (1) DIGP (1) | 15 (2) 20 (1) | Ammodaucus leucotrichus; Foeniculum vulgare; Carum carvi; Aloysia citriodora; Origanum majorana; Linum usitatissimum; Foeniculum vulgare (1) honey (1) | 8 | |||
| Piper cubeba L. f. | PIPERACEAE | HUMPOM839 | l-kabbâba الْكَبَّابَ | seeds (2) | powder (1) cooked powder (1) | oral route (2) | NUTI (1) WAR (1) GOD (1) | meal (1) soup or (djâj baldi) (1) | 3 | ||||
| Piper longum L. | PIPERACEAE | HUMPOM840 | dâr falfal دَارْ فَلْفَلْ | seeds (2) | powder (2) | oral route (2) | GOD (1) RHA (1) | the patient must not have cardiac or kidney problems (1) | honey (1) honey or hot milk (1) | 2 | |||
| Piper nigrum L. | PIPERACEAE | HUMPOM841 | labzâr لَبْزَارْ/ labzâr lakḥal لَبْزَارْ لَكْحَلْ/ labzâr labyaḍ لَبْزَارْ لَبْيَضْ | fruit (1) tops (1) | powder (2) | oral route (2) | WAR (2) GOD (2) | soup (1) hen (djâj baldi) (1) | 4 | ||||
| Pistacia atlantica Desf. | ANACARDIACEAE | HUMPOM750 | labṭam لَبْطَمْ | MAG (1) | 1 | ||||||||
| Pistacia Ientiscus L. | ANACARDIACEAE | HUMPOM751 | drû الدْرُو/ fâdîṣ فَادِيصْ | leaves (1) | decoction (1) powder (1) | external route (1) oral route (1) | SKP (1) DIGP (1) | lawsonia inermis (1) | one glass three times a day (1) | 2 | |||
| Prunus dulcis (Mill.) D. A. Webb | ROSACEAE | HUMPOM853 | lûz لُوزْ | fruit (1) | powder (1) | oral route (1) | NUTI (1) | honey (1) | 1 | ||||
| Punica granatum L. | LYTHRACEAE | HUMPOM824 | rommân رُمَّانْ | fruit bark (8) | powder (5) decoction (3) | oral route (8) | DIGP (8) | honey (3) milk (2) camellia sinensis (1) water (1) | one glass morning before meals (2) one glass per day (1) one spoon per day morning before meals or evening after meals (1) | 8 | |||
| Quercus faginea Lam. | FAGACEAE | HUMPOM804 | l’aṣfa الْعَصْفَ | powder (1) | external route (1) | SKP (1) | 1 | ||||||
| Quercus suber L. | FAGACEAE | HUMPOM805 | dbâġ الدّْبَاغْ/ tzâḵt تْزَاخْتْ | bark (8) | powder (4) dcocted powder (2) decoction (1) | oral route (6) external route (1) | DIGP (6) SKP (1) | 15 (1) | honey (3) milk (2) oil (1) water (1) | morning before meals (1) half a teaspoon (1) a glass in the morning (1) a glass three times a day (1) a spoon in the morning before meals or in the evening after meals (1) | 7 | ||
| Ricinus communis L. | EUPHORBIACEAE | HUMPOM792 | l-ḵarwa’ الْخَرْوَعْ/ lakrank لَكْرَنْكْ | seeds (4) | powder (4) | external route (2) oral route (2) | SKP (2) COLP (1) RHA (1) | toxic to the stomach (1) | mixture of plants (râs l-ḥanût) (1) honey (1) oil (1) | 4 | |||
| Rosa centifolia L. | ROSACEAE | HUMPOM854 | ward وَرْدْ | flowers (10) | decoction (5) powder (5) | oral route (6) external route (4) | SKP (5) DIGP (5) | toxic (1) | Cassia senna L. var. senna (1) mixture of plants (ḵalṭa) (1) | one glass per day (1) one spoon per day morning before meals (1) | 10 | ||
| Rosmarinus officinalis L. | LAMIACEAE | HUMPOM818 | azîr أَزِيرْ/ yazîr يَزِيرْ | leaves (11) | decoction (6) infusion (4) | oral route (11) | DIGP (3) REND (3) COLP (2) ALRP (1) NUTI (1) CAN (1) CHOD (1) CIRP (1) DIA (1) CVP (1) NSD (1) | patients with hypertenssion should not use it (1) | 15 (3) | a glass in the morning three times a day (2) a glass in the morning (1) a teaspoon plus a glass of water (1) | 16 | ||
| Rubia peregrina L. | RUBIACEAE | HUMPOM855 | l-fowwa فُوَّ | seeds (2) | infusion (2) decoction (1) | oral route (3) | DIGP (2) NUTI (1) | 15 (2) | Crocus sativus (1) | 3 | |||
| Ruta chalepensis L. | RUTACEAE | HUMPOM858 | l-fîjal لْفِيجَلْ/ awirmî أَوِرْمِي | flowers (5) leaves (2) | decoction (3) burn (1) decoction in oil (1) powder (1) | oral route (4) external route (2) inhalation (1) | MAG (5) SKP (1) DIA (1) COLP (1) NSD (1) | toxic (4) | rose water (1) | one glass three times a day (2) | 9 | ||
| Salvia officinalis L. | LAMIACEAE | HUMPOM819 | sâlmiya سَالْمِيَ | leaves (10) aerial part (2) | infusion (9) decoction (3) | oral route (11) khol (1) | DIA (5) DIGP (4) NUTI (2) ALRP (2) GOD (2) NSD (2) CHOD (1) CIRP (1) IFD (1) OPHP (1) | 15 (7) | 21 | ||||
| Sesamum indicum L. | PEDALIACEAE | HUMPOM838 | janjlân جَنْجْلَانْ | seeds (1) | decoction (1) | oral route (1) | CIRP (1) | 10 (1) | 1 | ||||
| Sorghum bicolor (L.) Moench | POACEAE | HUMPOM845 | l-bašna الْبَشْنَ | seeds (2) | decoction (1) powder (1) | external route (1) oral route (1) | SKP (1) DIA (1) | 2 | |||||
| Syzygium aromaticum (L.) Merr. & L. M. Perry (3) | MYRTACEAE | HUMPOM831 | l-qronfol الْقْرُنْفُلْ/ ‘ûd nnûwwâr عُودْ النُّوَّارْ | clove (3) | cookted (1) infusion (1) cookted powder (1) | oral route (2) mouthwash (1) | TOP (2) COLP (2) REND (1) | we must use a small amount because it is toxic (1) | mixture of plants (râs l-ḥanût) (1) meal (1) | 4 | |||
| Tamarindus indica L. | FABACEAE | HUMPOM801 | tmar hindî تَمْرْ هِنْدِي | fruit (3) | powder (3) | oral route (3) | WAR (2) GOD (2) NUTI (1) ALRP (1) | honey (1) Phoenix dactylifera; Alpinia officinarum; mixture of plants (râs l-ḥanût) and honey (2) | 6 | ||||
| Telephium imperati L. | CARYOPHYLLACEAE | HUMPOM784 | ḵayyâṭa خَيَّاطَ | aerial part (1) | powder (1) | external route (1) | CIRP (1) | 1 | |||||
| Terfesia (ND) | HUMPOM880 | ttarfâs التَّرْفَاسْ | tubers (1) | cookted (1) | oral route (1) | NUTI (1) | 1 | ||||||
| Terminalia chebula Retz. | COMBRETACEAE | HUMPOM786 | hlîlaj هْلِيلَجْ | seeds (4) | powder (4) | oral route (3) external route (1) | NUTI (2) GOD (2) SKP (1) DIGP (1) | honey (3) mixture of plants (râs l-ḥanût) (2) | 50 g with 1.5 kg honey (1) | 6 | |||
| Tetraclinis articulata (Vahl) Mast. | CUPRESSACEAE | HUMPOM789 | l-’ar’âr العرعار | leaves (6) seeds (2) roots (1) branches (1) | burn (4) decoction (2) powder (2) | inhalation (4) oral route (3) | DIGP (4) MAG (4) | patients with hypertenssin should not use it (1) | a spoon before meals (1) | 8 | |||
| Tetraena gaetula (Emb. & Maire) Beier & Thulin | ZYGOPHYlLACEAE | HUMPOM879 | l-’aggâya (الْعَكَّايَ) | leaves (3) | infusion (2) powder (1) | oral route (3) | DIGP (2) DIA (1) | 15 (2) | Origanum majorana; Salvia officinalis; Mentha spicata; Matricaria chamomilla (1) | 3 | |||
| Thymelaea hirsuta (L.) Endl. | THYMELAEACEAE | HUMPOM869 | l-matnân الْمَتْنَانْ | leaves (2) | infusion (2) | oral route (2) | DIGP (2) | 15 (1) | 2 | ||||
| Thymus broussonetii Boiss. | LAMIACEAE | HUMPOM820 | z’îtra زْعِيتْرَ/ ajûkannî (أَزُوكَنِّي) | leaves (3) | decoction (1) infusion (1) cookted powder (1) | oral route (3) | NUTI (1) CHOD (1) CIRP (1) DIA (1) COLP (1) REND (1) | 10(1)15(1) | meal (1) | 5 | |||
| Tilia sylvestris Desf. | MALVACEAE | HUMPOM826 | zzayzafûn الزَّيْزَفُونْ | infusion (1) | oral route (1) | DIGP (1) NSD (1) | 2 | ||||||
| Trigonella foenum-graecum L. | FABACEAE | HUMPOM802 | l-ḥalba الْحَلْبَ | seeds (7) | powder (4) decoction (2) without preparation (1) cookted powder (1) decocted powder (1) | oral route (6) external route (1) | NUTI (4) GOD (3) DIGP (2) DIA (1) REND (1) | Linum usitatissimum; Foeniculum vulgare; Glycine max and honey (1) Mentha spicata and honey (1) meal (1) | the seeds + glass of alcohol + 24 h after a glass of oil + 24 h is added and the mixture is decocted in a water bath until the alcohol has evaporated and a perfume is added (1) | 11 | |||
| Urtica dioïca L. | URTICACEAE | HUMPOM870 | l-ḥorrîġa الْحُرِّيكَ | leaves (7) aerial part (1) | infusion (7) decoction (1) | oral route (8) | DIA (4) NUTI (3) REND (3) CVP (2) CIRP (1) | 15 (6) | salvia officinalis; Vitis vinifera (1) Alpinia officinarum; Vitis vinifera; Crataegus laciniata; Origanum majorana (1) Rubia peregrina (1) | a spoon three times a day (4) a tea spoon three times a day (1) | 13 | ||
| Valeriana celtica L. | CAPRIFOLIACEAE | HUMPOM782 | السَّنْبَلْ ssanbal | decoction (1) | oral route (1) | REND (1) | 1 | ||||||
| Vicia faba L. | FABACEAE | HUMPOM803 | l-fûl الفُولْ | seeds (1) | cookted (1) | oral route (1) | ALRP (1) | maceration remove bark then powder and add camel fat (1) | a glass morning and evening (1) | 1 | |||
| Viscum album L. | SANTALACEAE | HUMPOM859 | linjbâr لِنْجْبَارْ | seeds (2) | powder (2) | oral route (2) | RHA (2) | milk (1) | 2 | ||||
| Vitis vinifera L. | VITACEAE | HUMPOM872 | ddâlya الدَّالْيَ | leaves (8) | infusion (8) | oral route (8) | CIRP (5) CHOD (2) DIA (2) NUTI (1) CVP (1) | it is toxic, causes diarrhea (6) | 15 (7) | Matricaria chamomilla, Myrtus communis, Origanum compactum, Rosmarinus officinalis, Ammodaucus leucotrichus, Pimpinella anisum, salvia officinalis (1) vinegar of Malus pumila (1) salvia officinalis; Urtica dioïca (1) Urtica dioïca (1) Origanum majorana; Cassia senna L. var. senna (1) Crataegus laciniata (1) milk (1) | 11 | ||
| Warionia saharae Benth. & Coss. | ASTERACEAE | HUMPOM773 | afassâs أَفَسَّاسْ | leaves (1) | decoction in oil (1) | massage (1) | MAG (1) | 1 | |||||
| Zea mays L. | POACEAE | HUMPOM846 | ddra الدّْرَ | pistil (2) | powder (2) | oral route (2) | DIGP (2) | honey (2) | 2 | ||||
| Zingiber officinale Roscoe | ZINGIBERACEAE | HUMPOM878 | sakkîn jbîr سَكِّينْ جْبِيرْ | rhizome (5) | powder (3) decoction (2) | oral route (4) massage (1) | DIGP (2) WAR (2) GOD (2) IFD (1) RHA (1) | the patient must not have cardiac or kidney problems (1) | honey (1) hot milk (1) soup (1) hen (djâj baldi) (1) oil (1) | 8 | |||
| Ziziphus lotus (L.) Lam. | RHAMNACEAE | HUMPOM849 | ssadra السَّدْرَ | fruit (3) seeds (2) | powder (4) decoction (1) | oral route (5) | DIGP (4) REND (1) | honey (4) | 5 | ||||
| Number | Percentage | Number | Percentage | |||||
|---|---|---|---|---|---|---|---|---|
| Plant prepared only | 42 | 31.11% | Monospecific recipes | 463 | 64.13% | |||
| Mixed plants | 93 | 68.89% | Recipes in the form of mixtures | ingredients of animal nature | 259 | 150 | 20.78% | 35.87% |
| vegetable ingredients | 59 | 8.17% | ||||||
| simply meals or beverages | 41 | 5.68% | ||||||
| swallowed with water | 9 | 1.25% | ||||||
| Total | 135 | 100% | 722 | 100 | ||||
| Category of Diseases | Symptom | NUR | NT | ICF |
|---|---|---|---|---|
| NUTI | analeptic; anemia; anorexia; appetizerappetizing; invigorating; obesity; refreshing; restorative; sliming; stimulating; strengthening; tiredeness; tonic | 68 | 42 | 0.39 |
| ALRP | allergy | 28 | 18 | 0.37 |
| CAN | cancer of various organs (stomach; lungliver; intestine, brain …) | 21 | 9 | 0.6 |
| CVP | aguainst palpitation; angina; arrythmia; warterosclerosis; cardiotonic; heart disease; syncope; tachocardia; hypertension; hypotensive | 26 | 15 | 0.44 |
| CHOD | hypercholesteremia | 16 | 15 | 0.07 |
| CIRP | bleeding; epistaxis; hemorroides; hemostatic; varicise veins | 23 | 18 | 0.23 |
| TOP | conjonctivitis; gengivitis; halitosis; odontorragie; scurvy; toothach | 5 | 4 | 0.25 |
| SKP | abscesses; acne; pruritus; aguainst freckles; aguainst itch; aguainstburns; alopecia; antifungal; antilice; antiscabis; astringeant; baldness; boils; burns; cellulite; chilblains; chope; cicatrization; dermatitis; eczema; injury; wound; itch; loss of hair; oedema; orbruise; parasitosis; pityriazis; pregnancy; pruritus; psoriasis; remove hair; repellent; ringworm; scabies; skin care; skin pimple; sunburn; swelling; vermin; vesicatory; vitiligo; vulnerary; warts; verruca; wound; wrinkless; parasitic skin; leishmanial | 51 | 27 | 0.48 |
| DIA | diabetes I and II | 31 | 18 | 0.43 |
| DIGP | abdominal pain; aerophagia; anthelmintic; antiacid; ascariasis; bilious care; bilious stimulation; bloating; carminatif; colic; constipation; delivery difficulties; diarrhea; emetic; enteritis; flotus; gastralgia; gastric scrubbing; gastric ulcers; gastritis; gastroenteritis; heartburn; helminthiasis; hepato biliary insufficiency; indigestin; intestinal winds; laxatif; liver disease; purgative; pyrosis, heatburn; spleen swelling; stomac pain; stomac ulcer or peptic ulcer; stomach ache; stomach ailment; swilling of the spleen; sytomacacidity; tanning; tenifuge; tonic; upset stomach; vomting; wormer | 132 | 56 | 0.58 |
| COLP | aguainst chill; calefacient; coldness; influenza; rheum | 47 | 27 | 0.43 |
| IFD | antirabic; bacterial infection; dysentery; gonorrhea; gonrrhea; hepatitis; icterusc; leprozy; measles; mumps; pertusis; rage, rabies, wrath; strengthensimmunity; trachoma; tuberculosis; typhoid; typhus; venereal disease; whoopingcaugh; antiparasitic; typhoïdes; syphilis | 15 | 10 | 0.36 |
| POI | antidote; antipoisonous; antitoxic; depurative; food poisoning; scorpion and snake bite | 8 | 7 | 0.14 |
| MAG | Magic | 23 | 13 | 0.45 |
| OPHP | ear ache; eye drops; eyes inflammation; ophtalmia | 7 | 6 | 0.17 |
| WAR | warmer | 34 | 22 | 0.36 |
| REND | bladder ailments; cystis; diuretic; enuresis; incontinence nocturne; kidney stones; lithiasis; oliguria; nephritic pain; nephritic pain; oliguria; hypouresis; prostate problems; urethritis | 33 | 20 | 0.41 |
| GOD | abortifacient; abortion; accouchement; aphrodisiac; chilbirth; cholagogue; dysmenorrhea; emenagogue; female infertility; frigidity; galactagogue; hypogalactie; lactation; leukorrhea; menstrual pains; menstrual pains; metrorrhagia; ovarial and menstrual pains | 58 | 35 | 0.4 |
| RESP | antitussif; asthma; bad breath; chespain; lung disorder; rhinosinusitis; sinusitis; sternitatory | 12 | 7 | 0.45 |
| RHA | arthrisis; arthrosis; bon care; gout; lumbago; muscle aches; ossification; osteoarthrite; rheumatic pain; rheumatoid arthritis; sciatica; strain; twist; wrech; rick; swelling; dislocation | 14 | 11 | 0.23 |
| NSD | amnesia; analgesic; anxiety; astonishing; epilepsy, epileptic; hypnotic; melancholy; narcotic; nervousness; neuralgia; neurosedative; overwork; sedative; tremor in the elderly | 56 | 27 | 0.53 |
| HEAD | cephalgia; cephalus; headache; migraine | 14 | 8 | 0.46 |
| Name of Letter | Symbol | Transliteration | Name of Letter | Symbol | Transliteration |
|---|---|---|---|---|---|
| alif | ا | â | ḍâd | ض | ḍ |
| bâ | ب | b | ṭâ | ط | ṭ |
| tâ | ت | t | ظ | ||
| ṯâ | ث | ṯ | ayn | ع | ‘ |
| jîm | ج | j | ġayn | غ | ġ |
| ḥâ | ح | ḥ | fâ | ف | f |
| ḵâ | خ | ḵ | qâf | ق | q |
| dâl | د | d | kâf | ك | k |
| ḍâl | ذ | ḍ | lâm | ل | l |
| râ | ر | r | mîm | م | m |
| zâ | ز | z | nûn | ن | n |
| sîn | س | s | hâ | ه | h |
| šîn | ش | š | wâw | و | û |
| ṣâd | ص | ṣ | yâ | ي | î |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fakchich, J.; Kharchoufa, L.; Bencheikh, N.; Zerkani, H.; Ouassou, H.; Bouhrim, M.; Cordero, M.A.W.; Alotaibi, A.; Elachouri, M. Assessment of Indigenous Plants Knowledge among Traditional Healers in Eastern Morocco: Quali-Quantitative Approach (Part I). Appl. Sci. 2022, 12, 12773. https://doi.org/10.3390/app122412773
Fakchich J, Kharchoufa L, Bencheikh N, Zerkani H, Ouassou H, Bouhrim M, Cordero MAW, Alotaibi A, Elachouri M. Assessment of Indigenous Plants Knowledge among Traditional Healers in Eastern Morocco: Quali-Quantitative Approach (Part I). Applied Sciences. 2022; 12(24):12773. https://doi.org/10.3390/app122412773
Chicago/Turabian StyleFakchich, Jamila, Loubna Kharchoufa, Noureddine Bencheikh, Hannou Zerkani, Hayat Ouassou, Mohamed Bouhrim, Mary Anne W. Cordero, Amal Alotaibi, and Mostafa Elachouri. 2022. "Assessment of Indigenous Plants Knowledge among Traditional Healers in Eastern Morocco: Quali-Quantitative Approach (Part I)" Applied Sciences 12, no. 24: 12773. https://doi.org/10.3390/app122412773
APA StyleFakchich, J., Kharchoufa, L., Bencheikh, N., Zerkani, H., Ouassou, H., Bouhrim, M., Cordero, M. A. W., Alotaibi, A., & Elachouri, M. (2022). Assessment of Indigenous Plants Knowledge among Traditional Healers in Eastern Morocco: Quali-Quantitative Approach (Part I). Applied Sciences, 12(24), 12773. https://doi.org/10.3390/app122412773








