Novel Instrument for Clinical Evaluations of Active Extraocular Muscle Tension
Abstract
1. Introduction
2. Materials and Methods
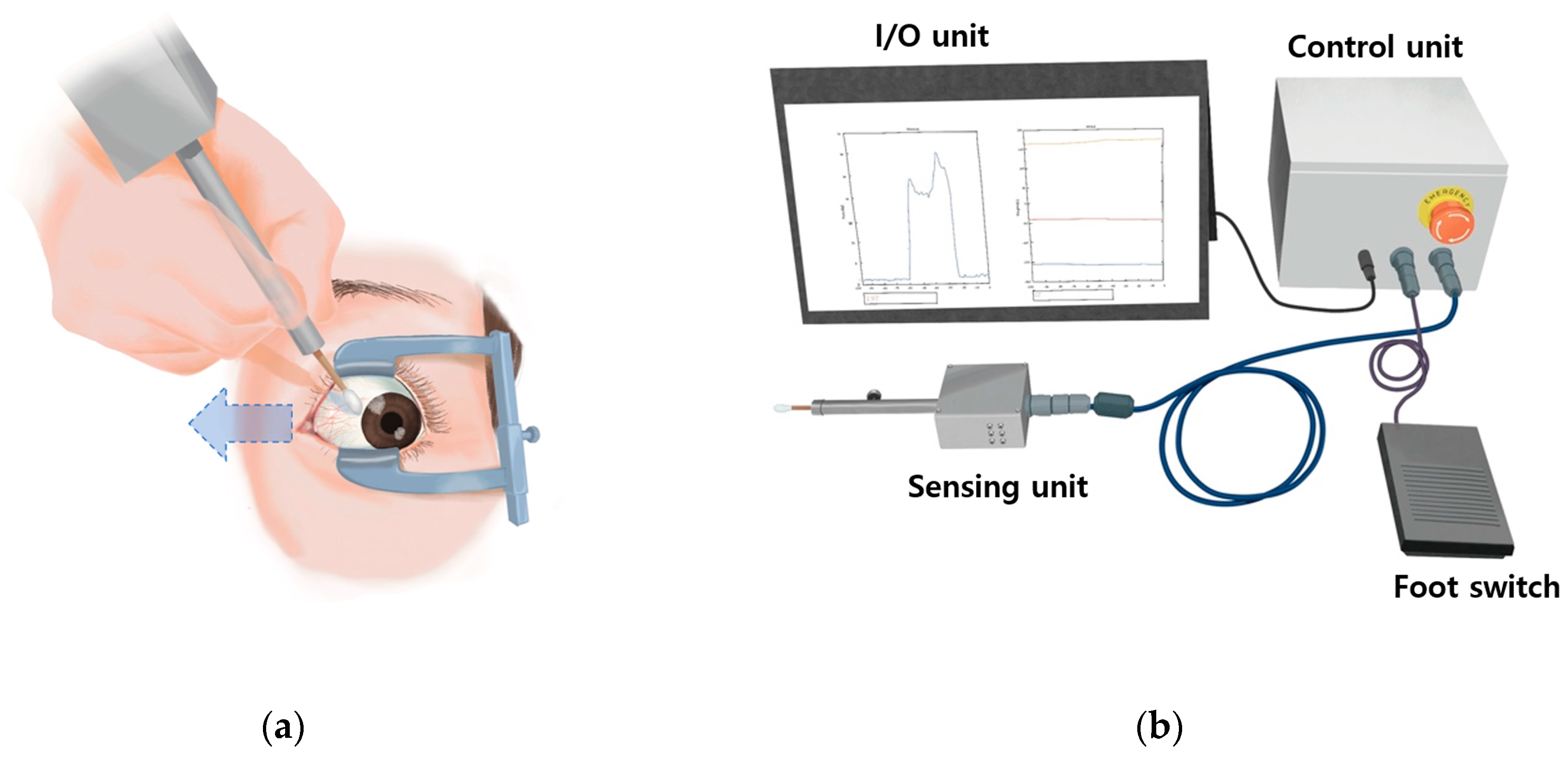
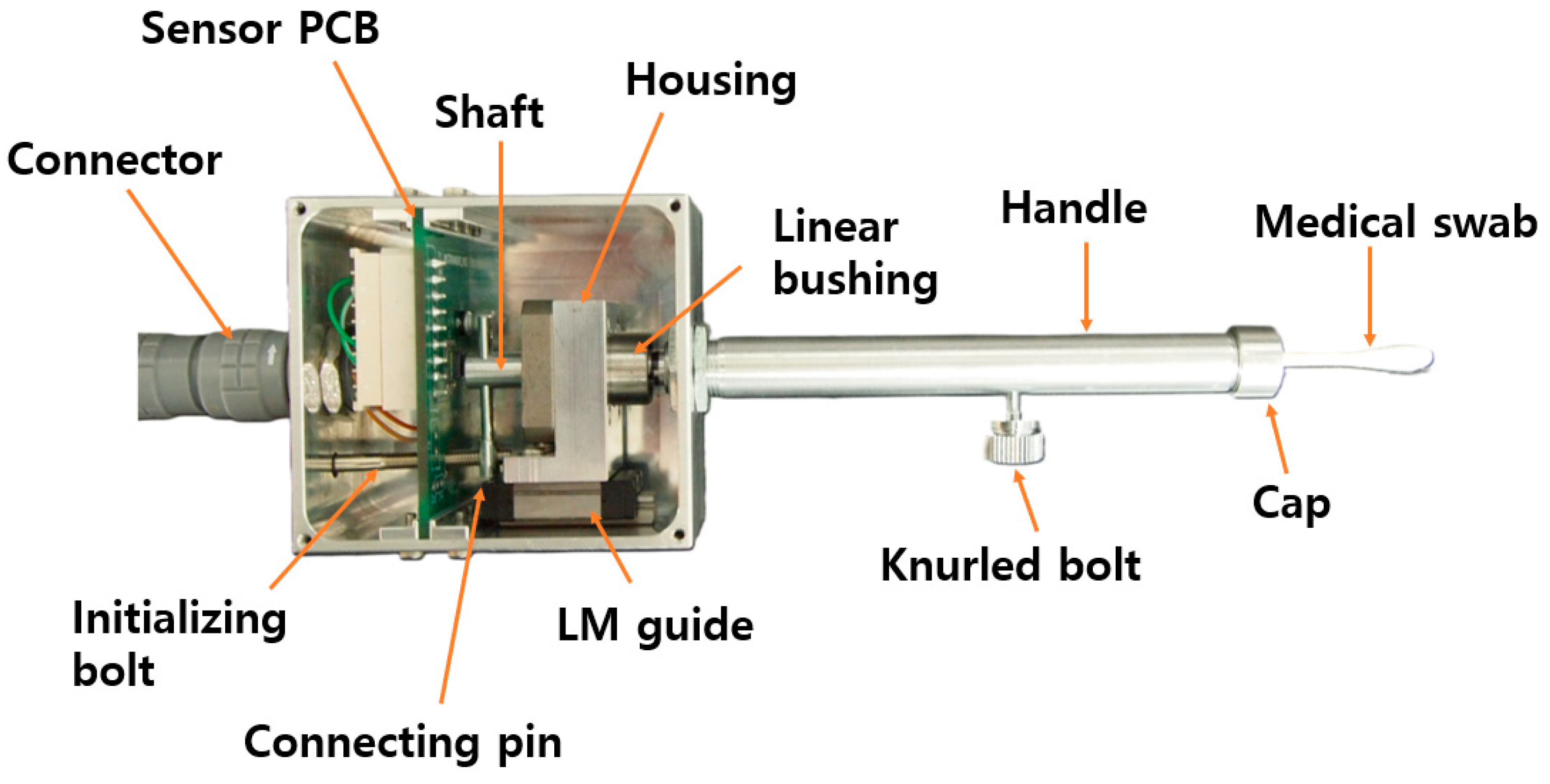
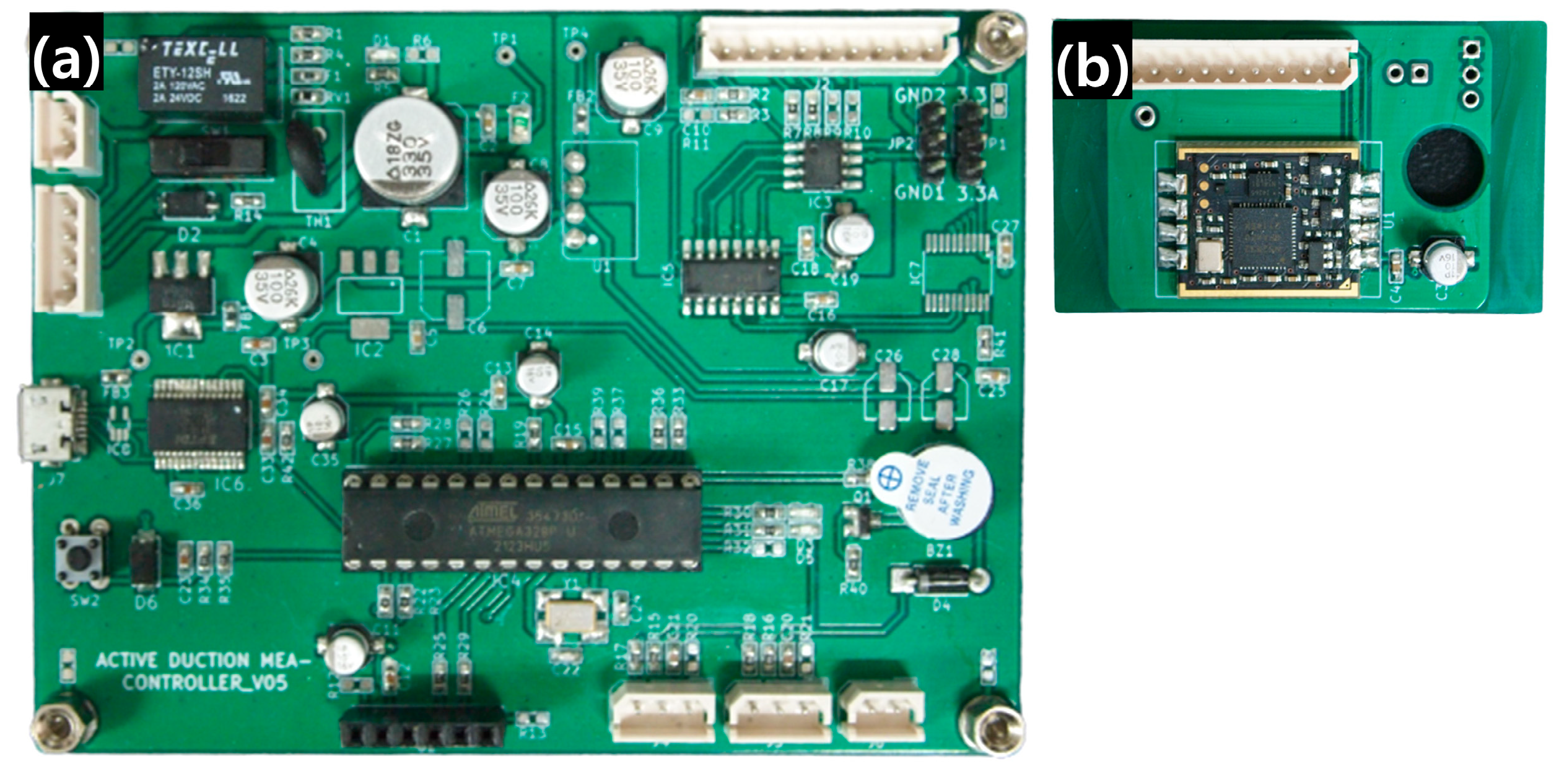
2.1. Design of Active EOM Tension Measuring Device
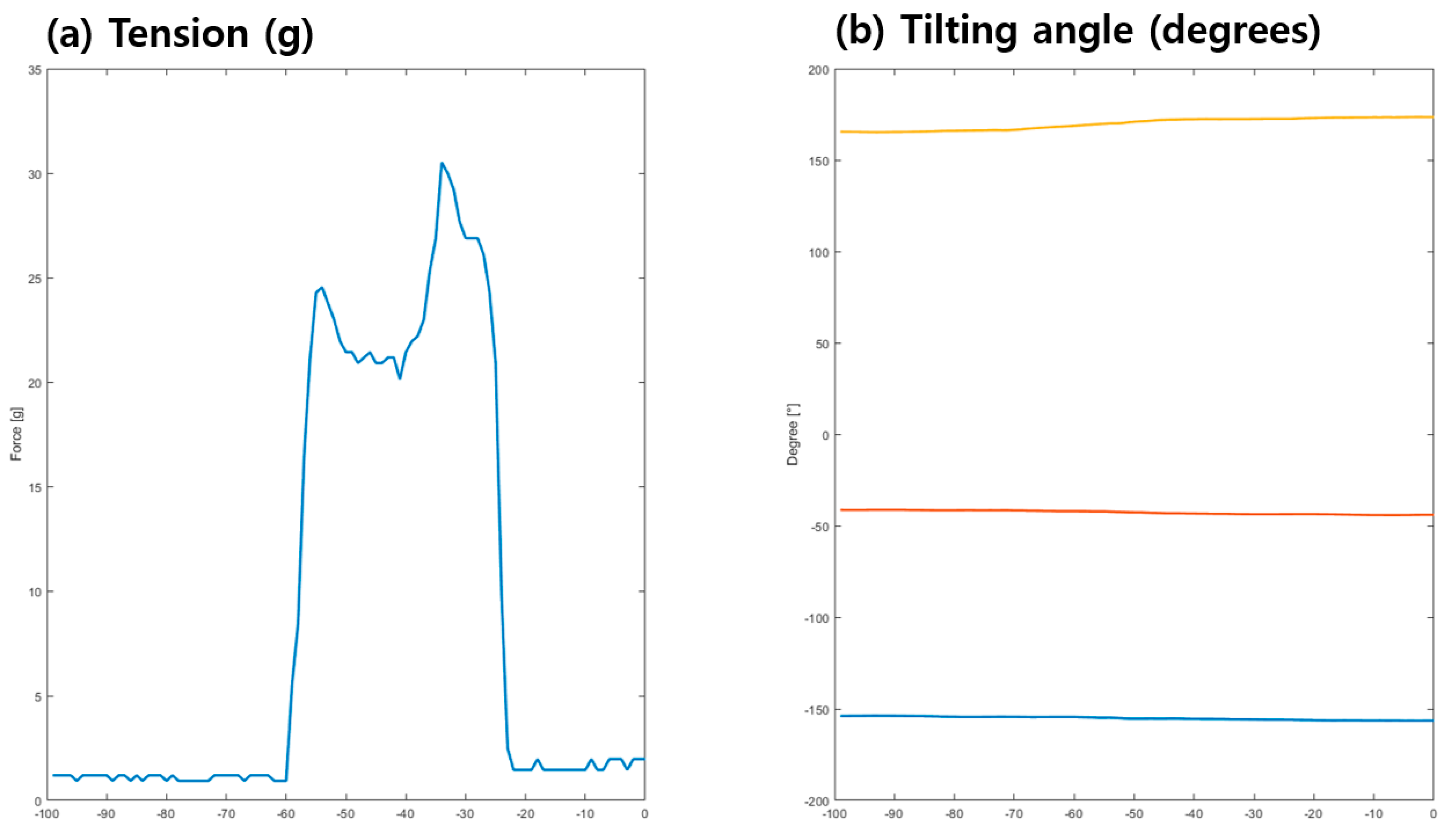
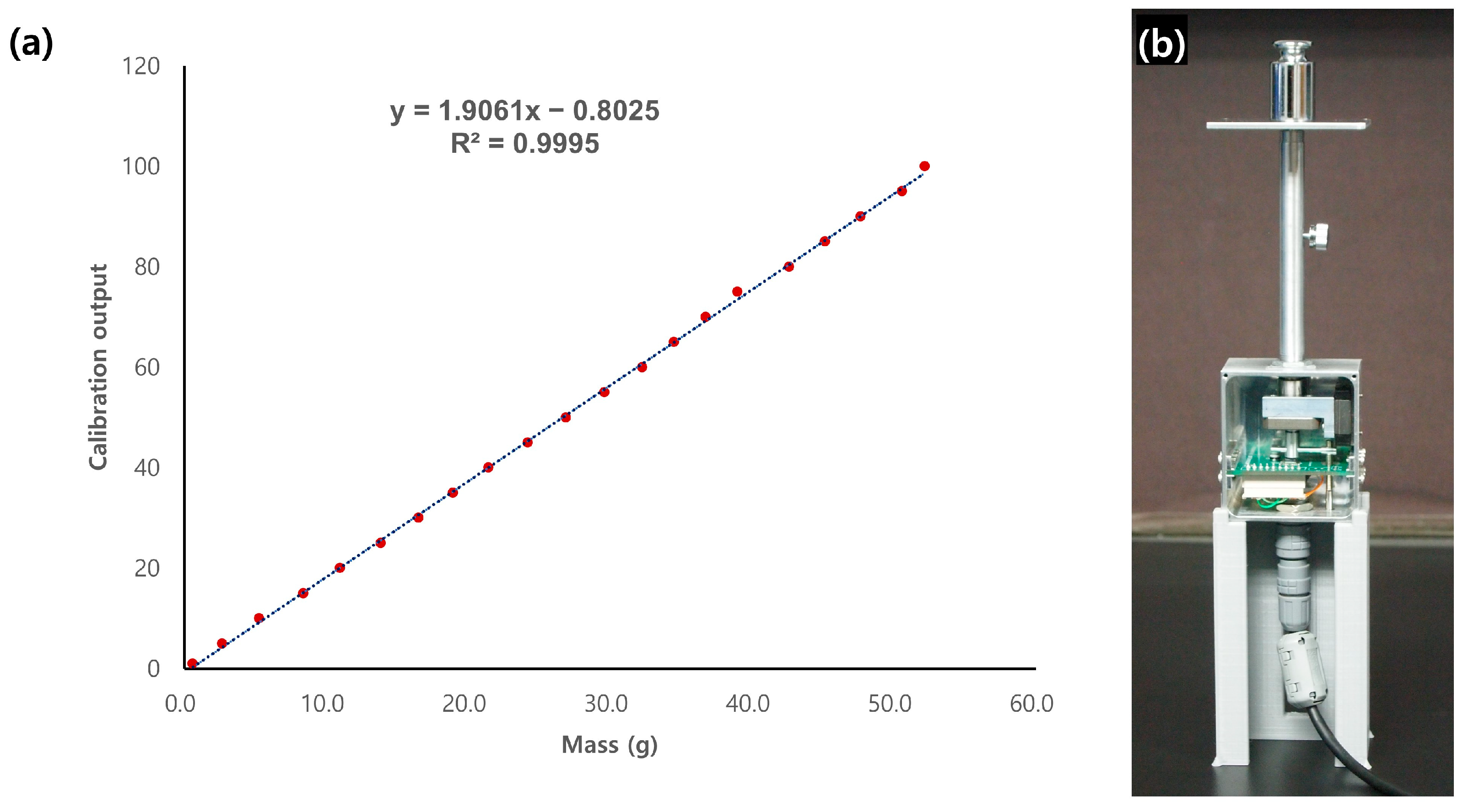
2.2. Structural Analysis and Calibration
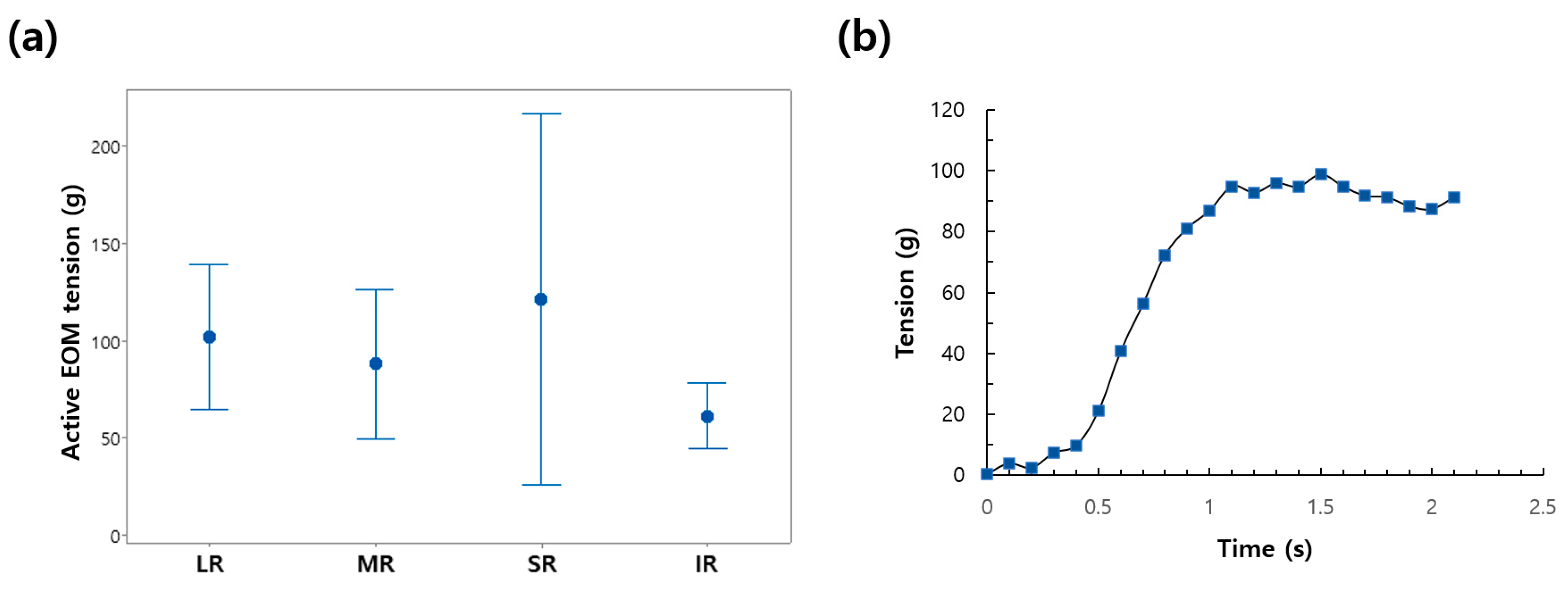
3. Results
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lennerstrand, G. Strabismus and sensory-motor function of eye muscles. J. Integr. Neurosci. 2005, 48, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Lennerstrand, G. Strabismus and eye muscle function. Acta Ophthalmol. Scand. 2007, 85, 711–723. [Google Scholar] [CrossRef] [PubMed]
- Gauthier, G.M.; Nommay, D.; Vercher, J.-L. The role of ocular muscle proprioception in visual localization of targets. Science 1990, 249, 58–61. [Google Scholar] [CrossRef]
- Franzblau, S.C. The diagnosis of amblyopia and strabismus: A programmed approach. J. Am. Optom. Assoc. 1977, 48, 1248–1257. [Google Scholar] [PubMed]
- Carlton, J.; Kaltenthaler, E. Health-related quality of life measures (HRQoL) in patients with amblyopia and strabismus: A systematic review. Br. J. Ophthalmol. 2011, 95, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.H.; Rah, S.H. The Clinical Course of Consecutive Esotropia after Surgical Correction. Korean J. Ophthalmol. 2007, 21, 228–231. [Google Scholar] [CrossRef]
- Baik, D.J.; Ha, S.G.; Kim, S.H. Clinical Manifestations of Delayed-onset Consecutive Esotropia after Surgical Correction of Intermittent Exotropia. Korean J. Ophthalmol. 2020, 34, 121–125. [Google Scholar] [CrossRef][Green Version]
- Lekskul, A.; Supakitvilekarn, T.; Padungkiatsagul, T. Outcomes of undercorrection in surgical management and binocular vision gained of adult intermittent exotropia. Clin. Ophthalmol. 2018, 12, 1763–1767. [Google Scholar] [CrossRef]
- Kushner, B.J.; Vrabec, M. Theoretical effects of surgery on length tension relationships in extraocular muscles. J. Pediatr. Ophthalmol. Strabismus 1987, 24, 126–131. [Google Scholar] [CrossRef]
- Jung, J.H.; Holmes, J.M. Quantitative Intraoperative Torsional Forced Duction Test. Ophthalmology 2015, 122, 1932–1938. [Google Scholar] [CrossRef][Green Version]
- Shin, H.J.; Lee, S.J.; Oh, C.S.; Kang, H. Novel compact device for clinically measuring extraocular muscle (EOM) tension. J. Biomech. 2020, 109, 109955. [Google Scholar] [CrossRef] [PubMed]
- Metz, H.S. Forced duction, active force generation, and saccadic velocity tests. Int. Ophthalmol. Clin. 1976, 16, 47–73. [Google Scholar] [CrossRef] [PubMed]
- Scott, A.B.; Collins, C.C.; O’Meara, D.M. A Forceps to Measure Strabismus Forces. Arch. Ophthalmol. 1972, 88, 330–333. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Yang, H.K.; Hwang, J.M. Surgical outcomes of unilateral recession and resection in intermittent exotropia according to forced duction test results. PLoS ONE 2018, 13, e0200741. [Google Scholar] [CrossRef]
- Collins, C.C.; Carlson, M.R.; Scott, A.B.; Jampolsky, A. Extraocular muscle forces in normal human subjects. Investig. Ophthalmol. Vis. Sci. 1981, 20, 652–664. [Google Scholar]
- Lennerstrand, G.; Schiavi, C.; Tian, S.; Benassi, M.; Campos, E.C. Isometric force measured in human horizontal eye muscles attached to or detached from the globe. Graefes Arch. Clin. Exp. Ophthalmol. 2006, 244, 539–544. [Google Scholar] [CrossRef]
- Kang, H.; Lee, S.H.; Shin, H.J.; Lee, A.G. New instrument for quantitative measurements of passive duction forces and its clinical implications. Graefes Arch. Clin. Exp. Ophthalmol. 2020, 258, 2841–2848. [Google Scholar] [CrossRef]
- Kang, H.; Lee, S.H.; Oh, C.S.; Shin, H.J.; Lee, A.G. Quantitative measurement of passive duction force tension in intermittent exotropia and its clinical implications. Graefes Arch. Clin. Exp. Ophthalmol. 2021, 259, 1617–1623. [Google Scholar] [CrossRef]
- Kang, H.; Shin, H.J.; Lee, A.G. Risk of consecutive esotropia after surgery for intermittent exotropia according to passive duction force. PLoS ONE 2023, 18, e0281392. [Google Scholar] [CrossRef]
- Amann, P.; Nicolay, P.; Chatziioannou, V.; Willmann, R. A “digital mouthpiece” for the autonomous analysis and improvement of brass musician performances. Proc. Mtgs. Acoust. 2022, 49, 035022. [Google Scholar] [CrossRef]
- Park, J.; Kim, J.; Kim, D.H.; Hwang, J.; Kim, Y.G.; Hyung, S.Y.; Ko, S.-H.; Lee, M. Design of a Soft Wearable Passive Fitness Device for Upper Limb Resistance Exercise. In Proceedings of the 2022 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Kyoto, Japan, 23–27 October 2022; pp. 8488–8493. [Google Scholar] [CrossRef]
- Caruso, M.; Miceli, R.; Romano, P.; Schettino, G.; Spataro, C.; Viola, F. A low-cost, real-time monitoring system for PV plants based on ATmega 328P-PU microcontroller. In Proceedings of the 2015 IEEE International Telecommunications Energy Conference (INTELEC), Osaka, Japan, 18–22 October 2015; pp. 1–5. [Google Scholar] [CrossRef]
- Mori, G.N.; Swaminarayan, P.R. Measuring IoT Security Issues and Control Home Lighting System by Android Application Using Arduino Uno and HC-05 Bluetooth Module. In Data Science and Intelligent Applications; Kotecha, K., Piuri, V., Shah, H., Patel, R., Eds.; Lecture Notes on Data Engineering and Communications Technologies; Springer: Singapore, 2021; Volume 52, pp. 375–382. [Google Scholar] [CrossRef]
- Xia, Z.; Wang, Q.; Liu, Q.; Wang, Y.; Liu, J.; Chen, G. A novel approach for automatic reconstruction of boundary condition in structure analysis. Adv. Eng. Softw. 2016, 96, 38–57. [Google Scholar] [CrossRef]
- Beer, G.; Duenser, C. Advanced Boundary Element analysis of geotechnical problems with geological inclusions. Comput. Geotech. 2016, 79, 86–95. [Google Scholar] [CrossRef]
- Zhou, N.; He, M. The finite element analysis of a three-story light wood-framed building. In Proceedings of the 2011 International Conference on Business Management and Electronic Information, Guangzhou, China, 13–15 May 2011; pp. 763–767. [Google Scholar] [CrossRef]
- Luo, Z.; Yu, L. PSO-based sparse regularization approach for structural damage detection. In Proceedings of the 2017 13th International Conference on Natural Computation, Fuzzy Systems and Knowledge Discovery (ICNC-FSKD), Guilin, China, 29–31 July 2017; pp. 1033–1039. [Google Scholar] [CrossRef]
- Flórez, J.A.; Velásquez, A. Calibration of force sensing resistors (fsr) for static and dynamic applications. In Proceedings of the 2010 IEEE ANDESCON, Bogota, Colombia, 15–17 September 2010; pp. 1–6. [Google Scholar] [CrossRef]
- Zhou, H.; Zeng, Z. A Fitting Method of the Temperature Characteristic Curve of Sensor. In Proceedings of the 2009 5th International Conference on Wireless Communications, Networking and Mobile Computing, Beijing, China, 24–26 September 2009; pp. 1–4. [Google Scholar] [CrossRef]
- Jebli, I.; Belouadha, F.-Z.; Kabbaj, M.I.; Tilioua, A. Prediction of solar energy guided by pearson correlation using machine learning. Energy 2021, 224, 120109. [Google Scholar] [CrossRef]
- Lennerstrand, G.; Bolzani, R.; Benassi, M.; Tian, S.; Schiavi, C. Isometric force development in human horizontal eye muscles and pulleys during saccadic eye movements. Acta Ophthalmol. 2009, 87, 837–842. [Google Scholar] [CrossRef] [PubMed]


| Conventional Force Generation Test | Novel Device in the Current Study | |
|---|---|---|
| Technique | Active force felt with the forceps or cotton tip | Load cell (force transducer) used to measure pushing force of cotton tip |
| Sensing unit | Hand of examiner | Electro-mechanical sensor |
| Accuracy | May yield less precise results due to subjective factors | Offers higher precision and accuracy in tension measurement |
| Data collection | Requires manual recording and analysis, potentially introducing human error | Automated continuous data collection reduces the risk of human error |
| Interpretation | Subjective | Objective |
| Inter-examiner variability | Highly variable | Less variable |
| Feedback | Limited ability to assess muscle active muscle tension dynamically | Enables dynamic assessment of active muscle tension, aiding in treatment optimization |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, H.J.; Kim, S.; Kang, H.; Lee, A.G. Novel Instrument for Clinical Evaluations of Active Extraocular Muscle Tension. Appl. Sci. 2023, 13, 11431. https://doi.org/10.3390/app132011431
Shin HJ, Kim S, Kang H, Lee AG. Novel Instrument for Clinical Evaluations of Active Extraocular Muscle Tension. Applied Sciences. 2023; 13(20):11431. https://doi.org/10.3390/app132011431
Chicago/Turabian StyleShin, Hyun Jin, Seokjin Kim, Hyunkyoo Kang, and Andrew G. Lee. 2023. "Novel Instrument for Clinical Evaluations of Active Extraocular Muscle Tension" Applied Sciences 13, no. 20: 11431. https://doi.org/10.3390/app132011431
APA StyleShin, H. J., Kim, S., Kang, H., & Lee, A. G. (2023). Novel Instrument for Clinical Evaluations of Active Extraocular Muscle Tension. Applied Sciences, 13(20), 11431. https://doi.org/10.3390/app132011431







