Potentilla paradoxa Nutt. Ethanol Extract Exhibits Anti-Inflammatory Effects by Suppression of the Src/NF-κB Signaling Pathway
Abstract
:1. Introduction
2. Results
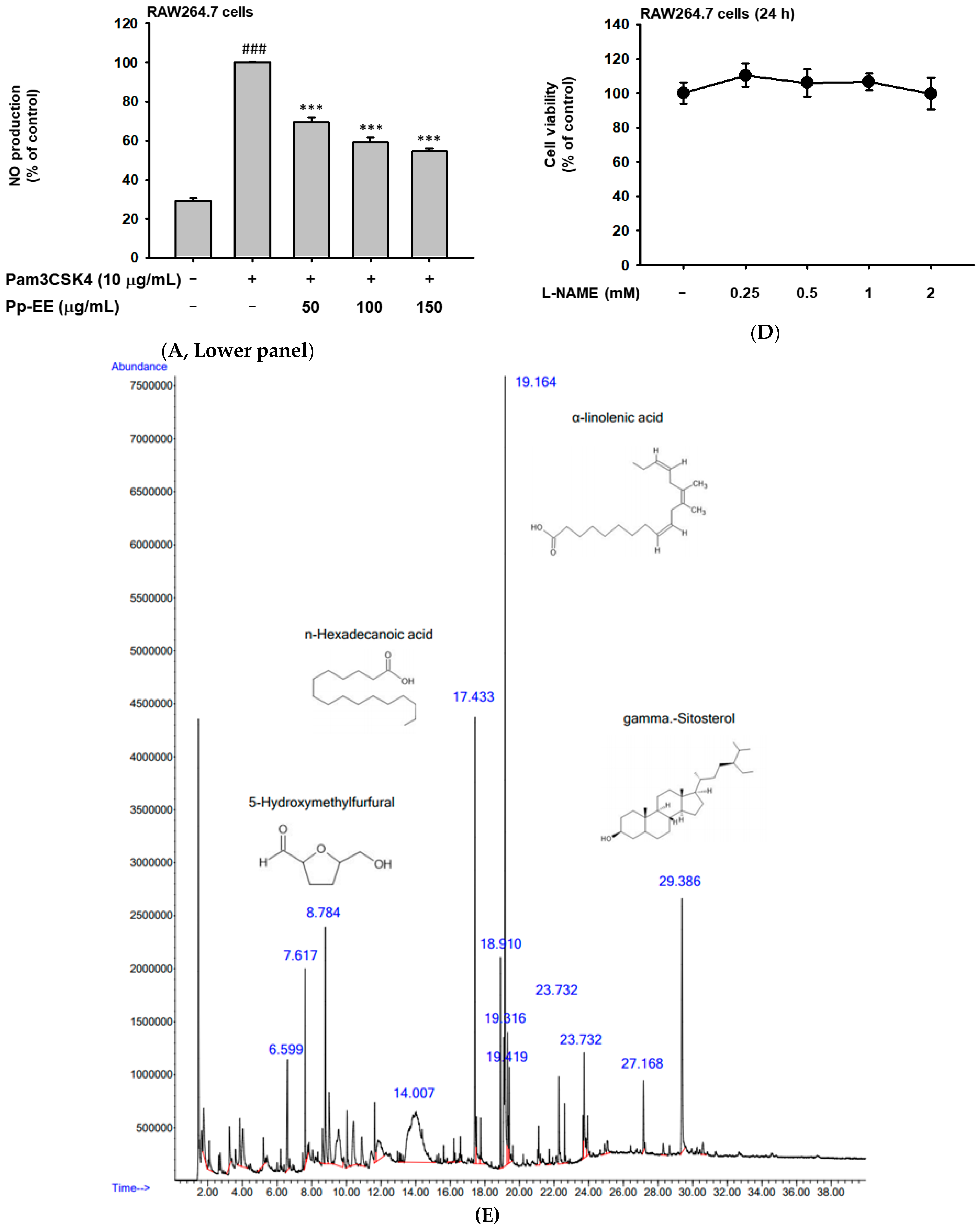
2.1. Pp-EE Suppressed the NO Production Level and Phytochemical Components in Pp-EE
2.2. Inhibitory Effect of Pp-EE on Inflammatory Gene Expression and Transcription Factors
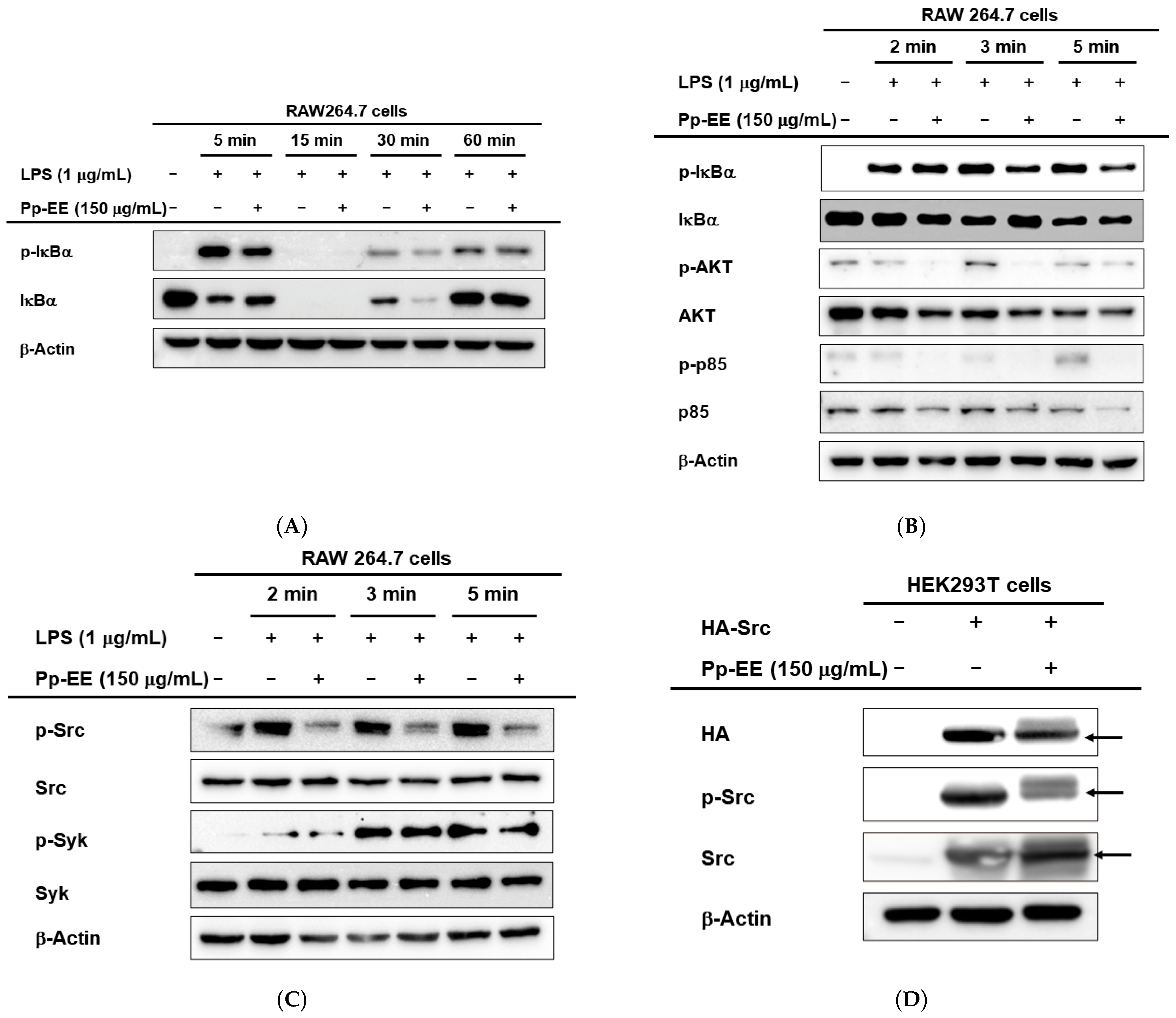
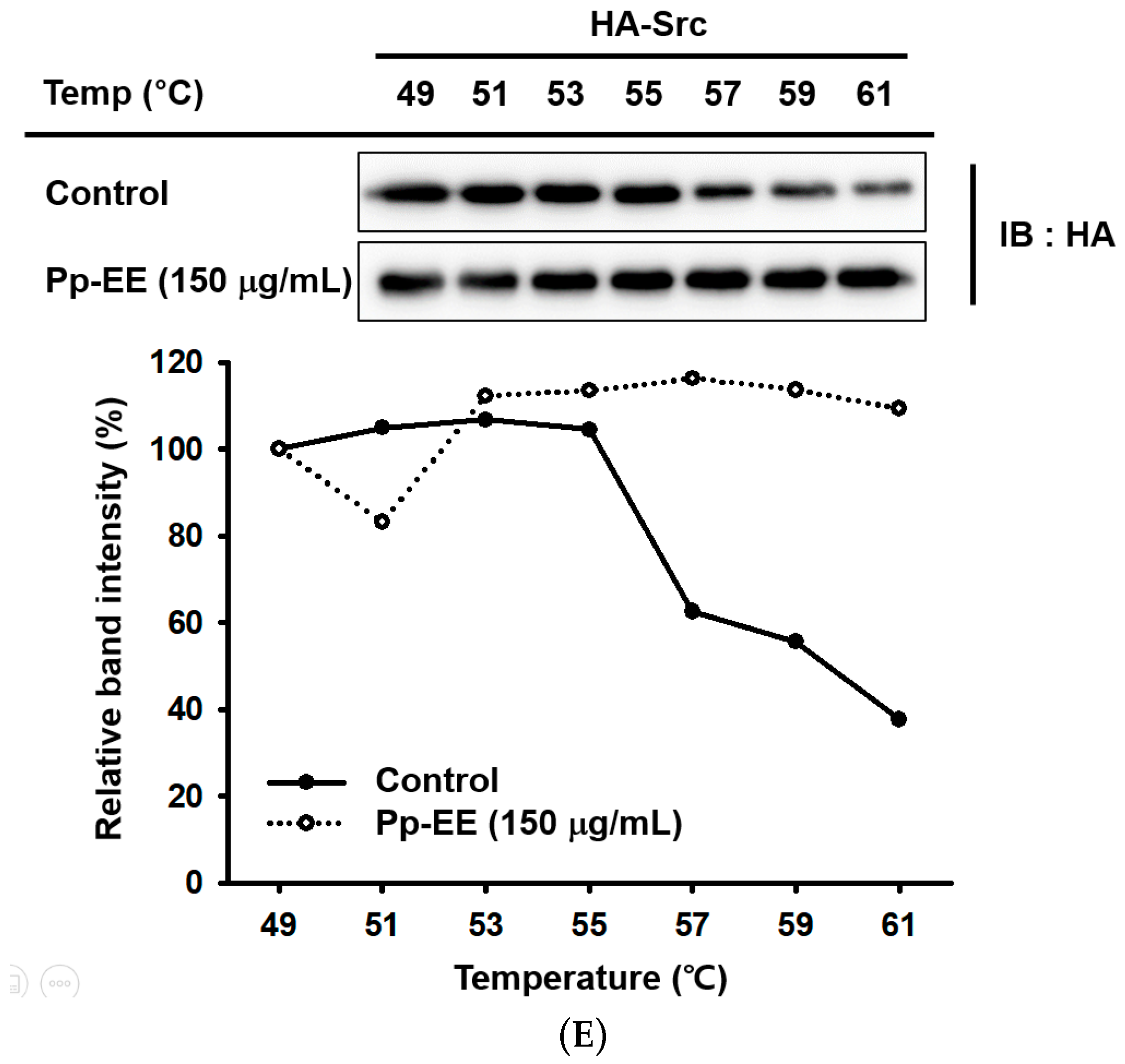
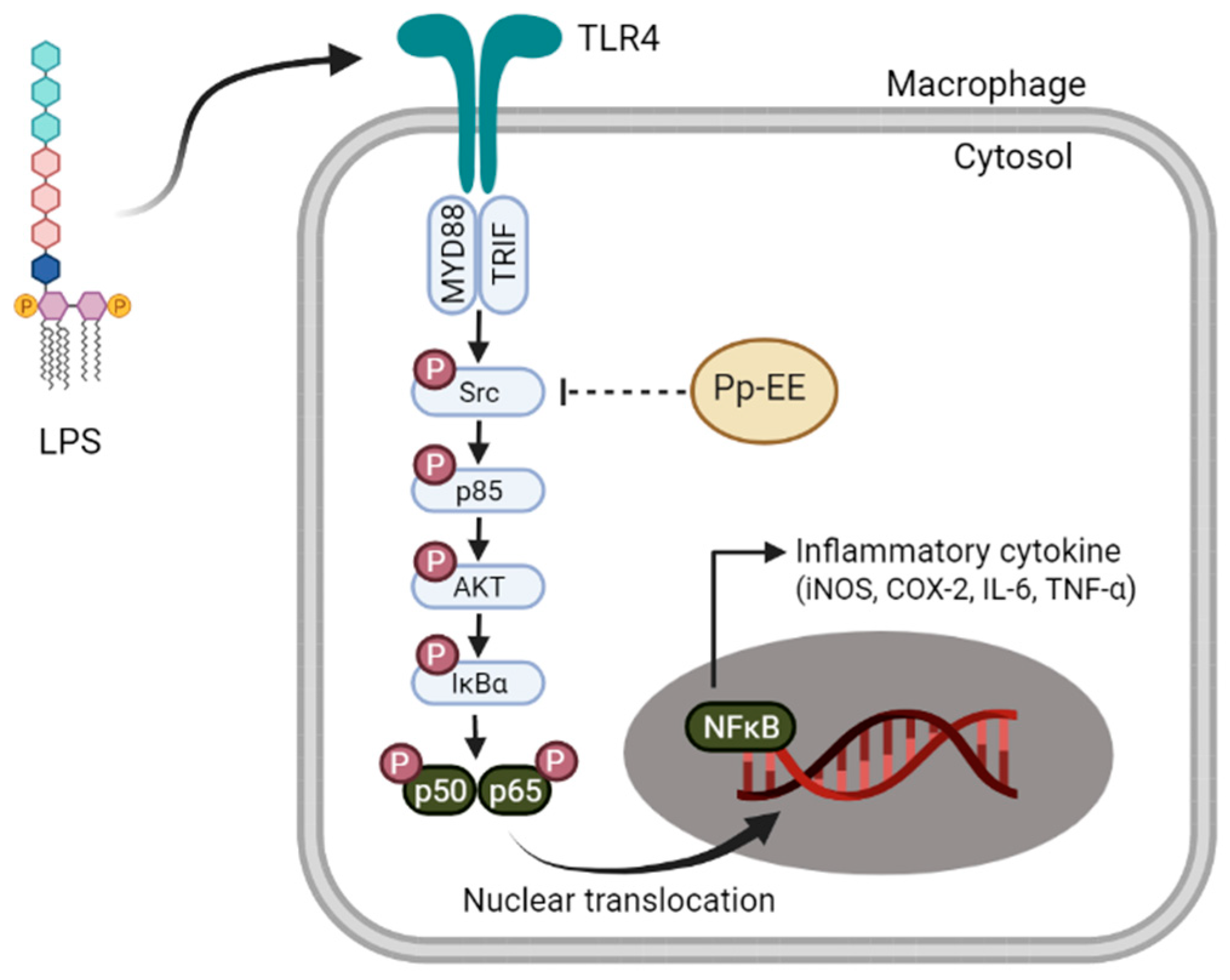
2.3. Pp-EE Inhibits Phosphorylation of Src in the NFκB Signaling Pathway
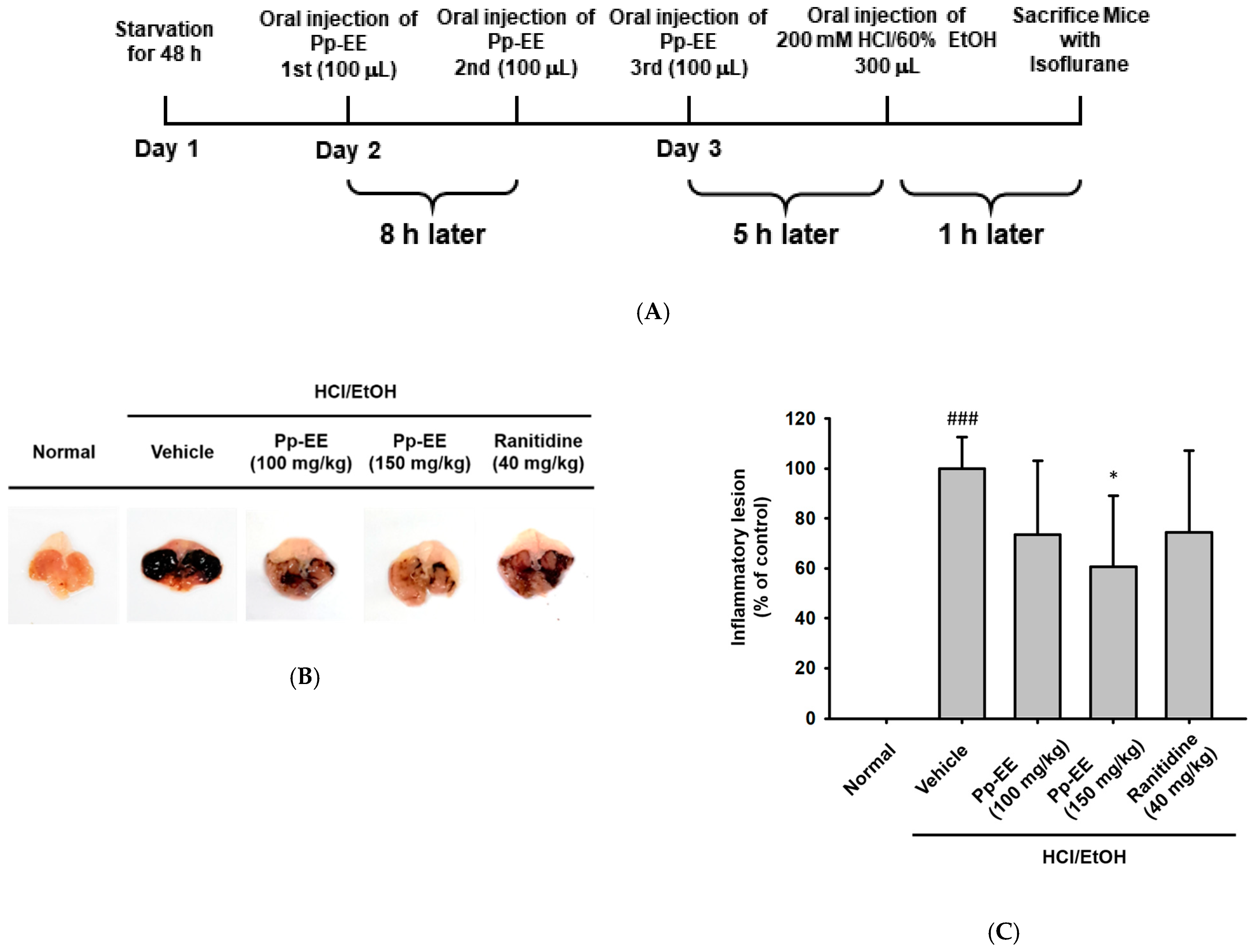
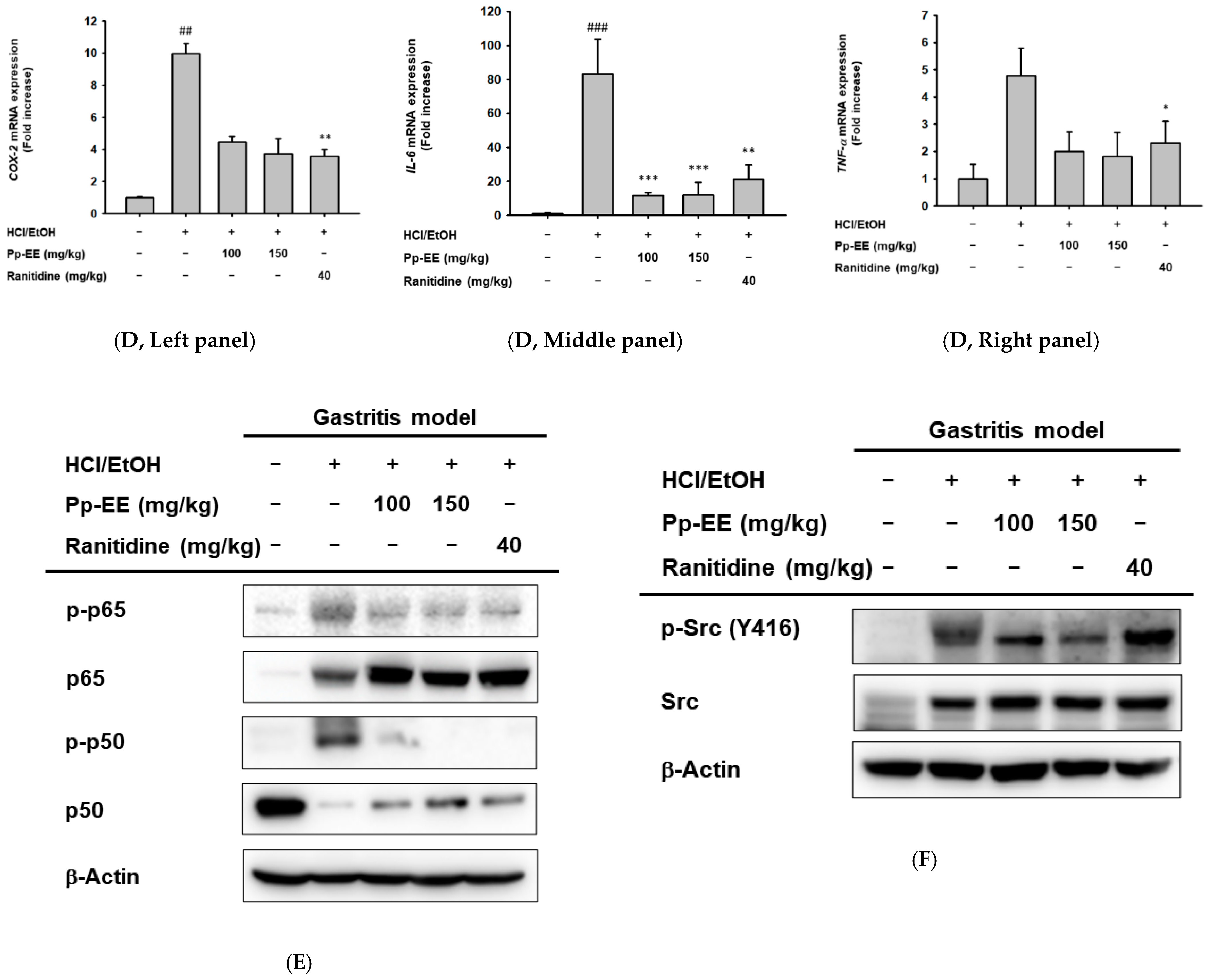
2.4. Effects of Pp-EE on an HCl/EtOH-Induced Gastritis Model
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Preparation of Pp-EE and Its Treatment
4.3. Cell Culture
4.4. Nitric Oxide (NO) Production Assay
4.5. Cell Viability
4.6. Gas Chromatography–Mass Spectrometry (GC–MS/MS)
4.7. mRNA Expression Level Analysis by Semi-Quantitative Reverse Transcriptase–PCR and Quantitative Real-Time PCR
4.8. Plasmid Transfection and Luciferase Reporter Gene Activity Assay
4.9. Whole Lysate Preparation and Western Blotting Assay
4.10. Cellular Thermal Shift Assay (CETSA)
4.11. Animals
4.12. EtOH/HCl-Induced Gastritis Mouse Model
4.13. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AP-1 | Activator protein-1 |
| COX-2 | Cyclooxygenase-2 |
| HA | Haemagglutanin |
| iNOS | Inducible nitric oxide synthase |
| IκBα | Inhibitor of kappa B alpha |
| IL-1β | Interleukin-1β |
| IL-6 | Interleukin 6 |
| MyD88 | Myeloid differentiation primary response 88 |
| NO | Nitric oxide |
| p85 | Phosphoinositide-3-kinase p85 |
| Pp-EE | Potentilla paradoxa Nutt. Ethanol extract |
| LPS | Lipopolysaccharide |
| NF-κB | Nuclear factor-κB |
| TRIF | TIR-domain-containing adapter-inducing interferon-β |
| TNF- | Tumor necrosis factor-alphaα |
References
- Ratan, Z.A.; Youn, S.H.; Kwak, Y.S.; Han, C.K.; Haidere, M.F.; Kim, J.K.; Min, H.; Jung, Y.J.; Hosseinzadeh, H.; Hyun, S.H.; et al. Adaptogenic effects of Panax ginseng on modulation of immune functions. J. Ginseng Res. 2021, 45, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Turner, M.D.; Nedjai, B.; Hurst, T.; Pennington, D.J. Cytokines and chemokines: At the crossroads of cell signalling andinflammatory disease. Biochim. Biophys. Acta 2014, 1834, 2563–2582. [Google Scholar] [CrossRef] [Green Version]
- Ferrero-Miliani, L.; Nielsen, O.H.; Andersen, P.S.; Girardin, S.E. Chronic inflammation: Importance of NOD2 and NALP3 in interleukin-1β generation. Clin. Exp. Immunol. 2007, 147, 227–235. [Google Scholar] [CrossRef]
- Ratan, Z.A.; Haidere, M.F.; Hong, Y.H.; Park, S.H.; Lee, J.O.; Lee, J.; Cho, J.Y. Pharmacological potential of ginseng and its major component ginsenosides. J. Ginseng Res. 2021, 45, 199–210. [Google Scholar] [CrossRef] [PubMed]
- Furman, D.; Campisi, J.; Verdin, E.; Carrera-Bastos, P.; Targ, S.; Franceschi, C.; Ferrucci, L.; Gilroy, D.W.; Fasano, A.; Miller, G.W.; et al. Chronic inflammation in the etiology of disease across the life span. Nat. Med. 2019, 25, 1822–1832. [Google Scholar] [CrossRef] [PubMed]
- Xue, Q.; He, N.; Wang, Z.; Fu, X.; Aung, L.H.H.; Liu, Y.; Li, M.; Cho, J.Y.; Yang, Y.; Yu, T. Functional roles and mechanisms of ginsenosides from Panax ginseng in atherosclerosis. J. Ginseng Res. 2021, 45, 22–31. [Google Scholar] [CrossRef]
- Shen-Orr, S.S.; Furman, D.; Kidd, B.A.; Hadad, F.; Lovelace, P.; Huang, Y.-W.; Rosenberg-Hasson, Y.; Mackey, S.; Gratemah, F.A.G.; Pickman, Y.; et al. Defective signaling in the JAK-STAT pathway tracks with chronic inflammation and cardiovascular risk in aging humans. Cell Syst. 2016, 3, 374–384.e374. [Google Scholar] [CrossRef] [Green Version]
- Fourati, S.; Cristescu, R.; Loboda, A.; Talla, A.; Filali, A.; Railkar, R.; Schaeffer, A.K.; Favre, D.; Gagnon, D.; Peretz, Y.; et al. Pre-vaccination inflammation and B-cell signalling predict age-related hyporesponse to hepatitis B vaccination. Nat. Commun. 2016, 7, 10369. [Google Scholar] [CrossRef]
- Verschoor, C.P.; Lelic, A.; Parsons, R.; Evelegh, C.; Bramson, J.L.; Johnstone, J.; Loeb, M.B.; Bowdish, D.M.E. Serum C-reactive protein and congestive heart failure as significant predictors of herpes Zoster vaccine response in elderly nursing home residents. J. Infect. Dis. 2017, 216, 191–197. [Google Scholar] [CrossRef] [Green Version]
- McDade, T.W.; Adair, L.; Feranil, A.B.; Kuzawa, C. Positive antibody response to vaccination in adolescence predicts lower C-reactive protein concentration in young adulthood in the philippines. Am. J. Hum. Biol. 2011, 23, 313–318. [Google Scholar] [CrossRef] [Green Version]
- Akira, S.; Uematsu, S.; Takeuchi, O. Pathogen recognition and innate immunity. Cell 2006, 124, 783–801. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawasaki, T.; Kawai, T. Toll-like receptor signaling pathways. Front. Immunol. 2014, 5, 461. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flynn, D.C. Adaptor proteins. Oncogene 2001, 20, 6270–6272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, J.K.; Shin, K.K.; Kim, H.; Hong, Y.H.; Choi, W.; Kwak, Y.S.; Han, C.K.; Hyun, S.H.; Cho, J.Y. Korean Red Ginseng exerts anti-inflammatory and autophagy-promoting activities in aged mice. J. Ginseng Res. 2021, 45, 717–725. [Google Scholar] [CrossRef] [PubMed]
- Granado-Serrano, A.B.; Martín, M.A.; Haegeman, G.; Goya, L.; Bravo, L.; Ramos, S. Epicatechin induces NF-κB, activator protein-1 (AP-1) and nuclear transcription factor erythroid 2p45-related factor-2 (Nrf2) via phosphatidylinositol-3-kinase/protein kinase B (PI3K/AKT) and extracellular regulated kinase (ERK) signalling in HepG2 cells. Br. J. Nutr. 2010, 103, 168–179. [Google Scholar] [CrossRef] [Green Version]
- Khalaf, H.; Jass, J.; Olsson, P.-E. Differential cytokine regulation by NF-κB and AP-1 in Jurkat T-cells. BMC Immunol. 2010, 11, 26. [Google Scholar] [CrossRef] [Green Version]
- Byeon, S.E.; Yi, Y.-S.; Oh, J.; Yoo, B.C.; Hong, S.; Cho, J.Y. The role of Src kinase in macrophage-mediated inflammatory responses. Mediat. Inflamm. 2012, 2012, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.O.; Hwang, S.H.; Shen, T.; Kim, J.H.; You, L.; Hu, W.; Cho, J.Y. Enhancement of skin barrier and hydration-related molecules by protopanaxatriol in human keratinocytes. J. Ginseng Res. 2021, 45, 354–360. [Google Scholar] [CrossRef]
- Tang, C.H.; Hsu, C.J.; Yang, W.H.; Fong, Y.C. Lipoteichoic acid enhances IL-6 production in human synovial fibroblasts via TLR2 receptor, PKCδ and c-Src dependent pathways. Biochem. Pharmacol. 2010, 79, 1648–1657. [Google Scholar] [CrossRef]
- Chen, Y.-J.; Hsieh, M.-Y.; Chang, M.Y.; Chen, H.-C.; Jan, M.-S.; Maa, M.-C.; Leu, T.-H. Eps8 protein facilitates phagocytosis by increasing TLR4-MyD88 protein interaction in lipopolysaccharide-stimulated macrophages. J. Biol. Chem. 2012, 287, 18806–18819. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.; Pham, H.; Pandol, S.; Ptasznik, A. Src as the link between inflammation and cancer. Front. Physiol. 2014, 4, 416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, Y.-M.; Kim, Y.-M.; Lee, Y.M.; Kim, H.-S.; Kim, J.D.; Choi, Y.; Kim, K.-W.; Lee, S.-Y.; Kwon, Y.-G. TNF-related activation-induced cytokine (TRANCE) induces angiogenesis through the activation of Src and phospholipase C (PLC) in human endothelial cells. J. Biol. Chem. 2002, 277, 6799–6805. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomczyk, M.P.R.; Wiater, A.; Pleszczyńska, M.; Kandefer-Szerszeń, M.; Szczodrak, J. The influence of aqueous extracts of selected Potentilla species on normal human colon cells. Acta Pol. Pharm. 2013, 70, 523–531. [Google Scholar] [PubMed]
- Gairola, S.; Sharma, J.; Bedi, Y.S. A cross-cultural analysis of Jammu, Kashmir and Ladakh (India) medicinal plant use. J. Ethnopharmacol. 2014, 155, 925–986. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.P.; Kim, D.S.; Park, S.H.; Shin, C.Y.; Woo, J.J.; Kim, J.W.; An, R.-B.; Lee, C.; Cho, J.Y. Antioxidant capacity of Potentilla paradoxa Nutt. and its beneficial effects related to anti-aging in HaCaT and B16F10 cells. Plants 2022, 11, 873. [Google Scholar] [CrossRef]
- Nam, J.-H.; Kim, H.-S.; Kim, B.-J.; Yu, H.-S.; Chang, D.-C.; Jin, Y.-I.; Yoo, D.-L.; Choi, J.-K.; Park, H.-J.; Lee, S.-B.; et al. In vitro anti-inflammatory activity of extracts from Potentilla supina in murine macrophage RAW 264.7 cells. J. Plant Biotechnol. 2017, 44, 76–81. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.; Shin, K.K.; Kim, H.G.; Jo, M.; Kim, J.K.; Lee, J.S.; Choung, E.S.; Li, W.Y.; Lee, S.W.; Kim, K.-H.; et al. Src/NF-κB-targeted anti-inflammatory effects of Potentilla glabra var. Mandshurica (Maxim.) Hand.-Mazz. ethanol extract. Biomolecules 2020, 10, 648. [Google Scholar] [CrossRef]
- Sharma, J.N.; Al-Omran, A.; Parvathy, S.S. Role of nitric oxide in inflammatory diseases. Inflammopharmacology 2007, 15, 252–259. [Google Scholar] [CrossRef]
- Ringbom, T.; Huss, U.; Stenholm, Å.; Flock, S.; Skattebøl, L.; Perera, P.; Bohlin, L. COX-2 inhibitory effects of naturally occurring and modified fatty acids. J. Nat. Prod. 2001, 64, 745–749. [Google Scholar] [CrossRef]
- Nam, K.-W.; Je, K.-H.; Lee, J.H.; Han, H.J.; Lee, H.J.; Kang, S.K.; Mar, W. Inhibition of COX-2 activity and proinflammatory cytokines (TNF-α and IL-1β) production by water-soluble sub-fractionated parts from bee (Apis mellifera) venom. Arch. Pharm. Res. 2003, 26, 383–388. [Google Scholar] [CrossRef]
- Zhang, J.-M.; An, J. Cytokines, inflammation, and pain. Int. Anesthesiol. Clin. 2007, 45, 27–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwenger, P.; Alpert, D.; Skolnik, E.Y.; Vilček, J. Activation of p38 mitogen-activated protein kinase by sodium salicylate leads to inhibition of tumor necrosis factor-induced IκBα phosphorylation and degradation. Mol. Cell. Biol. 1998, 18, 78–84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Erdinest, N.; Shmueli, O.; Grossman, Y.; Ovadia, H.; Solomon, A. Anti-inflammatory effects of alpha linolenic acid on human Corneal epithelial cells. Invest. Opthalmol. Vis. Sci. 2012, 53, 4396. [Google Scholar] [CrossRef]
- Aparna, V.; Dileep, K.V.; Mandal, P.K.; Karthe, P.; Sadasivan, C.; Haridas, M. Anti-inflammatory property of n-hexadecanoic acid: Structural evidence and kinetic assessment. Chem. Biol. Drug Des. 2012, 80, 434–439. [Google Scholar] [CrossRef]
- Kong, F.; Lee, B.; Wei, K. 5-Hydroxymethylfurfural mitigates lipopolysaccharide-stimulated inflammation via suppression of MAPK, NF-κB and mTOR activation in RAW 264.7 Cells. Molecules 2019, 24, 275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tripathi, N.; Kumar, S.; Singh, R.; Singh, C.J.; Singh, P.; Varshney, V.K. Isolation and identification of γ-sitosterol by GC-MS from the leaves of Girardinia heterophylla (Decne). Open Bioact. Comp. J. 2013, 4, 25–27. [Google Scholar] [CrossRef] [Green Version]
- Avbelj, M.; Hafner-Bratkovič, I.; Lainšček, D.; Manček-Keber, M.; Peternelj, T.T.; Panter, G.; Treon, S.P.; Gole, B.; Potočnik, U.; Jerala, R. Cleavage-mediated regulation of Myd88 signaling by inflammasome-activated caspase-1. Front. Immunol. 2022, 12, 258. [Google Scholar] [CrossRef]
- You, L.; Kim, M.Y.; Cho, J.Y. Protective effect of Potentilla glabra in UVB-induced photoaging process. Molecules 2021, 26, 5408. [Google Scholar] [CrossRef]
- Sun, J.; Zhang, X.; Broderick, M.; Fein, H. Measurement of nitric oxide production in biological systems by using Griess reaction assay. Sensors 2003, 3, 276–284. [Google Scholar] [CrossRef] [Green Version]
- Lee, C.Y.; Kim, H.G.; Park, S.H.; Jang, S.G.; Park, K.J.; Kim, D.S.; Kim, J.H.; Cho, J.Y. Anti-inflammatory functions of alverine via targeting Src in the NF-κB pathway. Biomolecules 2020, 10, 611. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.O.; Yang, Y.; Tao, Y.; Yi, Y.S.; Cho, J.Y. Korean Red Ginseng saponin fraction exerts anti-inflammatory effects by targeting the NF-kappaB and AP-1 pathways. J. Ginseng Res. 2022, 46, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Burnette, W.N. “Western Blotting”: Electrophoretic transfer of proteins from sodium dodecyl sulfate-polyacrylamide gels to unmodified nitrocellulose and radiographic detection with antibody and radioiodinated protein A. Anal. Biochem. 1981, 112, 195–203. [Google Scholar] [CrossRef]
- Rho, T.; Jeong, H.W.; Hong, Y.D.; Yoon, K.; Cho, J.Y.; Yoon, K.D. Identification of a novel triterpene saponin from Panax ginseng seeds, pseudoginsenoside RT8, and its antiinflammatory activity. J. Ginseng Res. 2020, 44, 145–153. [Google Scholar] [CrossRef]
- Lee, J.O.; Kim, J.H.; Kim, S.; Kim, M.Y.; Hong, Y.H.; Kim, H.G.; Cho, J.Y. Gastroprotective effects of the nonsaponin fraction of Korean Red Ginseng through cyclooxygenase-1 upregulation. J. Ginseng Res. 2020, 44, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.K.; Choi, E.; Hong, Y.H.; Kim, H.; Jang, Y.J.; Lee, J.S.; Choung, E.S.; Woo, B.Y.; Hong, Y.D.; Lee, S.; et al. Syk/NF-kappaB-targeted anti-inflammatory activity of Melicope accedens (Blume) T.G. Hartley methanol extract. J. Ethnopharmacol. 2021, 271, 113887. [Google Scholar] [CrossRef] [PubMed]



| Peak No. | R.T. Min | Name of the Chemical | Corr. Area | % of Total |
|---|---|---|---|---|
| 1 | 1.759 | Acetic acid | 21,109,327 | 1.635% |
| 2 | 2.083 | 3-Isopropoxypropylamine | 10,501,824 | 0.813% |
| 3 | 3.254 | Glyceraldehyde | 10,182,555 | 0.789% |
| 4 | 3.850 | Dihydro-2(3H)-thiophenone | 16,852,589 | 1.305% |
| 5 | 4.026 | Dihydroxyacetone | 23,960,724 | 1.856% |
| 6 | 5.219 | 1,3,4-Thiadiazol-2-amine | 3,874,410 | 0.300% |
| 7 | 6.599 | 1,3,5-Triazine-2,4,6-triamine | 30,477,893 | 2.360% |
| 8 | 7.617 | 2,3-Dihydro-3,5-dihydroxy-6-methyl-4-pyrone | 34,525,448 | 2.674% |
| 9 | 7.785 | 4-Hydroxydihydro-2(3H)-furanone | 3,349,145 | 0.259% |
| 10 | 8.629 | 2,3-Dihydrobenzofuran | 10,411,652 | 0.806% |
| 11 | 8.784 | 5-Hydroxymethylfurfural | 55,030,241 | 4.262% |
| 12 | 9.007 | 3-Hydroxypropane-1,2-diyl diacetate | 30,797,862 | 2.385% |
| 13 | 9.557 | 3-Hydroxy-2,3-dihydromaltol | 55,222,588 | 4.277% |
| 14 | 10.042 | 2-Methoxy-4-vinylphenol | 11,629,996 | 0.901% |
| 15 | 10.419 | 2,7-Oxepanedione | 28,292,149 | 2.191% |
| 16 | 10.892 | 1,2,3-Benzenetriol | 15,699,148 | 1.216% |
| 17 | 11.644 | Glutaric acid, 2-fluorophenyl 3-nitrobenzyl ester | 14,647,966 | 1.134% |
| 18 | 11.840 | Trans-2-Isobutyl-4-methyl-1,3-dioxolane | 32,966,709 | 2.553% |
| 19 | 14.007 | Methyl alpha-d-ribopyranoside | 237,519,046 | 18.395% |
| 20 | 16.218 | Neophytadiene | 2,958,855 | 0.229% |
| 21 | 16.583 | Phthalic acid, 7-bromoheptyl isobutyl ester | 5,313,241 | 0.411% |
| 22 | 17.433 | n-Hexadecanoic acid | 93,083,412 | 7.209% |
| 23 | 17.527 | Dibutyl phthalate | 15,955,128 | 1.236% |
| 24 | 17.758 | Hexadecanoic acid, ethyl ester | 11,265,920 | 0.873% |
| 25 | 18.910 | Phytol | 32,677,229 | 2.531% |
| 26 | 19.164 | 9,12,15-Octadecatrienoic acid, (Z, Z, Z)- | 211,802,731 | 16.404% |
| 27 | 19.316 | Octadecanoic acid | 30,759,152 | 2.382% |
| 28 | 19.419 | 9,12,15-Octadecatrienoic acid, ethyl ester, (Z, Z, Z)- | 19,525,879 | 1.512% |
| 29 | 21.100 | 9-Octadecenamide, (Z)- | 11,897,164 | 0.921% |
| 30 | 21.717 | Kauren-19-oic acid | 3,792,760 | 0.294% |
| 31 | 22.272 | Hexadecanoic acid, 2-hydroxy-1-(hydroxymethyl) ethyl ester | 21,655,818 | 1.677% |
| 32 | 22.610 | 1,2-Benzenedicarboxylic acid, bis (2-ethylhexyl) ester | 10,049,832 | 0.778% |
| 33 | 23.662 | 9,12-Octadecadienoic acid (Z, Z)-, 2-hydroxy-1-(hydroxymethyl) ethyl ester | 9,191,159 | 0.712% |
| 34 | 23.732 | Linolenic acid, 2-hydroxy-1-(hydroxymethyl) ethyl ester (Z, Z, Z)- | 31,457,746 | 2.436% |
| 35 | 23.940 | Thunbergol | 10,918,879 | 0.846% |
| 36 | 24.910 | 2-(Acetoxymethyl)-3-(methoxycarbonyl) biphenylene | 4,408,873 | 0.341% |
| 37 | 25.069 | 2-Ethylacridine | 6,372,792 | 0.494% |
| 38 | 27.168 | Vitamin E | 16,324,800 | 1.264% |
| 39 | 28.301 | Hexamethylcyclotrisiloxane | 4,756,890 | 0.368% |
| 40 | 29.386 | gamma-Sitosterol | 84,425,037 | 6.539% |
| 41 | 30.595 | 2-tert-Butylphenol, tert-butyldimethylsilyl ether | 5,550,719 | 0.430% |
| Gene (Type) | Direction | Sequences (5′ to 3′) |
|---|---|---|
| COX-2 (semi-RT-PCR) | Forward | TCACGTGGAGTCCGCTTTAC |
| Reverse | TTCGACAGGAAGGGGATGTT | |
| COX-2 (real-time PCR) | Forward | TTGGAGGCGAAGTGGGTTTT |
| Reverse | TGGCTGTTTTGGTAGGCTGT | |
| iNOS (semi-RT-PCR) | Forward | TGCCAGGGTCACAACTTTACA |
| Reverse | ACCCCAAGCAAGACTTGGAC | |
| IL-6 (semi-RT-PCR) | Forward | GCCTTCTTGGGACTGATGG |
| Reverse | TGGAAATTGGGGTAGGAAGGAC | |
| IL-6 (real-time PCR) | Forward | AGCCAGAGTCCTTCAGAGAGA |
| Reverse | AGGAGAGCATTGGAAATTGGGG | |
| TNF-α (semi-RT-PCR) | Forward | TGCCTATGTCTCAGCCTCTT |
| Reverse | GAGGCCATTTGGGAACTTCT | |
| TNF-α (real-time PCR) | Forward | TTGACCTCAGCGCTGAGTTG |
| Reverse | CCTGTAGCCCACGTCGTAGC | |
| GAPDH (semi-RT-PCR) | Forward | GAAGGTCGGTGTGAACGGAT |
| Reverse | AGTGATGGCATGGACTGTGG | |
| GAPDH (real-time PCR) | Forward | TGTTGAACGGATTTGGCCGTA |
| Reverse | ACTGTGCCGTTGAATTTGCC |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.W.; Kwon, K.W.; Kim, M.-Y.; Cho, J.Y. Potentilla paradoxa Nutt. Ethanol Extract Exhibits Anti-Inflammatory Effects by Suppression of the Src/NF-κB Signaling Pathway. Plants 2022, 11, 1750. https://doi.org/10.3390/plants11131750
Kim JW, Kwon KW, Kim M-Y, Cho JY. Potentilla paradoxa Nutt. Ethanol Extract Exhibits Anti-Inflammatory Effects by Suppression of the Src/NF-κB Signaling Pathway. Plants. 2022; 11(13):1750. https://doi.org/10.3390/plants11131750
Chicago/Turabian StyleKim, Ji Won, Ki Woong Kwon, Mi-Yeon Kim, and Jae Youl Cho. 2022. "Potentilla paradoxa Nutt. Ethanol Extract Exhibits Anti-Inflammatory Effects by Suppression of the Src/NF-κB Signaling Pathway" Plants 11, no. 13: 1750. https://doi.org/10.3390/plants11131750
APA StyleKim, J. W., Kwon, K. W., Kim, M.-Y., & Cho, J. Y. (2022). Potentilla paradoxa Nutt. Ethanol Extract Exhibits Anti-Inflammatory Effects by Suppression of the Src/NF-κB Signaling Pathway. Plants, 11(13), 1750. https://doi.org/10.3390/plants11131750







