Biomechanical Evaluation of Hydroxyapatite/poly-l-lactide Fixation in Mandibular Body Reconstruction with Fibula Free Flap: A Finite Element Analysis Incorporating Material Properties and Masticatory Function Evaluation
Abstract
1. Introduction
2. Materials and Methods
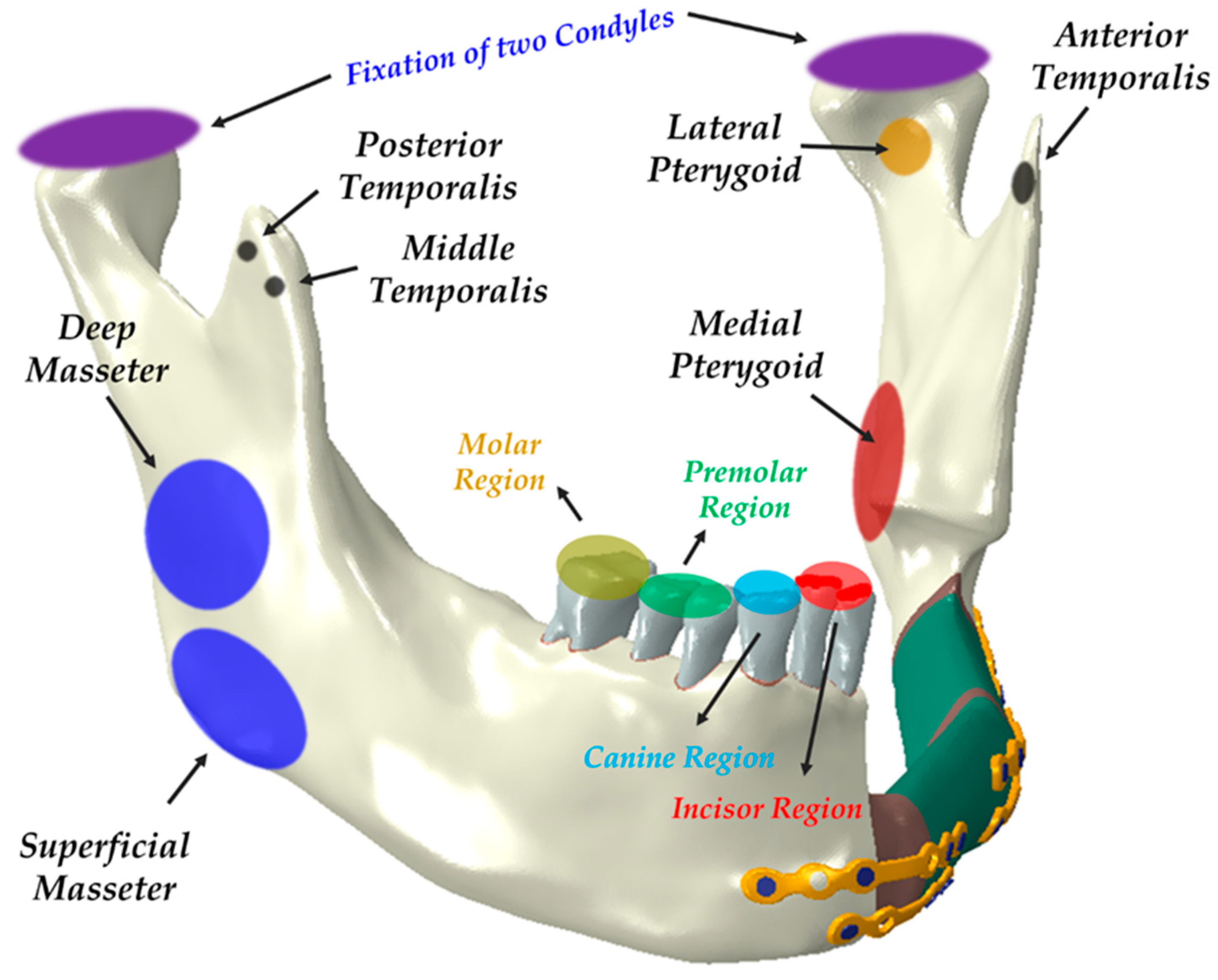
2.1. FEA Model
2.2. Evaluation of Masticatory Function and Occlusal Force in FEA Model
3. Results
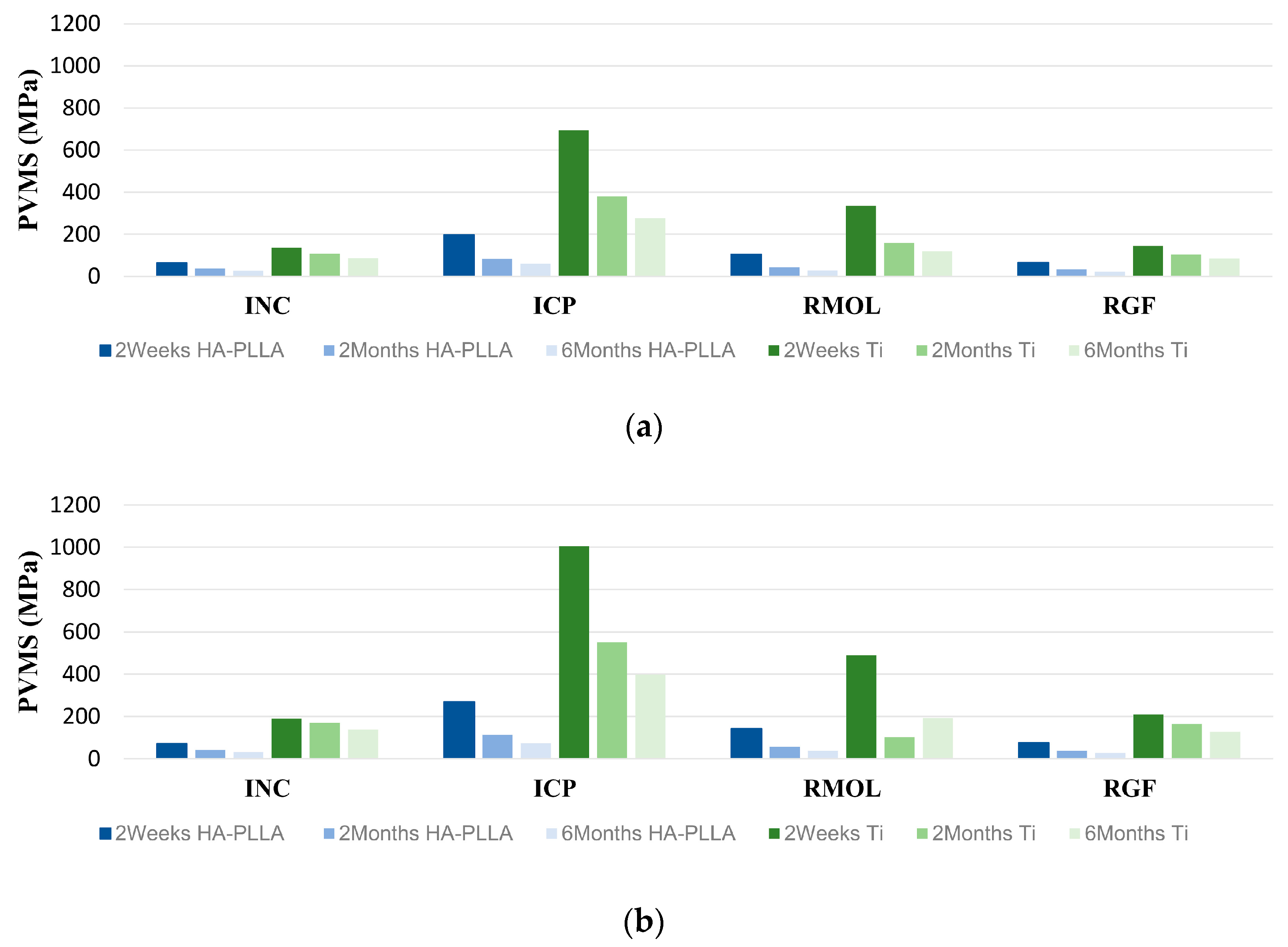
3.1. PVMS Distributions and Patterns
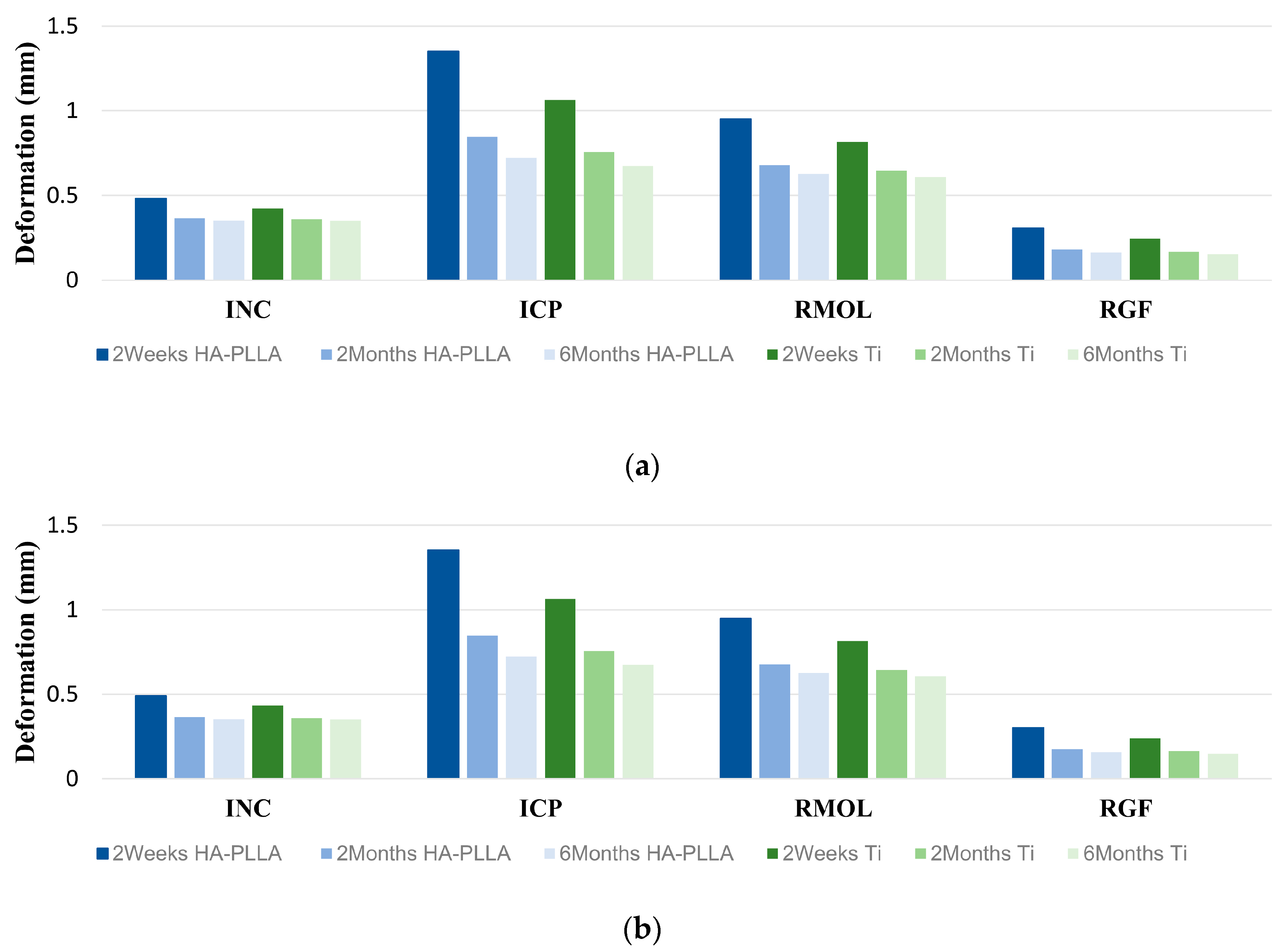
3.2. Fixation System’s Deformation with Clenching Tasks
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Steel, B.J.; Cope, M.R. A brief history of vascularized free flaps in the oral and maxillofacial region. J. Oral Maxillofac. Surg. 2015, 73, 786.e1–786.e11. [Google Scholar] [CrossRef] [PubMed]
- Takushima, A.; Harii, K.; Asato, H.; Momosawa, A.; Okazaki, M.; Nakatsuka, T. Choice of osseous and osteocutaneous flaps for mandibular reconstruction. Int. J. Clin. Oncol. 2005, 10, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Moubayed, S.P.; L’Heureux-Lebeau, B.; Christopoulos, A.; Sampalis, J.S.; Letourneau-Guillon, L.; Bissada, E.; Guertin, L.; Harris, P.G.; Danino, A.M.; Ayad, T. Osteocutaneous free flaps for mandibular reconstruction: Systematic review of their frequency of use and a preliminary quality of life comparison. J. Laryngol. Otol. 2014, 128, 1034–1043. [Google Scholar] [CrossRef] [PubMed]
- Wallace, C.G.; Chang, Y.M.; Tsai, C.Y.; Wei, F.C. Harnessing the potential of the free fibula osteoseptocutaneous flap in mandible reconstruction. Plast. Reconstr. Surg. 2010, 125, 305–314. [Google Scholar] [CrossRef]
- Peled, M.; El-Naaj, I.A.; Lipin, Y.; Ardekian, L. The use of free fibular flap for functional mandibular reconstruction. J. Oral Maxillofac. Surg. 2005, 63, 220–224. [Google Scholar] [CrossRef]
- Ferri, J.; Piot, B.; Ruhin, B.; Mercier, J. Advantages and limitations of the fibula free flap in mandibular reconstruction. J. Oral Maxillofac. Surg. 1997, 55, 440–448. [Google Scholar] [CrossRef]
- Sobti, N.; Ahmed, K.S.; Polanco, T.; Chilov, M.; Cohen, M.A.; Boyle, J.; Shahzad, F.; Matros, E.; Nelson, J.A.; Allen, R.J., Jr. Mini-plate versus reconstruction bar fixation for oncologic mandibular reconstruction with free fibula flaps: A systematic review and meta-analysis. J. Plast. Reconstr. Aesthet. Surg. 2022, 75, 2691–2701. [Google Scholar] [CrossRef]
- Zhang, Z.L.; Wang, S.; Sun, C.F.; Xu, Z.F. Miniplates versus reconstruction plates in vascularized osteocutaneous flap reconstruction of the mandible. J. Craniofac. Surg. 2019, 30, e119–e125. [Google Scholar] [CrossRef] [PubMed]
- Robey, A.B.; Spann, M.L.; McAuliff, T.M.; Meza, J.L.; Hollins, R.R.; Johnson, P.J. Comparison of miniplates and reconstruction plates in fibular flap reconstruction of the mandible. Plast. Reconstr. Surg. 2008, 122, 1733–1738. [Google Scholar] [CrossRef]
- Park, B.; Jung, B.T.; Kim, W.H.; Lee, J.H.; Kim, B.; Lee, J.H. The stability of hydroxyapatite/poly-l-lactide fixation for unilateral angle fracture of the mandible assessed using a finite element analysis model. Materials 2020, 13, 228. [Google Scholar] [CrossRef]
- Gareb, B.; Van Bakelen, N.B.; Vissink, A.; Bos, R.R.M.; Van Minnen, B. Titanium or biodegradable osteosynthesis in maxillofacial surgery? In vitro and in vivo performances. Polymers 2022, 14, 2782. [Google Scholar] [CrossRef] [PubMed]
- Buijs, G.J.; Stegenga, B.; Bos, R.R. Efficacy and safety of biodegradable osteofixation devices in oral and maxillofacial surgery: A systematic review. J. Dent. Res. 2006, 85, 980–989. [Google Scholar] [CrossRef]
- Gareb, B.; van Bakelen, N.B.; Buijs, G.J.; Jansma, J.; de Visscher, J.; Hoppenreijs, T.J.M.; Bergsma, J.E.; van Minnen, B.; Stegenga, B.; Bos, R.R.M. Comparison of the long-term clinical performance of a biodegradable and a titanium fixation system in maxillofacial surgery: A multicenter randomized controlled trial. PLoS ONE 2017, 12, e0177152. [Google Scholar] [CrossRef]
- Yaremchuk, M.J.; Posnick, J.C. Resolving controversies related to plate and screw fixation in the growing craniofacial skeleton. J. Craniofac. Surg. 1995, 6, 525–538. [Google Scholar] [CrossRef]
- Alpert, B.; Seligson, D. Removal of asymptomatic bone plates used for orthognathic surgery and facial fractures. J. Oral Maxillofac. Surg. 1996, 54, 618–621. [Google Scholar] [CrossRef] [PubMed]
- Sukegawa, S.; Kanno, T.; Katase, N.; Shibata, A.; Takahashi, Y.; Furuki, Y. Clinical evaluation of an unsintered hydroxyapatite/poly-l-lactide osteoconductive composite device for the internal fixation of maxillofacial fractures. J. Craniofac. Surg. 2016, 27, 1391–1397. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Park, E.S.; Nam, S.M.; Choi, C.Y.; Shin, H.S.; Kim, Y.B. Surgical treatment of mandible fracture using unsintered hydroxyapatite/poly l-lactide composite fixation system. J. Craniofac. Surg. 2019, 30, 2573–2575. [Google Scholar] [CrossRef]
- Song, I.S.; Choi, J.; Kim, S.R.; Lee, J.H. Stability of bioresorbable plates following reduction of mandibular body fracture: Three-dimensional analysis. J. Craniomaxillofac. Surg. 2019, 47, 1752–1757. [Google Scholar] [CrossRef]
- Sukegawa, S.; Kanno, T.; Yamamoto, N.; Nakano, K.; Takabatake, K.; Kawai, H.; Nagatsuka, H.; Furuki, Y. Biomechanical loading comparison between titanium and unsintered hydroxyapatite/poly-l-lactide plate system for fixation of mandibular subcondylar fractures. Materials 2019, 12, 1557. [Google Scholar] [CrossRef]
- Jung, B.T.; Kim, W.H.; Park, B.; Lee, J.H.; Kim, B.; Lee, J.H. Biomechanical evaluation of unilateral subcondylar fracture of the mandible on the varying materials: A finite element analysis. PLoS ONE 2020, 15, e0240352. [Google Scholar] [CrossRef]
- Jung, B.T.; Kim, W.H.; Kim, B.; Lee, J.H. Biomechanical integrity of hydroxyapatite/poly-l-lactide fixation system in mandibular body reconstruction with deep circumflex iliac artery free flap. J. Mater. Res. Technol. 2022, 18, 4662–4671. [Google Scholar] [CrossRef]
- Shikinami, Y.; Okuno, M. Bioresorbable devices made of forged composites of hydroxyapatite (HA) particles and poly-L-lactide (PLLA): Part I. Basic characteristics. Biomaterials 1999, 20, 859–877. [Google Scholar] [CrossRef] [PubMed]
- Shikinami, Y.; Matsusue, Y.; Nakamura, T. The complete process of bioresorption and bone replacement using devices made of forged composites of raw hydroxyapatite particles/poly l-lactide (F-u-HA/PLLA). Biomaterials 2005, 26, 5542–5551. [Google Scholar] [CrossRef]
- Furukawa, T.; Matsusue, Y.; Yasunaga, T.; Shikinami, Y.; Okuno, M.; Nakamura, T. Biodegradation behavior of ultra-high-strength hydroxyapatite/poly (L-lactide) composite rods for internal fixation of bone fractures. Biomaterials 2000, 21, 889–898. [Google Scholar] [CrossRef]
- Kojima, Y.; Fukui, H. A numerical simulation of tooth movement by wire bending. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 452–459. [Google Scholar] [CrossRef]
- Hong, K.; Kim, W.H.; Eghan-Acquah, E.; Lee, J.H.; Lee, B.K.; Kim, B. Efficient design of a clear aligner attachment to induce bodily tooth movement in orthodontic treatment using finite element analysis. Materials 2021, 14, 4926. [Google Scholar] [CrossRef]
- Bujtar, P.; Sandor, G.K.; Bojtos, A.; Szucs, A.; Barabas, J. Finite element analysis of the human mandible at 3 different stages of life. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 110, 301–309. [Google Scholar] [CrossRef]
- Osagie-Clouard, L.; Kaufmann, J.; Blunn, G.; Coathup, M.; Pendegrass, C.; Meeson, R.; Briggs, T.; Moazen, M. Biomechanics of two external fixator devices used in rat femoral fractures. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 2019, 37, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Assari, A.; Alasseri, N.; Mosadomi, H.A. Biomechanical assessment of unilateral sagittal split ramus osteotomy: A finite element analys. Front. Oral Maxillofac. Med. 2024, 1–9. [Google Scholar] [CrossRef]
- Choi, J.P.; Baek, S.H.; Choi, J.Y. Evaluation of stress distribution in resorbable screw fixation system: Three-dimensional finite element analysis of mandibular setback surgery with bilateral sagittal split ramus osteotomy. J. Craniofac. Surg. 2010, 21, 1104–1109. [Google Scholar] [CrossRef]
- Maurer, P.; Holweg, S.; Knoll, W.D.; Schubert, J. Study by finite element method of the mechanical stress of selected biodegradable osteosynthesis screws in sagittal ramus osteotomy. Br. J. Oral Maxillofac. Surg. 2002, 40, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Savignano, R.; Viecilli, R.F.; Oyoyo, U. Three-dimensional nonlinear prediction of tooth movement from the force system and root morphology. Angle Orthodont. 2020, 90, 811–822. [Google Scholar] [CrossRef] [PubMed]
- Prasad, K.N.; Mathew, S.; Shivamurthy, P.; Sabrish, S.; Sagarkar, R. Orthodontic Displacement and Stress Assessment: A Finite Element Analysis. World J. Dent. 2017, 8, 407–412. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; Dal Piva, A.M.D.O.; Rodrigues, V.A.; Borges, A.L.S.; Nishioka, R.S. Stress and strain distributions on short implants with two different prosthetic connections—An in vitro and in silico analysis. Braz. Dent. Sci. 2017, 20, 101–109. [Google Scholar] [CrossRef]
- Kim, W.H.; Song, E.S.; Ju, K.W.; Lee, J.H.; Kim, M.Y.; Lim, D.; Kim, B. Finite element analysis of novel separable fixture for easy retrievement in case with peri-implantitis. Materials 2019, 12, 235. [Google Scholar] [CrossRef]
- Zhang, G.; Yuan, H.; Chen, X.; Wang, W.; Chen, J.; Liang, J.; Zhang, P. A three-dimensional finite element study on the biomechanical simulation of various structured dental implants and their surrounding bone tissues. Int. J. Dent. 2016, 2016, 4867402. [Google Scholar] [CrossRef]
- Hijazi, L.; Hejazi, W.; Darwich, M.A.; Darwich, K. Finite element analysis of stress distribution on the mandible and condylar fracture osteosynthesis during various clenching tasks. Oral Maxillofac. Surg. 2016, 20, 359–367. [Google Scholar] [CrossRef]
- Zhou, W.; Rong, Q.; An, J.; Zhang, Y. Finite element analysis of two- and three-dimensional fixation in treating mandibular symphyseal fracture combined with bilateral condylar intracapsular fractures. J. Craniofac. Surg. 2021, 32, 2557–2561. [Google Scholar] [CrossRef]
- Korioth, T.W.; Hannam, A.G. Mandibular forces during simulated tooth clenching. J. Orofac. Pain 1994, 8, 178–189. [Google Scholar]
- Yamakawa, S.; Hayashida, K. Safety and efficacy of secondary mandibular reconstruction using a free osteo-cutaneous fibula flap after segmental mandibular resection: A retrospective case-control study. BMC Surg. 2021, 21, 189. [Google Scholar] [CrossRef]
- Al-Bustani, S.; Austin, G.K.; Ambrose, E.C.; Miller, J.; Hackman, T.G.; Halvorson, E.G. Miniplates Versus Reconstruction Bars for Oncologic Free Fibula Flap Mandible Reconstruction. Ann. Plast. Surg. 2016, 77, 314–317. [Google Scholar] [CrossRef] [PubMed]
- Bellenger, E.; Benhafid, Y.; Troussier, N. Framework for controlled cost and quality of assumptions in finite element analysis. Finite Elem. Anal. Des. 2008, 45, 25–36. [Google Scholar] [CrossRef]
- Lee, J.H.; Han, H.S.; Kim, Y.C.; Lee, J.Y.; Lee, B.K. Stability of biodegradable metal (Mg-Ca-Zn alloy) screws compared with absorbable polymer and titanium screws for sagittal split ramus osteotomy of the mandible using the finite element analysis model. J. Craniomaxillofac. Surg. 2017, 45, 1639–1646. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.Y.; Su, M.Z.; Chang, H.H.; Chiang, Y.C.; Tao, S.H.; Cheng, J.H.; Fuh, L.J.; Lin, C.P. Tension-compression viscoelastic behaviors of the periodontal ligament. J. Formos. Med. Assoc. 2012, 111, 471–481. [Google Scholar] [CrossRef]


| Components | HU | Papp | Young’s Modulus (MPa) | Poisson’s Ratio | |
|---|---|---|---|---|---|
| Titanium [28] | - | - | 96,000 | 0.36 | |
| HA-PLLA [29] | - | - | 9701 | 0.317 | |
| Cortical bone [30,31] | Healthy | - | - | 15,000 | 0.33 |
| Cancellous bone [30,31] | Healthy | - | - | 1500 | 0.3 |
| Tooth [32] | - | - | 20,000 | 0.3 | |
| PDL [33] | - | - | 0.69 | 0.45 | |
| Cortical bone [27] | 2 Weeks | 1399 | 1478.8 | 9238.29 | 0.33 |
| 2 Months | 1429 | 1514.8 | 9638.23 | 0.33 | |
| 6 Months | 1534 | 1640.8 | 9854.52 | 0.33 | |
| Callus [27] | 2 Weeks | 212 | 54.4 | 27.44 | 0.33 |
| 2 Months | 308 | 169.6 | 203.45 | 0.33 | |
| 6 Months | 376 | 251.2 | 406.49 | 0.33 | |
| Component | Number of Nodes | Number of Elements | Mesh Size | |
|---|---|---|---|---|
| Maximum | Minimum | |||
| Miniplate | 143,279 | 680,029 | 0.15 | 0.05 |
| Screw | 187,845 | 961,484 | 0.15 | 0.05 |
| Cortical bone | 377,281 | 1,853,115 | 0.8 | 0.15 |
| Cancellous bone | 357,839 | 1,909,969 | 0.8 | 0.15 |
| Tooth | 275,622 | 1,492,811 | 0.3 | 0.15 |
| PDL | 116,317 | 427,042 | 0.1 | 0.03 |
| Fibular bone | 88,182 | 423,717 | 0.8 | 0.15 |
| Callus | 13,097 | 63,035 | 0.8 | 0.15 |
| 2 Weeks after Surgery | 2 Months after Surgery | 6 Months after Surgery | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Loading Conditions | Ti | HA-PLLA | Ti | HA-PLLA | Ti | HA-PLLA | ||||||
| Screw | Plate | Screw | Plate | Screw | Plate | Screw | Plate | Screw | Plate | Screw | Plate | |
| INC | 136.7 | 188.7 | 64.2 | 71.6 | 106.6 | 169.5 | 37.36 | 41.8 | 86.62 | 137.8 | 26.1 | 30.6 |
| ICP | 693.6 | 1005 | 198.7 | 268.0 | 379.3 | 549.9 | 84.44 | 112.8 | 275.9 | 397.4 | 59.7 | 73.8 |
| RMOL | 334.9 | 490.6 | 104.5 | 141.9 | 158.1 | 103.0 | 44.4 | 56.0 | 118.5 | 192.5 | 28.1 | 37.9 |
| RGF | 144.5 | 209.5 | 65.7 | 74.7 | 103.0 | 163.7 | 33.4 | 37.7 | 85.76 | 127.8 | 22.7 | 26.4 |
| 2 Weeks after Surgery | 2 Months after Surgery | 6 Months after Surgery | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Loading Conditions | Ti | HA-PLLA | Ti | HA-PLLA | Ti | HA-PLLA | ||||||
| Screw | Plate | Screw | Plate | Screw | Plate | Screw | Plate | Screw | Plate | Screw | Plate | |
| INC | 0.433 | 0.424 | 0.491 | 0.482 | 0.358 | 0.358 | 0.366 | 0.366 | 0.350 | 0.349 | 0.352 | 0.351 |
| ICP | 1.065 | 1.065 | 1.353 | 1.351 | 0.756 | 0.756 | 0.847 | 0.845 | 0.675 | 0.674 | 0.723 | 0.721 |
| RMOL | 0.814 | 0.818 | 0.948 | 0.952 | 0.644 | 0.644 | 0.677 | 0.678 | 0.607 | 0.609 | 0.626 | 0.627 |
| RGF | 0.239 | 0.245 | 0.301 | 0.307 | 0.163 | 0.163 | 0.176 | 0.182 | 0.148 | 0.153 | 0.157 | 0.162 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.-M.; Jung, T.-G.; Kim, W.-H.; Kim, B.; Lee, J.-H. Biomechanical Evaluation of Hydroxyapatite/poly-l-lactide Fixation in Mandibular Body Reconstruction with Fibula Free Flap: A Finite Element Analysis Incorporating Material Properties and Masticatory Function Evaluation. Bioengineering 2024, 11, 1009. https://doi.org/10.3390/bioengineering11101009
Lee S-M, Jung T-G, Kim W-H, Kim B, Lee J-H. Biomechanical Evaluation of Hydroxyapatite/poly-l-lactide Fixation in Mandibular Body Reconstruction with Fibula Free Flap: A Finite Element Analysis Incorporating Material Properties and Masticatory Function Evaluation. Bioengineering. 2024; 11(10):1009. https://doi.org/10.3390/bioengineering11101009
Chicago/Turabian StyleLee, Sang-Min, Tae-Gon Jung, Won-Hyeon Kim, Bongju Kim, and Jee-Ho Lee. 2024. "Biomechanical Evaluation of Hydroxyapatite/poly-l-lactide Fixation in Mandibular Body Reconstruction with Fibula Free Flap: A Finite Element Analysis Incorporating Material Properties and Masticatory Function Evaluation" Bioengineering 11, no. 10: 1009. https://doi.org/10.3390/bioengineering11101009
APA StyleLee, S.-M., Jung, T.-G., Kim, W.-H., Kim, B., & Lee, J.-H. (2024). Biomechanical Evaluation of Hydroxyapatite/poly-l-lactide Fixation in Mandibular Body Reconstruction with Fibula Free Flap: A Finite Element Analysis Incorporating Material Properties and Masticatory Function Evaluation. Bioengineering, 11(10), 1009. https://doi.org/10.3390/bioengineering11101009







