Journal Description
Neurology International
Neurology International
is an international, peer-reviewed, open access journal which provides an advanced forum for studies related to all aspects of neurology and neuroscience, published monthly online by MDPI (from Volume 12 issue 3 - 2020). The Panhellenic Federation of Alzheimer's Disease and Related Disorders (PFADRD) is affiliated with Neurology International and its members receive discounts on the article processing charges.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, ESCI (Web of Science), PubMed, PMC, Embase, and other databases.
- Journal Rank: JCR - Q2 (Clinical Neurology)
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 21.4 days after submission; acceptance to publication is undertaken in 3.8 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
- Journal Cluster of Neurosciences: Brain Sciences, Neurology International, NeuroSci, Clinical and Translational Neuroscience, Neuroglia, Psychiatry International, Clocks & Sleep and Journal of Dementia and Alzheimer's Disease.
Impact Factor:
3.0 (2024);
5-Year Impact Factor:
3.3 (2024)
Latest Articles
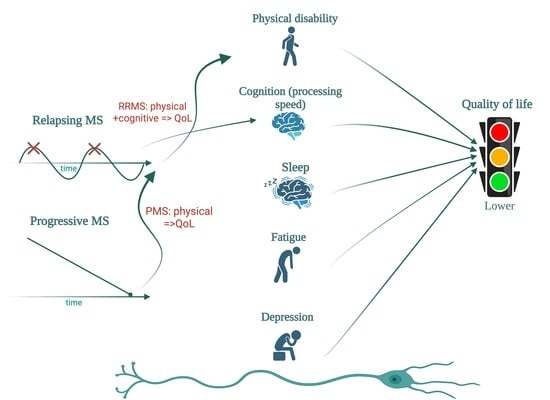
Multidimensional Impairment in Multiple Sclerosis: Physical Disability, Cognitive Dysfunction, Sleep Disturbance, Fatigue, Depression, and Their Impact on Quality of Life—A Possible Common Pathological Pathway
Neurol. Int. 2025, 17(11), 174; https://doi.org/10.3390/neurolint17110174 - 22 Oct 2025
Abstract
Background: Multiple sclerosis (MS) is a chronic inflammatory disease of the central nervous system, which can lead to physical and cognitive disability, fatigue, depression, and sleep disturbance, all of which may impair quality of life (QoL). While the physical disability is widely known
[...] Read more.
Background: Multiple sclerosis (MS) is a chronic inflammatory disease of the central nervous system, which can lead to physical and cognitive disability, fatigue, depression, and sleep disturbance, all of which may impair quality of life (QoL). While the physical disability is widely known to influence the QoL, the relative contributions of cognitive impairment, fatigue, and sleep quality remain incompletely defined. Objectives: To evaluate the relationship between QoL, physical and cognitive disability, sleep quality, fatigue, and depression in people with MS (PwMS), and to explore phenotype-specific differences between relapsing and progressive forms. Methods: In this monocentric cross-sectional study, 112 PwMS underwent physical assessment (EDSS, MSFC), cognitive testing (SDMT, PASAT, MoCA, MMSE), and QoL evaluation (MSIS-29, EQ-5D, EQ-VAS, MSNQ). A subgroup of 29 patients also completed the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), Modified Fatigue Impact Scale (MFIS), and Beck Depression Inventory (BDI). Correlation and group analyses were performed. Results: Progressive MS patients showed greater physical disability (mean EDSS 5.8 vs. 2.6, p < 0.001), poorer cognitive performance, and lower QoL. Across the cohort, QoL strongly correlated with physical disability (EDSS) and cognitive performance (SDMT), with physical measures showing stronger associations. In relapsing MS, physical and cognitive impairment were linked to reduced QoL, whereas in progressive MS, physical disability predominated. In the sleep subgroup, poorer PSQI scores, longer sleep latency, and daytime sleepiness correlated with higher fatigue (MFIS), depressive symptoms (BDI), and reduced QoL (MSIS-29, EQ-5D). Conclusions: QoL in MS reflects the combined burden of physical disability, cognitive impairment, fatigue, depression, and poor sleep quality, with phenotype-specific patterns. While physical disability is the main QoL determinant in progressive MS, cognitive deficits with slowed processing speed play an important role in relapsing MS. Comprehensive, multidimensional assessment, including sleep and mood screening, may support individualized management strategies in MS.
Full article
(This article belongs to the Topic Management of Multiple Sclerosis: Past, Present and Promise)
►
Show Figures
Open AccessReview
Autism Spectrum Disorder: The Cerebellum, Genes, and Pathways
by
Santosh R. D’Mello
Neurol. Int. 2025, 17(10), 173; https://doi.org/10.3390/neurolint17100173 - 14 Oct 2025
Abstract
►▼
Show Figures
Autism spectrum disorder (ASD) is a complex, heterogenous, and prevalent neurodevelopmental disorder characterized by core symptoms, including social communication deficits, restrictive interests, and repetitive behaviors. Although environmental factors contribute to the etiology of ASD, the disorder has a strong genetic basis, although the
[...] Read more.
Autism spectrum disorder (ASD) is a complex, heterogenous, and prevalent neurodevelopmental disorder characterized by core symptoms, including social communication deficits, restrictive interests, and repetitive behaviors. Although environmental factors contribute to the etiology of ASD, the disorder has a strong genetic basis, although the specific genes involved in causing or contributing to the disorder remain to be conclusively identified. Whereas previous studies have focused on the cerebral cortex, hippocampus, and associated brain regions to uncover the underpinnings of ASD, emerging evidence indicates that dysfunction of the cerebellum is one of the most consistent associates of ASD. Traditionally thought to function solely in motor control, more recent studies have established that projections from the cerebellum make mono- and polysynaptic connections to a variety of non-motor areas including the cerebral cortex, hypothalamus, and hippocampus, and is involved in a range of cognitive, sensory, and behavioral functions. While several reviews of the molecular underpinnings of ASD have focused on the other brain regions, primarily the cortex, in this review we describe the key role that the cerebellum plays in the development of ASD and then focus on genetic variations that cause ASD, focusing on genes expressed and studied in the cerebellum. We have divided the ASD-associated genes in two subgroups—those that have been identified through a candidate gene approach with knowledge of their function in the cerebellum and their relationship to ASD subsequently confirmed in experimental models, and those identified through unbiased genetic analyses of individuals with ASD, many of which have not yet been characterized extensively and/or not studied in animal models. We also provide recently reported information on non-genetic factors that combine with genetic factors to promote ASD. Together, we hope our review will provide information on recent and significant findings related to the cerebellar underpinnings in ASD.
Full article

Figure 1
Open AccessArticle
Latent Profiles Based on Combined Risk Factors for Cognitive Decline in European Older Adults: A Retrospective Study Based on the SHARE HCAP Project
by
Johnnatas Mikael Lopes, Paola Bertuccio, Riccardo Vecchio, Giacomo Pietro Vigezzi, Lorenzo Blandi and Anna Odone
Neurol. Int. 2025, 17(10), 172; https://doi.org/10.3390/neurolint17100172 - 14 Oct 2025
Abstract
Background/Objectives: Cognitive decline is common in ageing, ranging from mild to severe manifestations. Although several modifiable risk factors have been identified, they are typically examined individually. This study aimed to identify latent profiles based on combinations of dementia risk factors and to
[...] Read more.
Background/Objectives: Cognitive decline is common in ageing, ranging from mild to severe manifestations. Although several modifiable risk factors have been identified, they are typically examined individually. This study aimed to identify latent profiles based on combinations of dementia risk factors and to quantify the associations with cognitive impairment in a European population of older adults. Methods: Based on the SHARE HCAP project, we conducted a retrospective longitudinal study by linking individual data from wave 6 (2015) and wave 9 (2021–2022). The sample included 2685 individuals aged 50+. The study outcome was cognitive status, assessed using standardised neurological tests and questionnaire and categorised as normal cognition, mild cognitive impairment (MCI), or severe cognitive impairment (SCI). The exposures included clinical, psychosocial, and lifestyle variables. Latent Class Analysis (LCA) was applied to identify distinct profiles, and multinomial logistic regression models were carried out to estimate associations between latent profiles and cognitive status, expressed as odds ratios (ORs) with 95% confidence intervals (CI). Results: The study sample included 2326 participants, of whom 25.1% with MCI and 9.4% with SCI. Through LCA, we identified four profiles: Low-risk, Combined Cluster, Inactive Behaviour, and Cardiometabolic Risk. Compared with the Low-risk profile, the odds of MCI were significantly higher for Combined Cluster profile (OR = 3.11; 95% CI: 2.38–4.06) and CR (OR = 1.44; 95% CI: 1.07–1.93). For SCI, elevated odds were observed for Combined Cluster (OR = 7.30; 95% CI: 4.47–11.92), Cardiometabolic Risk (OR = 2.31; 95% CI: 1.31–4.05), and Inactive Behaviour (OR = 1.87; 95% CI: 1.01–3.48). Conclusions: Four latent profiles were identified, each showing distinct associations with MCI and SCI. The Combined Cluster—characterised by poor mental health, limited physical activity, and hypertension—showed the highest odds of cognitive impairment. Public health strategies should prioritise integrated actions against these risk factors.
Full article
(This article belongs to the Section Aging Neuroscience)
►▼
Show Figures

Graphical abstract
Open AccessArticle
Preliminary Findings from a Mindfulness-Based Intervention in Patients with Psychogenic Non-Epileptic Seizures
by
Rebecca Ciacchini, Ciro Conversano, Graziella Orrù, Chiara Pizzanelli, Claudia Scarpitta, Francesco Turco, Enrica Bonanni, Annachiara Bressan, Thomas Reali and Angelo Gemignani
Neurol. Int. 2025, 17(10), 171; https://doi.org/10.3390/neurolint17100171 - 14 Oct 2025
Abstract
Background/Objectives: Psychogenic non-epileptic seizures (PNES) are seizure-like episodes not caused by abnormal brain activity, often linked to emotional dysregulation, dissociation, and altered interoceptive awareness. Standardized treatments are limited. This study aimed to explore the feasibility and preliminary psychological effects of a group-based
[...] Read more.
Background/Objectives: Psychogenic non-epileptic seizures (PNES) are seizure-like episodes not caused by abnormal brain activity, often linked to emotional dysregulation, dissociation, and altered interoceptive awareness. Standardized treatments are limited. This study aimed to explore the feasibility and preliminary psychological effects of a group-based mindfulness-based intervention (MBI) in individuals with PNES. Methods: This single-arm, pre–post pilot study (no control group) enrolled fifteen participants in two cycles of an 8-week MBI delivered either in-person or online. Twelve participants completed pre/post self-report assessments of depression (BDI-II), anxiety (STAI-Y1), perceived stress (PSS-10), sleep quality (PSQI), dissociation (DES-II), meteoropathy (METEO-Q), mindfulness (FFMQ), and interoceptive awareness (MAIA). Results: The intervention was well tolerated (dropout rate: 20%). Trend-level, non-significant improvements emerged for depressive symptoms (p = 0.092, r = 0.564) and sleep quality (p = 0.078, r = 0.591). A significant reduction was observed in the FFMQ Describing subscale (p = 0.045, r = 0.697). No significant changes were found in anxiety, perceived stress, or interoceptive awareness, although certain MAIA subscales indicated small, non-significant increases. Conclusions: Despite the limited sample size and absence of a control group, these preliminary findings support the feasibility and acceptability of MBIs for PNES, warranting further controlled investigations.
Full article
(This article belongs to the Section Movement Disorders and Neurodegenerative Diseases)
►▼
Show Figures

Graphical abstract
Open AccessArticle
Clinical and Radiological Predictors for Early Hematoma Expansion After Spontaneous Intracerebral Hemorrhage: A Retrospective Study
by
EJun Kim, Jee Hye Wee, Yi Hwa Choi, Hyuntaek Rim, In Bok Chang, Joon Ho Song, Yong Gil Hong and Ji Hee Kim
Neurol. Int. 2025, 17(10), 170; https://doi.org/10.3390/neurolint17100170 - 12 Oct 2025
Abstract
Background: Early hematoma expansion is a major determinant of poor outcomes after spontaneous intracerebral hemorrhage (ICH). Identifying reliable predictors of hematoma expansion may facilitate risk stratification and timely interventions. This study aimed to evaluate clinical, laboratory, and radiological factors associated with early hematoma
[...] Read more.
Background: Early hematoma expansion is a major determinant of poor outcomes after spontaneous intracerebral hemorrhage (ICH). Identifying reliable predictors of hematoma expansion may facilitate risk stratification and timely interventions. This study aimed to evaluate clinical, laboratory, and radiological factors associated with early hematoma expansion within 24 h. Methods: We retrospectively analyzed consecutive patients with spontaneous ICH admitted to a tertiary hospital in Korea between 2009 and 2021. Inclusion criteria were aged ≥ 18 years, primary spontaneous ICH, baseline non-contrast CT (NCCT), and follow-up CT within 24 h. Clinical, laboratory, and medication histories were collected, and NCCT/CT angiography (CTA) imaging markers (spot sign, blend sign, hypodensity, swirl sign, black hole sign, island sign, mean hematoma density) were evaluated. Early hematoma expansion was defined as an absolute volume increase ≥6 cm3 or a relative increase ≥33% on follow-up CT. Multivariate logistic regression identified independent predictors. Results: Among 899 screened patients, 581 met inclusion criteria (mean age 61.6 years; 59.7% male). Seventy-eight patients (13.4%) experienced early hematoma expansion. Independent predictors included CTA spot sign (adjusted OR 9.001, 95% CI 4.414–18.354), blend sign (OR 3.054, 95% CI 1.349–6.910), mean hematoma density <60 HU (OR 2.432, 95% CI 1.271–4.655), male sex (OR 2.902, 95% CI 1.419–5.935), and statin use (OR 2.990, 95% CI 1.149–7.782). Prior antiplatelet therapy was associated with a reduced risk of hematoma expansion (OR 0.118, 95% CI 0.014–0.981). Conclusions: Early hematoma expansion occurred in 13.4% of patients and was predicted by a combination of CTA and NCCT markers, as well as clinical and pharmacological factors. Spot sign remained the strongest predictor, while NCCT features such as blend sign and low hematoma density also provided practical prognostic value. These findings underscore the multifactorial pathophysiology of ICH expansion and highlight the importance of integrating imaging, clinical, and therapeutic variables into prediction models to improve early risk stratification and guide targeted interventions.
Full article
(This article belongs to the Section Brain Tumor and Brain Injury)
►▼
Show Figures

Graphical abstract
Open AccessCase Report
The Diagnostic Pitfalls in the Pronator Teres Syndrome—A Case Report
by
Wiktoria Rałowska-Gmoch, Marcin Hajzyk, Tomasz Matyskieła, Beata Łabuz-Roszak and Edyta Dziadkowiak
Neurol. Int. 2025, 17(10), 169; https://doi.org/10.3390/neurolint17100169 - 12 Oct 2025
Abstract
Background: Pronator teres syndrome is a rare proximal median neuropathy caused by compression of the median nerve at various points. It is a rare condition, and many times it is mistaken for carpal tunnel syndrome. Methods: There are many authors who refer to
[...] Read more.
Background: Pronator teres syndrome is a rare proximal median neuropathy caused by compression of the median nerve at various points. It is a rare condition, and many times it is mistaken for carpal tunnel syndrome. Methods: There are many authors who refer to the pronator syndrome as a compression of the median nerve at several potential sites of en-trapment in the region of the antecubital fossa, more proximal compression at the Liga-ment of Strutters, and more distally, including lacerus fibrosus within the pronator teres muscle and the anterior interosseous nerve. Results: The diagnostic difficulties in a patient with severe right forearm pain during elbow flexion and pronation are presented. Routine test results, including MRI of the right elbow joint, nerve conduction study of the brachial plexus and ulnar nerve, and electromyographic study of the muscles of the right upper ex-tremity, were normal. Ultrasonography showed an enlarged pronator teres muscle. Conclusions: The patient underwent surgical removal of the lacertus fibrosus. All symptoms resolved.
Full article
(This article belongs to the Section Pain Research)
►▼
Show Figures

Figure 1
Open AccessArticle
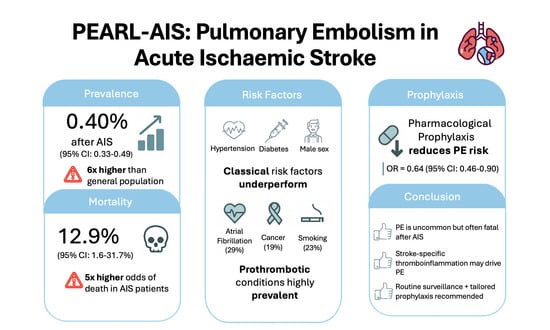
Pulmonary Embolism After Acute Ischaemic Stroke (PEARL-AIS): Global Prevalence, Risk Factors, Outcomes, and Evidence Grading from a Meta-Analysis
by
Darryl Chen, Yuxiang Yang and Sonu M. M. Bhaskar
Neurol. Int. 2025, 17(10), 168; https://doi.org/10.3390/neurolint17100168 - 12 Oct 2025
Abstract
Objectives: Pulmonary embolism (PE) is an uncommon but potentially fatal complication of acute ischaemic stroke (AIS). Its global burden and prevention remain incompletely defined. We performed a systematic review and meta-analysis (PEARL-AIS) to estimate prevalence, risk factors, outcomes, and prophylactic efficacy, with GRADE
[...] Read more.
Objectives: Pulmonary embolism (PE) is an uncommon but potentially fatal complication of acute ischaemic stroke (AIS). Its global burden and prevention remain incompletely defined. We performed a systematic review and meta-analysis (PEARL-AIS) to estimate prevalence, risk factors, outcomes, and prophylactic efficacy, with GRADE evidence appraisal. Methods: Following PRISMA 2020 and MOOSE guidelines, five databases (PubMed, Embase, Cochrane, Scopus, Web of Science) were searched (1995–2024). The protocol was prospectively registered (OSF s25ny). Random-effects models (DerSimonian–Laird; REML sensitivity) were used to pool prevalence and odds ratios; heterogeneity was evaluated with I2, Cochran’s Q, and τ2. Influence (leave-one-out) and subgroup analyses for prevalence and mortality of PE in AIS were explored. Bias was assessed using the Modified Jadad Scale; overall certainty was graded with the GRADE framework. Results: Twenty-four studies met the inclusion criteria (n = 25,666,067), of which seventeen studies (n = 23,637,708) contributed to pooled prevalence analyses. The pooled prevalence of PE after AIS was 0.40% (95% CI 0.33–0.49), approximately six-fold higher than in the general population, with considerable heterogeneity (I2 > 90%, Cochrane classification). The pooled mortality among AIS patients with PE was 12.9% (95% CI 1.6–31.7). Mortality risk was significantly higher in AIS patients with PE (OR 4.96, 95% CI 2.98–8.24). Atrial fibrillation (29%), cancer (19%), and smoking (23%) were common; hypertension (54%) and diabetes (23%) were prevalent but not predictive, with diabetes showing a paradoxical protective association (OR 0.88, 95% CI 0.84–0.92). Pharmacological prophylaxis was associated with a reduced risk of PE (OR 0.64, 95% CI 0.46–0.90; I2 = 0%), supported by moderate-certainty evidence. Conclusions: PE is an uncommon but often fatal complication of AIS. Traditional venous thromboembolism predictors underperform in this context, suggesting a stroke-specific thromboinflammatory mechanism linking the brain and lung axis. Despite considerable heterogeneity and low-to-moderate certainty of evidence, pharmacological prophylaxis demonstrates a consistent protective effect. Systematic PE surveillance and tailored prophylactic strategies should be integral to contemporary stroke care, while future studies should refine risk stratification and elucidate the mechanistic underpinnings of this brain–lung thromboinflammatory continuum.
Full article
(This article belongs to the Special Issue Innovations in Acute Stroke Treatment, Neuroprotection, and Recovery)
►▼
Show Figures
Graphical abstract
Open AccessCase Report
A Novel Frameshift Variant in the SPAST Gene Causing Hereditary Spastic Paraplegia in a Bulgarian–Turkish Family
by
Mariya Levkova, Mihael Tsalta-Mladenov and Ara Kaprelyan
Neurol. Int. 2025, 17(10), 167; https://doi.org/10.3390/neurolint17100167 - 11 Oct 2025
Abstract
Background: Hereditary spastic paraplegia (HSP) is a clinically and genetically heterogeneous group of neurodegenerative disorders characterized by progressive lower-limb spasticity and weakness. SPAST mutations are the most common cause of autosomal dominant HSP (SPG4). However, many pathogenic SPAST variants are unique and genetic
[...] Read more.
Background: Hereditary spastic paraplegia (HSP) is a clinically and genetically heterogeneous group of neurodegenerative disorders characterized by progressive lower-limb spasticity and weakness. SPAST mutations are the most common cause of autosomal dominant HSP (SPG4). However, many pathogenic SPAST variants are unique and genetic data from underrepresented communities remain limited. Methods: Whole-exome sequencing (WES) was performed on the index patient with HSP. Variant annotation tools included Ensembl VEP, LOFTEE, CADD, SIFT, PolyPhen-2, MutationTaster, and SpliceAI. Variant interpretation followed ACMG/AMP guidelines. Clinical evaluation and family history supported phenotypic correlation and segregation. Results: A novel heterozygous frameshift variant in SPAST (c.339delG; p.Glu114Serfs*47) was identified. The variant was predicted to cause nonsense-mediated decay, resulting in loss of the microtubule-interacting and AAA ATPase domains of spastin. It was absent from population databases (gnomAD, TOPMed, 1000 Genomes) and public variant repositories (ClinVar, HGMD). The variant segregated with disease in two affected siblings and could be classified as likely pathogenic. Conclusions: This novel SPAST frameshift variant expands the mutational spectrum of SPG4-HSP and highlights the importance of including isolated or minority communities in genomic research to improve variant interpretation.
Full article
(This article belongs to the Section Movement Disorders and Neurodegenerative Diseases)
►▼
Show Figures

Figure 1
Open AccessReview
Histological and Functional Breakdown of the Blood−Brain Barrier in Alzheimer’s Disease: A Multifactorial Intersection
by
Jordana Mariane Neyra Chauca and Graciela Gaddy Robles Martinez
Neurol. Int. 2025, 17(10), 166; https://doi.org/10.3390/neurolint17100166 - 9 Oct 2025
Abstract
Background: Alzheimer’s disease (AD) is a multifactorial neurodegenerative disorder characterized by amyloid-β (Aβ) plaques, neurofibrillary tangles, and progressive cognitive decline. Recent evidence has highlighted the role of blood–brain barrier (BBB) dysfunction in the early stages of AD pathology. Objective: We sought to explore
[...] Read more.
Background: Alzheimer’s disease (AD) is a multifactorial neurodegenerative disorder characterized by amyloid-β (Aβ) plaques, neurofibrillary tangles, and progressive cognitive decline. Recent evidence has highlighted the role of blood–brain barrier (BBB) dysfunction in the early stages of AD pathology. Objective: We sought to explore the histological structure and physiological function of the blood–brain barrier, and to identify the shared pathological mechanisms between BBB disruption and Alzheimer’s disease progression. Methods: This narrative review was conducted through a comprehensive search of peer-reviewed literature from 1997 to 2024, using databases such as PubMed, Elsevier, Scopus, and Google Scholar. Results: Multiple histological and cellular components—including endothelial cells, pericytes, astrocytes, and tight junctions—contribute to BBB integrity. The breakdown of this barrier in AD is associated with chronic inflammation, oxidative stress, vascular injury, pericyte degeneration, astrocyte polarity loss, and dysfunction of nutrient transport systems like Glucose Transporter Type 1 (GLUT1). These alterations promote neuroinflammation, amyloid-β (Aβ) accumulation, and progressive neuronal damage. Conclusions: BBB dysfunction is not merely a consequence of AD but may act as an early and active driver of its pathogenesis. Understanding the mechanisms of BBB breakdown can lead to early diagnostic markers and novel therapeutic strategies aimed at preserving or restoring barrier integrity in Alzheimer’s disease.
Full article
(This article belongs to the Section Movement Disorders and Neurodegenerative Diseases)
►▼
Show Figures

Graphical abstract
Open AccessBrief Report
Diverging Safety Signals: A Trend Analysis of Suspected Adverse Drug Reactions Reporting for Spinal Muscular Atrophy Therapies in the European Union
by
Andrej Belančić, Petar Mas, Ivana Stević, Dinko Vitezić and Slobodan Janković
Neurol. Int. 2025, 17(10), 165; https://doi.org/10.3390/neurolint17100165 - 8 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: The approval of disease-modifying therapies has significantly improved outcomes for patients with spinal muscular atrophy (SMA), yet their long-term safety profiles remain under continuous evaluation. This study aimed to assess trends in the reporting of suspected adverse drug reactions (ADRs) associated
[...] Read more.
Background/Objectives: The approval of disease-modifying therapies has significantly improved outcomes for patients with spinal muscular atrophy (SMA), yet their long-term safety profiles remain under continuous evaluation. This study aimed to assess trends in the reporting of suspected adverse drug reactions (ADRs) associated with nusinersen, onasemnogene abeparvovec, and risdiplam across the European Union. Methods: We conducted a secondary analysis of annual suspected ADR data reported to EudraVigilance from 2017 to 2024 for the three approved disease-modifying therapies for SMA. On top of general reporting trend, specific adverse reactions of interest included post-lumbar puncture syndrome for nusinersen, liver toxicity and elevated serum troponin for onasemnogene abeparvovec, and respiratory and gastrointestinal reactions for risdiplam. Joinpoint regression analysis was used to evaluate annual percent changes and identify statistically significant trend segments for each medicine. Results: The reporting of suspected ADRs for nusinersen showed an initial increase, followed by a significant decline after 2019. Onasemnogene abeparvovec exhibited a continued but decelerating increase in suspected ADRs, while risdiplam demonstrated a consistent upward trend across all reported reactions. Conclusions: Diverging patterns in adverse reaction reporting suggest a stabilizing safety profile for nusinersen and potential emerging safety signals for risdiplam and onasemnogene abeparvovec, underscoring the need for ongoing continued pharmacovigilance (e.g., post-authorization studies and spontaneous reporting).
Full article

Figure 1
Open AccessArticle
Cognitive, Functional, and Emotional Recovery in Patients with Stroke: A Multidimensional Prospective Analysis
by
Emilio Rubén Pego Pérez, Lourdes Bermello López, Eva Gómez Fernández, María del Rosario Marín Arnés, Mercedes Fernández Vázquez, Carlota Touza González and María Irene Núñez Hernández
Neurol. Int. 2025, 17(10), 164; https://doi.org/10.3390/neurolint17100164 - 8 Oct 2025
Abstract
Background: Stroke is a major cerebrovascular disease characterized by disrupted cerebral blood flow, leading to neuronal damage and significant physical, cognitive, and emotional sequelae. While advancements in acute stroke management have improved survival rates, long-term complications such as cognitive impairment and depression continue
[...] Read more.
Background: Stroke is a major cerebrovascular disease characterized by disrupted cerebral blood flow, leading to neuronal damage and significant physical, cognitive, and emotional sequelae. While advancements in acute stroke management have improved survival rates, long-term complications such as cognitive impairment and depression continue to hinder recovery. This study addresses these dimensions within the context of ischemic stroke. Aim: The aim of this study was to analyze the cognitive status, functionality, and depressive symptoms in patients with ischemic stroke, exploring interrelations between cognitive, functional, and emotional outcomes to prioritize clinical interventions. Design: This was an analytical, observational, cohort, and prospective study. Methods: The study included 81 subjects diagnosed with ischemic stroke admitted to the Neurology Department of Lucus Augusti University Hospital. Data were collected at three time points—admission, discharge, and follow-up—using validated instruments such as the National Institutes of Health Stroke Scale, Mini-Mental State Examination, Barthel Index, and Beck Depression Inventory. Statistical analyses included Spearman’s correlation, Kruskal–Wallis, and Mann–Whitney tests. Results: Patients with greater cognitive impairment at admission showed poorer functional recovery and higher depressive symptoms during follow-up. Depressive symptoms remained minimal in most cases, but correlations with cognitive and functional deficits were significant. NIHSS scores at admission strongly predicted both functional and emotional recovery, reinforcing its value in early prognosis and therapeutic planning. Conclusions: This study highlights the importance of integrating cognitive, functional, and emotional dimensions into stroke care protocols to optimize patient recovery and improve long-term outcomes.
Full article
(This article belongs to the Section Brain Tumor and Brain Injury)
►▼
Show Figures

Graphical abstract
Open AccessReview
Management of Myasthenic Crisis and Emerging Roles of Molecularly Targeted Therapies: A Narrative Review
by
Seiya Takahashi and Ryuta Kinno
Neurol. Int. 2025, 17(10), 163; https://doi.org/10.3390/neurolint17100163 - 8 Oct 2025
Abstract
Myasthenia gravis (MG) is a chronic autoimmune disorder characterized by fluctuating skeletal muscle weakness. Myasthenic crisis (MCr), a severe and potentially life-threatening complication, presents with respiratory failure and requires intensive care and rapid immunomodulatory intervention. Conventional MCr treatments—such as plasma exchange (PLEX), intravenous
[...] Read more.
Myasthenia gravis (MG) is a chronic autoimmune disorder characterized by fluctuating skeletal muscle weakness. Myasthenic crisis (MCr), a severe and potentially life-threatening complication, presents with respiratory failure and requires intensive care and rapid immunomodulatory intervention. Conventional MCr treatments—such as plasma exchange (PLEX), intravenous immunoglobulin (IVIG), and intravenous methylprednisolone (IVMP)—remain standard treatments; however, they present significant limitations, including delayed onset of action, adverse effects, and inconsistent efficacy. Recent therapeutic advances have led to the development of molecularly targeted therapies based on MG pathophysiology, particularly neonatal Fc receptor (FcRn) inhibitors and complement inhibitors, which have shown efficacy in refractory or maintenance settings. This review explores the potential application of these agents in MCr. We review published case reports involving FcRn inhibitors (efgartigimod, efgartigimod-SC, rozanolixizumab) and complement inhibitors (eculizumab, ravulizumab, zilucoplan), highlighting their rapid onset of action and safety profiles in MCr. While efgartigimod and eculizumab are the most commonly reported agents in MCr, data remain limited to small case series. Emerging evidence suggests these agents may offer effective alternatives to conventional therapies, with favorable safety and potential for rapid symptom resolution. We also discuss strategic considerations for therapy selection, including antibody subtype, coexisting autoimmune conditions, genetic factors, and transition to long-term maintenance. Though the current evidence is promising, large-scale randomized studies are needed to establish definitive roles for these therapies in MCr management.
Full article
(This article belongs to the Section Movement Disorders and Neurodegenerative Diseases)
►▼
Show Figures
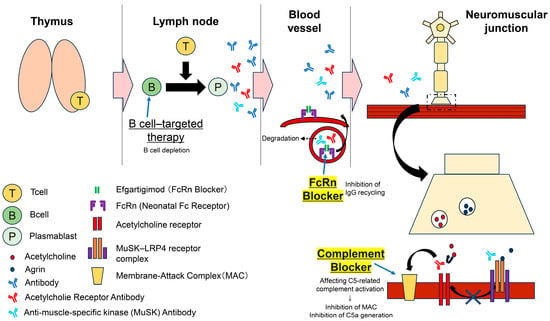
Figure 1
Open AccessArticle
Genetics of Frontotemporal Dementia in the Serbian Population: Findings from a Hospital-Based Cohort
by
Vuk Milošević, Jelena Bašić, Marija Semnic, Eva Antić, Marina Malobabić and Milan Stoiljković
Neurol. Int. 2025, 17(10), 162; https://doi.org/10.3390/neurolint17100162 - 7 Oct 2025
Abstract
Background and objectives: Frontotemporal dementia (FTD) is a heterogeneous neurodegenerative disorder with autosomal dominant forms most often linked to MAPT, GRN, and C9orf72. We aimed to evaluate the prevalence of pathogenic variants in these genes in a hospital-based cohort of
[...] Read more.
Background and objectives: Frontotemporal dementia (FTD) is a heterogeneous neurodegenerative disorder with autosomal dominant forms most often linked to MAPT, GRN, and C9orf72. We aimed to evaluate the prevalence of pathogenic variants in these genes in a hospital-based cohort of FTD patients assessed at a tertiary referral center in southeastern Serbia. Methods: We studied 58 consecutive patients with FTD spectrum syndromes evaluated at a tertiary referral center. All underwent standardized neurological, neuropsychological, and imaging assessments, and family history was recorded. Genetic testing included validated assays for C9orf72 repeat expansions and next-generation sequencing of MAPT and GRN. Results: Women comprised 53.45% of the cohort. The mean age was 67.88 years, with mean onset at 61.70 years. Behavioral variant FTD predominated (75.87%), while language forms were less frequent. Positive family history was present in 16 patients (27.59%). Pathogenic variants were identified in three individuals (5.17%): two unrelated carriers of the intronic MAPT mutation c.1920+16C>T and one patient with a C9orf72 expansion. No GRN variants were detected. Mutation frequency was 18.75% in familial cases, while none were found among sporadic patients (p = 0.018). Four of nine relatives were asymptomatic MAPT mutation carriers. Conclusions: This first genetic study of FTD in southeastern Serbia revealed a lower mutation frequency than in Northern and Western Europe, but similar to cohorts from Southeastern Europe. The detection of MAPT c.1920+16C>T in two unrelated families extends the geographic range of this splice-site variant and underscores the importance of systematic genetic testing and larger collaborative studies in the Balkans.
Full article
(This article belongs to the Section Movement Disorders and Neurodegenerative Diseases)
►▼
Show Figures

Graphical abstract
Open AccessArticle
Risk of Cognitive Decline in Women with Parkinson’s Disease Is Reduced by Early Age at Menarche
by
Giuseppe Schirò, Carlo Fazio, Paolo Aridon, Cesare Gagliardo, Chiara Davì, Valentina Picciolo, Tiziana Colletti, Chiara Tumminia, Salvatore Iacono, Paolo Ragonese and Marco D’Amelio
Neurol. Int. 2025, 17(10), 161; https://doi.org/10.3390/neurolint17100161 - 5 Oct 2025
Abstract
Background: Parkinson’s disease (PD) is a neurodegenerative disorder affecting men more frequently than women, a difference that might be due to many factors, including sexual hormones. Estrogens seem to confer a protective effect on the nigrostriatal pathway in experimental studies but their effects
[...] Read more.
Background: Parkinson’s disease (PD) is a neurodegenerative disorder affecting men more frequently than women, a difference that might be due to many factors, including sexual hormones. Estrogens seem to confer a protective effect on the nigrostriatal pathway in experimental studies but their effects on cognition in patients with PD are unknown. Aim: To investigate the impact of the exogenous and endogenous estrogens on cognitive impairment in women with PD. Methods and materials: We recruited and consecutively interviewed outpatient women affected by PD. Each patient underwent a cognitive assessment via the Montreal Cognitive Assessment scale (MoCA), an anamnestic collection of the reproductive lifespan variables and clinical features. We investigated if some of the reproductive lifespan variables investigated could predict cognition outcomes in post-menopausal women with PD. Results: A total of 90 women with PD were recruited. Women with MoCA ≥ 26 (n = 27) had a lower median age at menarche (11 [11,12] vs. 13 [12–14], p < 0.0001), lower disease duration in years (8.3 [6.1–12.7] vs. 9.4 [6–12.7], p = 0.6), and less advanced disease (1 [1,2] vs. 2 [1–3], p = 0.02). Among all the reproductive life-span variables, only earlier age at menarche significantly predicted higher scores on MoCA (aOR = 0.5 [0.3–0.8], p = 0.005). No other clinical and reproductive factors have been shown to have an influence on cognitive scores. Conclusions: Age at menarche correlated with cognitive outcomes. Our study suggests that earlier exposure to endogenous estrogens during a phase of development and plasticity of the brain might preserve women with PD from cognitive decline.
Full article
(This article belongs to the Section Aging Neuroscience)
►▼
Show Figures

Figure 1
Open AccessSystematic Review
PRISMA Systematic Review of Electroencephalographic (EEG) Microstates as Biomarkers: Secondary Findings in Memory Functions
by
Fernan Alexis Casas Osorio, Leonardo Juan Ramirez Lopez and Diego Renza Torres
Neurol. Int. 2025, 17(10), 160; https://doi.org/10.3390/neurolint17100160 - 4 Oct 2025
Abstract
Background: Monitoring brain activity through electroencephalography (EEG) has led to significant advancements in the study of brain microstates and their relationship with cognitive processes, such as memory. Objective: A systematic literature review was conducted following the PRISMA methodology, with the aim
[...] Read more.
Background: Monitoring brain activity through electroencephalography (EEG) has led to significant advancements in the study of brain microstates and their relationship with cognitive processes, such as memory. Objective: A systematic literature review was conducted following the PRISMA methodology, with the aim of identifying and analyzing potential biomarkers of memory functions derived from EEG microstate analysis. Methods: Searches were performed in five major databases (PubMed, Scopus, Web of Science, Springer, and institutional registers), covering studies published between 2019 and 2024. The initial search retrieved 179 records; after removing duplicates and ineligible works, 18 full-text articles were evaluated. Finally, 10 original studies met the inclusion criteria. Although primarily focused on other pathologies or baseline conditions, these studies reported relevant findings related to memory processes. This allowed for an exploratory synthesis of the potential role of EEG microstates as indirect biomarkers of memory. Results: The findings revealed that microstates, particularly microstates C and D, show significant alterations in their duration, coverage, and occurrence in various pathologies, such as Alzheimer’s disease, schizophrenia, and attention disorders, highlighting their potential as noninvasive biomarkers. Conclusions: Although methodological variability across studies represents a limitation, this review provides a solid foundation for future research aimed at standardizing the use of EEG microstates in clinical applications, improving diagnostic accuracy in memory-related diseases. Overall, EEG microstates hold great promise in both neuroscientific research and clinical practice.
Full article
(This article belongs to the Section Aging Neuroscience)
►▼
Show Figures

Figure 1
Open AccessReview
Clinical Methods Supporting Initial Recognition of Early Post-Stroke Seizures: A Systematic Scoping Review
by
Clare Gordon, Hedley C. A. Emsley, Catherine Elizabeth Lightbody, Andrew Clegg, Catherine Harris, Joanna Harrison, Jasmine Wall, Catherine E. Davidson and Caroline L. Watkins
Neurol. Int. 2025, 17(10), 159; https://doi.org/10.3390/neurolint17100159 - 3 Oct 2025
Abstract
Background: Stroke is a leading cause of seizures and epilepsy, both of which are linked to increased mortality, disability, and hospital readmissions. Early recognition and management of seizures in acute stroke are crucial for improving outcomes. Electroencephalogram (EEG) is not routinely used for
[...] Read more.
Background: Stroke is a leading cause of seizures and epilepsy, both of which are linked to increased mortality, disability, and hospital readmissions. Early recognition and management of seizures in acute stroke are crucial for improving outcomes. Electroencephalogram (EEG) is not routinely used for post-stroke seizure monitoring and is typically initiated only after clinical suspicion arises, making bedside recognition essential. This scoping review aimed to map the existing literature on clinical methods used for identifying and observing early post-stroke seizures (EPSSs) at the bedside. Methods: We included literature involving adults with acute ischaemic stroke or primary intracerebral haemorrhage who were diagnosed or suspected of having inpatient EPSS. Searches were conducted in Medline, CINAHL, Embase, and the Cochrane Library for English-language publications up to April 2023. Eligible sources included primary research, case reports, systematic reviews, clinical guidelines, consensus statements, and expert opinion. Reference lists of included articles were also reviewed. Data were charted and synthesised to assess the scope, type, and gaps in the evidence. Results: Thirty papers met inclusion criteria: 17 research studies, six expert opinions, four case reports, and three clinical guidelines. Empirical evidence on clinical methods for seizure recognition and monitoring in acute stroke was limited. No studies evaluated the effectiveness of different approaches, and existing recommendations lacked detail and consensus. Conclusions: Accurate EPSS diagnosis is vital due to its impact on outcomes. This review highlights inconsistency in monitoring methods and a clear need for targeted research into effective clinical identification strategies in acute stroke care.
Full article
(This article belongs to the Section Movement Disorders and Neurodegenerative Diseases)
►▼
Show Figures

Figure 1
Open AccessReview
Deep Brain Stimulation: Psychological and Neuroethical Perspectives
by
Stella Sremic, Antea Krsek and Lara Baticic
Neurol. Int. 2025, 17(10), 158; https://doi.org/10.3390/neurolint17100158 - 2 Oct 2025
Abstract
Deep brain stimulation (DBS) is an evolving neurosurgical treatment, originally developed for movement disorders such as Parkinson’s disease, essential tremor, and dystonia. In recent years, it has been increasingly applied to psychiatric and cognitive disorders. This review aimed to summarize the psychological and
[...] Read more.
Deep brain stimulation (DBS) is an evolving neurosurgical treatment, originally developed for movement disorders such as Parkinson’s disease, essential tremor, and dystonia. In recent years, it has been increasingly applied to psychiatric and cognitive disorders. This review aimed to summarize the psychological and neuroethical dimensions of DBS, with particular attention to cognitive, emotional, and personality-related outcomes. While DBS can significantly enhance quality of life, it may also lead to subtle or overt changes in cognition, affect, and self-perception, especially in patients with neuropsychiatric comorbidities. Comprehensive psychological evaluation, both pre- and post-operatively, is essential. Findings from recent trials highlight a balance of potential risks and benefits that must be communicated transparently to patients. From a neuroethical perspective, DBS raises important questions regarding personal identity and autonomy, concerns that will become increasingly relevant as the technology advances. This paper underscores the need for more systematic research and the development of personalized care protocols that address not only motor outcomes but also psychosocial well-being.
Full article
(This article belongs to the Section Movement Disorders and Neurodegenerative Diseases)
►▼
Show Figures

Figure 1
Open AccessReview
Is Vitamin B6 a Precision Therapy for Neonatal Seizures?
by
Raffaele Falsaperla, Vincenzo Sortino, Bruna Scalia and Marco Andrea Nicola Saporito
Neurol. Int. 2025, 17(10), 157; https://doi.org/10.3390/neurolint17100157 - 1 Oct 2025
Abstract
Background: Neonatal seizures are critical neurological events with long-term implications for brain development. Standard antiseizure medications, such as phenobarbital, often yield suboptimal seizure control and may be associated with neurotoxicity. This narrative review explores the role of vitamin B6 as a precision
[...] Read more.
Background: Neonatal seizures are critical neurological events with long-term implications for brain development. Standard antiseizure medications, such as phenobarbital, often yield suboptimal seizure control and may be associated with neurotoxicity. This narrative review explores the role of vitamin B6 as a precision therapy in neonatal seizure syndromes, particularly in pyridoxine-responsive conditions. Methods: We conducted a narrative review of the biochemical functions of vitamin B6, focusing on its active form, pyridoxal 5′-phosphate (PLP), and its role as a coenzyme in neurotransmitter synthesis. We examined the genetic and metabolic disorders linked to vitamin B6 deficiency, such as mutations in pyridox(am)ine 5’-phosphate oxidase (PNPO), Aldehyde Dehydrogenase 7 Family Member A1 (ALDH7A1), alkaline locus phosphatase (ALPL), and cystathionine β-synthase (CBS), and discussed the clinical rationale for empirical administration in acute neonatal seizure settings. Results: Vitamin B6 is essential for the synthesis of gamma-aminobutyric acid (GABA), dopamine, and serotonin, with PLP-dependent enzymes such as glutamic acid decarboxylase and aromatic L-amino acid decarboxylase playing central roles. Deficiencies in PLP due to genetic mutations or metabolic disruptions can result in treatment-resistant neonatal seizures. Early supplementation, especially in suspected vitamin B6-dependent epilepsies, may provide both diagnostic clarity and seizure control, potentially reducing exposure to conventional antiseizure medications. Conclusions: Vitamin B6-responsive epilepsies highlight the clinical value of mechanism-based, individualized treatment approaches in neonatology. Incorporating genetic and metabolic screening into seizure management may improve outcomes and aligns with the principles of precision medicine.
Full article
(This article belongs to the Section Movement Disorders and Neurodegenerative Diseases)
►▼
Show Figures

Graphical abstract
Open AccessSystematic Review
The Neuroanatomical Correlates of Bladder Filling: An Activation Likelihood Estimation Meta-Analysis of Functional Neuroimaging Studies
by
Christoph Müller and Albert Kaufmann
Neurol. Int. 2025, 17(10), 156; https://doi.org/10.3390/neurolint17100156 - 30 Sep 2025
Abstract
►▼
Show Figures
Background: Urinary continence relies on a complex interplay between urine storage and voiding involving both spinal reflex circuits and supraspinal brain areas to coordinate volun-tary control over emptying. Despite a vast number of studies on the pathophysiology of neurogenic bladder and urge incontinence,
[...] Read more.
Background: Urinary continence relies on a complex interplay between urine storage and voiding involving both spinal reflex circuits and supraspinal brain areas to coordinate volun-tary control over emptying. Despite a vast number of studies on the pathophysiology of neurogenic bladder and urge incontinence, less is known about the central correlates of bladder filling. Methods: An ALE (activation likelihood estimation) meta-analysis including a total count of 14 studies investigating 243 participants under different conditions of bladder filling during functional neuroimaging was performed to demonstrate the neuroanatomical correlates of bladder filling. The literature search and reporting were conducted according to the PRISMA-P 2020 guideline. Data analysis was performed using the GingerAle software version 3.0.2 and was displayed with the Mango software 4.1 on an anatomical MNI template. Results: Synthesizing studies on the functional neuroanatomy of urine storage, bihemispheric clusters of activation in the thalamus, the insula and the cingulate were observed. Conclusion: The present ALE meta-analysis indicates that the supraspinal representation of urine storage involves areas of autonomous–homeostatic processing which allow for the perception of the usually unconscious inner state of bladder filling and enable postponing and voluntary voiding.
Full article

Figure 1
Open AccessSystematic Review
Gut Microbiota, Mild Cognitive Impairment and Dementia: A Systematic Review
by
Claudio Tana, Samanta Moffa, Marco Tana, Claudio Ucciferri and Livia Moffa
Neurol. Int. 2025, 17(10), 155; https://doi.org/10.3390/neurolint17100155 - 28 Sep 2025
Abstract
Background: Alterations of the gut microbiota have been increasingly implicated in the pathogenesis of dementia through mechanisms involving systemic inflammation, immune dysregulation, and gut–brain axis disruption. Clinical evidence, however, remains fragmented. Objectives: This systematic review aimed to characterize gut microbiota profiles in individuals
[...] Read more.
Background: Alterations of the gut microbiota have been increasingly implicated in the pathogenesis of dementia through mechanisms involving systemic inflammation, immune dysregulation, and gut–brain axis disruption. Clinical evidence, however, remains fragmented. Objectives: This systematic review aimed to characterize gut microbiota profiles in individuals with mild cognitive impairment (MCI) or Alzheimer’s dementia (AD), explore mechanistic associations with neurodegeneration, and evaluate the impact of microbiota-targeted interventions on cognitive outcomes. Methods: Following PRISMA 2020 guidelines and a registered protocol (PROSPERO CRD420251074832), PubMed/Medline was searched through May 2025. Eligible studies included randomized controlled trials (RCTs) and cohort and case–control studies assessing microbiota composition or interventions in participants with MCI or AD. Results: Twenty-one studies were included (1 RCT, 20 observational; sample size 22–302). Most used 16S rRNA sequencing; one used shotgun metagenomics. Across cohorts, MCI and AD patients consistently showed reduced short-chain fatty acid-producing bacteria (Faecalibacterium, Ruminococcaceae, Lachnospiraceae) and increased pro-inflammatory taxa (Escherichia/Shigella, Enterobacteriaceae, Bacteroides). Several studies reported reduced microbial diversity. Specific taxa, including Akkermansia muciniphila and Faecalibacterium, were associated with amyloid burden, hippocampal atrophy, and cognitive decline. Environmental and dietary factors influenced microbial composition and cognition. The RCT reported that probiotic supplementation improved inflammatory markers and BDNF levels, although changes in microbiota composition were inconsistent. Conclusions: Gut dysbiosis is strongly associated with cognitive impairment and markers of neurodegeneration. Modulation of the microbiota through diet and probiotics emerges as a promising avenue for dementia prevention and management, though robust longitudinal and interventional studies are needed to confirm causality and therapeutic efficacy.
Full article
(This article belongs to the Section Aging Neuroscience)
►▼
Show Figures

Graphical abstract

Journal Menu
► ▼ Journal Menu-
- Neurology International Home
- Aims & Scope
- Editorial Board
- Instructions for Authors
- Special Issues
- Topics
- Sections & Collections
- Article Processing Charge
- Indexing & Archiving
- Editor’s Choice Articles
- Most Cited & Viewed
- Journal Statistics
- Journal History
- Journal Awards
- Society Collaborations
- Conferences
- Editorial Office
Journal Browser
► ▼ Journal BrowserHighly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Brain Sciences, Neurology International, NeuroSci
Management of Multiple Sclerosis: Past, Present and Promise
Topic Editors: Salvatore Iacono, Paolo RagoneseDeadline: 5 November 2025
Topic in
Brain Sciences, Neurology International, NeuroSci
The Interplay of the Brain, Behavior, and Immunity: Insights and Innovations
Topic Editors: Marinella Coco, Ashutosh TripathiDeadline: 10 December 2025
Topic in
Brain Sciences, Neurology International, NeuroSci
Language: From Hearing to Speech and Writing
Topic Editors: Ana Paula Soares, David ToméDeadline: 31 December 2025
Topic in
Brain Sciences, Neurology International, NeuroSci
Advances in Neurorehabilitation
Topic Editors: Nicola Marotta, Antonio Ammendolia, Ennio LoprestiDeadline: 31 January 2026

Conferences
Special Issues
Special Issue in
Neurology International
Biomarker Research in Neuromuscular Diseases
Guest Editor: Endre PálDeadline: 30 November 2025
Special Issue in
Neurology International
Advances in Molecular Mechanisms of Neurodegenerative Diseases
Guest Editors: Pravin Hivare, Joshna Gadhavi, Cristoforo ComiDeadline: 30 November 2025
Special Issue in
Neurology International
Towards an All-Inclusive Paradigm for Acute Stroke Treatment—Challenges and Innovations
Guest Editors: Riwaj Bhagat, Ekokobe FonkemDeadline: 30 November 2025
Special Issue in
Neurology International
Beyond the Brain: Neurological Involvement in Pediatric Systemic Diseases
Guest Editor: Andrea Domenico PraticòDeadline: 30 November 2025
Topical Collections
Topical Collection in
Neurology International
Advances in Neurodegenerative Diseases
Collection Editors: Vasileios Siokas, Efthimios Dardiotis
Topical Collection in
Neurology International
Biomarkers in Stroke Prognosis
Collection Editors: Dimitrios Tsiptsios, Konstantinos Vadikolias
Topical Collection in
Neurology International
Exclusive Papers from the Editorial Board Members (EBMs) of Neurology InternationalCollection Editor: Junji Yamauchi
Topical Collection in
Neurology International
Feature Papers in Movement Disorders and Neurodegenerative Diseases
Collection Editors: Tibor Hortobágyi, Cristoforo Comi