Patient-Specific Dosimetry Evaluations in Theranostics Software for Internal Radiotherapy
Abstract
1. Introduction
2. Materials and Methods
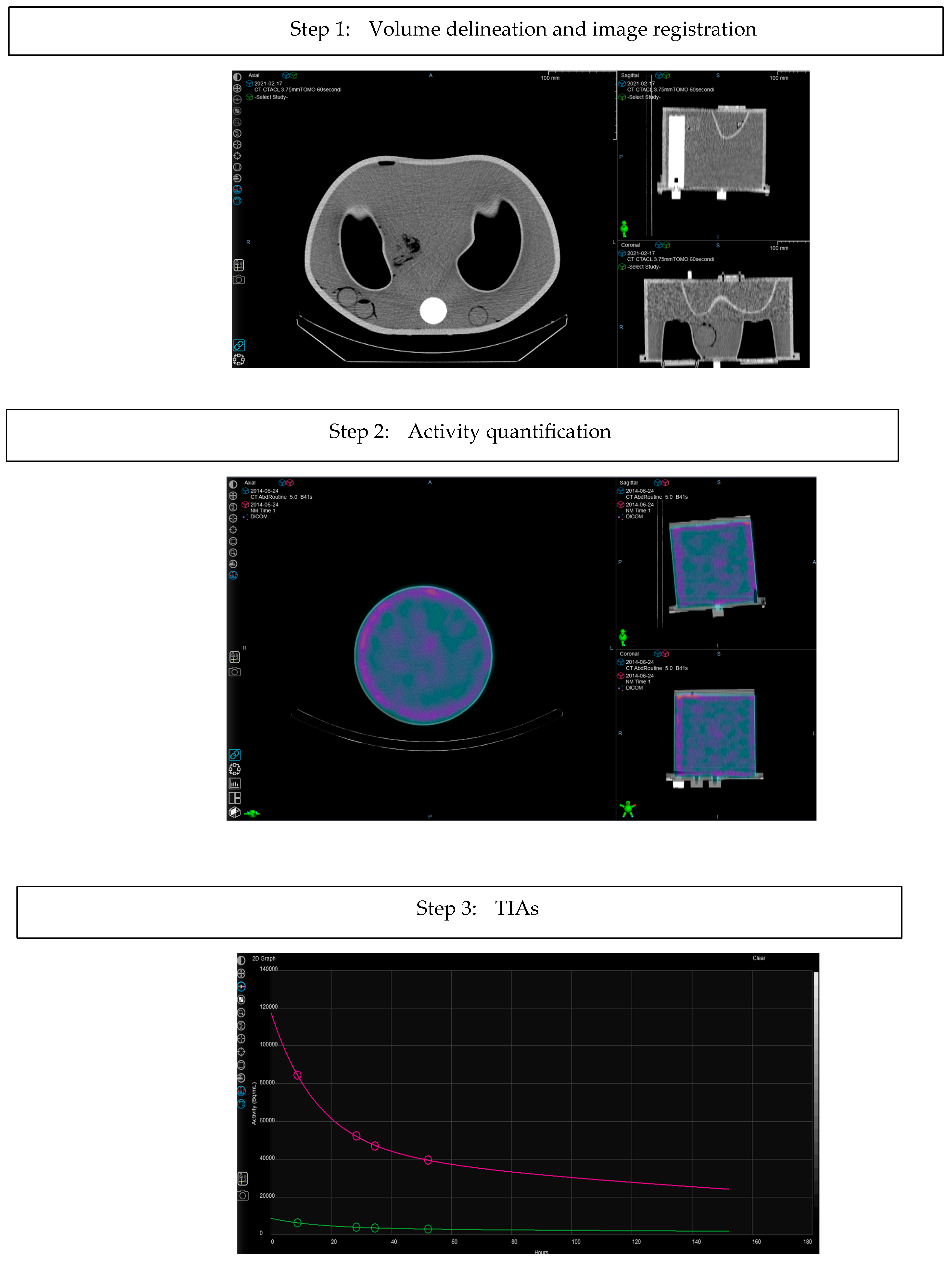
- Volume delineation: Volume of interest (VOI) delineation of Organ at Risk (OAR) and/or lesions is performed using the Velocity contouring tool. This tool enables the user to choose among different options, such as manual contouring, adaptive semi-automatic and threshold-based.
- Image registration: Sequential SPECT/CT images are automatically registered with a deformable algorithm based on CT data.
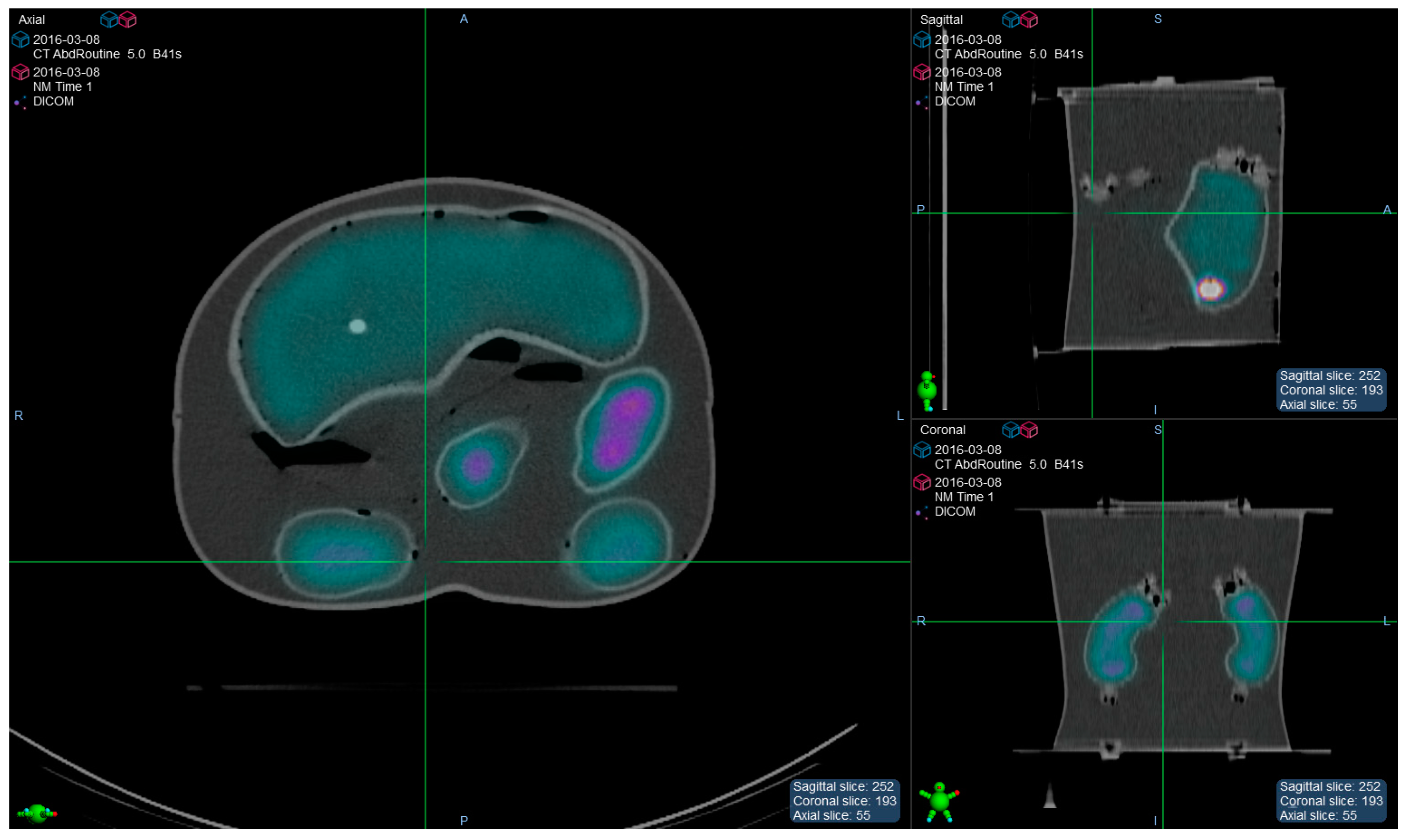
- Activity quantification: The counts–to-activity calibration factor (CF) is entered by the user. It can be extrapolated by acquiring a homogeneous phantom filled with a radioactive solution with the SPECT clinical protocol.
- CT Calibration: The accuracy of the calibration of CT numbers in relation to electron density is a relevant factor for absorbed dose calculations in a not homogeneous medium. It is possible to verify and customize the conversion of Hounsfield units (HU) into material composition and mass density using a tissue characterization phantom.
- Partial Volume Effect (PVE) correction: This can be applied by entering an equation which allows to estimate the recovery coefficients for VOI statistics, that are specific for the SPECT scanner in use.
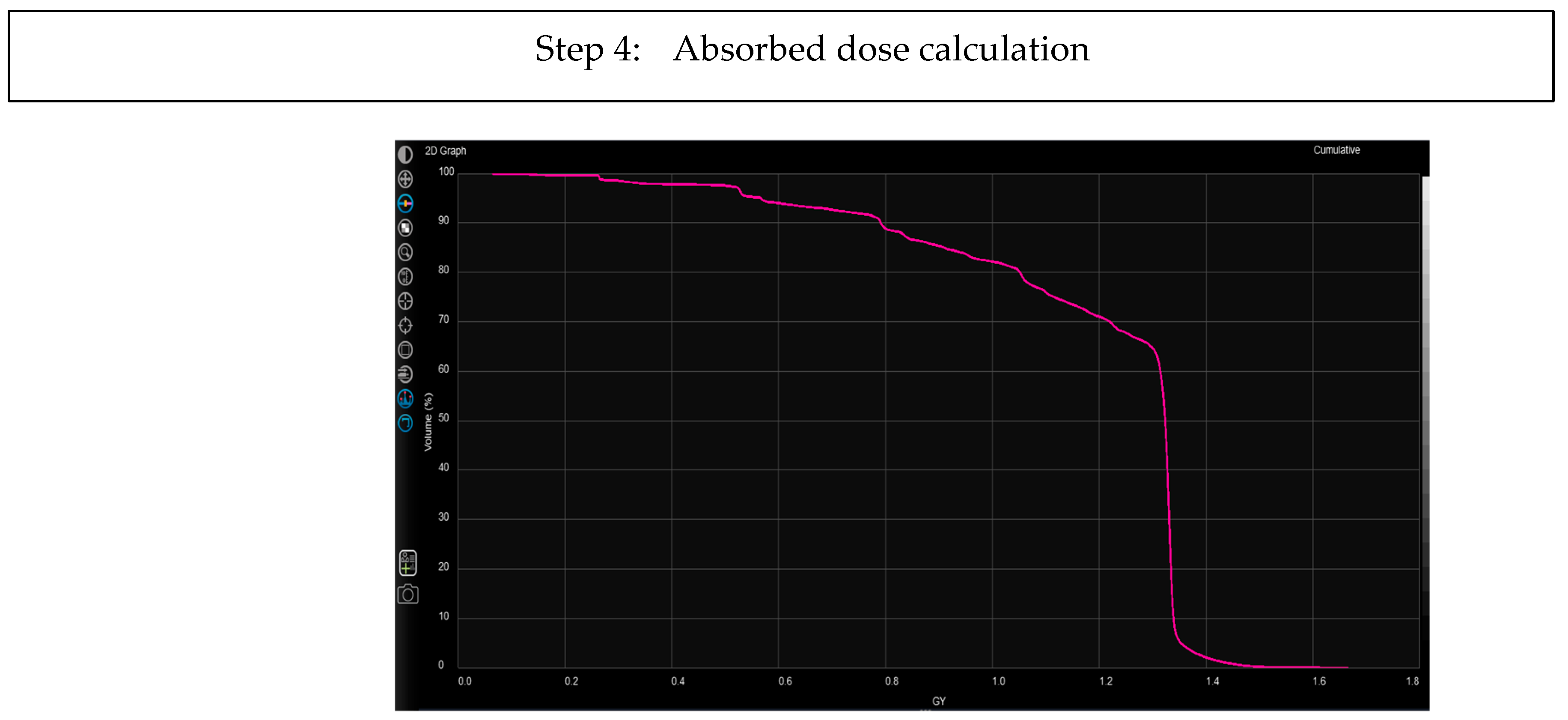
- Time-integrated activities (TIAs): The algorithm uses a fitting technique at voxel level, which estimates a fitting function (sums of exponentials) for each voxel, This process automatically selects the best model from a predefined list of possibilities, using the Akaike Information Criterion (AIC) [17]. The algorithm provides an error metrics statistics section based on the calculation of the symmetric mean absolute percentage error (SMAPE), which allows measuring the accuracy in terms of percentage (or relative) errors.
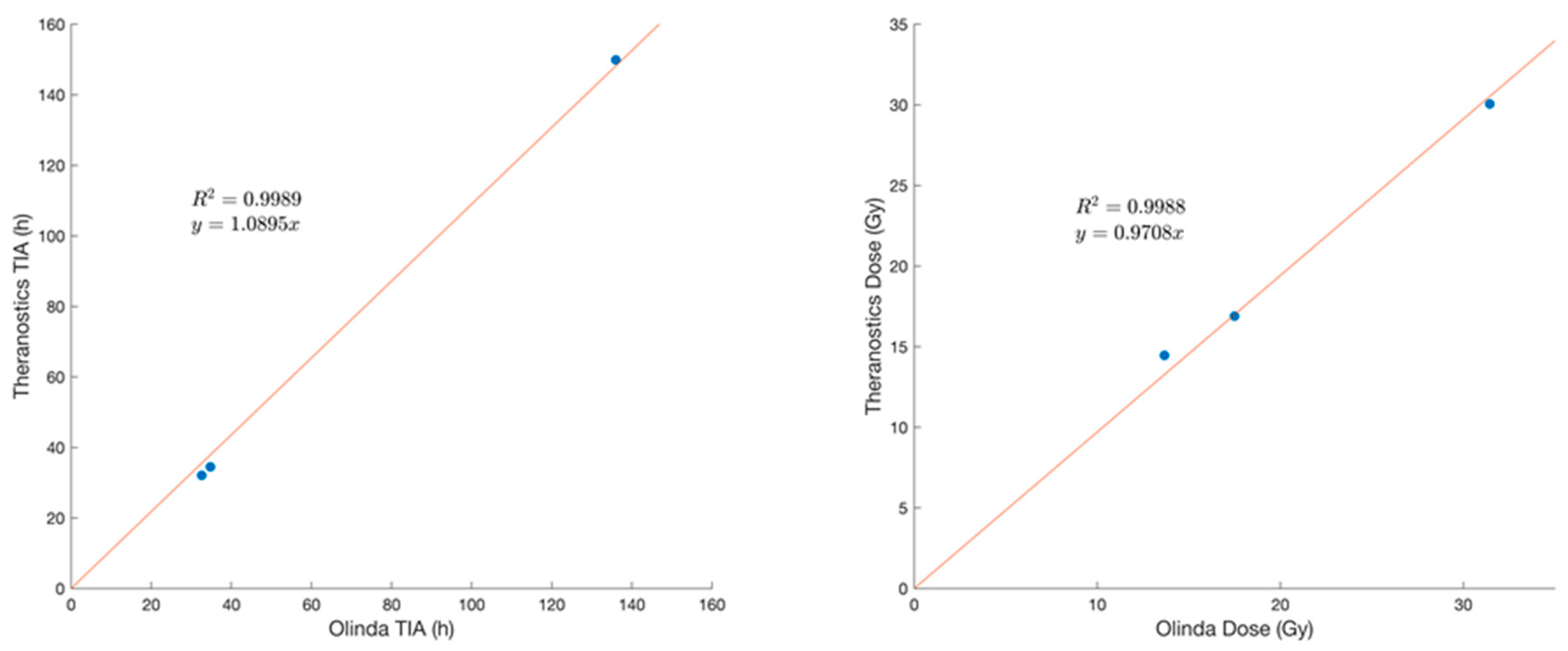
- Absorbed dose calculated with Acuros MRT algorithm: This deterministic solver is customized for internal therapies. It includes the solution of the linear Boltzmann transport equation (LBTE) for photons and the linear Boltzmann-Fokker-Planck transport equation (LBFPTE) for electrons and it takes into account that photon and electron energies for internal therapy applications are significantly lower than the energies used in external beam radiation therapy applications. The performances of the LBTE solver for internal therapies with 177Lu were considered and described in-depth by Kayal G. et al. [18]. The algorithm may perform voxel dosimetry. The resulting dose maps and dose-volume-histograms are then internally elaborated to provide the mean doses absorbed by the structures delineated on SPECT-CT images (organs and lesions). These values may be compared to the absorbed doses calculated by OLINDA 2.0.
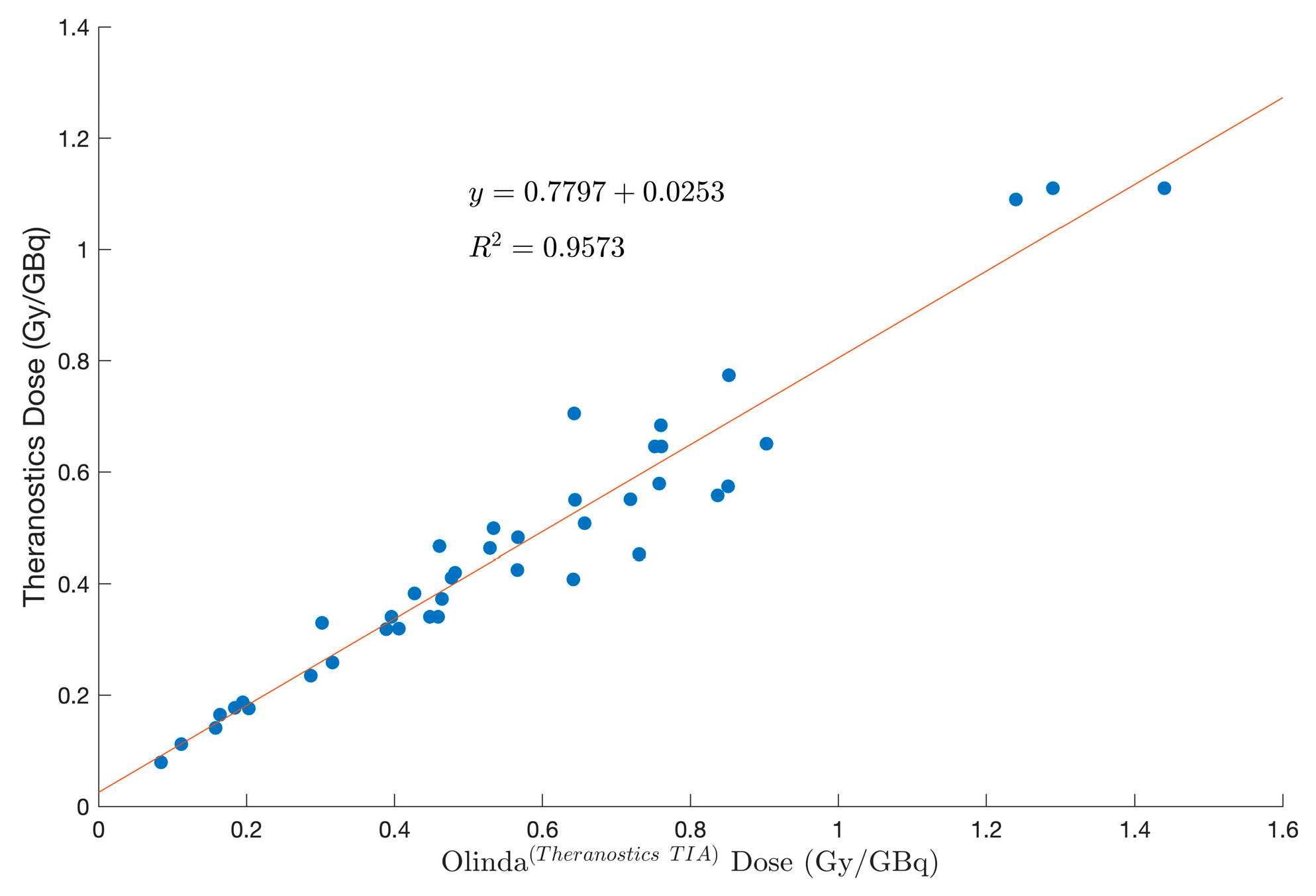
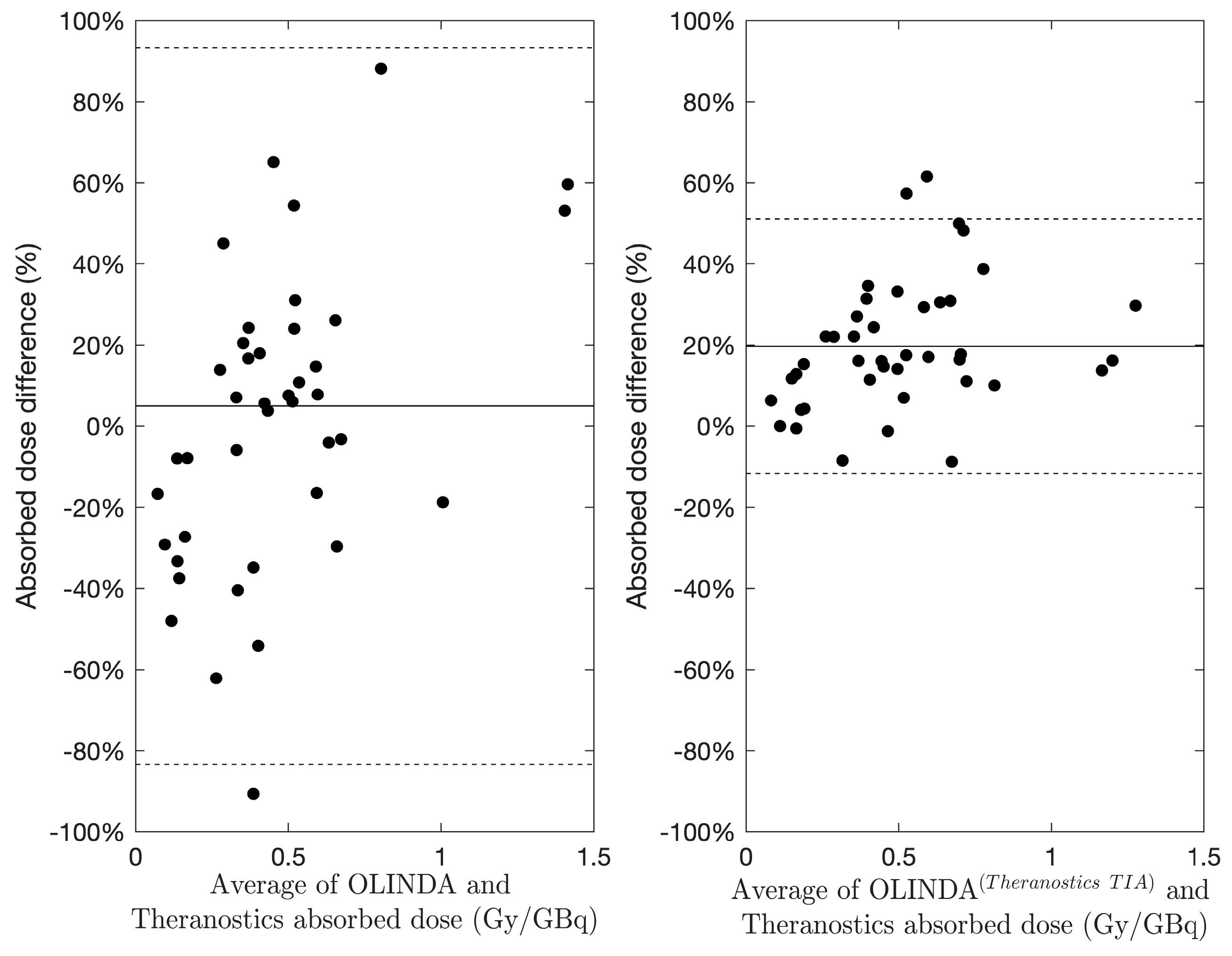
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sgouros, G.; Bodei, L.; McDevitt, M.R.; Nedrow, J.R. Radiopharmaceutical Therapy in Cancer: Clinical Advances and Challenges. Nat. Rev. Drug Discov. 2020, 19, 589–608. [Google Scholar] [CrossRef] [PubMed]
- Kesner, A.L.; Carter, L.M.; Ramos, J.C.O.; Lafontaine, D.; Olguin, E.A.; Brown, J.L.; President, B.; Jokisch, D.W.; Fisher, D.R.; Bolch, W.E. MIRD Pamphlet No. 28, Part 1: MIRDcalc-A Software Tool for Medical Internal Radiation Dosimetry. J. Nucl. Med. 2023, 64, 1117–1124. [Google Scholar] [CrossRef] [PubMed]
- Peters, S.; Tran-Gia, J.; Agius, S.; Ivashchenko, O.V.; Badel, J.N.; Cremonesi, M.; Kurth, J.; Gabiña, P.M.; Richetta, E.; Gleisner, K.S.; et al. Implementation of Dosimetry for Molecular Radiotherapy; Results from a European Survey. Phys. Medica 2024, 117, 103196. [Google Scholar] [CrossRef] [PubMed]
- Sjögreen-Gleisner, K.; Flux, G.; Bacher, K.; Chiesa, C.; de Nijs, R.; Kagadis, G.C.; Lima, T.; Georgosopoulou, M.L.; Gabiña, P.M.; Nekolla, S.; et al. EFOMP Policy Statement NO. 19: Dosimetry in Nuclear Medicine Therapy—Molecular Radiotherapy. Phys. Medica 2023, 116, 103166. [Google Scholar] [CrossRef] [PubMed]
- Chiesa, C.; Strigari, L.; Pacilio, M.; Richetta, E.; Cannatà, V.; Stasi, M.; Marzola, M.C.; Schillaci, O.; Bagni, O.; Maccauro, M. Dosimetric Optimization of Nuclear Medicine Therapy Based on the Council Directive 2013/59/EURATOM and the Italian Law N. 101/2020. Position Paper and Recommendations by the Italian National Associations of Medical Physics (AIFM) and Nuclear Medicine (AIMN). Phys. Medica 2021, 89, 317–326. [Google Scholar] [CrossRef]
- Finocchiaro, D.; Gear, J.I.; Fioroni, F.; Flux, G.D.; Murray, I.; Castellani, G.; Versari, A.; Iori, M.; Grassi, E. Uncertainty Analysis of Tumour Absorbed Dose Calculations in Molecular Radiotherapy. EJNMMI Phys. 2020, 7, 63. [Google Scholar] [CrossRef] [PubMed]
- Gear, J.I.; Cox, M.G.; Gustafsson, J.; Gleisner, K.S.; Murray, I.; Glatting, G.; Konijnenberg, M.; Flux, G.D. EANM Practical Guidance on Uncertainty Analysis for Molecular Radiotherapy Absorbed Dose Calculations. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 2456–2474. [Google Scholar] [CrossRef] [PubMed]
- Marcatili, S.; Pettinato, C.; Daniels, S.; Lewis, G.; Edwards, P.; Fanti, S.; Spezi, E. Development and Validation of RAYDOSE: A Geant4-Based Application for Molecular Radiotherapy. Phys. Med. Biol. 2013, 58, 2491–2508. [Google Scholar] [CrossRef] [PubMed]
- Villoing, D.; Marcatili, S.; Garcia, M.-P.; Bardiès, M. Internal Dosimetry with the Monte Carlo Code GATE: Validation Using the ICRP/ICRU Female Reference Computational Model. Phys. Med. Biol. 2017, 62, 1885–1904. [Google Scholar] [CrossRef]
- Stabin, M.G.; Sparks, R.B.; Crowe, E. OLINDA/EXM: The Second-Generation Personal Computer Software for Internal Dose Assessment in Nuclear Medicine. J. Nucl. Med. 2005, 46, 1023–1027. [Google Scholar] [CrossRef]
- Andersson, M.; Johansson, L.; Eckerman, K.; Mattsson, S. IDAC-Dose 2.1, an Internal Dosimetry Program for Diagnostic Nuclear Medicine Based on the ICRP Adult Reference Voxel Phantoms. EJNMMI Res. 2017, 7, 88. [Google Scholar] [CrossRef] [PubMed]
- Kayal, G.; Barbosa, N.; Marín, C.C.; Ferrer, L.; Fragoso-Negrín, J.-A.; Grosev, D.; Gupta, S.K.; Hidayati, N.R.; Moalosi, T.C.G.; Poli, G.L.; et al. Quality Assurance Considerations in Radiopharmaceutical Therapy Dosimetry Using PLANETDose: An International Atomic Energy Agency Study. J. Nucl. Med. 2024, 65, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Bensiali, M.; Anizan, N.; Leboulleux, S.; Lamart, S.; Davesne, E.; Broggio, D.; Desbrée, A.; Franck, D. Patient-Specific Biokinetics and Hybrid 2D/3D Approach Integration in OEDIPE Software: Application to Radioiodine Therapy. Phys. Medica 2023, 113, 102462. [Google Scholar] [CrossRef] [PubMed]
- Fraass, B.; Doppke, K.; Hunt, M.; Kutcher, G.; Starkschall, G.; Stern, R.; van Dyke, J. American Association of Physicists in Medicine Radiation Therapy Committee Task Group 53: Quality Assurance for Clinical Radiotherapy Treatment Planning. Med. Phys. 1998, 25, 1773–1829. [Google Scholar] [CrossRef] [PubMed]
- Mileva, M.; Marin, G.; Levillain, H.; Artigas, C.; van Bogaert, C.; Marin, C.; Danieli, R.; Deleporte, A.; Picchia, S.; Stathopoulos, K.; et al. Prediction of 177 Lu-DOTATATE PRRT Outcome Using Multimodality Imaging in Patients with Gastroenteropancreatic Neuroendocrine Tumors: Results from a Prospective Phase II LUMEN Study. J. Nucl. Med. 2024, 65, 236–244. [Google Scholar] [CrossRef]
- Stabin, M.G.; Siegel, J.A. RADAR Dose Estimate Report: A Compendium of Radiopharmaceutical Dose Estimates Based on OLINDA/EXM Version 2.0. J. Nucl. Med. 2018, 59, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Sarrut, D.; Halty, A.; Badel, J.; Ferrer, L.; Bardiès, M. Voxel-based Multimodel Fitting Method for Modeling Time Activity Curves in SPECT Images. Med. Phys. 2017, 44, 6280–6288. [Google Scholar] [CrossRef] [PubMed]
- Kayal, G.; Van, B.; Andl, G.; Tu, C.; Wareing, T.; Wilderman, S.; Mikell, J.; Dewaraja, Y.K. Linear Boltzmann Equation Solver for Voxel-level Dosimetry in Radiopharmaceutical Therapy: Comparison with Monte Carlo and Kernel Convolution. Med. Phys. 2024. Early View. [Google Scholar] [CrossRef] [PubMed]
- Grassi, E.; Fioroni, F.; Ferri, V.; Mezzenga, E.; Sarti, M.A.; Paulus, T.; Lanconelli, N.; Filice, A.; Versari, A.; Iori, M. Quantitative Comparison between the Commercial Software STRATOS® by Philips and a Homemade Software for Voxel-Dosimetry in Radiopeptide Therapy. Phys. Medica 2015, 31, 72–79. [Google Scholar] [CrossRef]
- Grassi, E.; Fioroni, F.; Mezzenga, M.; Finocchiaro, D.; Sarti, M.A.; Filice, A.; Versari, A.; Iori, M. Impact of a Commercial 3D OSEM Reconstruction Algorithm on the 177Lu Activity Quantification of SPECT/CT Imaging in a Molecular Radiotherapy Trial. Radiol Diagn Imaging 2017, 1, 1–7. [Google Scholar] [CrossRef]
- Sgouros, G.; Barest, G.; Thekkumthala, J.; Chui, C.; Mohan, R.; Bigler, R.E.; Zanzonico, P.B. Treatment Planning for Internal Radionuclide Therapy: Three-Dimensional Dosimetry for Nonuniformly Distributed Radionuclides. J. Nucl. Med. 1990, 31, 1884–1891. [Google Scholar] [PubMed]
- Grassi, E.; Fioroni, F.; Berenato, S.; Patterson, N.; Ferri, V.; Braglia, L.; Filice, A.; Versari, A.; Iori, M.; Spezi, E. Effect of Image Registration on 3D Absorbed Dose Calculations in 177Lu-DOTATOC Peptide Receptor Radionuclide Therapy. Phys. Med. 2018, 45, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Ivashchenko, O.V.; O’Doherty, J.; Hardiansyah, D.; Cremonesi, M.; Tran-Gia, J.; Hippeläinen, E.; Stokke, C.; Grassi, E.; Sandström, M.; Glatting, G. Time-Activity Data Fitting in Molecular Radiotherapy: Methodology and Pitfalls. Phys. Medica 2024, 117, 103192. [Google Scholar] [CrossRef] [PubMed]
- Fogliata, A.; Nicolini, G.; Clivio, A.; Vanetti, E.; Cozzi, L. Dosimetric Evaluation of Acuros XB Advanced Dose Calculation Algorithm in Heterogeneous Media. Radiat. Oncol. 2011, 6, 82. [Google Scholar] [CrossRef]



| Phantom | Phantom Volume (mL) | Insert Name | Insert Volume (mL) | Insert Activity Concentration (MBq/mL) | Background Activity Concentration (MBq/mL) |
|---|---|---|---|---|---|
| Liqui-Phill phantom | Left kidney | 142 | 0.81 | ||
| 11,600 | Right kidney | 142 | 0.82 | 0.03 | |
| Spleen Liver | 156 1470 | 1.10 0.53 |
| Insert Name | TIA (MBq h/MBq) | Absorbed Dose (Gy) | ||||
|---|---|---|---|---|---|---|
| Olinda 2.0 | Velocity Theranostics | Difference (%) | Olinda 2.0 | Velocity Theranostics | Difference (%) | |
| Kidneys | 34.8 | 34.5 | −0.9 | 17.5 | 16.9 | −3.5% |
| Spleen | 32.6 | 32.1 | −1.56 | 31.44 | 30.06 | −4.4% |
| Liver | 136 | 149.8 | 10.2 | 13.68 | 14.46 | 5.7% |
| Case | Kidneys | Liver | Spleen | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Olinda 2.0 | Velocity Theranostics | OLINDA(Theranostics TIA) | Olinda 2.0 | Velocity Theranostics | OLINDA(Theranostics TIA) | Olinda 2.0 | Velocity Theranostics | OLINDA(Theranostics TIA) | |
| 1 | 0.304 | 0.467 | 0.461 | 0.0605 | 0.705 | 0.643 | — | — | — |
| 2 | 0.440 | 0.373 | 0.464 | 0.295 | 0.259 | 0.316 | — | — | — |
| 3 | 0.575 | 0.464 | 0.529 | 0.136 | 0.187 | 0.195 | 0.563 | 0.341 | 0.459 |
| 4 | 0.321 | 0.341 | 0.448 | 0.398 | 0.341 | 0.396 | 0.619 | 0.574 | 0.851 |
| 5 | 0.253 | 0.551 | 0.719 | 0.110 | 0.176 | 0.203 | 0.145 | 0.383 | 0.427 |
| 6 | 0.519 | 0.483 | 0.567 | 0.0806 | 0.155 | 0.175 | 0.730 | 0.579 | 0.758 |
| 7 | 0.250 | 0.420 | 0.482 | 1.700 | 1.110 | 1.44 | 0.63 | 0.408 | 0.642 |
| 8 | 0.593 | 0.453 | 0.731 | 0.110 | 0.165 | 0.164 | — | — | — |
| 9 | 0.540 | 0.646 | 0.761 | 0.902 | 1.110 | 1.29 | 0.563 | 0.508 | 0.657 |
| 10 | 0.385 | 0.320 | 0.406 | 0.341 | 0.235 | 0.287 | 1.050 | 0.558 | 0.837 |
| 11 | 0.529 | 0.499 | 0.537 | 1.740 | 1.090 | 1.240 | 1.780 | 0.651 | 0.903 |
| 12 | 0.544 | 0.774 | 0.852 | 0.0793 | 0.112 | 0.112 | 0.410 | 0.330 | 0.302 |
| 13 | 0.620 | 0.646 | 0.752 | 0.0661 | 0.0793 | 0.0843 | 0.434 | 0.411 | 0.477 |
| 14 | 0.662 | 0.684 | 0.760 | 0.163 | 0.177 | 0.184 | 0.631 | 0.550 | 0.644 |
| 15 | 0.341 | 0.319 | 0.389 | 0.130 | 0.141 | 0.158 | 0.441 | 0.425 | 0.566 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grassi, E.; Finocchiaro, D.; Fioroni, F.; Andl, G.; Filice, A.; Versari, A.; El Ouati, A.; Spezi, E.; Iori, M. Patient-Specific Dosimetry Evaluations in Theranostics Software for Internal Radiotherapy. Appl. Sci. 2024, 14, 7345. https://doi.org/10.3390/app14167345
Grassi E, Finocchiaro D, Fioroni F, Andl G, Filice A, Versari A, El Ouati A, Spezi E, Iori M. Patient-Specific Dosimetry Evaluations in Theranostics Software for Internal Radiotherapy. Applied Sciences. 2024; 14(16):7345. https://doi.org/10.3390/app14167345
Chicago/Turabian StyleGrassi, Elisa, Domenico Finocchiaro, Federica Fioroni, George Andl, Angelina Filice, Annibale Versari, Ayman El Ouati, Emiliano Spezi, and Mauro Iori. 2024. "Patient-Specific Dosimetry Evaluations in Theranostics Software for Internal Radiotherapy" Applied Sciences 14, no. 16: 7345. https://doi.org/10.3390/app14167345
APA StyleGrassi, E., Finocchiaro, D., Fioroni, F., Andl, G., Filice, A., Versari, A., El Ouati, A., Spezi, E., & Iori, M. (2024). Patient-Specific Dosimetry Evaluations in Theranostics Software for Internal Radiotherapy. Applied Sciences, 14(16), 7345. https://doi.org/10.3390/app14167345







