Diagnosis and Management of Acute Ischemic Stroke
Topic Information
Dear Colleagues,
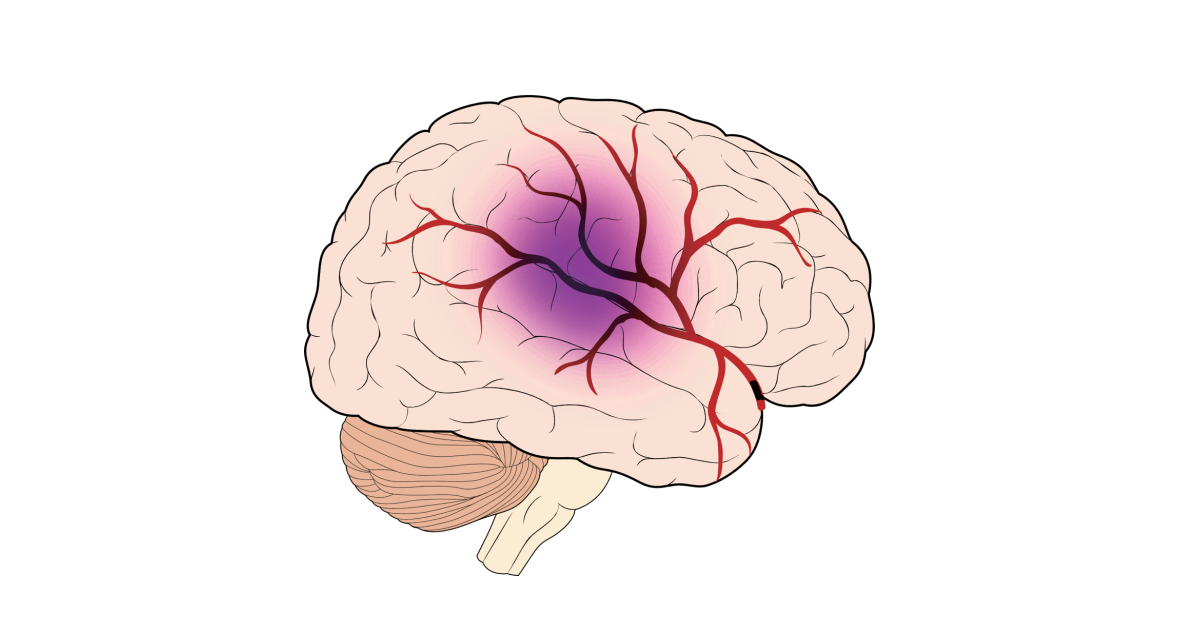
Stroke is the second most common cause of mortality and the second most common cause of disability worldwide. Various risk factors are associated with stroke including high blood pressure, diabetes, smoking, hyperlipidemia, cardiac disease, being overweight, and air pollution. While an etiologic diagnosis of stroke is critical for the secondary prevention of stroke, determining the etiologic classification of stroke is still probabilistic. Atherosclerosis, cardiac embolism, and lacunar infarction are the major causes of stroke. There are other, rare causes of stroke, especially in young age groups. Of all ischemic stroke patients, 9–25% are classified as embolic stroke of undetermined source (ESUS). ESUS is a heterogenous category and its management is challenging to physicians. The treatment of stroke should be individualized according to stroke subtype. An acute period of stroke is dynamic and the most important determinant of future prognosis. The use of recombinant tissue plasminogen activator (rtPA) has been the standard of care for the treatment of acute ischemic stroke for over two decades. However, low efficacy and potential harmfulness limit its effectiveness. Recent randomized trials and subsequent meta-analysis have consolidated the role of endovascular thrombectomy (EVT) in stroke patients with a large cerebral artery occlusion. The recanalization rate of EVT is approximately 80%, but only 50% of patients achieve functional independence. Therefore, new treatment strategies are needed to reduce the rate of poor outcomes. After the acute period, patients with stroke require tailored secondary prevention according to presumed etiologies. Antiplatelets, anticoagulants, and statins are the mainstay of secondary prevention. Risk factor control for individual patients should be achieved. Our Topic Issue will consider original articles, commentaries, and review articles that focus on the following potential topics (but not limited to these):
- Imaging and clinical diagnosis of stroke.
- Diagnosis and management of embolic stroke of undetermined source (ESUS).
- Clinical aspects of stroke.
- Artificial intelligence, mobile health and machine learning in stroke.
- Determinant of outcome after stroke.
- Pharmacologic intervention of stroke.
- Genetics in stroke.
- Determinants improving reperfusion therapy.
- Improving recanalization rate and outcomes in endovascular thrombectomy (EVT).
- Treatment and prognosis according to comorbidity and stroke subtype.
- Secondary stroke prevention according to comorbidity and stroke subtype.
- Improving treatment and prognosis using novel and practical tools.
- Cost-effective analysis of stroke.
- Application of neurosonology.
- Gut microbiota and stroke.
- Basic research in stroke.
- Epidemiology study of stroke.
Dr. Hyo Suk Nam
Dr. Byung Moon Kim
Dr. Tae-jin Song
Dr. Minho Han
Topic Editors
Keywords
- ischemic stroke
- comorbidity
- intervention
- precision medicine
- prevention
- prognosis
- rehabilitation
- risk factors
- treatment
- subtype