Background: Overweight and obesity in childhood and adolescence represent one of the most significant public health challenges of our century. Affected children and adolescents often face psychosocial maladaptation, including low self-esteem, depressive and anxiety symptoms, and behavioral problems, many of which may
[...] Read more.
Background: Overweight and obesity in childhood and adolescence represent one of the most significant public health challenges of our century. Affected children and adolescents often face psychosocial maladaptation, including low self-esteem, depressive and anxiety symptoms, and behavioral problems, many of which may persist till later in life. The aim of our study was to evaluate the impact of a multidisciplinary, personalized lifestyle intervention program on psychosocial and behavioral symptoms, assessed through standardized psychometric questionnaires, and to investigate their relation with cardiometabolic parameters in children and adolescents with overweight and obesity.
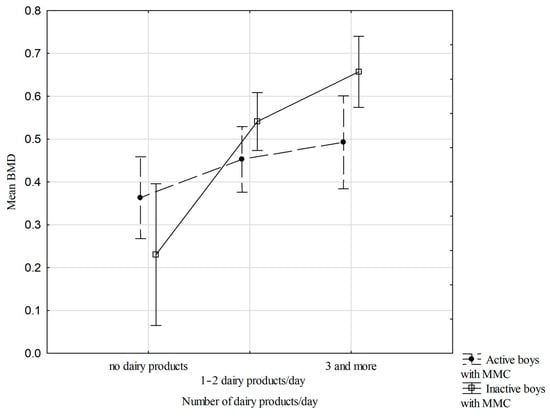
Methods: In this prospective cohort study, 537 children and adolescents (6–18 years; females: 52.9%; pubertal: 43.6%) with obesity (n = 44.3%), overweight (n = 33.7%), or normal BMI (n = 22%) participated in a personalized lifestyle intervention program for one year. Clinical and laboratory evaluations, including anthropometric, cardiometabolic, and endocrinologic parameters, as well as psychosocial functioning assessed by the Child Behavior Checklist (CBCL) and Youth Self-Report (YSR), were performed at the beginning and the end of the study. Linear regression analyses identified predictors of psychometric change.
Results: At initial evaluation, children and adolescents with obesity displayed a less favorable cardiometabolic profile and greater emotional/conduct difficulties compared to their overweight and normal-BMI counterparts. Following the intervention, significant improvements were observed in BMI, anthropometric and cardiometabolic parameters, as well as reductions in internalizing, externalizing, and total problem scores across multiple CBCL and YSR domains (
p < 0.05). The improvements in psychosocial functioning were partly independent of BMI reduction. Linear regression analyses identified cardiometabolic and endocrine markers as significant predictors of psychometric change (
p < 0.05), highlighting interactions between metabolic recovery, pubertal hormones, and stress physiology.
Conclusions: A personalized, multidisciplinary lifestyle intervention program implemented for 1 year led to parallel improvements in psychosocial and cardiometabolic health in children and adolescents with overweight and obesity. Identification of specific metabolic and endocrine predictors provides novel insights into potential biological mechanisms associated with adiposity, emotional well-being, and neurodevelopment.
Full article